ABSTRACT
Mucinous cystic neoplasms (MCNs) of the pancreas occurring during pregnancy constitute a rare condition requiring special management due to its large size, malignant potential and the risk of fetal growth restriction. The key points to manage MCNs are to perform a correct diagnosis, accurately evaluate the grade of malignant potential in order to establish the right time for pancreatic surgery and to choose the most appropriate fetal mode of delivery. We describe a case of an incidental abdominal mass detected in a third-trimester pregnant woman. At surgery, a huge pancreatic cystic tumour was found and a distal pancreatectomy with splenic preservation was performed. The histopathological analysis revealed an MCN of the pancreas with low-grade dysplasia. To our knowledge, this is the largest pancreatic MCN detected in a pregnant woman reported in the literature and one of the few successfully resected after vaginal delivery.
Keywords: Mucinous cystic neoplasms, Pregnancy, Pancreatic tumour, Hepatobiliary surgery
INTRODUCTION
Mucinous cystic neoplasms (MCNs) are uncommon pancreatic tumours, typically found in the body or tail of the pancreas [1, 2]. Their key defining feature is the presence of mucin-producing columnar epithelium supported by an ovarian-type stroma [1–4].
Because of the rapid tumour growth, the management of these tumours during pregnancy is challenging. Pancreatic MCNs are considered potentially malignant and the incidence of malignant transformation correlates directly with the overall size and the cyst’s complexity [1–4]. Nevertheless, there is no standardized management, and the decision whether to observe or to operate is based on expert opinions and small series reports.
In this report, we present a case of a 32-year-old pregnant woman with a large pancreatic MCN, which grew rapidly during late pregnancy, and a review of published cases, including clinical and tumour characteristics, surgical strategy and histologic findings.
CASE REPORT
A 32-year-old woman at 31 weeks of pregnancy was referred to our hospital due to an abdominal mass detected during routine check-up. She had no notable medical history. The third-trimester routine abdominal ultrasound revealed the presence of a cystic lesion in the left upper abdomen, which was not noted in previous ultrasounds. Further evaluation with magnetic resonance imaging (MRI) revealed a complex cystic lesion (21 × 13 × 14 cm) arising in the left quadrant of the abdomen, involving the tail of the pancreas (Fig. 1a). The cyst had two solid components, the largest one with 5.2 cm (Fig. 1b). There were also a few septa inside the cystic mass (Fig. 1a and c). The diagnostic hypotheses were an idiopathic retroperitoneal hematoma, a pancreatic MCN or retroperitoneal cystic lesion. Despite its large volume, the patient did not present complaints and physical examination revealed normal.
Figure 1.
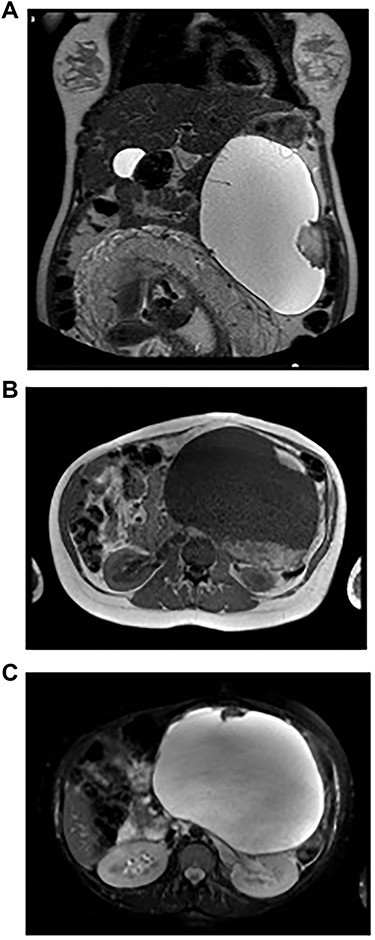
Imaging studies. A: Abdominopelvic T2-weighted coronal MRI – Voluminous left supramesocolic cystic formation (24 cm × 17 cm × 13 cm), with well-defined contours and small septa and parietal vegetation inside. B: Abdominopelvic T1-weighted axial MRI – The lesion with a solid component hyperintense on T1-weighted imaging, translating eventual area of haemorrhage. C: Abdominopelvic T2-weighted axial MRI – The lesion pushed the stomach to the right and the spleen upward, as well as the kidney to the back, apparently without direct invasion of these structures.
