Abstract
Context
Advance care planning (ACP) is essential to elicit goals, values, and preferences of care in older adults with serious illness and on trajectories of frailty. An exploration of ACP uptake in older adults may identify barriers and facilitators.
Objective
To conduct an integrative review of research on the uptake of ACP in older adults and create a conceptual model of the findings.
Methods
Using Whittemore and Knafl's methodology, we systematically searched four electronic databases of ACP literature in older adults from 1996 through December 2019. Critical appraisal tools were used to assess study quality, and articles were categorized according to level of evidence. Statistical and thematic analysis was then undertaken.
Results
Among 1081 studies, 78 met inclusion criteria. Statistical analysis evaluated ACP and variables within the domains of demographics, psychosocial, disability and functioning, and miscellaneous. Thematic analysis identified a central category of enhanced communication, followed by categories of 1) provider role and preparation; 2) patient/family relationship patterns; 3) standardized processes and structured approaches; 4) contextual influences; and 5) missed opportunities. A conceptual model depicted categories and relationships.
Conclusions
Enhanced communication and ACP facilitators improve uptake of ACP. Clinicians should be cognizant of these factors. This review provides a guide for clinicians who are considering implementation strategies to facilitate ACP in real-world settings.
Key Words: Advance care planning, communication, patient- and family-centered, older adults, conceptual model
Introduction
“It's always too early, until it's too late,” the words of the Conversation Project describe the not uncommon end-of-life (EOL) planning for older adults. “Too late” often means that an older adult has encountered a crisis (fall, sudden illness, exacerbation) in which he/she is unable to relay or express personal preferences about EOL care, thus underscoring the need for advance care planning (ACP). ACP enables patients and their families to identify and plan the care and treatments that are acceptable to them and that are consistent with their personal values and preferences.1
The growing field of palliative care and the rapidly aging population underscore the importance of ACP, given longevity may be accompanied by serious illness, symptom burden, functional dependence and frailty, caregiver burden, and high health-care utilization.2 , 3 The Institute of Medicine's (IOM) 2014 Dying in America report emphasized the need for new models of care that promote ACP conversations.4 Despite the medical, legal, and pragmatic utility and benefits of ACP, uptake remains below 20%,5 and EOL communication is still lacking in all clinical settings, including long-term care.6 Discussing ACP with older adults who face the end of life with greater uncertainty is an underexplored area of research. While risk prediction and prognostication related to aging and frailty is difficult at the individual level, the need for ACP before a crisis event is paramount.
In light of the need to improve ACP efforts in health care for older patients with and without a serious illness and looming frailty, we wished to explore ACP efforts directed specifically at uptake in older adults. Other recent systematic reviews related to ACP in older adults address other facets including specific conditions (heart failure, cancer)7 , 8; attitudes, experiences, and perspectives of older adults9 , 10; and outcomes of ACP.11 , 12 One review addressed barriers and facilitators of ACP in an acute care setting, but the section was brief and reported from three studies.12 We sought to take a deeper dive to better understand approaches (or lack of) to ACP that influence uptake and completion of the ACP process. Such an exploration might provide insight for future research and clinical practice in this growing population. Thus, the specific aim of this encompassing integrative review was to explore the literature that describes uptake of ACP in older adults and to create a conceptual model of relationships leading to ACP outcomes. Within this review, we define uptake according to Merriam-Webster's definition as “making use of” or “an act of absorbing and incorporating”.13 ACP is defined as a process that supports adults at any age or health status in understanding and sharing their values, goals, and preferences regarding future medical care.14
Material and Methods
The integrative review methodology, introduced by Whittemore and Knafl,15 allows for the combination of qualitative and quantitative methodologies to inform evidence-based practice. Although randomized controlled trials remain the gold standard for determining the efficacy of interventions, other studies can shed light on other important considerations. Integrative reviews capture a broader perspective to more fully understand a phenomenon through the inclusion of observational and experimental research.15 An integrative approach was selected for this review because of the growing population of older adults who are reaching their 90s and 100s with and without overriding chronic conditions and frailty in the final phase of life. A broad examination of multiple research designs can strengthen our understanding of ACP in this population and inform future research and clinical practice.
Literature Search
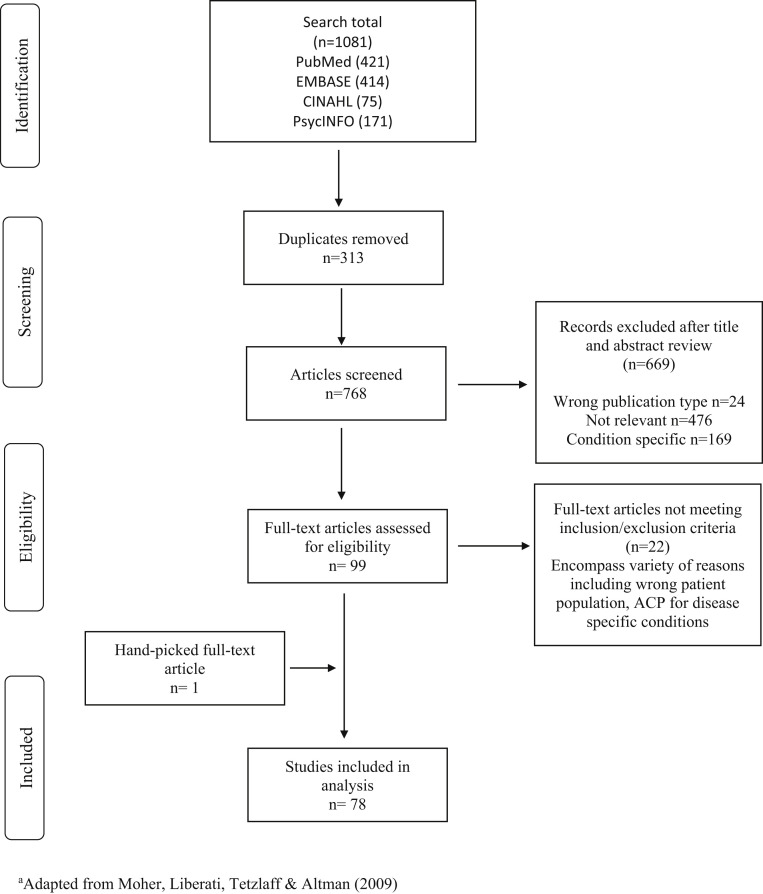
A search strategy was developed in collaboration with a coauthor medical librarian (R.L.W.). The search included MeSH terms: “advance care planning,” OR “advance directives,” OR “living wills,” AND “patient preferences,” OR “consumer participation,” OR “patient participation,” OR “personal autonomy” in multiple combinations. A filter of age 65 years and older was placed on each search. A comprehensive search was conducted through December 2019 in PubMed, CINAHL, PsycINFO, and Embase (Figure 1 ).
Fig. 1.
Prisma flow diagram.a ACP = advance care planning.
Studies were included if they met the following criteria: 1) addressed three factors: a) components of ACP (advance directives, identification of healthcare proxy, discussions with patients, families, and health-care providers), b) ACP uptake, and c) older adults; 2) peer-reviewed; 3) published in English; 4) featured primary research (data collected directly by investigators); and 5) encompassed serious illness, including frailty. Exclusion criteria included 1) published in a non-English language; 2) opinion articles, study protocols, case studies, and conference abstracts; 3) systematic reviews; and 4) focused on ACP for specific disease entities such as cancer, dementia, or congestive heart failure. The decision to exclude specific diseases was intentional and prognostication-related as ACP approaches differ between older adults with clear terminal conditions (i.e., heart failure, cancer) and those who are on trajectories of frailty and facing the end of life with greater uncertainty. We were most interested in ACP uptake in cases of uncertainty. Seventy-seven studies were preliminarily included in the review, with one additional study added from a subsequent hand search of references.
Data Evaluation and Analysis
An integrative design and synthesis approach was used to evaluate studies in an inductive stepwise process, including 1) quality appraisal of studies using critical appraisal tools, 2) extraction of descriptive content and rating of evidence (levels) with the research hierarchy,16 3) analysis of applicable statistical results (effect sizes) of factors (variables) that influence ACP as a dependent variable, and 4) content analysis of results to identify categories, defined themes, and descriptors within studies. Our approach allowed for the study findings to move beyond a summary used in a narrative review to an approach used to generate new insights and understanding of ACP uptake in a broad, yet systematic, manner.17
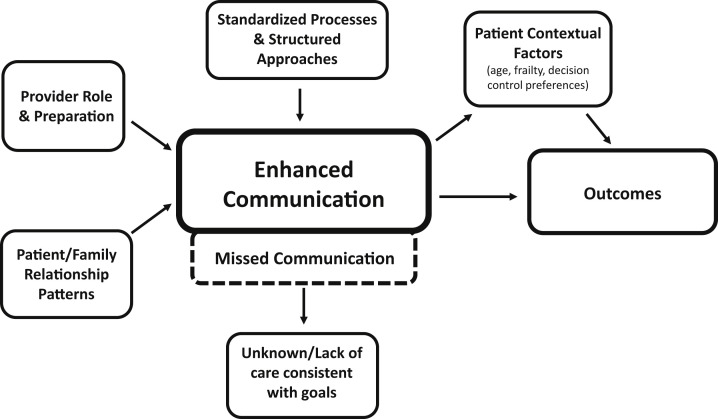
Quality appraisal of studies was conducted using Joanna Briggs Institute Critical Appraisal tools for analytical cross-sectional, quasi-experimental, randomized controlled trials (RCTs) and qualitative studies.18 Studies were examined to determine the extent to which each met appraisal criteria, noting limitations that might influence the accuracy of study findings (Appendix I). Data were reviewed by two independent researchers (E.F. and C.A.M.), and disagreements were resolved through discussion. In the second step, data were extracted from each study, and evidence tables were developed which included study objective(s), level of evidence, setting and location, sample and participant characteristics, study design and data collection methods, ACP uptake features/factors, and ACP uptake outcome (Appendix II). Results from studies comprising quantitative analyses from which effect sizes could be generated were categorized into key sets including 1) demographic variables, 2) psychosocial variables, 3) variables related to physical function/disability, and 4) other variables (i.e., targeted interventions, process facilitators). To extract categories and themes from studies, results sections of all studies containing a qualitative analysis were line-by-line coded for factors contributing, negatively or positively, to uptake of ACP. In the fourth step, categories were developed; themes from all 78 studies were defined and organized under each category, and descriptors from each study were placed in tables (Appendix III). From the tables of categories, themes and descriptors, an integrated conceptual model was developed (Figure 2 ) that provides a broad visual depiction of the major categories and relationships.15
Fig. 2.
Communication in advance care planning conceptual model.
Results
Summary of Descriptive Data and Evidence Levels
Seventy-eight studies (1996–2019) met inclusion criteria. The review included 23 qualitative, five mixed-methods and 50 quantitative studies (including 12 RCTs). Studies were conducted in 13 countries: United States n = 40, Canada n = 10, Australia n = 7, Hong Kong n = 3, Taiwan n = 1, United Kingdom n = 4, Norway n = 2, Germany n = 2, Belgium n = 3, South Korea n = 1, Japan n = 1, Sweden n = 1, and Netherlands n = 2. One study represented 11 countries as a whole, but results were not reported by country. Sample sizes for the 78 studies included qualitative (range: 719 to 50320), mixed-methods (range: 2121 to 28922), and quantitative (range: 1823-25,55024). The 12 RCT sample sizes ranged from 1425 to 2294.26 Details of age range, gender, and race/ethnicity of participants are shown in Appendix II.
Evidence Levels
Within the rating system for the hierarchy of evidence for treatment outcomes,27 , 28 12 studies were level II (well-designed RCTs); one study was level III (controlled trial without randomization); 37 studies were level IV (case control, cohort studies); and 28 studies were level VI (descriptive or qualitative).
Summary of Relevant Statistical Results
Statistical Results
A critical analysis and synthesis of methods, measurement tools, and statistical techniques to study the phenomenon was undertaken. For brevity, major findings are reported in this narrative with specific effect sizes in Table 1, Table 2, Table 3, Table 4 . Studies that were included specifically aligned with the ACP consensus definition, with ACP being the dependent outcome variable with the independent variables represented through domains of demographics, psychosocial, disability and functioning, and miscellaneous.
Table 1.
Effect Sizes for the Association of Demographic Characteristics With ACP
| Characteristic | Unadjusted O.R. | Adjusted O.R. | Study |
|---|---|---|---|
| Increasing age | |||
| Continuous | 1.31 | N/A | 29 |
| Continuous | AD: 0.90 POA: 0.88 |
N/A | 32a |
| Continuous | AD + Discussion: 2.22 Discussion only: 1.39 |
N/A | 30 |
| Continuous | 1.01 | N/A | 31 |
| Continuous | N/A | 1.1 | 37 |
| 18-64 vs. ≥85 | 1.76 | N/A | 33 |
| Gender, maleb vs. female | |||
| 0.93 | N/A | 29 | |
| AD + Discussion: 0.60 Discussion only: 1.14 |
N/A | 30 | |
| AD: 1.08 POA: 1.13 |
N/A | 32 | |
| 0.62 | N/A | 31 | |
| N/A | 0.77 | 34 | |
| 1.08 | N/A | 33 | |
| Race/ethnicity, whiteb | |||
| Ethnic/racial minorityb | AD + Discussion: 1.09 Discussion only: 0.37 |
N/A | 30 |
| African Americanb | N/A | 2.00 | 37 |
| Hispanicb | 1.00 | ||
| American Indian, Asianb | 1.40 | ||
| African Americanb | 1.29 | N/A | 38 |
| Marital status, not marriedb vs. married | |||
| 1.35 | N/A | 29 | |
| AD + Discussion: 1.84 Discussion only: 1.28 |
N/A | 30 | |
| AD: 1.07 POA: 1.13 |
N/A | 32 | |
| N/A | 1.00 | 37 | |
| Increasing education | |||
| <H.S.b vs. H.S. | N/A | 1.63 | 29 |
| <H.S.b vs. > H.S. | 3.90 | 2.40 | 29 |
| Continuous | AD + Discussion: 3.37 Discussion only: 1.72 |
N/A | 30 |
| Continuous | AD: 1.58 POA: 1.25 |
N/A | 32 |
| <Elementaryb vs. >H.S. | 0.80 | N/A | 33 |
| Place of residence | |||
| Institutionalb vs. private | AD: 0.66 POA: 0.53 |
N/A | 32 |
| Institutionalb vs. private | 0.54 | N/A | 29 |
ACP = Advance care planning; AD = advance directives.
To be included in this study, participants had to be older than 75 years.
The category (for categorical independent variables) that was the referent category in the analysis.
Table 2.
Effect Sizes for the Association of Psychosocial Characteristics With ACP
| Characteristic | Unadjusted O.R. | Adjusted O.R. | Study |
|---|---|---|---|
| Living situation and social support | |||
| Lives w/othersa vs. alone | 1.61 | N/A | 29b |
| Increasing social support | |||
| Someone to listen | 6.93 | N/A | 29 |
| Emotional support | 2.83 | N/A | 29 |
| Increased perceived health | |||
| Lowa vs. good | 1.01 | N/A | 29 |
| Lowa vs. excellent | 1.09 | N/A | 29 |
| Lowa vs. good/better | AD + Discussion: 1.90 Discussion only: 1.77 |
N/A | 30 |
| Continuous | AD: 0.90 POA: 1.06 |
N/A | 32 |
| Quality of life, unable to care for selfa | |||
| Some problems | N/A | 6.11 | 31 |
| No problems | 3.65 | ||
| Increased marital support | |||
| Continuous | AD + Discussion: 1.04 Discussion only: 1.72 |
N/A | 30 |
| Higher general family functioning | |||
| Continuous | AD + Discussion: 1.69 Discussion only: 1.99 |
N/A | 30 |
| Increasing number of children | |||
| Continuous | AD + Discussion: 0.58 Discussion only: 0.88 |
N/A | 30 |
| Increased support from children | |||
| Continuous | AD + Discussion: 1.10 Discussion only: 1.39 |
N/A | 30 |
| Increased religiosity/spirituality | |||
| Importance (continuous) | N/A | 1.32 | 35 |
| Influence medical (continuous) | 2.25 | 35 | |
| Decreased depressive symptoms | |||
| Higha vs. low | 2.31 | N/A | 29 |
| Continuousc | AD + Discussion: 1.40 Discussion only: 1.50 |
N/A | 30 |
| Higha vs. low | AD: 1.24 POA: 0.93 |
N/A | 32 |
| Precursors: personal preferences | |||
| Decision control preferences: lowa vs. high | Surrogate decision-maker: 0.93 Completed AD: 1.33 Made decision for self: 1.79 Made decision for others: 2.00 |
N/A | 36 |
| Wish to be informed of diagnosis of terminal disease, noa vs. yes | N/A | 9.19 | 31 |
ACP = advance care planning; AD = advance directives.
The category (for categorical independent variables) that was the referent category in the analysis.
Unique community-dwelling older adult (mean age 88 years) population.
Original OR = 0.72 and 0.69 indicating higher depression, less likelihood. These were inverted for consistency with the other ORs in this section (lower depression, increased likelihood).
Table 3.
Effect Sizes for the Association of Disability and Functioning With ACP
| Characteristic | Unadjusted O.R. | Adjusted O.R. | Study |
|---|---|---|---|
| Physical functioning, ADL/IADLa | |||
| ≥1 ADLa vs. None | 1.79 | N/A | 29 |
| Continuous, higher score, fewer ADLsa | AD: 0.91 POA: 1.09 |
N/A | 32 |
| Continuous, higher score, fewer IADLa | AD: 0.91 POA: 0.91 |
N/A | 32 |
| Physical functioning, ability to walk half a milea | |||
| Unablea vs. able | 1.88 | N/A | 29 |
| Physical functioning, use of assistive device to perform ADLa | |||
| Noa vs. yes | 0.76 | N/A | 29b |
| Noa vs. yes | AD + Discussion: 1.20 Discussion only: 1.26 |
N/A | 30 |
| Increasing frailty | |||
| Continuous | AD: 1.00 POA: 1.00 |
N/A | 32 |
| Cognitive functioning | |||
| Lowa vs. high | 1.57 | N/A | 29 |
| Self-report: memory worsea vs. same | AD: 1.02 POA: 0.94 |
N/A | 32 |
| MMSE, low - >higha | AD: 1.60 POA: 1.60 |
N/A | 32 |
| Comorbid illness | |||
| Nonea vs. 1 | 0.78 | N/A | 29 |
| Nonea vs. 2 | 0.89 | N/A | 29 |
| Nonea vs. 3 | 0.68 | N/A | 29 |
| Increasing number (continuous) | N/A | 1.30 | 37 |
| Nonea vs. >1 | N/A | 1.82 | 38 |
| Nonea vs. stroke | N/A | 0.33 | 33 |
| Use of health-care services | |||
| Nonea vs. ≥2 hospitalizations | 1.08 | N/A | 29 |
| Nonea vs. ≥2 outpatient visits | 1.16 | N/A | 29 |
| Noa vs. nursing home stay | 2.20 | N/A | 29 |
| Continuous (# inpatient services) | N/A | 0.80 | 37 |
| Continuous (# outpatient services) | N/A | 1.80 | 37 |
ACP = advance care planning; AD = advance directives; MMSE = Mini-Mental State Examination.
The category (for categorical independent variables) that was the referent category in the analysis.
Unique community-dwelling older adult (mean 88 years old) population.
Table 4.
Effect Sizes From Implementation and Clinical Trial studies Investigating Document and Process Facilitators Effect on ACP
| Characteristic | Unadjusted O.R. | Adjusted O.R. | Study |
|---|---|---|---|
| Facilitation of document completion | |||
| Controla vs. intervention | 3.20 | N/A | 26 |
| Controla vs. Intervention | 2.17 | N/A | 39 |
| Controla vs. Intervention | 23.27 | N/A | 40 |
| Facilitation of process | |||
| Single group, prea vs. post | 22.00 | N/A | 41 |
| Controla vs. intervention | 3.82 | 4.52 | 43 |
| Controla vs. intervention | 2.61 | N/A | 42 |
| Controla vs. intervention | Documentation: 17.14 Discussions: 5.60 |
N/A | 44 |
The category (for categorical independent variables) that was the referent category in the analysis.
Demographics
Demographic variables analyzed for their effects on ACP included age, gender, race/ethnicity, marital status, education, and place of residence. Most studies reported that the likelihood of engaging in ACP increased with increasing age (ORs = 1.01 to 2.22).29, 30, 31 Gender demonstrated generally mixed effects (ORs = 0.60 to 1.14)29, 30, 31, 32, 33, 34; however, being married increased likelihood of ACP as compared to not being married (OR = 1.07 to 1.84).29 , 30 , 32 Higher levels of education were most commonly associated with increased likelihood of ACP (OR = 1.25 to 3.90),29 , 30 , 32 and one study reported the effect after adjusting for other demographic variables (OR = 1.63 and 2.40).29 Living in a private setting, compared to an institutional setting, dramatically reduced the likelihood of ACP (OR = 0.53 to 0.66)32 (Table 1).
