Highlights
-
•
Children and adolescents are vulnerable groups during the COVID-2019 pandemic.
-
•
Children and adolescents may be experiencing symptoms for PTSD and GAD.
-
•
Comorbidity patterns of the symptoms for PTSD and GAD vary.
-
•
Perceived threat and stigma are risk factors related to PTSD and GAD.
Keywords: PTSD, GAD, Perceived threat, Stigma, COVID-19, Latent profile
Abstract
The present study aims to examine the comorbidity patterns of the symptoms (intrusion and avoidance) for posttraumatic stress disorder (PTSD) and generalized anxiety disorder (GAD) and the role of perceived threat and courtesy stigma in distinguishing specific patterns of the symptoms for PTSD and GAD among children and adolescents who are susceptible to coronavirus disease 2019 (COVID-19) in Hubei, China. A total of 1172 (683 female and 489 male) children and adolescents aged 8–18 years were involved in completing the measurements of PTSD, GAD, perceived threat of COVID-19, and COVID-19-related courtesy stigma. The Latent Profile Analysis identified the three profiles of the symptoms for PTSD and GAD which were labeled as Moderate PTSD, Mild Comorbidity, and Severe Comorbidity. The scores of the symptoms for PTSD, GAD, perceived threat, and stigma were different among the three profiles. The risk factors (i.e., perceived threat and stigma) that are related to comorbidity patterns were examined through a three-step method. The possibility of entry into the Severe Comorbidity Profile increased with increasing perceived threat and stigma. The mental health care interventions for children and adolescents who are susceptible to COVID-19 can be developed to reduce perceived threat and stigma.
1. Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease that began in December 2019, which is caused by the most recently discovered coronavirus (World Health Organization, 2020c). The coronavirus can spread rapidly through human-to-human transmission by droplets, contact, and fomite (World Health Organization, 2020a, World Health Organization, 2020b). As of March 21, 2020, 185 countries, areas, and territories worldwide have reported 267,013 people who have COVID-19 and 11,201 deaths (World Health Organization, 2020a, World Health Organization, 2020c). In Mainland China, Hubei reported the highest number of people who have COVID-19, including 67,800 individuals with 3139 reported deaths (4.6% mortality), and Wuhan had the highest number of people who have COVID-19 (50,005) and deaths (2508, 5.0% mortality) among all cities in Hubei (Chinese Center for Disease Control and Prevention, 2020).
To confront the COVID-19, most provinces including Hubei launched the first-level response to public health emergencies. Wuhan took the lead in implementing a lockdown strategy, which began Jan 23–24, 2020, followed by an increasing number of other cities. In the first 2–3 weeks after the lockdown strategy was implemented, the Chinese people, especially residents in Hubei, lacked knowledge about COVID-19, lacked protective equipment such as masks, lacked medical resources, and they were bombarded with various discomforting online information. Children and adolescents were out of school and were living with restrictions on movement. Children and adolescents, as vulnerable groups during public health emergencies, have their mental health negatively affected by the outbreak of COVID-19 and the unprecedented measures to contain its spread (Guessoum et al., 2020, Liu et al., 2020). They are at high risk for multiple mental health problems and were experiencing symptoms for posttraumatic stress disorder (PTSD) (Vindegaard and Eriksen Benros, 2020) and generalized anxiety disorder (GAD) (Huang and Zhao, 2020).