Laboratory tests showed slight anaemia with normal levels of amylase and liver enzymes. Tumour markers carcinoembryonic antigen (CEA) and carbohydrate antigens (CA19-9, CA15-3 and CA125) were negative.
The delivery was anticipated to 37-week gestation due to fetal growth restriction caused by increased tumour size, and the patient had a vaginal non-complicated delivery. At that point, the tumour measured 24 × 17 × 13 cm (longitudinal diameter/transverse diameter/anteroposterior axis).
The patient continued to have no subjective complaints, but an elastic large mass in the left upper quadrant was noted on physical examination (Fig. 2a).
Figure 2.
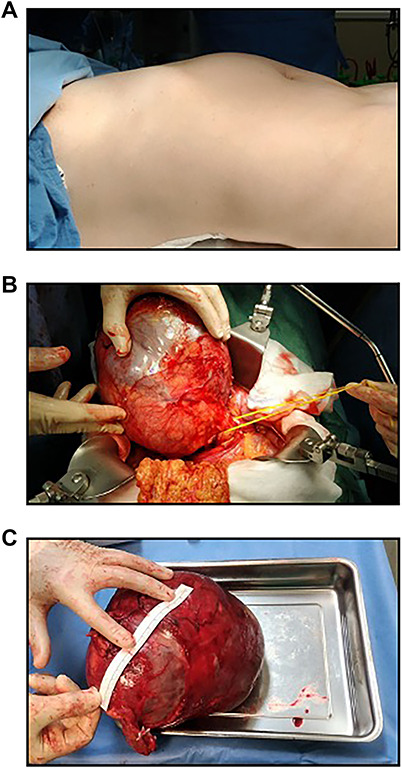
Intraoperative findings and macroscopic observations. A: Preoperative photograph of a postpartumpatient with a large pancreatic MCN. B: A large smooth cystic lesion occupied the body and tail of the pancreas. C: Macroscopic view of the resected tumour.
Five weeks after delivery, the patient was submitted to a laparotomy for tumour resection. Intraoperatively, a huge cystic mass arising from the pancreatic body was identified (Fig. 2b). Thus, a spleen-preserving distal pancreatectomy was performed (Warshaw technique). Since invasive carcinoma was not suspected, the spleen was preserved.
Macroscopic, the tumour measured almost 30 cm, had a smooth surface and was filled with a yellow–brownish mucinous fluid and necrotic debris, apparently with no communication with the pancreatic ductal system (Fig. 2c).
Histopathological examination revealed a mucin-producing columnar epithelium lining the inner wall of the unilocular cystic tumour, with ovarian-type stromal (Fig. 3a–c). Thus, the diagnosis of pancreatic MCN with low-grade dysplasia (PanIN1) was made, with tumour-free margins and non-affected lymph nodes. Analysis of the lesion’s mucous revealed CEA levels >15 000 and normal CA19-9, CA15-3 and amylase levels.
Figure 3.