Psychosocial
Results from studies of psychosocial variable effects on ACP uptake are summarized in Table 2. Those variables have included living situation, social support, perceived health, quality of life, nature of marital relationship, general family functioning, number of children, relationship with children, religiosity/spirituality, presence of depressive symptoms, and personal preferences. Social support, described as having someone to listen and provide emotional support, was associated with increased likelihood of ACP (someone to listen, OR = 6.93; someone to provide emotional support, OR = 2.83).30 If grouped into categories (good/better/excellent vs. poor), the likelihood of ACP generally was reported to increase with better perceptions of health (OR = 1.01 to 1.90).29 , 30 Higher family functioning, or the degree to which families function as a unit, was associated with increased likelihood of ACP (OR = 1.69 and OR = 1.99),30 as was increased emotional support from adult children (OR = 1.10, 1.39),30 yet the likelihood of ACP tended to decrease as the number of children increased (OR = 0.58, 0.88).30 Other psychosocial variables including religiosity/spirituality were associated with increased likelihood of ACP even when adjusted for religious affiliation, degree of religiosity or spirituality, beliefs, values, sociodemographic, and health status (ORs = 1.32, 2.25).35 Decreased or absent depressive symptoms were consistently associated with increased likelihood of ACP (OR = 1.24 to 2.31).29 , 30 , 32 A couple of studies looked at the effects of personal preferences as precursor variables (decision control preferences36 and wish to be informed of diagnosis of terminal disease31) on the likelihood of ACP. Generally, higher decision control preferences increased the likelihood of ACP (OR = 0.93 to 2.00),36 while the wish to be informed increased the likelihood after adjusting for age and gender (OR = 9.19)31 (Table 2).
Disability and Functioning
Disability and functioning variables included physical functioning, frailty, cognitive functioning, comorbidity, stroke, and the use of health-care services. As shown in Table 3, associations of physical functioning with ACP were mixed, yet most studies reported an increased likelihood of ACP with better functioning (OR = 1.79, 1.88,29 OR = 1.20–1.2630).
Increased cognitive functioning (higher Mini-Mental State Examination scores) was generally associated with increased likelihood of ACP (OR = 1.57;29 OR = 1.6032). After adjusting for age, sociodemographics, and other pertinent variables, studies generally found that the likelihood of ACP increased with increasing comorbidities (OR = 1.30, 1.82)37 , 38 (Table 3).
Other Variables
Several studies, as shown in Table 4, investigated the effect of specific programs/variables on engagement in ACP using implementation and clinical trial designs. Generally targeted interventions increased engagement outcomes (multifaceted, OR = 2.17;39 electronic motivational prompts, OR = 3.20;26 defined ACP program [Respecting Choices], OR = 23.2740), as did those that focused on process facilitators (decision aids, OR = 22.0,41 OR = 2.61;42 standardized templates, OR = 3.82;43 and online ACP program [PREPARE], OR = 17.14 [documentation], OR = 5.6 [discussions])44 (Table 4).
Thematic Analysis
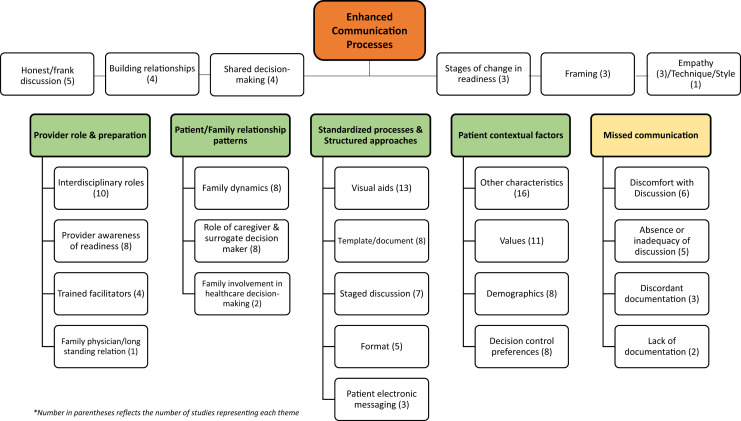
Line-by-line coding of factors associated with uptake of ACP was conducted by two investigators (E.F. and C.A.M.). Codes were organized to allow for translation of concepts/ideas from one study to another and for grouping of codes into categories, themes, and descriptors. Figure 3 provides an overview of the categories and themes derived from this process. A detailed breakdown of the process with groupings is reported in Appendix III. The analysis includes 27 thematic tables with studies (author/year) and descriptors related to the theme. From this process of analysis, we developed a conceptual model (Figure 2) that provides a high-level overview of our results. The following section presents our findings based on the conceptual model with a focus on the categories and themes represented under each category.
Fig. 3.
Categories and themes diagram.
Enhanced Communication Processes
The category of enhanced communication processes emerged as the central requisite addressed in some way in every study for successful ACP and improved outcomes. The term “enhanced” conveys the necessity of additional factors/traits required to move beyond the status quo.45 These requirements are represented by themes of honest/frank discussion,20 , 46, 47, 48, 49 building personal relationships,20 , 50, 51, 52 shared decision-making,30 , 47 , 53 , 54 stages of change in terms of readiness,20 , 55 , 56 framing,43 , 57, 58, 59 empathy,20 , 49 , 60 and technique/style.21
Five studies20 , 46, 47, 48, 49 reported the importance of honest/frank discussion in ACP with a focus on the delivery of truthful information. The concept of “conditional candour” in one study described a preference for frank information while also assessing readiness,48 and another highlighted the necessity for physicians to communicate through an honest and straightforward approach while continuing to be attentive to patients' informational and emotional needs.49 Another theme to emerge was that of building relationship and forming a connection or bond between two or more parties.20 , 50, 51, 52 The importance of building a relationship extended to both patients and surrogate decision-makers, highlighting engagement in ACP as a dyadic activity,52 with the surrogate being the one who knew the older adult best and would ensure their treatment was in accordance with values.51 The importance of being “known” by a provider was noted as critical to the ease of ACP discussions and honoring preferences.50
Shared decision-making is reported as a way to support and maintain individual patient autonomy while requiring skilled providers to seek permission and respect patient communication and patient engagement.30 , 47 , 53 , 54 Another approach focused on the assessment of readiness for change in participants as a factor for modifying/adapting individual approaches.20 , 55 , 56 Recognition of ACP as specific behaviors in which individuals progress through stages of change or readiness has been explored by Fried et al. and grounded in the Transtheoretical Model of behavior change.61
Provider Role and Preparation
The role of the provider in approaching conversations with patients about the end of life is key, as is recognition that conversations are often emotionally charged and require preparation. Health-care providers have a responsibility to assist in the decision-making process through education about ACP and communication skills that impart compassion and empathy.45 The specific roles and necessary preparation of health-care providers is critical for the uptake of ACP and the timing of ACP to occur within a framework that emphasizes responsiveness to patient and family emotions, while also focusing on overall goals of a patient's care.45 The category of provider role and preparation is supported by four themes, including interdisciplinary roles,23 , 33 , 39 , 43 , 59 , 62, 63, 64, 65, 66 provider awareness of readiness,19 , 22 , 36 , 46 , 48 , 65, 66, 67 trained facilitators,23 , 33 , 40 , 57 and a long-standing relation with a family physician.22 Ten studies reported the use of interdisciplinary team members as part of a study protocol to deliver ACP education, assess ACP knowledge, lead ACP meetings, and complete care planning documents.23 , 33 , 39 , 43 , 59 , 62, 63, 64, 65, 66 Four studies used a social worker to conduct ACP during home visits or an office visit before the scheduled provider visit,23 , 39 , 62 , 63 noting that the social workers' professional role of counseling and facilitative communication is a natural fit for ACP. Nurses' role in ACP is represented in five studies23 , 43 , 59 , 64 , 65 through a nurse facilitator to guide participants toward sharing and expressing their EOL wishes43 to a nurse-led interactive educational workshop64 and advance practice registered nurses' leading conversations following a Respecting Choices model.23
The theme of provider awareness of readiness was represented with 8 studies19 , 22 , 36 , 46 , 48 , 65, 66, 67 reporting the need for providers to understand patients/families' desire or lack of desire to engage in a conversation about EOL. The concept of readiness was further demonstrated in these studies through 1) patients' readiness to ask questions to doctors and participate in question-asking behaviors,36 2) increasing readiness to discuss EOL issues,46 3) timing of readiness when one is cognitively intact and has the ability to communicate wishes,65 and 4) the readiness to invite family to be part of the conversations as they know the patient's life story.19 The importance of sharing information when people are mentally prepared to receive it was stressed as otherwise it may be detrimental to a patient's emotional welfare or the patient-physician relationship.48
Patient/Family Relationship Patterns
The category of patient/family relationship patterns is supported by three themes of family dynamics,19 , 29 , 30 , 52 , 57 , 58 , 68 , 69 family involvement in health-care decision-making,38 , 70 and the role of caregiver and surrogate decision-maker.25 , 52 , 71, 72, 73, 74, 75 , 76 Eight studies highlighted the importance of understanding patterns of how patients and family members relate to one another.19 , 29 , 30 , 52 , 57 , 58 , 68 , 69 These studies characterized how family relations influence ACP through emotionally supportive or critical relationships.30 Family member involvement in care plan meetings where they were “moral witnesses to a key transition in the patient's life course”68 was invaluable to understanding how long-lasting family dynamics and relationship patterns held true in ACP.69 The participation of family in discussions was also noted to be a crucial factor, emphasizing the importance of including family whenever possible29 , 57 and recognizing the perception of patients and relatives as an “intertwined unit.”19
Standardized Processes and Structured Approaches
The category of standardized processes and structured approaches to ACP included the following themes: the use of visual aids,25 , 39 , 41, 42, 43, 44 , 49 , 55 , 62 , 64 , 77, 78, 79 template/document for ACP,23 , 80, 81, 82, 83, 84, 85, 86 staged discussion,20 , 24 , 58 , 60 , 62 , 87 , 88 format of ACP discussion,60 , 64 , 78 , 89 , 90 and patient electronic messaging.26 , 91 , 92 Standardized and structured approaches build in or incorporate defined processes for older adults to receive ACP materials (information and documents) and allot time to enhance their understanding. These approaches also make the point of the need for documentation of discussions by health-care providers.
Patients make increasingly complex decisions about their medical care in ACP, underscoring the need for decision aids or additional information to increase understanding. Research has led to the development of aids that facilitate health-care decision-making by patients and families and improve the way physicians or providers present information.93 Five studies reported the use of an ACP workbook or booklet that was personalized to reflect life stories, patient views, and preferences.39 , 43 , 49 , 62 , 64 Four studies used a video decision aid which allows for a visual representation medium that engages patients in a way that verbal descriptions, whether written or oral, do not.25 , 41 , 42 , 78 Other visual aids include ACP through pictures, story boards, and media extracts,79 a “Go Wish” card game,77 an individualized feedback report,55 and a patient-facing interactive online ACP program.44
Patient Contextual Influences
Prior work has shown that in addition to structural constraints of health-care and legal systems, contextual factors that influence the uptake of ACP are complex and multifaceted and span the social and cultural beliefs of patients, families, and health professionals.94 Contextualization acknowledges that other factors that influence uptake of ACP exist for every person. This review encompassed a variety of other factors29 , 30 , 35 , 95, 96, 97 including frailty,40 , 73 , 98 culturally sensitive care,38 , 43 , 44 , 64 , 80 attitudinal differences,32 , 54 one's own values,77 , 99 , 100 demographic characteristics,29, 30, 31, 32, 33, 34 , 37 , 38 and decision control preferences.20 , 36 , 47 , 53 , 54 , 67 , 72 , 88 The condition of frailty was represented in three studies40 , 73 , 98 using validated instruments to assess patients' degree of frailty. The trajectory of frailty can occur over months or years but ultimately predicts poor outcomes that lead to eventual death. Frailty is an important consideration as many older adults will experience frailty or progressive dwindling, may be more likely to become dependent, have frequent hospitalization readmissions, and may benefit from discussions about care wishes through ACP.101 Consideration of culture-related preferences was represented through five studies that were specifically culturally sensitive in their ACP approach, including 1) involvement from diverse backgrounds to help create advance directive documentation,80 2) consideration of influence of race/ethnicity in EOL care discussions,38 3) creation of a culturally appropriate ACP program in both English and Spanish,44 and 4) culturally sensitive ACP education.43 , 64 The influence of life values as a basis for ACP discussion and treatment preferences was explored in 11 studies. Studies reported that using life values as part of an advance directive may help to elucidate patients' desired medical care and guide physicians and proxies toward optimal representation of stated values.99 Six major personal life values included religiosity/spirituality,20 , 35 , 51 , 72 control,51 , 54 , 60 dignity,48 , 51 , 72 , 100 autonomy,51 , 72 comfort,72 , 79 , 100 and burden.79 , 100
Missed Communication
A sixth and final category centered on missed opportunities for ACP, reflected through themes of discomfort with discussion,20 , 54 , 58 , 65 , 75 , 86 absence or inadequacy of discussion,20 , 22 , 53 , 102 , 103 lack of documentation,37 , 102 and discordant documentation.65 , 98 , 102 An uncomfortable stage for ACP was discussed in six studies, describing patients' fears concerning death and dying,54 varying degrees of reticence, evasion, or reluctance to engage in conversations,86 the emotional burdens and responses associated with reflecting on death,20 , 58 and health-care providers' concern for causing maleficence to the patient.65 Caregiver discomfort with EOL topics was reflected in a desire to preserve normalcy.75 Five studies discussed the absence or inadequate nature of discussion, with two taking place in nursing homes, noting that very few nursing home patients and relatives had participated in conversations with nursing home staff about preferences and wishes regarding EOL care.53 , 103 The theme of discordant documentation was reported in three studies emphasizing incongruencies between written and verbal information that may lead to erroneous information entered into the electronic medical record. Discrepancies can lead to safety and quality concerns,98 and variance in documentation systems between care settings may hinder teamwork and jeopardize the medical safety of the patients if access of information is limited.65
Outcomes
Before 2018, the field of ACP research lacked a consensus about patient-centered outcome domains and constructs that defined successful ACP.104 The Delphi panel that created the consensus definition of ACP comprised a multidisciplinary panel of ACP experts to identify and rate patient-centered ACP outcomes that best define successful ACP.104 An Organizing Framework of ACP outcomes was created with four outcomes domains: 1) process, 2) action, 3) quality of care, and 4) health-care outcomes.104 Consistent with this framework, ACP outcomes in each of the reviewed studies were categorized under these domains ranging from process (e.g., increased comprehension of disease state) and action outcomes (e.g., completion of documents) to quality of care (e.g., family satisfaction) and health-care outcomes (e.g., decreased anxiety and depression). All the outcomes represent “uptake” or “absorbing and incorporating” ACP. A detailed description of ACP outcomes from our review is reported in Appendix II.
Discussion
From this integrative review, we determined the category of enhanced communication processes to be a vital necessity for successful ACP in older adults. While seemingly intuitive, this central category demonstrates that ACP does not occur without specific intention or conscious awareness on the part of health-care providers, organizations, and other stakeholders who recognize the need for ACP. This highlights opportunities for settings across the continuum to develop and integrate these processes based on available resources that are specific to the subpopulation of older adults at specific locations. For example, a faith community (church) of ethnically diverse older adults might integrate group discussions with a trained leader into regularly scheduled gatherings. Inversely, while enhanced communication may contribute to ACP, we also conclude that successful ACP reflects that an enhanced communication process has occurred.
This review reflects a broad and comprehensive appraisal of research that explored the uptake of ACP among older adults. Broadly, our findings portray optimal uptake of ACP as most likely to occur in older married adults with higher education and cognitive function, little to no mental health problems, strong social and family support, and who are able to receive structured enhanced communication approaches from prepared and qualified providers/clinicians. Regrettably, only a small segment of society fits this description or is fortuitous to receive the optimal approaches addressed in this review. In addition, subpopulations of older adults (minorities, economically disadvantaged) may respond differently to structured approaches. Our findings highlight opportunities for future research and clinical practice.
Future Research
Population aging and longer lifespans that lead to frailty and eventual EOL call for health-care systems that are proactive or that anticipate eventualities that will confront almost every person who reaches advanced age. The World Health Organization (WHO) stressed the need for a conceptual shift from reactive disease-based models to proactive health-based models that emphasize intrinsic capacity (composite of a person's physical and mental capacities) throughout the life course.105 Equipping older adults with increased understanding about intrinsic capacity related to aging that changes their awareness regarding the need to prepare and plan is an unexplored area for research. Such interventions might lead to improved uptake of ACP because individuals are better able to contemplate their aging, eventual decline and end of life, leading to a greater desire for control of their personal trajectory of aging and end of life. From this perspective, ACP might occur more upstream and in ways that normalize the process. Within health-care systems, innovative approaches are needed to proactively address the needs of prefrail and frail older adults and their families, including information needs and symptom management specific to age-related problems (e.g., loss of appetite, fatigue, pain, incontinence). Development of models of care that are patient-centered, holistic, and that recognize the unique legacy of older individuals is an area for innovation. Frailty-ready health-care systems are also needed to reduce older adult admissions requiring crisis care (e.g., falls) that lead to rapid decline and death.106
In contrast to the optimal scenario portrayed from our results, racially and economically disadvantaged older adults experience poorer health and more chronic conditions, depressive symptoms, shorter lifespans, and greater long-term care needs. Forty percent of older adults live at or near poverty levels, comprising a population that stands to benefit from cost-effective interventions that target disparities. Research has consistently reported low uptake of ACP among ethnic/racial minorities.107 , 108 Recent studies109 , 110 indicate that older ethnic/racial minorities are more likely to engage in ACP through informal dialogue than through the structured approaches presented in our review. Development of interventions that incorporate informal discussions about aging, frailty, and the need for ACP in natural settings (community centers, churches, assisted living) is an area for future research.
Clinical Practice
This integrative review holds implications for clinical practice by all members of the interdisciplinary health-care team. Recognition of the holistic elements that encompass ACP is the first step toward successful efforts to promote the uptake of ACP in older adults. For example, a clinician working in an outpatient setting may encounter an older patient with advanced frailty who may be more receptive to engage in ACP as they may be witnessing their body's transition. A clinician working in an inpatient setting about to conduct a family meeting in the intensive care unit may recognize the patient and family relationship patterns' affect decision-making related to the patient's personal values, goals, and preferences dealing with current critical illness. And a health-care worker in the skilled nursing facility may recognize the missed opportunity for communication with patients and families about care wishes, which resulted in an unnecessary transfer to the hospital given unknown care desires. It is also important to note that this integrative review specifically addresses ACP for older adults that may have chronic or serious illnesses along an aging trajectory. Specifically, ACP in older adults related to the acute pandemic of COVID-19 may require a different set of ACP skills and nuanced approaches.
Strengths and Limitations
A strength of this review is the broad and expansive nature that illuminates the older adults who are more likely to engage in ACP but also those who are less likely to engage via the structures and processes that traditionally facilitate ACP. Our conceptual model places “enhanced communication processes” as central to any ACP endeavor and calls for both public health and other care settings to be more proactive toward embedding approaches and processes that facilitate upstream planning for aging/frailty and ACP.
We also identified limitations within our review. The Joanna Briggs quality appraisal criteria recommend reporting of researchers' influence on the conducted research and vice versa. Few, if any of the studies that we reviewed reported such influence. Although old age is associated with accumulation of chronic conditions and multimorbidity, we did not include these terms in our search. Inclusion might have contributed to a richer understanding of ACP uptake related to aging. Several studies addressed the need for agreement about treatment preferences between patients and surrogates and patient-provider dyads. This may be reflected in the increased trust an older adult has in their family members and health-care providers carrying out their wishes. This is an area of future research highlighting age-group generational differences. Measurement of “care consistent with goals” is challenging as there is no standardized, valid, or reliable method to measure this outcome especially with a seriously ill population in which preferences may change over time.111 Finally, a major limitation revolves around the inconsistency of how ACP is depicted and explained in the research, as this was quite evident in the statistical and thematic reviews. Further recommendations involve using the ACP consensus definition as well as ACP outcome domains.
Conclusions
This integrative review advances understanding about the complexities involved in ACP uptake among older adults and provides a framework for evaluation of future efforts. ACP has evolved over the years to be more inclusive of the process involved rather than tasks of document completion. Future research in the field of ACP related to aging is needed across health-care disciplines, public domains (i.e., legal experts), governmental and policy officials, and the general public. Such efforts are essential to expanding the field and the underlying mission of advancing approaches to serious illness, aging, and frailty.
Disclosures and Acknowledgments
This research received no specific funding/grant from any funding agency in the public, commercial, or not-for-profit sectors. The authors declare no conflicts of interest.
Appendix I. Critical appraisal of studies
Appendix Table 1.
Critical Appraisal Qualitative Mixed Methods
| Author (Year) | Congruity Between the Stated Philosophical Perspective and the Research Methodology? | Congruity Between the Research Methodology and the Research Question or Objectives? | Congruity Between the Research Methodology and the Methods Used to Collect Data? | Congruity Between the Research Methodology and the Representation and Analysis of Data? | Congruity Between the Research Methodology and the Interpretation of Results? | Statement Locating the Researcher Culturally or Theoretically? | Is Influence of the Researcher on the Research, and Vice-Versa, Addressed? | Are Participants, and Their Voices, Adequately Represented? | Is the Research Ethical According to Current Criteria or, for Recent Studies? and Is There Evidence of Ethical Approval by an Appropriate Body? | Do the Conclusions Drawn in the Research Report Flow from the Analysis, or Interpretation, of the Data? |
|---|---|---|---|---|---|---|---|---|---|---|
| Romo (2017)47 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Braun (2014)67 | Y | Y | Y | Y | Y | Y | N | Y | Y, Y | Y |
| Almack (2012)86 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Abdul-Razzak (2014)48 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Barnes (2007)60 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Gjerberg (2015)53 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y | Y |
| Karasz (2010)68 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y | Y |
| Malcomson (2009)50 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Seymour (2003)79 | Y | Y | Y | Y | Y | UKN | UKN | Y | Y, Y | Y |
| Piers (2013)54 | Y | Y | Y | Y | Y | Y | N | Y | Y, Y | Y |
| Pollak (2015)21 | Y | Y | Y | Y | Y | N | Y | Y | Y, Y | Y |
| Fried (2017)57 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| van Eechoud (2014)69 | Y | Y | Y | Y | Y | Y | N | Y | Y, Y | Y |
| Towsley (2015)103 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y | Y |
| Cheang (2014)66 | Y | Y | Y | Y | Y | N | UKN | Y | Y, Y | Y |
| Lum (2016)90 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Vandrevala (2002)51 | Y | Y | Y | Y | Y | Y | UKN | Y | Y, Y | Y |
| Thoresen (2016)19 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y | Y |
| Michael (2017)58 | Y | Y | Y | Y | Y | Y | UKN | Y | Y, Y | Y |
| Simon (2015)20 | Y | Y | Y | Y | Y | Y | UKN | Y | Y, Y | Y |
| Peck (2018)49 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y | Y |
| Taneja (2019)88 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y | Y |
| Shaw (2018)56 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y | Y |
| Schubart (2018)75 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Groebe (2019)59 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Kastbom (2019)65 | Y | Y | Y | Y | Y | N | N | Y | Y, Y | Y |
| Overbeek (2018)40 | Y | Y | Y | Y | Y | Y | N | Y | Y, Y | Y |
| De Vleminck (2018)22 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y | Y |
Y = yes; N = no.