PTSD appears after traumatic experiences (i.e., actual or threatened death, serious injury, or sexual violence) that happened to people directly or something they witnessed and is characterized by a typical symptom pattern of intrusion, avoidance, arousal, and negative changes in beliefs and feelings (American Psychological Association, 2013). Since the diagnosis of PTSD requires individuals to have all the symptoms lasting more than one month (American Psychological Association, 2013), only the symptoms for PTSD can be investigated in the short time after the outbreak of COVID-19 (Liu et al., 2020, Vindegaard and Eriksen Benros, 2020). Generalized Anxiety Disorder (GAD) is characterized by excessive worries about untoward events and chronic anxiety (American Psychological Association, 2013). Several studies have explored the co-occurrence of PTSD and GAD symptoms among children and adolescents who experience natural disasters. Marthoenis, Ilyas, Sofyan, & Schouler-Ocak (2019) conducted a 6-month cross-sectional study after the 2016 Aceh Earthquake among 321 senior high school students. A total of 58.3%, 32.1%, and 24.9% of adolescents reported the clinical symptoms of PTSD, GAD, and both, respectively. Researchers used a longitudinal design on 1573 adolescents who were exposed to the 2008 Wenchuan earthquake in China to confirm the co-occurrence of PTSD and GAD and determine their mutually predictive power (Geng et al., 2019). However, these studies mainly adopted the variable-centered approach, which treats each variable as a separate construct, to study the relationship between variables across persons (Marsh, Lüdtke, Trautwein, & Morin, 2009). This phenomenon may overlook the interindividual heterogeneity in different comorbid patterns of PTSD and GAD.
Latent Profile Analysis (LPA) is an alternative person-centered approach that focuses on interindividual variation in different components of variables to classify individuals into heterogeneous subgroups (Marsh et al., 2009). Only two studies used LPA to explore the comorbidity of PTSD and GAD among children and adolescents. Lai, Kelley, Harrison, Thompson, and Self-Brown (2015) examined the typologies of PTSD, GAD, and depression symptoms among 353 children (aged 8–15 years) who were exposed to Hurricane Katrina and identified a No Disturbance group, a PTSD Only group, and a Mixed Internalizing group. Essau and de la Torre-Luque (2019) explored the number of comorbidity profiles of 26 kinds of lifetime mental disorders, including PTSD and GAD, among adolescents (aged 13–18 years) who participated in the National Comorbidity Survey Adolescent Supplement in the United States. At present, few studies have been conducted to identify the varying comorbidity patterns of PTSD and GAD among children and adolescents who are exposed to infectious diseases. The present study aimed to use LPA in examining the comorbidity patterns of the symptoms for PTSD and GAD among children and adolescents who are susceptible to COVID-19.
Risk factors related to comorbidity patterns should be identified to provide empirical support for evidence-based interventions. A meta-analysis of 64 independent samples (N = 32,238) in children and adolescents aged 6–18 years confirmed that factors relating to the subjective experience of the event (e.g., perceived threat) were the strongest predictors for post-trauma variables (e.g., PTSD or GAD) of the cognitive and psychosocial factors (Trickey, Siddaway, Meiser-Stedman, Serpell, & Field, 2012). A longitudinal study found that the onset of PTSD among children and adolescents was associated particularly with subjective threat (Meiser-Stedman et al., 2019). Similarly, the perceived threat has a significant effect on GAD among children and adolescents (Cho, Przeworski, & Newman., 2019). Besides, infectious disease-related stigma has gained increasing research attention because it is associated with trauma-related symptoms, such as low mood, irritability, insomnia, depression, and anxiety (Lee et al., 2005, Mo et al., 2015). The fear and misperception of emerging infectious diseases (e.g., Ebola and COVID-19) can lead to prejudice, discrimination, rejection, and stigmatization of people residing in places where the disease is widespread (Joffe, 2011, Ren et al., 2020). People who live in those places would perceive courtesy stigma, which is a subtype of stigma that a person perceived or experienced due to their social association with a stigmatized individual or group (e.g., relatives of people with schizophrenia) (Angermeyer et al., 2003).
This study attempted to fill in the research gap by examining the comorbidity patterns of the symptoms for PTSD and GAD among children and adolescents who are susceptible to COVID-19 via a person-centered approach named LPA. The role of perceived threat and courtesy stigma in distinguishing specific patterns of the symptoms for PTSD and GAD was further investigated. As above-mentioned, COVID-19 is a public health emergency and pandemic that has a sudden but huge impact on the mental health of children and adolescents. Although it is currently impossible to get the clinical screening and diagnosis of PTSD and GAD done, timely exploration of the symptoms for PTSD and GAD in a short period can provide empirical evidence for the design of professional and effective mental health services to aid the mental health of children and adolescents who are susceptible to COVID-19.