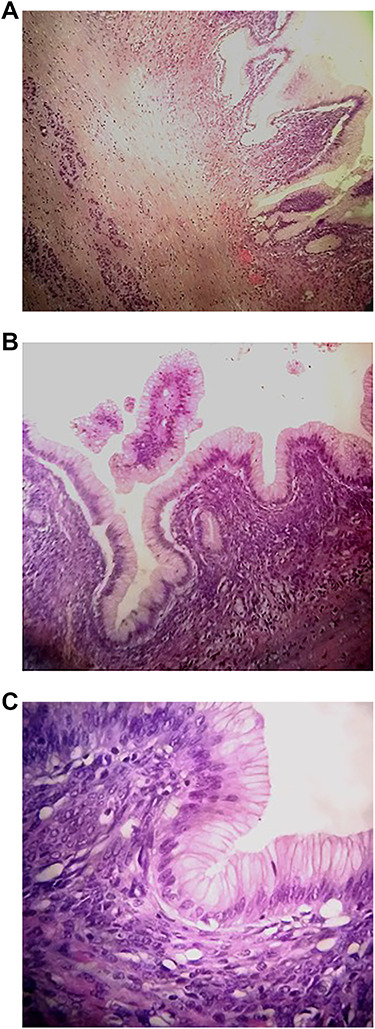
Histological analysis. A: Pancreatic cystic wall (Hematoxylin and eosin stain (HE); ×40 magnification). B: Pancreatic cystic wall lined by foveolar gastric type surrounded by dense ovarian type stroma (HE; ×100). C: Details of epithelium with low grade dysplasia (HE; ×400).
The patient had an uneventful post-operative course and was discharged on the 10th post-operative day.
Clinical examination, analysis and abdominopelvic computerized tomography (CT) were performed 6 months after surgery showing no abnormalities. The patient maintained regular follow-up with CT, remaining disease-free for 12 months after surgery.
DISCUSSION
The occurrence of a pancreatic tumour in a young patient is rare and the association of MCN with pregnancy is exceptional [1]. MCNs of the pancreas tend to grow slowly and remain indolent for many years but MCNs developing during pregnancy tend to grow rapidly and can become huge [2]. This report supports the theory that pancreatic MCN is a hormone-dependent tumour, which can achieve large sizes in late pregnancy. Few cases of pancreatic MCN associated with pregnancy have been reported. To our best knowledge, there are only 21 cases described in the literature to date. In the reviewed published reports, 10 patients underwent surgery after delivery but just 6 had a vaginal delivery. One patient had a missed abortion at 10 weeks of gestation [2]. The remaining 11 MCNs reported were resected during the second trimester of pregnancy [4–9]. The largest tumour size reported was 22 cm, with the mean size reported being 14 cm (Fig. 4) [5].
Figure 4.
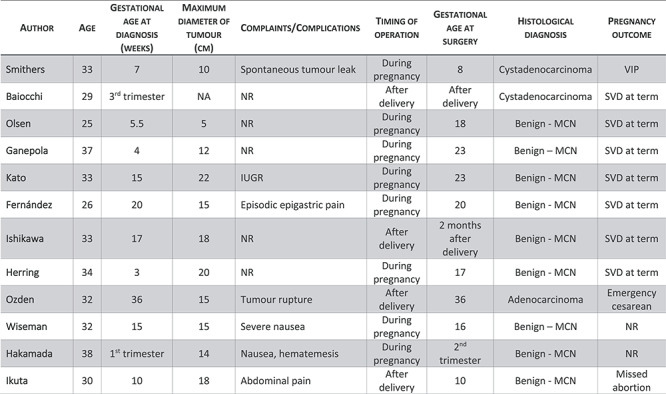
Clinical characteristics of reported pancreatic MCN during pregnancy.
Figure 4. Clinical characteristics of reported pancreatic MCN during pregnancy.
A pancreatic MCN detected during pregnancy requires a careful management. The malignant potential request a surgical resection but the possible adverse effects on the fetus also need to be consider. An important issue regarding the management of MCNs is to decide when to perform pancreatic surgery. There are some concerns that should be deemed: an appropriate diagnosis of a pancreatic neoplasm with careful evaluation of the malignant potential is necessary, and to consider the effects of surgery on mother and fetus.