Appendix Table 2.
Critical Appraisal Randomized Controlled Trials
| Author (Year) | Was True Randomization Used for Assignment of Participants to Treatment Groups? | Was Allocation to Treatment Groups Concealed? | Were Treatment Groups Similar at the Baseline? | Were Participants Blind to Treatment Assignment? | Were Those Delivering Treatment Blind to Treatment Assignment? | Were Outcomes Assessors Blind to Treatment Assignment? | Were Treatment Groups Treated Identically Other Than the Intervention of Interest? | Was Follow-up Complete? and if not, Were Differences Between Groups in Terms of Their Follow-up Adequately Described and Analyzed? | Were Participants Analyzed in the Groups to Which They Were Randomized? | Were Outcomes Measured in the Same Way for Treatment Groups? | Were Outcomes Measured in a Reliable Way? | Was Appropriate Statistical Analysis Used? | Was the Trial Design Appropriate, and any Deviations From the Standard RCT Design (Individual Randomization, Parallel Groups) Accounted for in the Conduct and Analysis of the Trial? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Volandes (2009)25 | Y | Y | Y | UKN | N | N | Y | Y | Y | Y | Y | Y | Y |
| Pearlman (2005)39 | N | N | Y | Y | N | UKN | Y | Y | Y | Y | Y | Y | Y |
| Detering (2010)57 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Bravo (2016)62 | N | N | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Tieu (2017)26 | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y |
| Periyakoil (2017)80 | Y | Y | Y | Y | Y | Y | Y | NA | Y | Y | Y | Y | Y |
| Overbeek (2018)40 | Y | N | Y | UKN | N | N | Y | Y | Y | Y | Y | Y | Y |
| Sudore (2018)44 | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Paiva (2019)55 | UKN | UKN | N | UKN | UKN | UKN | Y | Y | UKN | Y | Y | Y | Y |
| Bose-Brill (2018)91 | N | N | Y | UKN | N | N | Y | Y | Y | Y | Y | Y | Y |
| Bravo (2018)71 | N | N | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Lum (2018)96 | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y |
Y = yes; UKN = unknown; N = no.
Appendix Table 3.
Critical Appraisal Analytical Cross Sectional
| Author (Year) | Were the Criteria for Inclusion in the Sample Clearly Defined? | Were the Study Subjects and the Setting Described in Detail? | Was the Exposure Measured in a Valid and Reliable Way? | Were Objective, Standard Criteria Used for Measurement of the Condition? | Were Confounding Factors Identified? | Were Strategies to Deal with Confounding Factors Stated? | Were the Outcomes Measured in a Valid and Reliable Way? | Was Appropriate Statistical Analysis Used? |
|---|---|---|---|---|---|---|---|---|
| Brimblecombe (2014)81 | Y | Y | Y | Y | Y | Y | Y | Y |
| Chiu (2016)36 | Y | Y | Y | Y | Y | Y | Y | Y |
| Wu (2008)37 | Y | Y | Y | Y | Y | Y | Y | Y |
| Volandes (2016)41 | Y | Y | Y | Y | Y | Y | Y | Y |
| Silvester (2013)82 | Y | Y | Y | Y | Y | Y | Y | Y |
| Lankarani-Fard (2010)77 | Y | Y | Y | Y | Y | Y | Y | Y |
| McCarthy (2008)29 | Y | Y | Y | Y | Y | Y | Y | Y |
| Ratner (2001)63 | Y | Y | Y | Y | Y | Y | Y | Y |
| Luck (2017)32 | Y | Y | Y | Y | Y | Y | Y | Y |
| Boerner (2013)30 | Y | Y | Y | Y | Y | Y | Y | Y |
| Chu (2011)31 | Y | Y | Y | Y | Y | Y | Y | Y |
| Hawkins (2005)72 | Y | Y | Y | Y | Y | Y | Y | Y |
| Chung (2017)34 | Y | Y | Y | Y | Y | Y | Y | Y |
| Winter (2013)100 | Y | Y | Y | Y | Y | Y | Y | Y |
| Heyland (2013)102 | Y | Y | Y | Y | Y | Y | Y | Y |
| Garrido (2013)35 | Y | Y | Y | Y | Y | Y | Y | Y |
| Schonwetter (1996)99 | Y | Y | Y | Y | Y | Y | Y | Y |
| Tzeng (2019)95 | Y | Y | Y | Y | Y | Y | Y | Y |
| Nair (2019)42 | Y | Y | Y | Y | Y | Y | Y | Y |
| Dignam (2019)85 | Y | Y | Y | Y | Y | Y | Y | Y |
| Hinderer (2019)64 | Y | Y | Y | Y | Y | Y | Y | Y |
| Kim (2019)89 | Y | Y | Y | Y | Y | Y | Y | Y |
| Peterson (2019)38 | Y | Y | Y | Y | Y | Y | Y | Y |
| Cardona (2019)46 | Y | Y | Y | Y | Y | Y | Y | Y |
| Chu (2018)33 | Y | Y | Y | Y | Y | Y | Y | Y |
| Shaku (2019)76 | Y | Y | Y | Y | Y | Y | Y | Y |
| Zapata (2018)78 | Y | Y | Y | Y | Y | Y | Y | Y |
| Sable-Smith (2018)24 | Y | Y | Y | Y | Y | Y | Y | Y |
| DePriest (2019)84 | Y | N | Y | Y | Y | Y | Y | Y |
| David (2018)97 | Y | Y | Y | Y | Y | Y | Y | Y |
| Abdul-Razzak (2019)73 | Y | Y | Y | Y | Y | Y | Y | Y |
| Hold (2019)83 | Y | Y | Y | Y | Y | Y | Y | Y |
| Mirarchi (2019)98 | Y | Y | Y | Y | Y | Y | Y | Y |
| Brungardt (2019)92 | Y | Y | Y | Y | Y | Y | Y | Y |
| Hunter (2018)74 | Y | Y | Y | Y | Y | Y | Y | Y |
| Torke (2019)23 | Y | Y | Y | Y | Y | Y | Y | Y |
| Tan (2019)87 | Y | Y | Y | Y | Y | Y | Y | Y |
Y = yes; N = no.
Appendix Table 4.
Critical Appraisal Quasi-Experimental (Nonrandomized Experimental Studies)
| Author (Year) | Is It Clear in the Study What Is the “Cause” and What Is the “Effect”? | Were the Participants Included in Any Comparisons Similar? | Were the Participants Included in Any Comparisons Receiving Similar Treatment/Care, Other than the Exposure or Intervention of Interest? | Was There a Control Group? | Were There Multiple Measurements of the Outcomes Both Before and After the Intervention/Exposure? | Was Follow-up Complete? And if Not, Were Differences Between Groups in Terms of Their Follow-up Adequately Described and Analyzed? | Were the Outcomes of Participants Included in Any Comparisons Measured in the Same Way? | Were Outcomes Measured in a Reliable Way? | Was Appropriate Statistical Analysis Used? |
|---|---|---|---|---|---|---|---|---|---|
| Chan (2010)43 | Y | Y | Y | Y | Y | Y | Y | Y | Y, Y |
Y = yes.
Appendix II. Data Extraction Table for Uptake of Advance Care Planning (ACP) in Older Adults (78 Studies)
| References; Evidence Level | Study Objective | Setting and Location | Sample and Participant Characteristic | Design and Data Collection | ACP Uptake Feature or Factor | ACP Uptake Outcome |
|---|---|---|---|---|---|---|
| Romo (2017)47 Level 6 |
To explore how older adults in the community with a limited life expectancy make healthcare decisions and the processes used when they are not in an acute crisis | Outpatient; Medical programs and geriatrics clinics at the UCSF and San Francisco VAMC | n = 20; median 89, age range 67–98; male 65%, female 35% | Qualitative; semi-structured interviews conducted in participants' homes. | Interview guide developed to elicit participants' experience with decision-making and explore the underlying processes | Four themes emerged from the analysis that reflect the various approaches participants used to articulate their goals and maintain a sense of control: 1) direction communication, 2) third-party analogies, 3) adaptive denial, and 4) engaged avoidance. Importance of shared decision-making with provider-patient communication. Older adults allowed option of taking a more passive approach while still maintaining sense of control and personal autonomy |
| Luck (2017)32 Level 4 |
To examine the dissemination of advance directives (AD) specifically in the oldest-old individuals | Outpatient; General practice patients part of AgeQualiDe study; Participants recruited with six study centers in Germany | n = 704; Mean age 88.7 years; 472 (67.0%) women and 232 (33.0%) men. Not reported: age range, ethnicity | Quantitative; Observational, cross-sectional study. Home assessment | Interview: (i) frequency of ADs for health care, (ii) associated factors, (iii) groups of persons assisting in preparation of ADs, (iv) reasons for not having ADs in the very old, (v) information on frequency of POAs, (vi) associated factors, (vii) the groups of persons empowered. | Most frequently stated reason for not having ADs for health care was that the respondents trust their relatives or physicians to make right decisions for them when necessary (staged by 59.4% and 44.8% of those without ADs). Attitudinal reasons such as not wanting to concern themselves with the topic of ADs (28.1%) or have too many concerns regarding the usefulness of ADs (16.7%). When planning programs to offer ACP to oldest old, consider attitudinal differences of this target group, some simple trust their relatives/physicians in making the right decisions for them, and some may need more explanation and support for drawing up an advance care document |
| Brimblecombe (2014)81 Level 4 |
To review implementation of a Goals of Patient Care (GOPC) summary in medical inpatients and its applicability in emergency medical response (EMR) situations | Inpatient; general hospital in Mebourne, Australia | n = 101; mean age 72; age range 69–75; female n = 55; 36.6% non-English speaking; 71 patients admitted under general medicine. Targeted those likely to have issues of frailty and comorbidity that would impact treatment decisions. Not reported: ethnicity | Quantitative; Single center cross-sectional study | GOPC: presence and content. Secondary review of decision-making and discussion documentation, patient characteristics; EMR precipitants and outcomes | 80/82 patients with GOPC summary had life-prolonging treatment goals. Three months after introduction of the GOPC summary, formal consideration and documentation of overall aims occurred for 4/5 medical inpatients, with 85% of summaries completed within the first 48h of admission. Doctors may still have difficulties relating their medical judgement about prognosis and outcomes to a shared understanding of the individual's aims and do not consistently document discussion or details of decision-making |
| Chan (2010)43 Level 3 |
To develop an ACP program and determine its feasibility among Chinese frail nursing home residents. | Long term care; 4 residential nursing care homes in Hong Kong | n = 121; mean age 83.5 years, age range 66–100; female 69% | Quantitative; quasi-experimental with an intervention and comparison group; 1-year study. Each participating nursing home had one intervention and one comparison group. Participants divided according to the story their lived on. | Let me talk ACP program designed to encourage participants to talk about their deepest concerns with a nurse facilitator guiding the participants to share their stories and express their end-of-life care wishes. A personal booklet summarizing participants' life stories and views and documenting their health care concerns, life-sustaining treatment preferences and preferred decision-maker was prepared for each participant by end of program. After completion of program, participant's family members were invited to a family conference for addressing the participant's concerns and end-of-life care preferences. The facilitator acted as a mediator to facilitate communication between the participant and family or caregivers | Participants in intervention group were able to indicate their treatment preferences. Many nursing home residents were prepared to discussion death and dying issues that are considered taboo topics in Chinese culture. Program effective in enhancing the preference stability in the intervention group. One possible explanation is that the story-telling approach encouraged the participants to review past experiences and thus explore their deeply held personal values and beliefs which enabled them to ascertain their life goals and clarify their preferences. The mitigation of existential distress noted in this study may partly relate to the life storytelling process, which allowed older people to visualize their life as a whole and once again be conscious of its meaning. |
| Volandes (2009)25 Level 2 |
To compare the concordance of preferences among elderly patients and their surrogates listening to only a verbal description of advanced dementia or viewing a video decision support tool of the disease after hearing the verbal description | Outpatient; Community dwelling elderly and their surrogates conducted at 2 geriatric clinics affiliated with 2 academic medical centers in Boston | n = 14 pairs of patients and their surrogates; n = 6 verbal narrative, n = 8 video after verbal narrative. Elderly persons n = 14, mean age 83, female 50%, white n = 14. Surrogates n = 14, mean age 67.5, female 79%, White n = 14 | Quantitative; RCT; all patient-surrogate dyads randomized into 1 of 2 decision-making modalities: control group (listening to verbal narrative describing advanced dementia) or intervention group (listening to a verbal narrative followed by viewing a 2-minute video decision-support tool depicting a patient with advanced dementia). | Video depicts a person with advanced dementia together with her 2 daughters in the nursing home setting. The patient fails to respond attempts at conversation, is pushed in a wheelchair, and is hand-fed pureed food, all depicting someone with FAST 7a dementia | Patients and surrogates viewing video decision-support tool for advanced dementia are more likely to concur about the patient's end-of-life preferences than when listening to a verbal description of the disease. Viewing the video decision-support tool was associated with a trend toward more knowledge of advanced dementia among both patients and their surrogates |
| Boerner (2013)30 Level 4 |
To evaluate the effects of three aspects of family relations- general family functioning, support and criticism from spouse, and support and criticism from children- on both overall ACP and specific durable power of attorney for health care (DPAHC) | Outpatient; two large university hospitals and one comprehensive cancer center in New Jersey. Participants from the New Jersey End-of-Life study of noninstitutionalized adults aged 55 years and older | n = 293; average age 69: female ∼67%. Not reported: ethnicity | Quantitative; cross-sectional study; 1.5 hours face to face interview using computer-assisted personal interview technology | Consideration of family dynamics affect on ACP through categories of a two-pronged approach (AD and discussions), discussions only, and no planning (omitted category) | In general, families who are best equipped to make collaborative decisions about end-of-life care and to weather the distress associated with bereavement are precisely the persons who engage in ACP in the first place, those with high levels of family functioning. Person with low levels of family functioning including problematic decision making and communication styles are least likely to engage in ACP |
| Heyland (2013)102 Level 4 |
To inquire about patients' ACP activities before hospitalization and preferences for care from the perspectives of patients and family members, as well as to measure real-time concordance between expressed preferences for care and documentation of those preferences in the medical record | Inpatient; 12 acute care hospitals in Canada | n = 278 patients, mean age 80, female 53%, white n = 263; n = 225 family members, mean age mean age 60.8 years, female 61%, white n = 221 | Quantitative; Multicenter, prospective study; separate face-to-face interviews with patients and family members | Assessment of ACP activities and preferences through a questionnaire and then concordance of expressed preferences and orders of care documented in the medical record. Questions related to domains relevant to communication and decision making (relationship with physicians, communication, decision making, and role of family) | The majority of patients and family members had considered and discussed the use or nonuse of life-sustaining technologies near the EOL and could clearly express their preferences for EOL care. There was little effective communication about ACP between the patient or family and members of the health care team before hospitalization. Less than one-third of patients and families reported that they had been asked about their advance care plans on admission to the hospital |
| Pearlman (2005)39 Level 2 |
To evaluate the effectiveness of a comprehensive, systems-oriented ACP intervention that included the Your Life, Your Choices workbook | Outpatient; Department of Veteran Affairs outpatient clinics | Intervention group n = 119, mean age 68.5, male 95%; White 89%, African American 8%, Other 3%; Control group n = 129, mean age 69.5, male 95%, White 88%, African American 9%, Other 3%; Primary care providers recruited and then patients from their practices recruited | Quantitative; Block-RCT with multifaceted ACP intervention. Two days after index visit, patients in both groups were called whether they had discussed ACP with their providers. All other outcomes data collected 4 months after the index visit to allow sufficient time for the ACP process and follow-up visits to occur | ACP workbook, Your Life, Your Choices, a 52-page workbook that incorporates concepts from multiple frameworks including stages of behavioral change, the health belief model, self-efficacy, the relationship between states/fates worse than death and patient preferences to forego life-sustaining treatment, and general guidelines about human information processing and information design. Workbook has three parts: 1) case stories written to convey basic information and motivate persons to engage in ACP behaviors; 2) 4 subsections including exercises to elicit values about quality of life, glossary describing health states that may cause decisional incapacity, life-sustaining treatments, and palliative care, documents for recording health state ratings and treatment preferences, and advice about communicating with family members and health care providers; 3) advice about communicating with family members and health care providers. Intervention group received workbook, 30-minute appointment with Social Worker before provider visit. Control group mailed 8-page advance directive packet which included the living will and durable power of attorney for health care forms prior to scheduled appointment. | The intervention was successful in increasing ACP discussion, all aspects of directive completion, and filing of advance directives in the medical record. Rate of documentation doubled, though achieved 48%, and may represent ceiling effect if advance directives are not for everyone. The intervention had no effect on agreement between proxies and patients for any of the treatments of quality-of-life assessments. |
| Chiu (2016)36 Level 4 |
To determine the decision control preferences (DCPs) of diverse, older adults and whether DCPs are associated with participant characteristics, ACP, and communication satisfaction | Mixed; hospital, Veteran Affairs medical center, low-income senior centers, cancer support groups all in San Francisco | n = 146; mean age 70.8; female 41%, White n = 69, African American n = 39, Latino or Hispanic n = 10, Asian or Pacific Islander n = 19, Multiethnic n = 9 | Quantitative; Cross-sectional survey data pooled from four cohort studies | Use of DCPs to assess the degree of control patients prefer medical decisions made with their doctors. Doctor makes all decisions (low), shares with doctor (medium), makes own decisions (high) | 18% wanted doctors to make all of their medical decisions (low DCPS). 34% wanted to share medical decisions (moderate DCPs). 48% wanted to make their own medical decisions. Almost one-fifth of diverse, community dwelling older adults with multiple comorbidities wanted their doctors to make medical decisions for them. Older age was the only patient characteristic significantly associated with lower DCPs. |
| Wu (2008)37 Level 4 |
To describe end-of-life ACP among the oldest-old and to identify patient characteristics and healthcare utilization patterns associated with likelihood of care planning documentation | Mixed, chart review; Veterans Affairs Greater Los Angeles Healthcare System (VA GLAHS) | n = 175; median 88 years old, age range (85–104), Male n = 174, White n = 133, African American n = 24, Hispanic n = 8, other n = 1 | Quantitative; retrospective chart review | Examination of care preference documentation using electronic medical records | Care preference documentation and surrogate identification occurred for 50/149 (34%). Thirty (60%) care preferences were first documented during an inpatient episode. Seventy-nine (53%) had no preference documentation, including 14 (9%) provider attempts to elicit discussion. Sixty-eight (46%) of 149 charts documented a surrogate for health care decisions. Eighty-one (54%) patients had no identified surrogate, including 9 (6%) with attempted discussions. Outpatient utilization had the largest impact on documentation, dictated mostly by general and geriatric visits |
| Chu (2011)31 Level 4 |
To describe the knowledge and preferences of Hong Kong Chinese older adults regarding advance directive and end-of-life care decisions, and to investigate the predictors of preferences for advance directive and community end-of-life care in nursing homes | Long-term care; 140 nursing homes in Hong Kong | n = 1600; mean age 82.37; female n = 1060; | Quantitative; cross-sectional survey; face-to-face interviews | Interview with discussion of advance directives, hypothetical conditions (cancer and noncancer terminal conditions), life-sustaining treatments or devices, and location of care settings in end-of-life. | 94.2% Participants would prefer to be informed of the diagnosis if they had a terminal disease. 77.3% would prefer to stay in their present nursing home until the last days of life. 96% participants had not heard of the term advance directive previously. After explanation of the meaning of advance directive, 88% agreed that it would be good to have an advance directive for them regarding medical treatment decisions in the future. 90% participants would prefer to know the diagnosis of a terminal disease. The strongest predictor for having an advance directive was the wish to be informed of a terminal illness |
| Volandes (2016)41 Level 4 |
To examine with ACP documentation would increase after ACP video implementation. To evaluation use of hospice, hospital mortality, and cost associated in the last month of life | Mixed; Community; Hilo, Hawaii which is serviced by one 276 bed hospital, one hospice, and 30 primary care practices | City of Hilo in Hawaii (population 43,263); Population of diverse backgrounds: Asian 34%, 2 or more races 33%, White 18%, Native Hawai'ian and Pacific Islander 14%, Latino 10%; Inpatient: Control: n = 346, mean age 67, Female 45%; Video intervention: n = 2773, mean age 70.2, Female n = 1292. Outpatient: All PCPs not in Hilo: n = 42,099, mean age 84.1, Female = 25,680; All PCPs in Hilo: n = 3888, mean age 84.0, Female n = 2294 | Quantitative; Implementation study x 21 months | ACP video decision aid. Videos attempt to provide a general framework to which to understand ACP including the broad questions that patients should reflect upon and how individual preferences can be translated into actionable medical orders and interventions | After intervention, there was an increase in ACP documentation of patients' preferences in the inpatient and outpatient settings. More patients with advanced illness were likely to be discharged to hospice, which was reflected in decreased hospital death rates. In the year after the implementation of videos, the hospice admission rate grew in Hilo (28%) relative to the rest of the state (12%) and national trends (4%) and decreased costs in the last month of life for decedents. Recommendations: decisions aids can play an important role in prompting discussions with providers who may not feel that they were adequately trained to have these discussions otherwise |
| Braun (2014)67 Level 6 |
To describe self-reported decision-making styles and associated pathways through end-of-life (EOL) decision-making for African-American, Caucasian, and Hispanic seriously ill male Veterans, and to examine potential relationships of race/ethnicity on these styles | Community; VA Medical Center in Houston, Texas | n = 44 participated in one of eight focus groups; mean age 57.8, age range 55–83, female n = 1, African American n = 14, Hispanic n = 17, Caucasian n = 13 | Qualitative; Focus groups lasting 5–90 minutes. Focus groups organized by race/ethnicity with female, trained, race/ethnicity concordant moderators with experience in qualitative research | Focus groups to determine patients' selection of their preferred decision-making style as the first step in EOL decision making. | Two fundamental decision-making styles emerged: deciding for oneself or allowing others to decide, with five important variants in how patients expressed and justified these styles. Deciding for oneself: “Autonomists” (takes responsibility for one's decisions) and “Altruists” (does not want to burden others with decision making). Letting others decide: “Authorizers” (transfers authority by explicit authorization), “Absolute Truster” (transfers authority by implicit authorization), and “Avoider” (accepts surrogates' decision making by default). No apparent relation to race/ethnicity in terms of the two basic decision-making styles or the five variants. |