2. Methods
2.1. Participants and procedures
An online survey called Social Cognition and Behavior Investigation of COVID-19 was conducted to understand how people in Wuhan, other cities in Hubei excluding Wuhan, and other cities outside of Hubei perceived and responded to the threat of COVID-19. Data were collected from Jan 31 to Feb 8, 2020, in Mainland China. Till the time and at the time the survey was conducted, the newly increased number of people who have COVID-19 and the cumulative number of people who have COVID-19 in Hubei peaked (Chinese Center for Disease Control and Prevention, 2020). All participants were recruited by convenience sampling through social media. Convenient sampling through social media is a typical and common method used in studies of a public health emergency (e.g., Elrggal et al., 2018, Vartti et al., 2009). A total of 7058 participants (2157 male and 4901 female; mean age: 26.06, SD: 12.91, and range: 8–72) voluntarily participated in the investigation. Ethics approval was obtained from the Human Subjects Ethics Subcommittee of East China University of Science and Technology. Informed online consent of the participant was obtained by clicking the “AGREE” button before the completion of the investigation.
The sample of children and adolescents for this study is a subset of the total population that was sampled (including Wuhan, other cities in Hubei, and other cities outside Hubei). The following criteria were adopted to screen qualified participants: (a) understand and respond in Chinese, (b) currently residing in Hubei, (c) age within 8–18 years, (d) identified COVID-19 as a major stressful event experienced in the past 2 weeks, and (e) total PTSD score of >17 (Perrin, Meiser-Stedman, & Smith, 2005). As a result, 1172 children and adolescents (683 female and 489 male; mean age = 12.80, SD = 1.64) were involved in the current study for final statistical analysis.
2.2. Measures
2.2.1. Sociodemographic statistics
Self-reported general health was assessed by a single question (“In general, would you say that your health is? 1 = very poor, 2 = poor, 3 = fair, 4 = good, 5 = very good”) which is well-documented in many studies to describe the subjective health status of the participants (e.g., Fiorillo & Sabatini, 2011). The widely used MacArthur Scale of Subjective Socioeconomic Status ladder (Adler, Epel, Castellazzo, & Ickovics, 2000) was adopted to assess the subjective socioeconomic status. On the ladder with 10 rungs, in which lower rungs represent low social standing (1 = lowest, 10 = highest), the participants chose the rung that indicated their subjective status relative to other people.
2.2.2. Symptoms for PTSD
The self-reported eight-item Children’s Revised Impact of Event Scale (CRIES-8) (Perrin et al., 2005) was used to assess the severity of the symptoms for PTSD. The CRIES-8 included intrusion and avoidance subscales with four items for each. All items, such as “Did you have waves of strong feeling about the COVID-19-related events?” (intrusion) and “Did you try to remove COVID-19-related events from your memory?” (avoidance), were adapted to the current COVID-19. Participants were required to respond the items on a 4-point scale (0 = not at all, 1 = rarely, 3 = sometimes, and 5 = often). The total scores of the scale indicate the severity of the PTSD symptoms, ranging from 0 to 40. A score of 17 and above has been confirmed as an effective cut-off score in screening the diagnosed cases of PTSD symptoms (Perrin et al., 2005). The CRIES-8 has good internal consistency and construct validity among the Chinese context (Lau et al., 2013). The Cronbach’s alpha of the whole scale, the intrusion subscale, and the avoidance subscale were all 0.87 in the present study.
2.2.3. GAD symptoms
The 2-item Generalized Anxiety Disorder scale (i.e., GAD-2) (Kroenke, Spitzer, Williams, Monahan, & Löwe, 2007) was adopted to measure the presence and severity of GAD symptoms. There are two items “I feeling nervous, anxious, or on edge” and “I cannot stop or control myself from worrying”. Participants were asked to answer the frequency that they felt daily on the four-point Likert scale (0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day). The total score of the two items higher than 3 has been confirmed as an effective cut-off point in screening the diagnosed cases of GAD (Kroenke et al., 2007). The Chinese version of GAD-2 showed good internal consistency (Cronbach’s α = 0.85) among Chinese children aged approximately 12 years old (Wang et al., 2019). The Cronbach’s α of GAD-2 in the present study was 0.78.