The estimation of malignant potential represents a difficult task. There are some radiographic findings on CT scan suggesting an invasive mucinous cystadenocarcinoma, but the definitive diagnosis can only be made through histological analysis. CT scans increase the risk of fetal malformation and should be avoided during pregnancy; endoscopic ultrasound is an invasive procedure and serum levels of the tumour markers are even less useful. CEA alone seems to be the most accurate indicator with the most used value of 192 ng/ml [3, 10]. The best investigation for pancreatic MCNs associated with pregnancy remains the MRI [4, 6]. The implications of an increasing MCN on both fetal development and on maternal disease progression risk should be taken into account. According to literature, the second trimester is considered the safest period for surgery since it is easier in this period and the risk of abortion in lower [4–9].
In this case, the tumour was detected in the third trimester of gestation, the patient had no complains and serum tumour markers were negative. The multidisciplinary decision was to proceed the pregnancy with closed follow-up and to postpone surgery until after delivery.
MCNs of the pancreas during pregnancy are rare and their management is challenging. We believe that tumour imaging considering the malignant predictors, clinical condition of the mother and the fetus and the stage of pregnancy should be evaluated in an interdisciplinary setting and should dictate the surgical strategy. To the best of our knowledge, this is the largest pancreatic MCN detected in a pregnant woman reported in literature and one of the few successfully resected after vaginal delivery.
Conflict of Interest
Authors declare no conflict of interest.
REFERENCES
- [1]. Tica AA, Tica OS, Saftoiu A, Camen D, Tica VI. Large pancreatic mucinous cystic neoplasm during pregnancy: what should be done? Gynecol Obstet Invest 2013;75:132–8. [DOI] [PubMed] [Google Scholar]
- [2]. Ikuta S, Aihara T, Yasui C, Iida H, Yanagi H, Mitsunobu M, et al. . Large mucinous cystic neoplasm of the pancreas associated with pregnancy. World J Gastroenterol 2008 Dec 21;14:7252–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Matthews JB. Shackelford’s Surgery of the Alimentary Tract, 8Ed edn. Elsevier, 2018. [Google Scholar]
- [4]. Ishikawa K, Hirashita T, Kinoshita H, Kitano M, Matsuoi S, Matsumata T, et al. . Large mucinous cystadenoma of the pancreas during pregnancy: report of a case. Surgery Today: Official Journal of the Japan Surgical Society. 2007;37:1013–7. [DOI] [PubMed] [Google Scholar]
- [5]. Kosumi K, Takamori H, Hashimoto D, Tanaka H, Abe S, Nakahara O, et al. . Mucinous cystic neoplasm of the pancreas activated during pregnancy. Surg Case Rep 2015;1:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Boyd CA, Benarroch-Gampel J, Kilic G, Kruse EJ, Weber SM, Riall TS. Pancreatic neoplasms in pregnancy: diagnosis, complications, and management. Gastrointest Surg 2012 May;16:1064–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Herring AA, Graubard MB, Gan SI, Schwaitzberg SD. Mucinous cystadenocarcinoma of the pancreas during pregnancy. Pancreas 2007;34:470–3. [DOI] [PubMed] [Google Scholar]
- [8]. Kato M, Kubota K, Kita J, Shimoda M, Rokkaku K, Inaba N, et al. . Huge mucinous cystadenoma of the pancreas developing during pregnancy: a case report. Pancreas 2005;30:186–8. [DOI] [PubMed] [Google Scholar]
- [9]. Fernández EML, Malagón AM, Gonzalez IA, Montes JRM, Luis HD, Hermoso FG, et al. . Mucinous cystic neoplasm of the pancreas during pregnancy: the importance of proper management. J Hepatobiliary Pancreat Surg 2005;12:494–7. [DOI] [PubMed] [Google Scholar]
- [10]. Brugge WR, Lewandrowski K, Lee-Lewandrowski E, Centeno BA, Szydlo T, Regan S, et al. . Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology 2004;126:1330–6. [DOI] [PubMed] [Google Scholar]