| Almack (2012)86 Level 6 |
To explore with patients, carers, and health care professionals if, when and how advance care planning conversations about patients' preferences for place of care (and death) were facilitated and documented | Mixed; five care services with involvement in palliative care were selected across one region (urban and rural England), chosen to cover palliative care provision for cancer and noncancer populations | n = 18 cases (18 patients; 11 relatives) initial interview, female = 8; mean age 73; n = 6 cases (5 patients; 5 relatives) follow-up interview | Qualitative; exploratory case study design; retrospective audit of care delivered in the last four weeks of life and then followed by interviews | Explore perspectives of all parties concerned (healthcare professionals, patients and family carers). Use Preferred Place of Care (PPC) tool. Discussion and recording of these preferences of patients on place of care and death were felt as important means of supporting and enabling patient choice. | Patients demonstrated varying degrees of reticence, evasion, or reluctance to initiate any conversations about end-of-life care preferences. Most assumed staff would initiate conversations and often staff were hesitant to do so. Staff identified barriers including the perceived risks of taking away hope and issues of timing. Staff were often guided by cues from the patient or by intuition about when to initiate these discussions |
| Abdul-Razzak (2014)48 Level 6 |
To understand patients' preferences for physician behaviors during end-of-life communication | Inpatient; 3 Canadian academic tertiary hospitals | n = 16; Female 69%, age: 55–59 (n = 1), age 60–69 (n = 4), age 70–79 (n = 2), age 80–89 (n = 6), age >89 (n = 3); Caucasian n = 12, non-Caucasian n = 0; 70% noncancer diagnosis | Qualitative; Interpretative descriptive method from semi-structured interviews conducted with patients admitted to general medical wards. Interviews ranged from 22 to 78 minutes in duration | Interview guide with qualitative approach to understand patient perspectives on physician behaviors to incorporate into physician's clinical practice and gain information for communication skills training initiatives for physicians and trainees | Two major themes: 1) “knowing me” relates to the influence of life history and social relationships on shaping personal values and preferences for health care; theme subdivided into subthemes of acknowledging family roles and respecting one's background; 2) ‘conditional candour’ describes a preference for receiving frank information from a physician, but with some important qualifications, which are elaborated in subthemes of assessing readiness, being invited to the conversation, and appropriate delivery of information |
| Schonwetter (1996)99 Level 4 |
To determine whether life values are related to resuscitation preferences and living will completion in an older population and to assess beliefs about the applicability of living wills | Community: independent retirement community | n = 132; mean age 79.3; well-educated, informed older population that may have obtained knowledge of subject matter at social service department of the retirement community; Not reported: gender, ethnicity | Quantitative; structured, individual interviews | Questionnaire with knowledge assessment, preference of care in hypothetical clinical scenarios, and completion of 13 life value statements in terms of their importance for their medical decision-making near the end-of-life | Results suggest discussions concerning advance directives should include an evaluation of the patient's value system and that patients should be better educated concerning the applicability of their advance directive documents. Using life values as part of an advance directive may not only allow patients to better understand the type of medical care they want in the future but also guide physicians and proxies by the patient's stated values |
| Barnes (2007)60 Level 6 |
To explore the acceptability of an interview schedule designed to encourage conversations regarding future care and to explore the suitability of such discussions and inquire about their possible timing, nature and impact | Mixed; outpatient, hospice, day unit; Focus group occurred at academic department of university setting; United Kingdom | n = 22; age range 32–80, median age 60; female 59%, Caucasian n = 21 | Qualitative; Focus groups, 8 total, each lasting about 1 hour, no more than 4 participants in each group; Participants considered the ACP interview schedule for one week and then attended a focus group | ACP interview schedule inquired about experiences of care, clinical and personal circumstances, worries and concerns regarding the future, and whether the patient might wish to complete a written advance directive. Focus groups used to explore wider acceptability of the interview schedule, suitability of discussions and timing, nature and impact. | Emergent themes include: prompting patients to think about issues, timing of ACP, recognizing individuality, person conducting ACP discussion, losing a sense of hope, maintaining a sense of control, advance directives, and effect of taking part in a focus group. |
| Garrido (2013)35 Level 4 |
To evaluate the extent to which religious affiliation and self-identified religious importance affect advance care planning via beliefs about control of life length and end-of-life values | Outpatient; from New Jersey EOL study; participants recruited from two hospital clinics and a cancer center | n = 305; average age 69, age range 55–90; Female n = 193; White 60.3%, Black 26.2%, Hispanic 18%, Other 13.4%. Most common religious affiliations were Catholic (31.1%), mainline Protestant (22.3%), Jewish (17.4%), and conservative Protestant (16.4%) | Quantitative; cross-sectional | Examination of whether and how religion affects ACP via beliefs and values about EOL control | Religion/spirituality was very or extremely important to most respondents (74.8%). Beliefs in God's control over life length were associated with lower likelihood of ACP (informal or formal) whereas valuing individual control over EOL circumstances was associated with greater ACP likelihood |
| Chung (2017)34 Level 4 |
To describe the knowledge, attitude, and preferences of the general Hong Kong adult population across different age groups regarding EOL care decisions, place of care and death, as well as advance directives | Community; Hong Kong; Telephone | n = 1067; age 30–39 (11.5%), age 40–49 (17.4%), age 50–59 (22.8%), age 60–69 (27.4%), age 70–79 (13.8%), age 80+ (7.1%); female n = 669 (62.7%); largest proportion rated their health as fair | Quantitative population-based cross-sectional survey; conducted by telephone by experienced interviewers; | Inclusive survey to general population >30 years old to focus on 3 important aspects of EOL care including: advance decisions, palliative care, place of care/death | After explaining ADs, 73.9% agreed that making their own medical decisions in advance was a good approach, and 60.9% would consider making an AD if legislated. 87.6% of the participants would prefer appropriate palliative care that gives comfort even though it may not prolong life as they approach their end of life. 31.2% wanted to die at home, but after considering that they might not have sufficient care and support, 19.5% remained to prefer home as their place of death |
| Gjerberg (2015)53 Level 6 |
To describe 1) the extent nursing home patients and relatives have been involved in end-of-life care discussion, and the desirability of such conversations, 2) their views on medical information, and 3) how they perceive their own role in future end-of-life care decisions | Long-term care; 6 nursing homes in Southeast part of Norway | n = 35 patients; mean 86, age range 68–98; Female 77%; n = 33 relatives participated in 7 focus group interviews consisting of 3–8 persons | Qualitative; Explorative design; Combination of individual semi-structured interviews with nursing home patients and focus group interviews with relatives. Interviews carried out in the patient's room and each interview lasted between 20–40 minutes | Interviews with patients focused on EOL care communications, information, and shared decision-making. Focus group interviews covered 8 questions, of which five were related to EOL care communications, information, and shared decision-making. | 3 main categories emerged from the interviews: 1) the lack of EOL care communication, 2) wishing to be informed, 3) shared decision-making. Very few nursing home patients and relatives had participated in conversations with the nursing home staff about preferences and wishes for EOL care. Some patients wanted to talk about this, while others were reluctant or indifferent to discussions. Most people wanted their voice to be heard in decisions about medical treatment, though several patients wanted to leave the decisions to health-care professionals |
| Karasz (2010)68 Level 6 |
To analyze the following questions: 1) What is the family's understanding of decision making in the context of the family meeting? 2) To what extent do members of the staff and family members use the rational choice model in their discussions about end-of-life care? 3) How well do the three standards of the rational choice model appear to reflect the values and priorities of patients' families? 4) What other types of moral priorities play a role in family decision making? | Inpatient; 2 general medicine wards and an intensive care unit in public teaching hospital in the Bronx, New York | n = 26 decision-making meetings between hospital staff and family members were observed; n = 23 patients, mean age 72, female 52%, black 39%, Hispanic 30%, white 26%, Asian 4% | Qualitative; observation of family meetings and semi-structured follow-up interviews | Decision-making meetings between hospital staff and family members were observed and recorded. Following the meetings, families engaged in in-depth group interviews focusing on their experience and interpretation of the meeting that had just taken place. Then conducted follow-up interviews with families by phone. Family also interviewed when a patient died during the study period. Consideration of rational decision model and moral decision making were the focus for the study analysis | For both staff and families, consideration of a patient's best interests generally took priority over the patient's wishes. Staff generally introduced discussion of the patient's wishes for rhetorical purposes, such as persuasion. Description of family meeting: families appreciated the meeting was not necessarily the opportunity to weigh options and influence the course of their relative's care, but to be acknowledged as moral witnesses to a key transition in the patient's life course. |
| Malcomson (2009)50 Level 6 |
To explore the ACP perspectives of healthy elders | Mixed; Community; 1 community senior center and 2 assisted living facilities | n = 20; age range 60–94 years old; female n = 15 (7%), Caucasian n = 18 (90%), no response n = 2 (10%) | Qualitative; 4 Focus groups ranging from 50–80 minutes in length with the two investigators facilitating with 4–6 participants | Focus groups of health elders to uncover: 1) What forms of communication have healthy elders had regarding ACP? 2) What is the comfort level of healthy elders regarding discussion of end-of-life preferences? 3) What factors contribute to and impede communication and comfort on the issue of ACP? | 5 major themes: 1) ACP is strongly influenced by concern for others, 2) elders assume that preferences are known to their trusted friends, family, and providers, even in the absence of explicit communication with these people, 3) elders value a healthcare system that supports provider time, focus, and continuity; 4) being “known” to a provider is critical to comfort that ACP preferences will be respected, 5) elders are generally ready and eager to discuss ACP. Additional findings include: elders are better prepared for the event of death than the dying process; lawyers and financial planners play a prominent role in guiding elders through end-of-life decisions; and elders believe that the optimal time for ACP discussion is during periods of relative wellness. |
| Silvester (2013)82 Level 4 |
To report on the quality of ACP documents in use in residential aged care facilities (RACF) in areas of Victoria Australia prior to a systematic intervention; to report on the development and performance of an aged care specific ACP template used during the intervention | Long-term care; Metropolitan and regional areas of Victoria, Australia | n = 19 RACFs; bed range under 50 to over 100, all provide high-level care; Not reported: patient age, gender, ethnicity | Quantitative; Retrospective review of preimplementation ACP documentation. Chart audit of Advance Care Plans completed on recommended template. | Development of the aged care specific Advance Care Plan template. Key components included Medical Enduring Power of Attorney (MEPOA) and details; whether the resident was competent at the time of completion; and information concerning the resident's end-of-life values and important wishes. | Standardization of ACP processes and documentation is likely to improve the quality and ultimately the outcomes of ACP in the residential aged care sector. The guiding principles of ACP in aged care and the use of the template presented should assist RACFs and their staff to increase the frequency and quality of completion of Advance Care Plans in the residential aged care setting |
| Seymour (2003)79 Level 6 |
To examine older peoples' beliefs and risk perceptions regarding the use of innovative health technologies in EOL care and to relate these beliefs to their ideas about ‘natural death’ | Community; Sheffield, United Kingdom | n = 77 total; Focus group: n = 32, age <55 n = 2, age 55–64 n = 7, age 65–74 n = 15, age 75–84 n = 5, age 85+ n = 2; female 30%; White British n = 26, White Irish n = 2, Black Caribbean n = 2, Black British n = 1; Interview group: n = 45, age <55 n = 0, age 55–64 n = 2, age 65–74 n = 16, age 75–84 n = 15, age 85+ n = 12; female 64%; White British n = 45, White Irish n = 0, Black Caribbean n = 0, Black British n = 0 | Qualitative; two-phase exploratory study. All interviews conducted in participants' own homes or in their care home. Phase 1- eight focus group discussion; phase 2- conducted in participants' home | Use of pictures, story boards and media extracts used during study phases 1 & 2. Phase 1 Focus groups- participants invited to commit on a simple ‘aide memoire’ presented through power point presentation on following: 1) Where is the best place to be cared for (home, hospital, nursing home or hospice)? 2) Using technology to prolong life (resuscitation and artificial feeding), 3) Using technology to give comfort (terminal sedation and morphine), 4) Who should decide (clinical staff/patient/family communications and advance care statements)? Phase 2 Interviews- two hypothetical vignette scenarios introducing key options associated with ‘life prolonging’ and ‘basic care’ approaches to EOL care were used in the interviews. | Life prolonging technologies: Focus group responses to materials on resuscitation and artificial feeding was a consensus that the availability of life prolonging interventions should not make their use automatic. Majority of participants felt discussion about resuscitation reduces uncertainty and gives patients information about their bodies, allows for autonomous decision making, has potential to facilitate discussions with patients and their families about death and dying, and helps the doctor foster the ideal doctor-patient relationship build on respect and mutual understanding. A minority of participants felt doctors should not discuss resuscitation as they need to protect patients from burdens and a family carer should act as a proxy or protector role. Basic care technologies: focus groups and interview participants identified home as the preferred place to be cared for at the EOL in ideal circumstances but recognized the practical and moral problems including worries of burdens on family, caring skills of family carers and risk of receiving inadequate symptom relief. |
| Piers (2013)54 Level 6 |
To explore and understand elderly patients' perspective on end-of-life care planning with a main focus on planning future medical treatments | Mixed: nursing home, inpatient (acute geriatric ward, medical oncology, palliative care unit), home services | n = 38; age median 81, age range 71–104; female 68%; Not reported: ethnicity | Qualitative; semi-structured interviews, mean duration 50 minutes; interviewed in their own home, nursing home, or private room of hospital | Interviewers tried to elicit interviewees' personal narratives of 1) what was important in their life at that moment to explore the patients' broad values and 2) their wishes and attitudes toward planning for end of life | 3 main categories emerged from the interviews: the lack of EOL care communication, wishing to be informed, shared decision-making. Very few nursing home patients and relatives had participated in conversations with the nursing home staff about preferences and wishes for EOL care. Some patients wanted to talk about this, while others were reluctant or indifferent to discussions. Most people wanted their voice to be heard in decisions about medical treatment, though several patients wanted to leave the decisions to health-care professionals |
| Pollak (2015)21 Level 6 |
To describe how patients and caregivers perceived motivational interview (MI) techniques in palliative care role-play encounters | Outpatient; Patients and caregivers identified from seven internal medicine physicians' panels | n = 21 patients and caregivers; Patient n = 12, caregiver n = 9; age mean 69.8; female n = 16 (76.2%), White n = 19 (90.5%), Asian n = 1 (4.8%), other n = 1 (4.8%) | Mixed; qualitative analyses of the “think-aloud” interviews in conjunction with the role-play encounters; quantitative analyses of the Consultation And Relational Empathy (CARE) measure; pilot study | Role play with patients and caregivers who face serious illness with three palliative care scenarios involving decisions regarding completing advance directives, pursuing further chemotherapy, or electing hospice The designated study physician then entered the room, turned on the audio recorder, and started the role play. After the role play ended, the study physician left, and the study staff member asked the participant to complete a survey that assessed perceived empathy. A cognitive interview "think-aloud" was conducted with staff member and participant as audio-recorded conversations were listened to and stopped the recording any time the study physician said something that was helpful or unhelpful. | 3 themes related to communication elements that were acknowledged by study participants as helpful: 1) reflection and validation of values, 2) autonomy support and ability to change mind, 3) open questions acting as catalysts for talk. 1 theme describing unhelpful communication elements: closed questions and physician-dominated talk. Role-play encounters between participants and the MI-trained study physician were associated with higher ratings of perceived empathy and shorter duration than the nontrained MI physician. |
| Fried (2017)52 Level 6 |
To understand the perspectives of both patients and the person who would make medical decisions for them if they were unable (surrogates) on their participation in ACP | Community; VA Connecticut Healthcare System | n = 31 veteran-surrogate dyads; Veteran: age 55–59 n = 9, age 60–69 n = 12, age 70+ n = 10; female n = 10 (32%), White n = 23, Other n = 8; Surrogate: age <50 n = 6, age 50–59 n = 15, age 60–69 n = 10; White n = 24, other n = 7 | Qualitative cross-sectional; veterans and surrogates interviewed separately with closed-ended interviews. Then a dyadic telephone interview was conducted with a discussion guide. | Participation in ACP activities assessed: two communication activities (communication with loved one regarding the use of life-sustaining treatment, communication with loved one regarding valuation of quantity vs quality of life) and two procedural activities (formal appointment of a healthcare surrogate decision-maker and completion of a living will). The veteran was asked about participation on his/her own behalf and the surrogate about participation on behalf of the veteran. Participants were asked about acceptability of different health states resulting from treatment of serious illness. Veterans were asked whether they believed the states were acceptable and surrogates asked what they believed the veteran would say | Disagreement about engagement in ACP ranged from 33% for communication about quality of life to 48% for appointment of a healthcare surrogate. The most frequently discussed facilitator of ACP was direct experience with others, either by the veteran or by the surrogate. Findings suggest engagement in ACP as a dyadic activity. Surrogates can both help and hinder efforts to promote ACP. If perspectives on ACP engagement not shared, this can be evidence of misunderstanding, mismatched readiness to communicate, and a process that has failed to meet need of the members of the dyad |
| van Eechoud (2014)69 Level 6 |
To gain understanding of the involvement of family members in ACP for older people near the end-of-life by exploring their views and experiences concerning this process | Mixed, three geriatric settings: nursing homes, an academic hospital (the acute geriatric ward, the medical oncology ward, and the palliative care unit), and homes services for older people at home but requiring help for activities of daily living; Flanders, Belgium | n = 21 family members; family members interviewed of patients in age range 69–104; not reported: gender, ethnicity | Qualitative; semi-structured interviews; mean interview duration 56 minutes, interviewed at location of participant's choice | Interview focused on: personal narratives of their experiences with the patient's disease, their opinion about planning the patient's end-of-life care, and their role in the end-of-life care planning | Result themes: lack of accurate knowledge and different positions of family members (burdened with decision-making, feeling disowned by being excluded from decision-making, permitted to avoid decision-making, permitted to take direction in decision-making, together in decision-making). Several factors influenced how much responsibility the family member wanted to take and/or to what extent the family member felt the patient expected him/her to play a part including: patient's course regarding imminent death, experience family members previously had with death and dying, the opinion of family members about benefits of ACP had an impact on the extent to which they wanted to take responsibility in ACP, consideration of initiation of conversations about death and dying to be burdensome due to taboo subject or desire to spare their loved one this emotional issue and EOL, family member's trust in health-care providers. Long-lasting family dynamics and relationship patterns held true in ACP of the patient |
| Detering (2010)57 Level 2 |