2.2.4. Perceived threat of COVID-19
The perceived threat of COVID-19 was assessed by an 8-item scale that was adapted from the Perceived Threat of the Middle East Respiratory Syndrome (MERS) scale (Yoo, Choi, & Park, 2016). Two subscales named perceived susceptibility and perceived severity are present. The sample items in the perceived susceptibility and severity subscales were “COVID-19 infection can happen anytime and to anyone, even to a healthy individual” and “COVID-19 causes death quickly,” respectively. Each item was scored on the scale from 1 (completely disagree) to 5 (completely agree). The mean score of the entire scale indicated the level of the perceived threat of COVID-19. In the context of MERS in South Korea, the scale showed good internal consistency (Cronbach’s α = 0.89) (Yoo et al., 2016). In the present study, the Cronbach’s alpha was 0.80, 0.85, and 0.82 for the whole scale, the susceptibility subscale, and the severity subscale, respectively.
2.2.5. COVID-19-related courtesy stigma
COVID-19-related courtesy stigma was measured by five items that fit the research context selected from the Chinese Courtesy Stigma Scale, which is designed to measure courtesy stigma (Liu, Xu, Sun, Dumenci, & Seedat, 2014). Statements were modified using COVID-19-related words. For example, the item “Because of my family member’s HIV status, I feel estranged by people around me” was modified to “Because the COVID-19 outbreak took place in Wuhan/Hubei, I feel estranged by people around me.” The participants were required to answer the items on a four-point Likert scale (1 = none, 2 = a little, 3 = some, and 4 = a lot). The mean score of the scale indicated the level of COVID-19-related courtesy stigma. The Chinese Courtesy Stigma Scale had good reliability (Cronbach’s α ≥ 0.83) and construct validity (factor loadings = 0.72–0.93) in the Chinese context (Liu et al., 2014). The Cronbach’s α for the scale was 0.91 in the present study.
3. Results
3.1. Sociodemographic, descriptive and correlation statistics
The sociodemographic characteristics of the participants are summarized in Table 1 . A total of 93.00% of the participants are primary school students or secondary school students (N = 1090). A total of 81.74% of the participants (N = 958) reported that they had a good or very good general health, while only approximately 1.37% of the participants rated their health status as poor or very poor (N = 16). The mean score of the subjective socioeconomic status was 4.96 (SD = 1.95).
Table 1.
Sample characteristics (N = 1172).
| Variable | Participants (N = 1172) |
|
|---|---|---|
| Number | Percentage | |
| Gender | ||
| Male | 489 | 41.72% |
| Female | 683 | 58.28% |
| Education | ||
| Primary school | 262 | 22.35% |
| Secondary school | 828 | 70.65% |
| High school | 68 | 5.80% |
| Junior college and beyond | 14 | 1.20% |
| Health Status | ||
| Very poor | 1 | 0.09% |
| Poor | 15 | 1.28% |
| Fair | 198 | 16.89% |
| Good | 483 | 41.21% |
| Very good | 475 | 40.53% |
| Subjective Socioeconomic Status | ||
| 1 (Lowest) | 76 | 6.48% |
| 2 | 51 | 4.35% |
| 3 | 108 | 9.22% |
| 4 | 141 | 12.03% |
| 5 | 414 | 35.32% |
| 6 | 201 | 17.15% |
| 7 | 74 | 6.31% |
| 8 | 51 | 4.35% |
| 9 | 19 | 1.62% |
| 10 (Highest) | 37 | 3.16% |
Descriptive statistics, including mean scores and SD, as well as correlations of all variables, are shown in Table 2 . The total PTSD score was positively correlated with GAD (r = 0.16, p < 0.001), perceived threat (r = 0.08, p < 0.01), and stigma (r = 0.14, p < 0.001). Intrusion was negatively correlated with avoidance (r = −0.18, p < 0.001) and positively correlated with GAD (r = 0.29, p < 0.001) and perceived threat (r = 0.13, p < 0.01). However, the correlation between intrusion and stigma was not significant (p > 0.05). Avoidance was positively correlated with stigma (r = 0.15, p < 0.001) but not significantly associated with GAD and perceived threat (p > 0.05).