To investigate the impact of advance care planning on EOL care in elderly patients | Inpatient; Melbourne, Australia | n = 309; Intervention group: n = 154, age median 85; Control group: n = 155, age median 84; Not reported: gender, ethnicity | Quantitative; Prospective randomized controlled trial; Intervention group received formal ACP. Control group usual medical care but no ACP unless it was specifically requested | Formal ACP from a trained facilitator using the Respecting Patient Choices model for the intervention group. Primary outcome measure was the proportion of patient who had died and whose EOL wishes were known and respected by their doctors. Secondary outcome measures included survey of patient satisfaction on their hospital stay and an assessment of the impact of a patient's death on relative using the impact of events scale and hospital anxiety and depression scale | Essential elements of the program responsible for the primary outcome of successful ACP: trained facilitators, patient centered discussions, involvement of family in discussions, correctly filed documentation, and systematic education of doctors. ACP reduces the incidence of anxiety, depression, and posttraumatic stress in surviving relatives. ACP improves patient and family satisfaction with EOL care |
| Bravo (2016)62 Level 2 |
To test an intervention designed to motivate older adults in documenting their healthcare preferences in advance, and to guide proxies in making hypothetical decisions that match those of the older adult | Community; Health education program occurred at the meeting room at the research center; Experimental intervention occurred at the home of one of the dyad members and at the meeting room at the research center; Canada | Experimental group: n = 118, Older adults' age mean 77.6, female 46%; Proxies' age mean 70.5, female 71%; Control group: n = 117 Older adults' age mean 77.6, female 46%; Proxies' age mean 70.0, female 68%; Proxies had known the older adult for nearly 50 years on average. Not reported: ethnicity | Quantitative; Randomized controlled trial; Baseline interviews collected for both groups. Concordance assessments repeated in the month following the end of the intervention and six months later to assess its effect on accuracy of substitute decision making | Multimodal ACP intervention consisting of an educational component, a structured approach to reflecting on preferences for future health care, and a way for those preferences to be communicated. My Preferences booklet allowed for interested individuals to record their wishes regarding future health care should they lose the capacity to make decisions on their own | The intervention was found effective in motivating older adults to document their preferences but not in helping their proxy make hypothetical decisions that match their own. 80% of participants documented their preferences for future health care should they be incapacitated. Most older adults opted for comfort care in circumstances such as event of incapacity. The intervention did not improve their proxy's ability to make more concordant decisions in hypothetical situations, except if highly discordant at baseline. Consideration of a less-intensive intervention that still includes the three essential elements including education, structured approach to reflection on preferences for future health care, and a way for preferences to be communicated, should be considered. |
| Winter (2013)100 Level 4 |
To test whether patient values are associated with treatment preferences, compare values and preferences to responses from a standard living will, and determine whether some values are better predictors than others | Community; Philadelphia metropolitan region; | n = 304; age mean 72.4, age range 60–96; Female 77% | Quantitative; Cross-sectional study; Participants interviewed in their homes by telephone | Interview consisted of an 8-item EOL values scale, a standard living will question, preferences for 4 life-prolonging treatments in each of the 6 scenarios, and sociodemographic questions | EOL values are useful guides to EOL treatment preferences. Both value factors predicted treatment preferences independently of each other and demographic characteristics. The religion/longevity/family wishes values predicted treatment wishes in all scenarios; dignity/pain/burden values predicted treatment wishes in most scenarios, excluding only the extremes. It was noted that only in religion/longevity that family wishes values contributed to unique variance over and above the living will responses, whereas dignity/pain/burden values seemed redundant with the living will response. Also in knowing an individual's values regarding religion, longevity, and following family wishes may be helpful in predicting the EOL care he or she would prefer in most EOL scenarios, over and above preferences expressed in a living will or sociodemographic characteristics. Therefore, these values would be useful additions to an ACP document to guide medical care decision making |
| Towsley (2015)103 Level 6 |
To describe the communication, content and process, related to EOL conversations among residents, family, and staff | Long term care; Four nursing homes in southeastern Pennsylvania (3 urban, one suburban) | n = 16 nursing residents, mean age 88.4, age range 64–100, female n = 10 (62.5%), African American n = 9 (56.3%), More than one race n = 1 (6.3%), White n = 6 (37.5%); n = 12 family members, mean age 61.3, age range 52–79, female n = 11 (91.6%), African American n = 5 (41.6%), White n = 7 (58.3%) | Qualitative, descriptive study; semi-structured interviews conducted with residents, family, and staff. Interviews conducted face to face in confidential settings and ranged from 20 to 60 minutes. | Interviews to describe conversations about EOL preferences, participants' conversation, timing of conversation, and content of discussion. Barriers and facilities were queried to capture EOL care in nursing home setting | The overarching theme that emerged from the analyses was missed conversations. Residents, families, and staff did not routinely, if ever, discuss EOL care preferences, pass along information about preferences, or initiate conversations about preferences with each other. They talked about current food preferences, daily activities, medications/medication changes, or burial plans. Conversations did not commonly include discussion of a living will/AD, preferences for code status or hospitalization, use of hospice, or other care practices that might bring residents comfort. Interviews revealed inconsistencies in the process of discussing EOL treatment preferences in the NH and revealed inconsistencies in staff roles. Eliciting preferences about EOL was not integrated into care provision. |
| Cheang (2014)66 Level 6 |
To assess prevalence of advance care directives and documented medical orders about end-of-life care for elderly inpatients; to explore the feasibility of an ACP screening interview | Inpatient; Royal North Shore Hospital in Australia | n = 100; age mean 87, age range 80–98; Female n = 64. No report: ethnicity | Mixed; Single-center cross-sectional analysis with inclusion of qualitative interview | ACP screening interview exploring their views on ACP an if an ACP was previously documented | Patients may prefer discussing ACP in outpatient setting but many are happy to discuss ACP in the hospital environment and this is supported by the high level of comfort with the ACP screening interview and openness to further ACP discussions reported by patients. |
| Lum (2016)90 Level 6 |
To describe the feasibility of the first primary care-based group visit model focused on ACP | Outpatient; Seniors geriatric clinic at University of Colorado Hospital. Clinic is a patient-centered medical home that provides primary care for about 1900 xolder adults | n = 32 patient participants in 5 group visit cohorts (40% participation rate from 80 patients approached); n = 27 participated in both sessions (87% retention rate); mean age 79; Female n = 19 (59%); Native American n = 1 (3.1%), Hispanic or Latino n = 1 (3.1%), Black or African American n = 7 (2.2%), White n = 23 (72%); n = 48 patient that did not participate, mean age n = 78, Female n = 34 (71%), ethnicity not reported | Mixed; Pilot demonstration; GMV sessions were audio recorded, transcribed, and analyzed using a mixed inductive and deductive approach | Development of the first ACP group visit “Conversation Group Medical Visit (GMV).” This model of group medical visits leverages group dynamic to transform the typical patient-clinician encounter related to ACP. The Conversation Group Medical Visit aims to engage patients in a discussion of key ACP concepts and support patient-initiated ACP actions- choosing surrogate decision makers, deciding on preferences during serious illness, discussing preferences with decision makers and health care providers, and documenting advance directives in EHR | RE-AIM: Reach: Patient Participation- the goal was to schedule 8 to 12 patients per cohort, but actual group sizes ranged from 4 to 9 patients due to patient cancellations. Effectiveness: Patient Acceptance of and Engagement in ACP Conversations- majority of patients rated the Conversation GMV better than usual clinic visits for talking about ACP, thought they received useful information, felt comfortable talking about ACP in the group, and found talking with others about ACP to be helpful. Adoption: Clinical Referral Patterns-ten of 11 clinicians referred at least 1 patient to the conversation GMV, median 5, range 1 to 23. Implementation: Patient Retention and Aspects of ACP discussed- 27 of 32 patients participated in both sessions. Key discussion themes included sharing personal values and challenges related to ACP and discussing a broad range of patient raised topics related to ACP. Maintenance: not evaluated in pilot. |
| Lankarani-Fard (2010)77 Level 4 |
To evaluate the feasibility of using the Go Wish card game with seriously ill patients in the hospital | Inpatient; VA Greater Los Angeles Healthcare System | n = 33; age mean 62, age range 31–83; Male n = 33 (100%); Caucasian n = 21 (64%), African American n = 10 (30), Latino/Hispanic n = 2 (6%) | Quantitative; Observational study | Go Wish card game can be used as a decision-making tool by chronically ill inpatients to prompt consideration of their preferences across a wide range of isues. The game can serve as an initial step in clarifying goals of care and be implemented with minimal training and within a reasonable time period | All of the 36 cards appeared in at least one patient's top 10 list. The highest-ranking value overall was “to be free from pain,” a provider-focused value. This value was chosen by 20 of 33 (60%) of the subjects and usually ranked high on the list. The second and third most frequently selected value when adjusted for rank concerned spirituality and faith: “to be at peace with God” and “to pray.” The similarity of the study's patients' responses to other studies suggest that the card game accurately reflects a patient's priorities in an efficient manner. The Go Wish game allows patients to consider values across a broad range of topics that may not be instinctively important at first to the patient or the provider. The deck of cards is inexpensive and was completed by 25% of the patient approached despite their acuity of illness. Because patient sorted through the card game in private, they were allowed ample time to reflect on their values in a non- stressful setting |
| Tieu (2017)26 Level 2 |
To measure the impact of a personalized ACP electronic message on advance directive (AD) completion in the primary care setting | Outpatient; Mayo Clinic 's Division of Primary Care Internal Medicine Clinic in Rochester, Minnesota | n = 200 intervention electronic message, age mean 71.9, Female n = 93 (47%); n = 2294 control, age mean 71.7, Female n = 1197 (52%); Not reported: ethnicity | Quantitative; Randomized controlled trial; intervention arm & usual care | Patients randomized to the intervention arm received a personalized patient electronic messaging (PEM) explaining the ACP process and encouraging them to compete an AD. The electronic message also included a link to an ACP workbook that guided the individual and their loved ones through each step of the ACP process. The workbook included a Minnesota-specific AD form with instructions on how to return the completed document to the patient's primary care provider. Eight weeks after the initial message was sent out, a reminder message was delivered to those individuals who had not yet returned an ACP. Final outcomes data were collected at 12 weeks | Individuals receiving personalized, electronic motivational prompts and electronic resources were statistically significantly more likely to complete and return an AD document when compared to usual care. The content of the ADs that were completed as a result of this minimally intrusive intervention was both comprehensive and clinically useful. Among the intervention group, 11 (5.5%) completed and returned an AD during the study period compared to 46 (2%) in the usual care group. Of the 200 patients randomized to receive the intervention, 149 (74.5%) opened their electronic message. This randomized trial demonstrates the feasibility and utility of electronic messaging systems in facilitating ACP in some primary care patients. Motivational portal messaging has established utility as a low touch, inexpensive intervention that has increased patients' willingness to participate in various aspects of health care |
| McCarthy (2008)29 Level 4 |
To describe self-reported ACP, health care preferences, use of advance directives, and health perceptions in a very elderly community-dwelling sample | Community; Occurred in Framingham Health Study clinic in Framingham, Massachusetts or at offsite locations because of distance | n = 220 respondents; age mean 88; Female 67%; surveyed surviving participants of the original cohort of the Framingham Heart Study; must be cognitively intact and community-dwelling; Not reported: ethnicity | Quantitative; Prospective observational cohort study; surviving original cohort participants attended their 28th biennial examination | The Framingham Heart Study participants have been followed extensively across adulthood to collect detailed medical and social information. Study examined the extent that these adults report ACP, describe their preferences for care and reported use of advance directives, and examined how these factors relate to social support, illness burden, physical functioning, cognitive functioning, depressive symptoms, health perceptions, and previous health care use | Many very elderly adults still reside in community settings and are capable of making treatment decisions near the end of life. Most elders were able to state their preferences, and few appeared upset or bothered when asked about EOL. The majority of participants prefer comfort measures at the EOL, though many indicated that they would endure life-prolonging interventions and distressing health states to avoid death. Very few respondents reported having discussed their preferences with their providers. Overall 69% discussed their wishes for medical care at EOL with someone, but only 17% discussed their wishes with a physician or health care provider. Two-thirds had a health care proxy, 55% had a living will, and 41% had both. 80% respondents preferred comfort care over life-extending care, and 71% preferred to die at home, however fewer respondents said they would rather die than receive specific life-prolonging interventions (chronic ventilator 63% and feeding tube 64%). Many were willing to endure distressing health states, with less than half indicating that they would rather die than live out their life in a great deal of pain (46%) or be confused/forgetful (45%) all of the time. |
| Periyakoil (2017)80 Level 2 |
To compare the acceptability of the letter advance directive (LAD) to the traditional advance directive (TAD) of the state of California | Community; project link posted on the Letter Project portal and disseminated through social media outlets and electronic list services to recruit participants | n = 400 total participants; Intervention Letter directive: n = 216, age 40–49 n = 63, age 50–59 n = 62, age 60–69 n = 65, age 70–90 n = 26, Black or African American n = 31 (14.4%), Non-Hispanic White n = 69 (31.9%), Hispanic/Latino n = 74 (34.3%), Asian Americans n = 42 (19.4%); Traditional directive (control): n = 184, age 40–49 n = 66, age 50–59 n = 37, age 60–69 n = 53, age 70–90 n = 28, Black or African American n = 23 (12.5%), Non-Hispanic White n = 58 (31.5%), Hispanic/Latino n = 60 (32.6%), Asian Americans n = 43 (23.4%) | Quantitative; Web-based, randomized controlled trial; participants randomized to one of two types of advance directives: LAD or TAD; pilot testing showed average time to complete either form about 12 minutes | LAD available as online fillable document written at a fifth-grade level and available at the Letter Project portal. It is available in eight languages in print, as an interactive web-based form, an iOS application, and an Android application. The TAD (control) is available as an online fillable document written at a 12th grade reading level and is posted on the State of California's Department of Justice portal | In comparison of the LAD with the TAD document, it was found that participants preferred the letter as it is easy to read and understand and allowed patients to express what matters most to them, as well as their specific choices for treatments at the EOL. The LAD allows for a patient to customize the level of support desired and then describe the conditions under which such support should be discontinued. This flexible approach allows patients to express descriptive responses abut time-limited trials of specific treatments with end points, thus clarifying their wishes and preferences. LAD also offers guidance to the doctor on what to do in event the proxy fails to honor the patient's stated choices. A majority (89.4%) of the participants agreed or strongly agreed that they were more comfortable using the LAD compared to 72.8% for the TAD. |
| Ratner (2001)63 Level 4 |
To determine whether home health agency patients' preferences to die at home can be honored following a structed, professionally facilitated ACP process provided in the home | Community; large, urban home health agency owned by a not-for-profit integrated healthcare system; most discussed with patient and families occurred around the kitchen table | n = 84; median age 75, age range 37–94; 71% patients age 65 and older, 29% under 65; Female 51%; Not reported: ethnicity | Quantitative; Case series of patients who were identified by their home health agency nurses as having a life-limiting illness and then referred for social service assessment; Followed for at least 6 months, medial follow-up 191 days | Formally structured social work visits at patients' homes to discuss EOL issues, with communication of results to home health nurses and attending physicians. Social workers performed standard psychosocial assessments, obtained patient and family preferences regarding EOL care, and provided education about hospice services | Acceptance of ACP: 83 of 84 (99%) patients offered assistance with ACP agreed to discuss issues of EOL with the social workers. Timing of ACP: 58 (69%) of the patients had died by the end of follow-up. Preferences for location of EOL care: 54 (64%) cases expressed and documented a preference for location of EOL care. 46 (85% preferred care at home, with residential hospice preferred by three (6%) and nursing home preferred by 5 (9%). None of the patients expressing a preference wanted to die in the hospital. Location of death: of the 58 patients who died, 40 (70%) died at home and an additional three (5%) died in a home-like residential hospice. Use of hospice: of the 84 patients participating in the project, 51 (61%) had enrolled in hospice by the completion of the project. |
| Hawkins (2005)72 Level 4 |
To examine patients' and surrogates' attitudes about using advance directives to manage EOL medical care. To explore process preferences, or how patients want decisions to be made | Outpatient; 6 primary care practices in northeast Ohio; three in-home interviews with coparticipating surrogate decision makers | n = 337 patients: mean age 72.9; Female n = 190 (56%); White n = 311 (92%), Non-White n = 26 (8%); n = 337 surrogate decision makers: mean age 63.7; Female n = 227 (68%), White n = 310 (92%), Non-White n = 27 (8%); surrogates were primarily spouses or children of patients and had relationships that were both long (mean > 48 years) | Quantitative; 2-year Longitudinal study ADVANCE (Advance Directives, Values Assessment, and Communication Enhancement project) investigated psychological assumptions underlying the use of advance directives. The data used in present study came from third and final wave | interview structure focused on a way to redirect attention from patient preferences for specific life-sustaining treatments, which have most often been the focus of past research, and instead begin to examine individuals' metapreferences, or what is referred to as process preferences. Process preferences include individuals' wishes about whether and in what way they are interested in ACP, the amount of leeway they want surrogate decision makers to have in EOL decisions, and the people they want involved in the decision-making process | Very few individuals wished to document specific medical treatment preferences and mandate that they be followed without exception near death. Most desired more general preferences such as values and goals for care and to allow surrogate decision makers leeway in decision making. ”Having a dignified death” was the most highly endorsed value by both patients and surrogates. Study findings suggest that many patients do not desire to micromanage the course of medical treatment they receive at the end of life and that being encouraged to convey different types of information and preferences in advance directives may be advantageous. |
| Vandrevala (2002)51 Level 6 |
To investigate non-hospitalized older people's views about EOL care decision making. Examine older people's views on discussing ACP with their doctors and family members with particular reference to resuscitation and DNAR order | Community; United Kingdom | n = 12; mean age 70, age range 60–79; Female n = 6 (50%); Not reported: ethnicity | Qualitative; semi-structured interviews; conducted in the participant's home or at the university; interviews lasted about 1 hour | Interview explored patients' conceptualizations of decision-making in the later stages of life and the significant others they would like involved in the process. Topic of EOL introduced with questions about recent high profile legal cases, which were used to explore the participant's interest in issues of death and dying. Interview probes were used to explore the values that were important while talking or making decisions about EOL care | Three major categories emerged: 1) when participants would like to discuss EOL issues, 2) with whom they would like to discuss EOL issues and the issues or concerns raised when discussing these issues, 3) living wills as a means of effective communication. Concept of ‘right time’ was an important determinant of thinking and/or talking about EOL issues with emergence of 4 themes: chronological age vs mental age, fear vs. acceptance of dying, technology and reality of dying, and personal experience with death and illness. Older people wish to talk about their medical care in the later stages of life, because dying with dignity, maximizing quality of life and having autonomy and control over the dying process was important to them. Older people want to talk to their doctors and family members about their EOL issues. Older people maintained that doctors needed to accept the reality of death to be able to communicate EOL issues with their patients. Older people wished to talk to their family members as these were the individuals who really knew them and would ensure that their medical treatment was in accordance with their values. Communication between the older person, the doctor and the family takes place against the backdrop of contextual factors, namely the context of religious values and beliefs and the legislative and organizational factors that exist in society. |
| Thoresen (2016)19 Level 6 |
To examine how family involvement in ACP conversations can 1) contribute to identifying what is important to the nursing home patient at this point of life, and 2) promote the patients' participation in decisions on future treatment and EOL care | Long-term care; 8 nursing homes in Norway; spring 2014 | n = 7 ACP-conversations and participants; patient age range 80–100, Female n = 6 (85.7%); Not reported: ethnicity | Qualitative; Observational study; Participant observation of 7 ACP-conversations between nursing home staff, patients, and relatives; present study part of a larger research project, “End-of-life Communication in Nursing Homes, Patient Preferences and Participation” | ACP-conversation between nursing home staff, patients and/or relatives. Then conduct follow-up semi-structured interview that focused on the observed conversation and what had taken place | Three themes emerged: 1) patients and relatives are perceived as an intertwined unit, 2) relatives' involvement and participation in ACP-conversations is significant to get to know what is important in the patients' lives, and 3) families share experiences of dying and death. Including the patient's and the relatives' earlier experiences of dying and death in an ACP-conversation, can be a way of starting such a conversation, and can also contribute to understanding one's own life and dying as part of a larger narrative, and thus something which brings meaning. |
| Michael (2017)58 Level 6 |
To examine the awareness, attitudes, and experiences of ACP amongst older people and unrelated offspring/caregivers of older people residing in the community | Community; Australia | n = 42 total; Older people n = 15, age 55–64 n = 7, age 65–74 n = 5, age 75 + n = 3; Offspring/caregivers n = 27, age 18–34 n = 2, age 35–44 n = 1, age 45–54 n = 11, age 55–64 n = 8, age 65–74 n = 4, age 75+ n = 1; offspring/caregivers relation to older adult: Daughter n = 18, Partner n = 6, Son/son-in-law n = 2, Sister n = 1 | Qualitative; Descriptive, semi-structured question framework; 8 total focus groups between 5–7 participants conducted at meeting rooms at community health centers | Focus group questions focused on participants' understandings and views about ACP; related discussion or documentation experiences; future health concerns for themselves or those being cared for; and experiences related to planning future healthcare | Challenges faced by both older adults and their offspring/caregivers in contemplating ACP was recognized when the older adults is in the ‘gray zone’ of aging. Other themes including transitioning from independence to dependence, capacity to incapacity, ACP literacy and communication, and challenges contemplating mortality. The study's findings reinforce the importance of ACP and suggest ACP programs should accord with the ‘life-cycle model.’ This model proposes that aspects of ACP should occur throughout the continuum of the human life cycle. Discussions about life values and goals should commence at key life maturation point such as turning 18, being married or starting a family having children, and throughout primary health care in the community, and with a diagnosis of a serious illness and its progression. This process helps normalize ACP and reduces emotional burden that may arise in those who have not adequately prepared for making EOL care decisions. |
| Simon (2015)20 Level 6 |
To explore seriously ill, older hospitalized patients' and their family members' perspectives on the barriers and facilitators of ACP | Inpatient; 12 acute care hospitals in Canada | n = 503 respondents; n = 278 patients, mean age 80, Female 52.9%; n = 225 family members, mean age 60.8, 75.9% Female; Not reported: ethnicity | Qualitative; Descriptive study; Patients and family members were interviewed face-to-face separately and alone; Interviews took place between 48–120 hours after hospital admission | Interview questionnaire explored ACP activities during two time periods: before the current hospitalization and since the admission to hospital. Questions inquired about barriers and facilitators to communication about the patient's plan of care, prognosis and use of life-sustaining therapies, in the periods before and since hospitalization. Family members were asked about their wishes for the patient, not a proxy assessment of patient wishes | Most patients (76.3%) and families (81.7%) had thought about kinds of life-sustaining treatments desirable. Three major categories emerged: 1) the person (patient or family respondent attributes, 2) access to doctors and ACP resources and 3) the interaction between the doctor and the patient/family |
| Peck (2018)49 Level 6 |
To determine the barriers and facilitators to ACP engagement after discharge from hospital | Inpatient; General internal medicine teaching units in Ottawa, Ontario | N = 17; age range 57–89; Male (n = 9), female (n = 8) | Qualitative; semi-structured interviews at location of participant's choosing. Use of theoretical domain framework (TDF) | Discussion with patient using a conversation guide and then ACP workbook. Post-hospital interview explored patients' memory of the conversation in the hospital and any contemplation or ACP they engaged in since discharge from hospital. Interview questions explored how two parts of intervention (conversation & ACP workbook) acted as facilitators or barriers to ACP engagement | 12/14 TDF domains identified as barriers or facilitators. Social/professional identity and behavioral regulation were not identified. Facilitators: Knowledge, skills, beliefs about capabilities, memory attention and decision processes, beliefs about consequences, social influences, environmental context and resources, emotion, reinforcement, intention and goals Barriers: all except intention and goals. Optimism also a barrier. Admission to hospital was a catalyst that made ACP more relevant. Some people did not think timing right to discuss ACP and had no recollection of receiving information about ACP. Uncertainty about future health motivated some participants engage in ACP and others felt ACP discussions prevented them from living in the moment and stripped them of hope that better days were ahead. Hospital environment barrier with little privacy and roommates. |
| Taneja (2019)88 Level 6 |
To describe how lay people understand and make decisions for life-sustaining interventions when engaging in ACP | Community; Mid-size Canadian urban community |
N = 20; mean age 66; female 60%, male 40% N = 10 chosen for follow-up interviews, 4 months later |
Qualitative; semi-structured interviews using constructivist grounded theory methodology and purposive sampling | During interview, participants shown a document listing common life-sustaining interventions provided in a contemporary acute care hospital with a brief description of each interview and its implications Follow-up interviews asked about experience of ACP in intervening time after initial interview and rationale for changing preferences or decision conflicts. |
Four major themes identified: 1) lack of knowledge of life-sustaining interventions toward end of life, 2) confidence in substitute decision makers' ability to make the right decision in the future, 3) expression of preferences in terms of unacceptable functional outcomes rather than desired interventions and decision conflicts while articulating preferences Decision conflicts may serve as triggers for timely communication with health-care providers so that specific questions can be discussed and documented |
| Overbeek (2018)40 (JAGS) Level 2 |
To determine the effectiveness of ACP in frail older adults | Long term care; n = 16 residential care homes in Netherlands | N = 201 (n = 101 intervention, n = 100 control); mean age 86, range 75–102 (intervention), mean age 87, range 73–101 (control). Inclusion factor included being frail (Tilburg Frailty Index score ≥5, range 0–15) | Quantitative, Cluster RCT | Adjusted Respecting Choices ACP program 3 core elements: information provision through leaflets; facilitated ACP conversations based on scripted interview cards; and completion of an AD, including appointment of surrogate decision-maker |
No effect of ACP on degree of patient activation, quality of life, satisfaction with healthcare, or medical care use was found. There was an effect on completion of ADs 93% and appointment of surrogate decision-makers 94% in the intervention group compared with 34% completed an AD and 67% appointed a decision-maker |
| Overbeek (2018)40 Level 6 |
To investigate 1) how bereaved relatives of frail older patients experience ACP conversations and 2) whether ACP has an effect on relatives' preparation for decision-making and on their levels of anxiety and depression | Long-term care; 16 residential care homes; Netherlands | N = 101 intervention, N = 100 control; surveys conducted with 39/51 (76%) bereaved relatives | Mixed Methods; data collected in context of a randomized trial; mixed sample scheme where qualitative and quantitative data integrated into one interview | 3 months after death of patient, appointed relatives were sent an invitation for phone interview. Questions asked about how they had experienced the facilitated ACP conversation | Most bereaved relatives appreciated the facilitated ACP conversations which allowed for clarity concerning patients' preferences for medical treatment and care and facilitated healthcare decision-making. Among relatives who had been involved in decision-making, ACP had a positive effect on the perceived level of preparation for decision-making. ACP had no significant effect on levels of satisfaction, anxiety and depression |
| Tzeng (2019)95 Level 4 |
To examine the associations between older adults' demographic characteristics (age, sex, marital status, residential site, and educational level) and their perceived importance of four self-care actions for EOL planning, as well as their desire and ability to perform these actions | Community; living in southern United States | N = 123; age 65–75 48.8%; age 75–85 35.8%; age 85 + 15.4%; female 73.3% | Quantitative; cross-sectional; self-administered survey with Patient Action Inventory for Self-Care and demographics questionnaire | Examined planning for end of life care from three angles- importance, desirability, and ability to perform each of the previously defined EOL planning actions; Use of patient action inventory for self-care questionnaire where participants indicate yes or not for each action statement from three perspectives: (a) is this important to you? (b) do you want to do this? (c) are you able to do this? | Older adults less likely to have engaged in EOL planning were associated with not having a high school education being advanced in age, being married, and living in a rural area. These demographic characteristics are the social determinants of health among older adults in relation to developing an EOL care plan. |
| Nair (2019)42 Level 4 |
To determine if a video aimed at educating and engaging hospitalized patients on a standardized ACP order set can improve 1) inpatient understanding of key ACP concepts, 2) ACP documentation within 48 hours of hospital admission, 3) concordance between a patient's expressed and chart-documented care preferences, 4) patient satisfaction with decision-making, and 5) patient's decisional confidence | Inpatient; community-based. Hospital in British Columbia, Canada | N = 252; mean age 69.8 years; female 48% (n = 121) | Quantitative Prospective, non-randomized pre-post intervention study |
ACP-MOST video (13 minutes); Video content describes ACP and MOST form | ACP video improved patient understanding of key ACP concepts, rates of ACP documentation, and patient satisfaction with decision-making |
| Dignam (2019)85 Level 4 |
To compare 2011 and 2017 documentation of resuscitation decisions in older patients, including the frequency and clarity of documentation | Inpatient; teaching hospital in Australia | N = 130; mean 83 | Quantitative; chart retrospective review | The Resuscitation Plan 7-Step Pathway (the Pathway) and the Resuscitation Alert: 7-Step Pathway form (the Alert Form); The process of the pathway recommends that in response to any of the 5 specified clinical triggers, the treating team should consider creating an end-of-life clinical care plan in consultation with patient or substitute decision maker according to the patient's wishes, if these are documented on an advance directive | The structured pathway has improved frequency of documented discussion, the rate of recorded Not for CPR status, and clarity of documentation. |
| Shaw (2018)56 Level 6 |
To explore the readiness among these stakeholders and the factors that influence the degree of readiness in supportive living facilities | Long term care; assisted living facilities n = 4 in Canada | N = 27; 10 residents (9 female, 1 male; age range 72–86), 8 family members (8 female, age range 40–75), 9 health care practitioners (majority female & RNs, and nurse aides) | Qualitative; semi-structured interviews; interpretive description | Interview guide with patients, families, and clinicians | Themes that emerged that influence readiness for engagement in ACP discussions included the influence of prior experience for residents and family members, perception of treatment goals, and understanding of roles in the process between groups |
| Hinderer (2019)64 Level 4 |
To estimate the impact of a culturally tailored nurse-driven educational intervention on the relationship between attitudes toward ADs and AD completion and ACP discussions | Community; Chinese community center in metropolitan area of Washington, DC | Baseline n = 71, postintervention n = 72. Mean age 61.1, age range 32–87. Female 63.9%; 62.5% completing college of graduate school |
Quantitative; non-experimental pre-test post-test repeated measures | Nurse-led interactive, educational workshop conducted in both English and Mandarin that incorporated a culturally sensitive approach to ACP. Five Wishes booklet used. | Culturally tailored, community-based, nursing-driven approach to ACP had a positive influence on attitudes toward and completion of ADs in Chinese Americans. Involvement of nurses in current study highlighted that ACP is a shared responsibility among healthcare providers and clients and reinforced the concept of ACP engagement |
| Kim (2019)89 Level 4 |
To examine knowledge, attitudes and barriers/benefits regarding ADs and their associations with AD treatment preferences among chronically ill, low-income, community-dwelling older people. | Community; home visiting service for chronic disease management; South Korea | N = 112; mean age 74.9, range 60–89; female 83.9%, male 16.1% | Quantitative; Descriptive, correlational design |
Home visit nurses in part of a home visitation service. Incorporate ACP discussions while extending service to embrace ACP issues such as disease prognosis, goals of care, individual's health issues, needs, and preferences for medical care, and palliative concerns in addition to disease management | Different modifiable and non-modifiable factors were associated with each AD treatment preference. Several modifiable targets for interventions include perceived barriers to and benefits of ACP and knowledge of ADs. Non-modifiable demographic factors include marital status, education or having a CVD/stroke, as factors associated with aggressive treatment preferences |
| Cardona (2019)46 Level 4 |
To investigate views, determinants and barriers to end-of-life discussions for doctors, nurses and members of the public (MoP) and their acceptability of risk prediction tools | Community; Australia | N = 360 clinicians; 73.5% female; N = 497 MoP, 65.7% female, 75.4% aged ≥60 years | Quantitative; Cross-sectional |
Survey tailored specifically for clinicians and one for MoP | MoP with or without chronic illness feel strongly about knowing the truth and being involved in their treatment decisions. Older people appeared very ready to discuss EOL issues despite the clinicians' opinion that about half their terminal patients do not wish to know their own prognosis, belief that patients are not equipped with knowledge to make decisions and perception that families request for information to be withheld from patients |
| De Vleminck (2018)22 Level 6 |
(i) To describe to what extent patients aged 50 and older who are relatively stable or in good health are thinking about the end of life (EOL) and willing to discuss this with their family physician (FP) and (ii) to explore whether patients and FPs indicate the same topics as triggers for ACP discussions in family practice | Outpatient; family practice; Flanders, Belgium | N = 289 patients in survey; age 50–59 43%, age 60–69 27.5%, age 70–79 18.7%, age 80 + 10.9%; female 50.3%, male 48.6%; semi structured interviews patients n = 5, family physicians n = 5 | Mixed-methods; cross-sectional | Patient questionnaire and qualitative interview guide | Majority of patients thought about EOL (69.8%) and would appreciate if their FP would initiate a conversation about this (75.9%); Qualitative- 4 interrelated themes captured thoughts of people aged ≥ 50 years according to patients and FP: 1) care dependency, 2) physical and mental deterioration at the EOL, 3) dying alone, 4) having the paperwork in place |
| Sudore (2018)44 Level 2 |
To compare the efficacy of PREPARE plus an easy-to-read advance directive with an advance directive alone to increase advance care planning documentation and patient-reported engagement | Outpatient; 4 safety-net, primary-care clinics San Francisco | N = 986; mean age 63.3; female n = 603, male n = 383; 39.7% had limited health literacy; 45.1% Spanish speaking | Quantitative; comparative efficacy RCT | Easy-to-read AD and patient-directed, interactive, online ACP program in English and Spanish called PREPARE For Your Care. Intervention: online PREPARE program plus AD. Control: AD-only intervention | Patient-facing tools (PREPARE + easy to read AD) may enable diverse populations to engage in ACP process without additional clinician-level or system-level interventions |
| Chu (2018)33 Level 4 |
To evaluate a program to systematically conduct advance care planning (ACP) communication for hospitalized patients in Taiwan and identify the factors associated with AD completion | Inpatient; Taipei City Hospital in Taiwan | N = 1411; mean age 78.2; female 43.8%, male 56.2% | Quantitative; Retrospective evaluation of ACP program |
Healthcare provider trained in ACP. ACP meeting held with healthcare provider (physician, nurse, social worker), patients, family | With ACP communication, overall rate of AD completion was 82.6%. Social workers may play an important role for ACP communication with patients |
| Shaku (2019)76 Level 4 |
The aim of this study was to examine the preferences of home caregivers on patient advance care planning (ACP), including life-sustaining treatment (LST) and the factors relating to these preferences | Community; Japan | N = 309 caregivers (110 males, 199 females); mean age 65.29 | Quantitative; Cross-sectional |
Self-written questionnaire for caregivers included items on caregiver demographics, care duration, comprehension level of a doctor's explanations regarding his or her patient's condition, patients' diseases, whether a caregiver has or has not told his or her parents about their disease, level of nursing care, and LST preference | More than half of caregivers were not sure of their patient's LST. Sex, number of people living together in care home, care duration, comprehension of level of doctor's explanations found to be significant factors relating to caregivers' LST preference. Health care providers should be aware of background factors relating to caregiver ACP preferences when making decisions on LST |
| Schubart (2018)75 Level 6 |
To characterize post-ACP conversations regarding medical wishes between seriously ill patients and their family caregivers | Community; northeastern region of United States | N = 188 caregivers; mean age 56.7; 74.5% female | Qualitative; semi-structured interviews conducted 4–6 weeks after ACP | Interviews conducted to elucidate the subsequent communications regarding medical wishes. If no conversations post-ACP held, reasons and barriers explored | Weeks after ACP event, majority of patient-family caregiver dyads had a few short conversations mostly about patients' general quality of life issues and medical treatments desired or not under specific scenarios. If they did not have conversation, most often due to feeling that conversation not needed as previously discussed topic. |
| Groebe (2019)59 Level 6 |
To get insights into specific requirements and conditions for communication about the end of life in various end-of-life care settings | Mixed: outpatient, inpatient, and long-term care; Germany | N = 18 participants, female n = 16, male n = 2; professional staff and hospice volunteers from 1 outpatient hospice service, 1 inpatient palliative care unit in a hospital, and 2 inpatient nursing homes | Qualitative; 4 focus groups | Semi structured interview guideline addressing personal experiences (how and when experiences take place), requirements and conditions (what enables or disables conversations about death and dying), and need for tools (do you think tools can help to assess attitudes, preferences, wishes, and worries toward EOL of people in EOL care settings) | 4 main themes: 1) communicating about the EOL: experiences in different care settings, 2) EOL topics in conversations, 3) requirements and conditions of daily care practice for EOL conversations, 4) usefulness of tools |
| Lum (2018)96 Level 2 |
The objective of the study was to compare the effects of an easy-to-read AD versus an ACP web site plus the AD (PREPARE + AD) on Behavior Change Processes and Actions, including discussions and documentation | Outpatient; 4 safety-net, primary-care clinics San Francisco | N = 414 participants; n = 205 intervention, n = 209 control; mean age 71.1; female 9%; 43% nonwhite | Quantitative; secondary data from a completed ACP RCT | PREPARE + AD. Use of ACP Engagement Survey which includes 57 behavior change ACP “process” measures and 25 ACP “action” measures at baseline, one week, 3 months, and 6 months after enrollment | PREPARE + AD resulted in greater increases in all behavioral change processes subscales and actions related to decision makers, quality of life, and flexibility. PREPARE + AD and AD only increased ACP engagement in a full range of ACP behaviors, including discussions and documentation, and engagement nearly 100% with PREPARE + AD |
| Sable-Smith (2018)24 Level 4 |
To identify factors associated with completion of Advance Care Planning (ACP) by patients seen in primary care in developed countries | Community; Multiple countries: 11 (Australia, Canada, France, Germany, Netherlands, New Zealand, Norway, Sweden, Switzerland, USA, UK) | N = 25,550, mean age 68.2, male 42.6% | Quantitative; analysis from the 2014 Commonwealth Fund International Health Policy Survey of Older Adults in 11 Countries | Survey consists of computer-assisted telephone interviews. 3 survey questions address ACP activities: discussion about wishes with family/friend/health care professional, written plan or document, or written name of surrogate decision maker | ACP seems to occur when a person is in closer proximity to mortality, through age and multimorbidity, and interacting with the healthcare system, either directly through hospitalization or while serving as an informal caregiver |
| DePriest (2019)84 Level 4 |
To determine whether acute care providers would find our pilot living will more helpful when caring for their older adult patients | Inpatient; those working in acute care/intensive care; United States | N = 126 providers representing 39 states; convenience sample of members of the Society of Hospital Medicine (n = 118 physicians, n = 5 ACNP, n = 4 PA) | Quantitative; survey | Pilot living will designed for those with end-stage medical conditions (ESMC). Elements include: 1) overview of when living wills are used, definitions of ESMC and persistent vegetative state, and discussion about potentially reversible acute illnesses, 2) review of different levels of care, 3) checklist of primary focus on potentially reversible acute medication conditions across four different quality of life, 4) a separate checklist scenario for permanent unconsciousness | 86% indicated pilot living will helped them understand their patients' general EOL preferences, 87.5% indicated pilot living will would be more helpful in making specific treatment decisions for their patients, 85% indicated pilot living will would better facilitate EOL discussions with surrogates |
| David (2018)97 Level 4 |
To determine whether patient activation is associated with ACP | Outpatient; primary-care clinic at San Francisco Veterans Affairs Medical Center | N = 414; Veterans; mean 71.1; 9.2% women | Quantitative; cross-sectional | Survey; ACP engagement, Patient activation measure | Higher patient activation to manage one's overall healthcare is associated with higher engagement in ACP |
| Abdul Razzak (2019) Level 4 |
To quantify agreement between patients and their family members on their own values and preferences for use or non-use of life-sustaining treatments for the patient | Inpatient; 16 Canadian hospitals | N = 323 patient-family member dyads; patient: mean age 80, female 56.4%; family member mean age 62, female 73.6%; Clinical Frailty Scale used | Quantitative; cross-sectional | Questionnaire with eight items that ask participants to rate the importance they place on specific values related to the use of life-sustaining treatment. Family members then asked to indicate their own values, rather than predicting the patient's values | Moderate agreement between patients and family members with respect to values and preferences for life-sustaining treatment, beyond CPR preferences alone. In exploratory multivariate analysis, spousal relationships, higher patient education level and frailty are predictive of patient-family agreement in preferences |
| Torke (2019)23 Level 4 |
To determine whether the intervention could be feasibly implemented within the GRACE CCM program | Community; complex care management program in Midwestern urban hospital; GRACE = Geriatrics Resources for Assessment and Care of Elders | N = 18; mean age 77.8; 77.8% female; 66.7% African American, 33.3% White | Quantitative; single-arm feasibility study | GRACE clinicians trained in Respecting Choices Last Steps model. POLST facilitation visit conducted in patient's home with GRACE staff. GRACE clinician completed note in EMR and contacted patient's primary care provider. Form then scanned in EMR. Follow-up interview conducted by research team 4–6 weeks after enrollment to assess outcomes related to decision quality and experience | It was found feasible to deliver POLST facilitation by nonphysicians to frail older adults and their surrogates in a complex care management setting, leading to an increase in POLST form completion and availability in the medical record |
| Hold (2019)83 Level 4 |
To explore the success of advanced care planning at a large, rural long-term care (LTC) facility | Long-term care; Rural setting in Northwest region of the state of Georgia; 182 bed facility | N = 167 residents; age range 54–101; female 85.1%; 88.1% Caucasian, 7.1% African Americans | Quantitative; descriptive, retrospective chart review | Resident preference for life-sustaining treatment (RPLST). For residents who do not have formal prepared AD documents, RPLST serves to define resident and family choices for resuscitation and implementation of fluids, nutrition, medications, and antibiotics | Completion rate of EOL preferences of 86.7% within 100 days of being admitted to the nursing home. Within 10 days of admission, 76.7% completed RPLST. Form helped to create and sustain a supportive culture toward talking about death and dying starting at the admission process |
| Brungardt (2019)92 Level 4 |
To increase ACP outcomes by engaging older adults through portal-based ACP tools, including an electronic Medical Durable Power of Attorney (MDPOA) form | Outpatient; Primary care geriatric clinic in Colorado | N = 105; mean 77.7; female 64% | Quantitative | Portal-based electronic message and mailed postcard. ACP tools implemented into My Health Connection, the health system's patient portal integrated with Epic EHR. Motivational message sent to eligible patients about importance of health care decision maker and their lack of POA in EHR, instructions for assessing the portal-based ACP tools, and contact information for the centralized ACP support team for questions | Portal-based messages about ACP are feasible and may increase ACP outcomes for older adults in primary care |
| Mirarchi (2019)98 Level 4 |
To determine 1) whether do-not-resuscitate (DNR) orders created upon hospital admission or Physician Orders for Life-Sustaining Treatment (POLST) are consistent patient preferences for treatment and 2) patient/health care agent (HCA) awareness and agreement of these orders | Inpatient; Pennsylvania hospital | N = 101; mean age 76; female 55%; 85% white; Patients were assessed for frailty based on validated clinical scoring algorithm | Quantitative | Patients with capacity of healthcare agents interviewed to determine their knowledge and awareness of DNR orders (hospital DNR or POLST) | DNR and POLST orders can be inaccurate, undisclosed, and discordant with patient wishes for medical care. In 25% of cases, patients/HCAs were unaware of the DNR order, 50% were unsure of their prognosis, and another 40% felt their condition was not terminal. 44% of time, the existing DNR and POLST were discordant with patient wishes and 38% were rescinded |
| Bose-Brill (2018)91 Level 2 |
To determine its impact on frequency and quality of advance care planning documentation | Outpatient; 2 primary-care clinics; United States | N = 419 participants (control = 219, intervention = 200) | Quantitative; pragmatic trial | Use of open-ended ACP framework (4 questions) sent to EHR patient portal | ACP documentation rates increased by 105% (19/39 to 39/39) and quality improved among all patients who engaged in the previsit planning framework (n = 39) |
| Kastbom (2019)65 Level 6 |
To investigate clinicians' perspectives on the factors that shape the process of advance care planning in a nursing home context | Long term care; 9 nursing homes in Sweden | N = 25; physicians n = 14, nurses n = 11 | Qualitative; interviews | Interviews with healthcare providers. Interview guide developed with open questions about ACP | 4 categories: 1) exploration of preferences and views, 2) integration of preferences and views, 3) decision and documentation of the ACP, 4) implementation and re-evaluation of the ACP. Latent theme, establishing beneficence- defending oneself against tacit accusations of maleficence, emerged as a deeper meaning of all four parts of the ACP process |
| Paiva (2019)55 Level 2 |
To determine the feasibility of conducting a cluster randomized controlled trial providing individualized feedback reports to increase advance care planning (ACP) engagement in the primary care setting | Outpatient; two primary-care practices; United States | N = 38 intervention; n = 42 control | Quantitative, pilot cluster RCT; Use of Sharing and Talking About My Preferences (STAMP) program | Brief assessment of readiness to engage (stages of change) for 3 ACP behaviors (healthcare agent assignment, communication with agent about quality vs quantity of life, living will completion) generating an individual feedback report and stage-matched brochure | Feasibility of intervention delivered in clinical practice to provide print-tailored feedback materials with goal of increased engagement in ACP was achieved. Challenges in recruitment identified |
| Zapata (2018)78 Level 4 |
To assess the feasibility and impact of a video-based website to facilitate GVs to engage diverse adults in ACP | Outpatient; 2 primary-care clinics in Northern California safety-net setting | N = 22; mean age 64; 55% female; 73% racial or ethnic minorities | Quantitative; feasibility pilot study | Group visit and PREPARE. Participants attended 2 90minute group visits and viewed the five steps of the movie version of the PREPARE website. | Using PREPARE in group visit setting to facilitate ACP for diverse adults in safety-net primary care setting was feasible and improved ACP engagement. Participants showed improved knowledge, confidence, and readiness about ACP topics and took steps toward designating a decision maker and completing an AD |
| Peterson (2019)38 Level 4 |
To examine racial, ethnic, and other factors associated with whether older adults discussed their end-of-life (EOL) care wishes with family | Community; participants taken from six senior centers, senior service organizations, housing complexes in 5-county area of Florida | N = 364; mean age 72; female 75%; White, non-Hispanic 61%, African American 26%, Hispanic 13% | Quantitative; cross-sectional | Structured questionnaire with questions on discussion of one's end of life care preferences with family vs having not done so, demographics, family involvement in health-care decision-making, support in decision making, health literacy, and religiosity | Knowing the involvement of patients' family/friends could help providers initiate end of life care discussions. |
| Bravo (2018)71 Level 2 |
To investigate how confidence in surrogates' ability to make consistent decisions in the future change over time, in the context of an ACP intervention that did not improve surrogates' ability to predict an older adult's hypothetical treatment preferences | Community; Canada |
N = 235; mean age 77; female 46%, male 54% | Quantitative; RCT (Bravo 201662) | Experimental group- 1) home visit by SW for older adult to reflect on and communicate their personal values, beliefs and wishes regarding future health care to their surrogates, 2) group information session on purposes, uses, practical limitations of recording healthcare wishes in an advance directive, 3) second home visit by same SW who checked participants' understanding of the information delivered during the group session, provided clarification as required, and assisted interested older adult in documenting their wishes. Control group- three nurse-led interactive workshops promoting healthy behaviors (ACP not discussed) | ACP increases older adults' confidence in their surrogates' predictive ability. Surrogates' rating of their own ability to make concordant decisions for their loved ones also increased. |
| Hunter (2018)74 Level 4 |
To determine how frequently the default surrogate decision maker (SDM) matched the patient's preferred SDM, and whether patients knew who would serve as their SDM should they become incapacitated | Outpatient; preoperative assessment, consultation, and treatment clinic; United States | N = 474; female 59.9%, male 40.1% | Quantitative; cross-sectional | Survey asking about relationship of patient to his/her next of kin, patient's beliefs as to who would be allowed to make decisions on his/her behalf if become incapacitated, and whom patient would prefer to make decisions if needed | 18% of patients believed someone other than next of kin would be asked to make decisions; 20.3% participants and 9.3% married participants, identified someone other than their next of kind as their preferred surrogate decision maker. Encouragement of designation of healthcare proxy is important in order to result in a greater change of following the patient's wishes for medical treatment |
Appendix III. Categories, Themes, Definitions and Descriptors of Factors Influencing Uptake of ACP in Older Adults
Enhanced Communication
| Building Relationship: Establishment of Connection and a Bond Between Two or More Parties | |
|---|---|
| Study | Themes |
| Malcomson (2009)50 |
|
| Fried (2017)52 |
|
| Simon (2015)20 |
|
| Vandrevala (2002)51 |
|
| Shared Decision-Making: a Process Where Patients and Clinicians Work Together to Make Decisions | |
|---|---|
| Study | Themes |
| Boerner (2013)30 |
|
| Gjerberg (2015)53 |
|
| Romo (2017)47 |
|
| Piers (2013)54 |
|
| Stages of Change in Readiness: Series of Stages Involved in Behavior Modification. Underlying Theoretical Foundation in the Transtheoretical Model, which Recognizes Change as a Process that Unfolds over Time, Involving Progress through a Series of Stages | |
|---|---|
| Study | Themes |
| Simon (2015)20 |
|
| Shaw (2018)56 |
|
| Paiva (2019)55 |
|
| Framing of the Discussion: Underlying Creation of Structure or Foundation that ACP Discussion can be Built Around | ||
|---|---|---|
| Study | Factor | Themes |
| Chan (2010)43 |
|
|
| Detering (2010)57 & Michael (2017)58 |
|
|
| Groebe (2019)59 |
|
|
| Empathy: The Integration of Compassion, Care, and Establishment of Rapport When Conducting ACP Discussions | |
|---|---|
| Study | Themes |
| Barnes (2007)60 |
|
| Simon (2015)20 |
|
| Peck (2018)49 |
|
| Techniques/Style: Unique Style That ACP Discussion is Built Around | |
|---|---|
| Pollak (2015)21 | Motivational interviewing |
| |
| |
| Honest/Frank Discussion: Being Straightforward, Sincere, and Truthful in Discussion | |
|---|---|
| Study | Themes |
| Romo (2017)47 |
|
| Abdul-Razzak (2014)48 |
|
| Simon (2015)20 |
|
| Peck (2018)49 |
|
| Cardona (2019)46 |
|
Provider Role and Preparation
| Interdisciplinary Roles: Trained Clinicians With a Defined Role Aimed at Advance Care Planning (ACP) Processes and/or Documentation | ||
|---|---|---|
| Study | Clinician | Role |
| Cheang (2014)66 | Residents in geriatric medicine | Invitation to participate in an ACP screening interview |
| Chu (2018)33 | Healthcare providers | Lead an ACP meeting to discuss patients' treatment and preferences |
| Ratner (2001)63 | Social workers | Discussion of preferences regarding EOL |
| Pearlman (2005)39 | Social workers | Facilitation of a multifaceted intervention (Your Life, Your Choices) |
| Bravo (2016)62 | Social workers | Facilitation of a multifaceted intervention (home visits, My Preferences booklet) |
| Kastbom (2019)65 | Nurses and Physicians in LTC setting | Exploring preferences and views early and re-evaluation |
| Torke (2019)23 | Advance Practice Registered Nurse & Social worker | Conversation following Respecting Choices model |
| Hinderer (2019)64 | Nurses in community settings | Nurse-led interactive educational workshop |
| Chan (2010)43 | Trained nurse facilitator within LTC setting | “Let Me Talk” program & interview guide |
| Groebe (2019)59 | Nursing home staff | Communication about end of life (EOL), “conversation partner” |
| Training: Completion of Formalized Educational Learning and Utilization of Trained Facilitators of ACP | ||
|---|---|---|
| Study | Content | Themes |
| Detering (2010)57 |
|
Use of a coordinated, systematic model of patient centered ACP using nonmedical ACP facilitators |
| Overbeek (2018)40 |
|
Nurses used as trained facilitators |
| Torke (2019)23 |
|
GRACE clinicians trained in Respecting Choices Last Steps model. Use open-ended questions to explore values and lead discussion about POLST form |
| Chu (2018)33 |
|
Didactic and simulation training on terminal illness, emotional support, communication skills, patients' rights regarding advance directives |
| Provider Awareness of Readiness: Having Understanding of Patients/Families Desire to Engage in Conversation About EOL | ||
|---|---|---|
| Study | Factor | Themes |
| Braun (2014)67 | Decision making styles
|
Types of decision-makers:
|
| Abdul-Razzak (2014)48 |
|
|
| Thoresen (2016)19 |
|
|
| Cheang (2014)66 |
|
|
| Chiu (2016)36 |
|
|
| Kastbom (2019)65 |
|
|
| Cardona (2019)46 |
|
|
| De Vleminck (2018)22 |
|
|
| Family Physician/Long-Standing Relationship: Longitudinal Doctor/Patient Relationships That Promote Trust, Coordination, and Continuity of Care | |
|---|---|
| De Vleminck (2018)22 | Themes that prompt conversations:
|
Patient/Family Relationship Patterns
| Family Dynamics: Recognition of the Role of Families | |
|---|---|
| Study | Themes |
| Karasz (2010)68 |
|
| Fried (2017)52 |
|
| Van Eechoud (2014)69 |
|
| Thoresen (2016)19 |
|
| Michael (2017)58 |
|
| McCarthy (2008)29 |
|
| Boerner (2013)30 |
|
| Detering (2010)57 |
|
| Family Involvement in Health-Care Decision-Making: Taking Family into Account for Decision-Making | |
|---|---|
| Study | Themes |
| Overbeek (2019)70 |
|
| Peterson (2019)38 |
|
| Role of Caregiver & Surrogate Decision-maker: Identifying a Person Close to the Patient Who Also May Step in to a Decision-making Role for the Patient | |
|---|---|
| Study | Themes |
| Shaku (2019)76 |
|
| Volandes (2009)25 |
|
| Fried (2017)52 |
|
| Hawkins (2005)72 |
|
| Schubart (2018)75 | After ACP event:
|
| Abdul-Razzak (2019)73 |
|
| Bravo (2018)71 |
|
| Hunter (2018)74 |
|
Standardized Processes and Structured Approaches
| Visual Aids: Visual Items that Contribute to the Understanding of a Concept in Addition to Spoken Word | ||
|---|---|---|
| Study | Specific Visual Aid | Usage |
| Seymour (2003)79 |
|
|
| Chan (2010)43 |
|
|
| Volandes (2009)25 |
|
|
| Volandes (2016)41 |
|
|
| Bravo (2016)71 |
|
|
| Pearlman (2005)39 |
|
|
| Lankarani-Fard (2010)77 |
|
|
| Zapata (2018)78 |
|
|
| Peck (2018)49 |
|
|
| Nair (2019)42 |
|
|
| Hinderer (2019)64 |
|
|
| Sudore (2018)44 |
|
|
| Paiva (2019)55 | Individualized feedback report |
|
| Template/Document: Structured Form to Document ACP | ||
|---|---|---|
| Study | Form Name | Description |
| Almack (2012)86 |
|
|
| Brimblecombe (2014)81 |
|
|
| Silvester (2013)82 |
|
|
| Periyakoil (2017)80 |
|
|
| Hold (2019)83 |
|
|
| DePriest (2019)84 |
|
|
| Dignam (2019)85 |
|
|
| Torke (2019)23 |
|
|
| Prompts, Patient Electronic Messaging: Use of Electronic Nudges to Convey Information Through Electronic Health Record (EHR) | |
|---|---|
| Study | Description |
| Tieu (2017)26 |
|
| Brungardt (2019)92 |
|
| Bose-Brill (2018)91 |
|
| Staged Discussion: Consideration of the Frequency or Extent of Time Involved in ACP, and the Timing of a Discussion | ||
|---|---|---|
| Study | Factor | Themes |
| Barnes (2007)60 |
|
|
| Michael (2017)58 |
|
|
| Simon (2015)20 |
|
|
| Bravo (2016)62 |
|
|
| Taneja (2019)88 |
|
|
| Tan (2019)87 |
|
|
| Sable-Smith (2018)24 |
|
|
| Format: Underlying Structure and Layout in Introduction of ACP | ||
|---|---|---|
| Study | Structure | Description |
| Barnes (2007)60 |
|
|
| Lum (2016)90 |
|
|
| Zapata (2018)78 |
|
|
| Hinderer (2019)64 |
|
|
| Kim (2019)89 |
|
|
Patient Contextual Factors
| Decision Control Preferences: Understanding One's Desire for Control in Decision-Making | |
|---|---|
| Study | Themes |
| Braun (2014)67 |
|
| Romo (2017)47 |
|
| Chiu (2016)36 |
|
| Simon (2015)20 |
|
| Hawkins (2005)72 |
|
| Piers (2013)54 |
|
| Gjerberg (2015)53 |
|
| Taneja (2019)88 |
|
| Values: Use of Characteristic Traits Representative of One's Personhood or Belief System | ||
|---|---|---|
| Value | Study | Usage |
| Values (in general) | Schonwetter (1996)99 Winter (2013)100 Lankarani-Fard (2010)77 |
|
| Religiosity/spiritua lity | Hawkins (2005)72 Garrido (2013)35 Simon (2015)20 Vandrevala (2002)51 |
|
| Control | Barnes(2007)60 Piers (2013)54 Vandrevala (2002)51 |
|
| Dignity | Abdul-Razzak (2014)48 Vandrevala (2002)51 Winter (2013)100 Hawkins (2005)72 |
|
| Autonomy | Vandrevala (2002)51 Hawkins (2005)72 |
|
| Comfort | Seymour (2003)79 Winter (2013)100 Hawkins (2005)72 |
|
| Burden | Seymour (2003)79 Winter (2013)100 |
|
| Demograghics Characteristics: Representative Personal Traits that Were Influential in the Uptake of ACP Through Statistical Analysis | ||
|---|---|---|
| Characteristic | Study | Description |
| Age |
|
|
| Gender |
|
|
| Race/ethnicity |
|
|
| Marital status |
|
|
| Education |
|
|
| Place of residence |
|
|
| Other Characteristics: Additional Characteristics that Were Influential in the Uptake of ACP | ||
|---|---|---|
| Characteristic | Study | Description & Themes |
| Perceived health |
|
|
| Spirituality |
|
|
| Frailty |
|
|
| Social determinants |
|
|
| Culturally sensitive |
|
|
| Behavioral: Engagement Patient Activation Perception |
|
|
| Attitudinal differences |
|
|
Missed Communiation
| Uncomfortable Stage: Generalized Experience of Something Being Difficult, Awkward, or Distressing | |
|---|---|
| Study | Themes |
| Piers (2013)54 |
|
| Almack (2012)86 |
|
| Michael (2017)58 |
|
| Simon (2015)20 |
|
| Kastbom (2019)65 |
|
| Schubart (2018)75 |
|
| Lack of Communication/Ineffective: The Absence of Discussion or the Inadequate Nature of the Discussion | |
|---|---|
| Study | Themes |
| Simon (2015)20 |
|
| Heyland (2013)102 |
|
| Towsley (2015)103 |
|
| Gjerberg (2015)53 |
|
| De Vleminck (2018)22 |
|
| Lack of Documentation: Missing, Incomplete, or absent Written ACP Information | |
|---|---|
| Study | Themes |
| Heyland (2013)102 |
|
| Wu (2008)37 |
|
| Discordance Documentation: Information that is Written down that may be Incorrectly Documentated or in Disagreement With Patient's Wishes | |
|---|---|
| Study | Themes |
| Mirarchi (2019)98 |
|
| Kastbom (2019)65 |
|
| Heyland (2013)102 |
|
References
- 1.Brinkman-Stoppelenburg A., Rietjens J.A.C., van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28:1000–1025. doi: 10.1177/0269216314526272. [DOI] [PubMed] [Google Scholar]
- 2.Morrison R.S. Research priorities in geriatric palliative care: an introduction to a new series. J Palliat Med. 2013;16:726–729. doi: 10.1089/jpm.2013.9499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Figueroa J.F., Joynt Maddox K.E., Beaulieu N., Wild R.C., Jha A.K. Concentration of potentially preventable spending among high-cost medicare subpopulations: an observational study. Ann Intern Med. 2017;167:706–713. doi: 10.7326/M17-0767. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine . The National Academies Press; Washington, DC: 2015. Dying in America: Improving quality and honoring individual preferences near the end of life. [PubMed] [Google Scholar]
- 5.Lewis E., Cardona-Morrell M., Ong K.Y., Trankle S.A., Hillman K. Evidence still insufficient that advance care documentation leads to engagement of healthcare professionals in end-of-life discussions: a systematic review. Palliat Med. 2016;30:807–824. doi: 10.1177/0269216316637239. [DOI] [PubMed] [Google Scholar]
- 6.Mignani V., Ingravallo F., Mariani E., Chattat R. Perspectives of older people living in long-term care facilities and of their family members toward advance care planning discussions: a systematic review and thematic synthesis. Clin interventions Aging. 2017;12:475. doi: 10.2147/CIA.S128937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Caoimh R., Cornally N., O'Sullivan R., et al. Advance care planning within survivorship care plans for older cancer survivors: a systematic review. Maturitas. 2017;105:52–57. doi: 10.1016/j.maturitas.2017.06.027. [DOI] [PubMed] [Google Scholar]
- 8.Nishikawa Y., Hiroyama N., Fukahori H., et al. Advance care planning for adults with heart failure. Cochrane Database Syst Rev. 2020:CD013022. doi: 10.1002/14651858.CD013022.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharp T., Moran E., Kuhn I., Barclay S. Do the elderly have a voice? Advance care planning discussions with frail and older individuals: a systematic literature review and narrative synthesis. Br J Gen Pract. 2013;63:e657–e668. doi: 10.3399/bjgp13X673667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ke L.-S., Huang X., Hu W.-Y., O'Connor M., Lee S. Experiences and perspectives of older people regarding advance care planning: a meta-synthesis of qualitative studies. Palliat Med. 2017;31:394–405. doi: 10.1177/0269216316663507. [DOI] [PubMed] [Google Scholar]
- 11.Weathers E., O'Caoimh R., Cornally N., et al. Advance care planning: a systematic review of randomised controlled trials conducted with older adults. Maturitas. 2016;91:101–109. doi: 10.1016/j.maturitas.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 12.Hopkins S., Bentley A., Phillips V., Barclay S. Advance care planning with frail older patients in the acute hospital setting: a systematic review. BMJ Support Palliat Care. 2020;10:164–174. doi: 10.1136/bmjspcare-2019-002093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Uptake. In Merriam-Webster.com. Available at: Accessed August 19, 2020.
- 14.Sudore R.L., Lum H.D., You J.J., et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manage. 2017;53:821–832.e1. doi: 10.1016/j.jpainsymman.2016.12.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whittemore R., Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52:546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 16.Melnyk B.M., Fineout-Overholt E. Lippincott, Williams & Wilkins; Philadelphia: 2011. Evidence-based practice in nursing and healthcare: A guide to best practice. [Google Scholar]
- 17.Mays N., Pope C., Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005;10:6–20. doi: 10.1258/1355819054308576. [DOI] [PubMed] [Google Scholar]
- 18.Joanna Briggs Institute Critical Appraisal Tools. 2017. http://joannabriggs.org/research/critical-appraisal-tools.html Available from.
- 19.Thoresen L., Lillemoen L. “I just think that we should be informed” a qualitative study of family involvement in advance care planning in nursing homes. BMC Med Ethics. 2016;17:72. doi: 10.1186/s12910-016-0156-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simon J., Porterfield P., Bouchal S.R., Heyland D. ‘Not yet’ and ‘Just ask’: barriers and facilitators to advance care planning—a qualitative descriptive study of the perspectives of seriously ill, older patients and their families. BMJ Support Care Palliat Care. 2015;5:54–62. doi: 10.1136/bmjspcare-2013-000487. [DOI] [PubMed] [Google Scholar]
- 21.Pollak K.I., Jones J., Lum H.D., et al. Patient and caregiver opinions of motivational interviewing techniques in role-played palliative care conversations: a pilot study. J Pain Symptom Manage. 2015;50:91–98. doi: 10.1016/j.jpainsymman.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Vleminck A., Batteauw D., Demeyere T., Pype P. Do non-terminally ill adults want to discuss the end of life with their family physician? An explorative mixed-method study on patients' preferences and family physicians' views in Belgium. Fam Pract. 2018;35:495–502. doi: 10.1093/fampra/cmx125. [DOI] [PubMed] [Google Scholar]
- 23.Torke A.M., Hickman S.E., Hammes B., et al. POLST facilitation in complex care management: a feasibility study. Am J Hosp Palliat Care. 2019;36:5–12. doi: 10.1177/1049909118797077. [DOI] [PubMed] [Google Scholar]
- 24.Sable-Smith A., Arnett K.R., Nowels M.A., et al. Interactions with the healthcare system influence advance care planning activities: results from a representative survey in 11 developed countries. Fam Pract. 2018;35:307–311. doi: 10.1093/fampra/cmx113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volandes A.E., Mitchell S.L., Gillick M.R., Chang Y., Paasche-Orlow M.K. Using video images to improve the accuracy of surrogate decision-making: a randomized controlled trial. J Am Med Directors Assoc. 2009;10:575–580. doi: 10.1016/j.jamda.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tieu C., Chaudhry R., Schroeder D.R., et al. Utilization of patient electronic messaging to promote advance care planning in the primary care setting. Am J Hosp Palliat Care. 2017;34:665–670. doi: 10.1177/1049909116650237. [DOI] [PubMed] [Google Scholar]
- 27.Ioannidis J.P., Haidich A.-B., Pappa M., et al. Comparison of evidence of treatment effects in randomized and nonrandomized studies. JAMA. 2001;286:821–830. doi: 10.1001/jama.286.7.821. [DOI] [PubMed] [Google Scholar]
- 28.Concato J., Shah N., Horwitz R.I. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342:1887–1892. doi: 10.1056/NEJM200006223422507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCarthy E.P., Pencina M.J., Kelly-Hayes M., et al. Advance care planning and health care preferences of community-dwelling elders: the Framingham Heart Study. J Gerontol Ser A: Biol Sci Med Sci. 2008;63:951–959. doi: 10.1093/gerona/63.9.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boerner K., Carr D., Moorman S. Family relationships and advance care planning: do supportive and critical relations encourage or hinder planning? J Gerontol Ser B: Psychol Sci Social Sci. 2013;68:246–256. doi: 10.1093/geronb/gbs161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chu L.-W., Luk J.K.H., Hui E., et al. Advance directive and end-of-life care preferences among Chinese nursing home residents in Hong Kong. J Am Med Dir Assoc. 2011;12:143–152. doi: 10.1016/j.jamda.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 32.Luck T., Rodriguez F.S., Wiese B., et al. Advance directives and power of attorney for health care in the oldest-old – results of the AgeQualiDe study. BMC Geriatr. 2017;17:85. doi: 10.1186/s12877-017-0482-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chu D., Yen Y.-F., Hu H.-Y., et al. Factors associated with advance directives completion among patients with advance care planning communication in Taipei, Taiwan. PLoS One. 2018;13:e0197552. doi: 10.1371/journal.pone.0197552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chung R.Y., Wong E.L., Kiang N., et al. Knowledge, attitudes, and preferences of advance decisions, end-of-life care, and place of care and death in Hong Kong. A Population-Based Telephone Survey of 1067 Adults. J Am Med Dir Assoc. 2017;18:367.e19–367.e27. doi: 10.1016/j.jamda.2016.12.066. [DOI] [PubMed] [Google Scholar]
- 35.Garrido M.M., Idler E.L., Leventhal H., Carr D. Pathways from religion to advance care planning: beliefs about control over length of life and end-of-life values. Gerontologist. 2013;53:801–816. doi: 10.1093/geront/gns128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chiu C., Feuz M.A., McMahan R.D., Miao Y., Sudore R.L. “Doctor, make my decisions”: decision control preferences, advance care planning, and satisfaction with communication among diverse older adults. J Pain Symptom Manage. 2016;51:33–40. doi: 10.1016/j.jpainsymman.2015.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu P., Lorenz K.A., Chodosh J. Advance care planning among the oldest old. J Palliat Med. 2008;11:152–157. doi: 10.1089/jpm.2007.0134. [DOI] [PubMed] [Google Scholar]
- 38.Peterson L.J., Hyer K., Meng H., et al. Discussing end-of-life care preferences with family: role of race and ethnicity. Res Aging. 2019;41:823–844. doi: 10.1177/0164027519858716. [DOI] [PubMed] [Google Scholar]
- 39.Pearlman R.A., Starks H., Cain K.C., Cole W.G. Improvements in advance care planning in the veterans affairs system: results of a multifaceted intervention. Arch Intern Med. 2005;165:667–674. doi: 10.1001/archinte.165.6.667. [DOI] [PubMed] [Google Scholar]
- 40.Overbeek A., Korfage I.J., Jabbarian L.J., et al. Advance care planning in frail older adults: a cluster randomized controlled trial. J Am Geriatr Soc. 2018;66:1089–1095. doi: 10.1111/jgs.15333. [DOI] [PubMed] [Google Scholar]
- 41.Volandes A.E., Paasche-Orlow M.K., Davis A.D., et al. Use of video decision aids to promote advance care planning in Hilo, Hawai'i. J Gen Intern Med. 2016;31:1035–1040. doi: 10.1007/s11606-016-3730-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nair R., Kohen S.A. Can a patient-directed video improve inpatient advance care planning? A prospective pre-post cohort study. BMJ Qual Saf. 2019;28:887–893. doi: 10.1136/bmjqs-2018-009066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chan H.Y., Pang S.M. Let me talk--an advance care planning programme for frail nursing home residents. J Clin Nurs. 2010;19:3073–3084. doi: 10.1111/j.1365-2702.2010.03353.x. [DOI] [PubMed] [Google Scholar]
- 44.Sudore R.L., Schillinger D., Katen M.T., et al. Engaging diverse English-and Spanish-speaking older adults in advance care planning: the PREPARE randomized clinical trial. JAMA Intern Med. 2018;178:1616–1625. doi: 10.1001/jamainternmed.2018.4657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tulsky J.A. Beyond advance directives: importance of communication skills at the end of life. JAMA. 2005;294:359–365. doi: 10.1001/jama.294.3.359. [DOI] [PubMed] [Google Scholar]
- 46.Cardona M., Lewis E., Shanmugam S., et al. Dissonance on perceptions of end-of-life needs between health-care providers and members of the public: quantitative cross-sectional surveys. Australas J ageing. 2019;38:e75–e84. doi: 10.1111/ajag.12630. [DOI] [PubMed] [Google Scholar]
- 47.Romo R.D., Allison T.A., Smith A.K., Wallhagen M.I. Sense of control in end-of-life decision-making. J Am Geriatr Soc. 2017;65:e70–e75. doi: 10.1111/jgs.14711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abdul-Razzak A., You J., Sherifali D., Simon J., Brazil K. ‘Conditional candour’ and ‘knowing me’: an interpretive description study on patient preferences for physician behaviours during end-of-life communication. BMJ Open. 2014;4:e005653. doi: 10.1136/bmjopen-2014-005653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peck V., Valiani S., Tanuseputro P., et al. Advance care planning after hospital discharge: qualitative analysis of facilitators and barriers from patient interviews. BMC Palliat Care. 2018;17:127. doi: 10.1186/s12904-018-0379-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Malcomson H., Bisbee S. Perspectives of healthy elders on advance care planning. J Am Acad Nurse Pract. 2009;21:18–23. doi: 10.1111/j.1745-7599.2008.00369.x. [DOI] [PubMed] [Google Scholar]
- 51.Vandrevala T., Hampson S., Chrysanthaki T. Older people's perspectives on end-of-life decision. Qual Ageing Pol Pract Res. 2002;3:36–49. [Google Scholar]
- 52.Fried T., Zenoni M., Iannone L. A dyadic perspective on engagement in advance care planning. J Am Geriatr Soc. 2017;65:172–178. doi: 10.1111/jgs.14497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gjerberg E., Lillemoen L., Førde R., Pedersen R. End-of-life care communications and shared decision-making in Norwegian nursing homes - experiences and perspectives of patients and relatives. BMC Geriatr. 2015;15:103. doi: 10.1186/s12877-015-0096-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Piers R.D., van Eechoud I.J., Van Camp S., et al. Advance care planning in terminally ill and frail older persons. Patient Education Couns. 2013;90:323–329. doi: 10.1016/j.pec.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 55.Paiva A., Redding C.A., Iannone L., et al. Feasibility of delivering a tailored intervention for advance care planning in primary care practice. J Am Geriatr Soc. 2019;67:1917–1921. doi: 10.1111/jgs.16035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shaw M., Hewson J., Hogan D.B., Raffin Bouchal S., Simon J. Characterizing readiness for advance care planning from the perspective of residents, families, and clinicians: an interpretive descriptive study in supportive living. Gerontologist. 2018;58:739–748. doi: 10.1093/geront/gnx006. [DOI] [PubMed] [Google Scholar]
- 57.Detering K.M., Hancock A.D., Reade M.C., Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. Br Med J. 2010;340:847. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Michael N., O'Callaghan C., Sayers E. Managing ‘shades of grey’: a focus group study exploring community-dwellers' views on advance care planning in older people. BMC Palliat Care. 2017;16:2. doi: 10.1186/s12904-016-0175-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Groebe B., Rietz C., Voltz R., Strupp J. How to talk about attitudes toward the end of life: a qualitative study. Am J Hosp Palliat Care. 2019;36:697–704. doi: 10.1177/1049909119836238. [DOI] [PubMed] [Google Scholar]
- 60.Barnes K., Jones L., Tookman A., King M. Acceptability of an advance care planning interview schedule: a focus group study. Palliat Med. 2007;21:23–28. doi: 10.1177/0269216306073638. [DOI] [PubMed] [Google Scholar]
- 61.Fried T.R., Redding C.A., Robbins M.L., et al. Stages of change for the component behaviors of advance care planning. J Am Geriatr Soc. 2010;58:2329–2336. doi: 10.1111/j.1532-5415.2010.03184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bravo G., Trottier L., Arcand M., et al. Promoting advance care planning among community-based older adults: a randomized controlled trial. Patient Educ Couns. 2016;99:1785–1795. doi: 10.1016/j.pec.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 63.Ratner E., Norlander L., McSteen K. Death at home following a targeted advance-care planning process at home: the Kitchen Table Discussion. J Am Geriatr Soc. 2001;49:778–781. doi: 10.1046/j.1532-5415.2001.49155.x. [DOI] [PubMed] [Google Scholar]
- 64.Hinderer K.A., Lee M.C. Chinese Americans' attitudes toward advance directives: an assessment of outcomes based on a nursing-led intervention. Appl Nurs Res. 2019;49:91–96. doi: 10.1016/j.apnr.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 65.Kastbom L., Milberg A., Karlsson M. ‘We have no crystal ball’-advance care planning at nursing homes from the perspective of nurses and physicians. Scand J Prim Health Care. 2019;37:191–199. doi: 10.1080/02813432.2019.1608068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cheang F., Finnegan T., Stewart C., Hession A., Clayton J.M. Single-centre cross-sectional analysis of advance care planning among elderly inpatients. Intern Med J. 2014;44:967–974. doi: 10.1111/imj.12550. [DOI] [PubMed] [Google Scholar]
- 67.Braun U.K., Beyth R.J., Ford M.E., Espadas D., McCullough L.B. Decision-making styles of seriously ill male Veterans for end-of-life care: autonomists, altruists, authorizers, absolute trusters, and avoiders. Patient Education Couns. 2014;94:334–341. doi: 10.1016/j.pec.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 68.Karasz A., Sacajiu G., Kogan M., Watkins L. The Rational Choice Model in family decision making at the end of life. J Clin Ethics. 2010;21:189–200. [PubMed] [Google Scholar]
- 69.van Eechoud I.J., Piers R.D., Van Camp S., et al. Perspectives of family members on planning end-of-life care for terminally ill and frail older people. J Pain Symptom Manage. 2014;47:876–886. doi: 10.1016/j.jpainsymman.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 70.Overbeek A., Korfage I.J., Hammes B.J., van der Heide A., Rietjens J.A. Experiences with and outcomes of Advance Care Planning in bereaved relatives of frail older patients: a mixed methods study. Age and ageing. 2019;48:299–306. doi: 10.1093/ageing/afy184. [DOI] [PubMed] [Google Scholar]
- 71.Bravo G., Sene M., Arcand M., Hérault É. Effects of advance care planning on confidence in surrogates' ability to make healthcare decisions consistent with older adults' wishes: findings from a randomized controlled trial. Patient Educ Couns. 2018;101:1256–1261. doi: 10.1016/j.pec.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 72.Hawkins N.A., Ditto P.H., Danks J.H., Smucker W.D. Micromanaging death: process preferences, values, and goals in end-of-life medical decision making. Gerontologist. 2005;45:107–117. doi: 10.1093/geront/45.1.107. [DOI] [PubMed] [Google Scholar]
- 73.Abdul-Razzak A., Heyland D.K., Simon J., et al. Patient-family agreement on values and preferences for life-sustaining treatment: results of a multicentre observational study. BMJ Support Palliat Care. 2019;9:e20. doi: 10.1136/bmjspcare-2016-001284. [DOI] [PubMed] [Google Scholar]
- 74.Hunter J.J., Walters W. Patient beliefs and preferences regarding surrogate decision makers. South Med J. 2018;111:518–523. doi: 10.14423/SMJ.0000000000000863. [DOI] [PubMed] [Google Scholar]
- 75.Schubart J.R., Reading J.M., Penrod J., et al. Family caregivers' characterization of conversations following an ACP event. Am J Hosp Palliat Care. 2018;35:1161–1167. doi: 10.1177/1049909118760302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shaku F., Tsutsumi M., Nakamura A., et al. Factors relating to caregivers' preference for advance care planning of patients in Japan: a cross-sectional study. Am J Hosp Palliat Med. 2019;36:727–733. doi: 10.1177/1049909119844517. [DOI] [PubMed] [Google Scholar]
- 77.Lankarani-Fard A., Knapp H., Lorenz K.A., et al. Feasibility of discussing end-of-life care goals with inpatients using a structured, conversational approach: the Go Wish card game. J Pain Symptom Manage. 2010;39:637–643. doi: 10.1016/j.jpainsymman.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 78.Zapata C., Lum H.D., Wistar E., Horton C., Sudore R.L. Feasibility of a video-based advance care planning website to facilitate group visits among diverse adults from a safety-net health system. J Palliat Med. 2018;21:853–856. doi: 10.1089/jpm.2017.0476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Seymour J. Technology and “natural death”: a study of older people. J Gerontol Geriatr. 2003;36:339–346. doi: 10.1007/s00391-003-0166-1. [DOI] [PubMed] [Google Scholar]
- 80.Periyakoil V.S., Neri E., Kraemer H. A randomized controlled trial comparing the letter project advance directive to traditional advance directive. J Palliat Med. 2017;20:954–965. doi: 10.1089/jpm.2017.0066. [DOI] [PubMed] [Google Scholar]
- 81.Brimblecombe C., Crosbie D., Lim W.K., Hayes B. The Goals of Patient Care project: implementing a proactive approach to patient-centred decision-making. Intern Med J. 2014;44:961–966. doi: 10.1111/imj.12511. [DOI] [PubMed] [Google Scholar]
- 82.Silvester W., Parslow R.A., Lewis V.J., et al. Development and evaluation of an aged care specific Advance Care Plan. BMJ Support Palliat Care. 2013;3:188–195. doi: 10.1136/bmjspcare-2012-000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hold J., Payne C., Lesandrini J., Glover A.C. Successful advance care planning in a rural nursing home. Am J Hosp Palliat Care. 2019;36:357–361. doi: 10.1177/1049909118812162. [DOI] [PubMed] [Google Scholar]
- 84.DePriest J., Jagannath P., Iannetti M., Kemper S. A more directive living will for older adult patients with end-stage medical conditions? South Med J. 2019;112:531–534. doi: 10.14423/SMJ.0000000000001028. [DOI] [PubMed] [Google Scholar]
- 85.Dignam C., Brown M., Thompson C.H. Changes in resuscitation and end-of-life documentation in older patients' clinical case notes: a comparison of 2011 and 2017 practice. Australas J ageing. 2019;38:28–32. doi: 10.1111/ajag.12587. [DOI] [PubMed] [Google Scholar]
- 86.Almack K., Cox K., Moghaddam N., Pollock K., Seymour J. After you: conversations between patients and healthcare professionals in planning for end of life care. BMC Palliat Care. 2012;11:15. doi: 10.1186/1472-684X-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tan W.S., Bajpai R., Ho A.H.Y., Low C.K., Car J. Retrospective cohort analysis of real-life decisions about end-of-life care preferences in a Southeast Asian country. BMJ Open. 2019;9:e024662. doi: 10.1136/bmjopen-2018-024662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Taneja R., Faden L.Y., Schulz V., et al. Advance care planning in community dwellers: a constructivist grounded theory study of values, preferences and conflicts. Palliat Med. 2019;33:66–73. doi: 10.1177/0269216318803487. [DOI] [PubMed] [Google Scholar]
- 89.Kim J., Heo S., Hong S.W., Shim J., Lee J.A. Correlates of advance directive treatment preferences among community dwelling older people with chronic diseases. Int J Old People Nurs. 2019;14:e12229. doi: 10.1111/opn.12229. [DOI] [PubMed] [Google Scholar]
- 90.Lum H.D., Jones J., Matlock D.D., et al. Advance care planning meets group medical visits: the feasibility of promoting conversations. Ann Fam Med. 2016;14:125–132. doi: 10.1370/afm.1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bose-Brill S., Feeney M., Prater L., et al. Validation of a novel electronic health record patient portal advance care planning delivery system. J Med Internet Res. 2018;20:e208. doi: 10.2196/jmir.9203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Brungardt A., Daddato A.E., Parnes B., Lum H.D. Use of an ambulatory patient portal for advance care planning engagement. J Am Board Fam Med. 2019;32:925–930. doi: 10.3122/jabfm.2019.06.190016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gillick M.R., Volandes A.E. In: Encyclopedia of Psychology of Decision Making. Murphy D., Longo D., editors. Nova Science Publishers, Inc.; 2009. The Psychology of using and creating video decision aids for advance care planning; pp. 183–196. [Google Scholar]
- 94.Lovell A., Yates P. Advance Care Planning in palliative care: a systematic literature review of the contextual factors influencing its uptake 2008–2012. Palliat Med. 2014;28:1026–1035. doi: 10.1177/0269216314531313. [DOI] [PubMed] [Google Scholar]
- 95.Tzeng H.M., Barker A., Kang Y., Okpalauwaekwe U., Yin C.Y. Are older adults' demographic characteristics social determinants of their perceived importance, desire, and ability to perform end-of-life self-care actions? Nursing Forum. 2019;54:565–574. doi: 10.1111/nuf.12371. Wiley Online Library. [DOI] [PubMed] [Google Scholar]
- 96.Lum H.D., Barnes D.E., Katen M.T., et al. Improving a full range of advance care planning behavior change and action domains: the PREPARE randomized trial. J Pain Symptom Manage. 2018;56:575–581.e7. doi: 10.1016/j.jpainsymman.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.David D., Barnes D.E., McMahan R.D., et al. Patient activation: a key component of successful advance care planning. J Palliat Med. 2018;21:1778–1782. doi: 10.1089/jpm.2018.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mirarchi F.L., Juhasz K., Cooney T.E., et al. Triad XII: are patients aware of and agree with DNR or POLST orders in their medical records. J Patient Saf. 2019;15:230. doi: 10.1097/PTS.0000000000000631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schonwetter R.S., Walker R.M., Solomon M., Indurkhya A., Robinson B.E. Life values, resuscitation preferences, and the applicability of living wills in an older population. J Am Geriatr Soc. 1996;44:954–958. doi: 10.1111/j.1532-5415.1996.tb01867.x. [DOI] [PubMed] [Google Scholar]
- 100.Winter L. Patient values and preferences for end-of-life treatments: are values better predictors than a living will? J Palliat Med. 2013;16:362–368. doi: 10.1089/jpm.2012.0303. [DOI] [PubMed] [Google Scholar]
- 101.Oliver D. David Oliver: “Progressive dwindling,” frailty, and realistic expectations. BMJ. 2017;358:j3954. doi: 10.1136/bmj.j3954. [DOI] [PubMed] [Google Scholar]
- 102.Heyland D.K., Barwich D., Pichora D., et al. Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Intern Med. 2013;173:778–787. doi: 10.1001/jamainternmed.2013.180. [DOI] [PubMed] [Google Scholar]
- 103.Towsley G.L., Hirschman K.B., Madden C. Conversations about end of life: perspectives of nursing home residents, family, and staff. J Palliat Med. 2015;18:421–428. doi: 10.1089/jpm.2014.0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sudore R.L., Heyland D.K., Lum H.D., et al. Outcomes that define successful advance care planning: a Delphi panel consensus. J Pain Symptom Manage. 2018;55:245–255.e8. doi: 10.1016/j.jpainsymman.2017.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cesari M., Araujo de Carvalho I., Amuthavalli Thiyagarajan J., et al. Evidence for the domains supporting the construct of intrinsic capacity. J Gerontol Ser A. 2018;73:1653–1660. doi: 10.1093/gerona/gly011. [DOI] [PubMed] [Google Scholar]
- 106.Lim W.S., Wong S.F., Leong I., Choo P., Pang W.S. Forging a frailty-ready healthcare system to meet population ageing. Int J Environ Res Public Health. 2017;14:1448. doi: 10.3390/ijerph14121448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Harrison K.L., Adrion E.R., Ritchie C.S., Sudore R.L., Smith A.K. Low completion and disparities in advance care planning activities among older Medicare beneficiaries. JAMA Intern Med. 2016;176:1872–1875. doi: 10.1001/jamainternmed.2016.6751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kale M.S., Ornstein K.A., Smith C.B., Kelley A.S. End-of-Life discussions with older adults. J Am Geriatr Soc. 2016;64:1962–1967. doi: 10.1111/jgs.14285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hong M., Yi E.-H., Johnson K.J., Adamek M.E. Facilitators and barriers for advance care planning among ethnic and racial minorities in the US: a systematic review of the current literature. J immigrant Minor Health. 2018;20:1277–1287. doi: 10.1007/s10903-017-0670-9. [DOI] [PubMed] [Google Scholar]
- 110.Hong M., Kim K. Advance care planning among ethnic/racial minority older adults: prevalence of and factors associated with informal talks, durable power of attorney for health care, and living will. Ethn Health. 2020:1–10. doi: 10.1080/13557858.2020.1734778. [DOI] [PubMed] [Google Scholar]
- 111.Sanders J.J., Curtis J.R., Tulsky J.A. Achieving goal-concordant care: a conceptual model and approach to measuring serious illness communication and its impact. J Palliat Med. 2018;21:S17–S27.. doi: 10.1089/jpm.2017.0459. [DOI] [PMC free article] [PubMed] [Google Scholar]