Table 2.
Bivariate Correlations (Pearson's r), Mean (M), and Standard Deviation (SD) among Key Study Variables (N = 1172).
| Variables | 1 | 2 | 3 | 4 | 5 | M | SD |
|---|---|---|---|---|---|---|---|
| 1 PTSD | – | 23.16 | 5.27 | ||||
| 2 Intrusion | 0.56*** | – | 13.65 | 3.73 | |||
| 3 Avoidance | 0.72*** | −0.18*** | – | 9.51 | 4.45 | ||
| 4 GAD | 0.16*** | 0.29*** | −0.06 | – | 2.96 | 1.83 | |
| 5 Perceived Threat | 0.08** | 0.13*** | −0.01 | 0.09** | – | 2.81 | 0.78 |
| 6 Stigma | 0.14*** | 0.02 | 0.15*** | 0.19*** | 0.08** | 1.76 | 0.69 |
* p < 0.05, ** p < 0.01, ***p < 0.001.
3.2. LPA
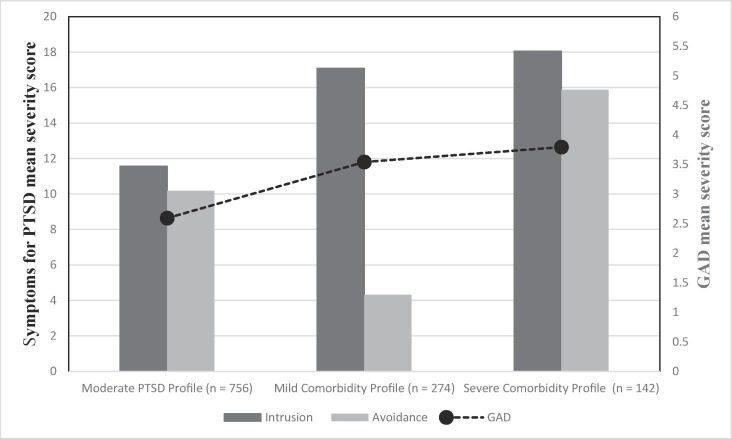
LPA was performed using Mplus 7.4 software to determine the coexistence of PTSD and GAD symptoms among the children and adolescents who were susceptible to COVID-19. The low Akaike information criteria, Bayesian information (BIC), adjusted BIC values, and high entropy as well as the significant Lo–Mendell–Rubin adjusted likelihood ratio and bootstrap likelihood ratio indicated the superior fit of the LPA model (Lo et al., 2001, Nylund et al., 2007, Ramaswamy et al., 1993, Yang, 2006). In the present study, the four-profile solution was the preferred one (Table 3 ). However, only 41 (3.4%) of the participants belonged to one of the profiles in the four-profile solution, which was less than the minimum number (n = 50) of participants required per latent profile (Yang, 2006). As a result, the alternative three-profile solution was adopted (Table 3 and Fig. 1 ).
Table 3.
Goodness of fit indices for different latent profile analysis models (N = 1172).
| Model | AIC | BIC | ABIC | Entropy | LMR-A P-value | BLRT P-value |
|---|---|---|---|---|---|---|
| 1-Profile | 17982.53 | 18012.93 | 17993.87 | – | – | – |
| 2-Profile | 17786.79 | 17837.46 | 17805.70 | 0.70 | < 0.001 | <0.001 |
| 3-Profile | 17483.25 | 17554.18 | 17509.71 | 0.82 | < 0.001 | <0.001 |
| 4-Profile | 17332.99 | 17424.18 | 17367.01 | 0.86 | < 0.001 | < 0.001 |
| 5- Profile | 17282.12 | 17393.58 | 17323.70 | 0.82 | 0.16 | <0.001 |
Note: AIC = Akaike information criterion, BIC = Bayesian information criterion, ABIC = Adjusted Bayesian information criterion, LMR-A = Lo–Mendell–Rubin adjusted likelihood ratio test, BLRT = Bootstrapped likelihood ratio test.
Fig. 1.
Mean severity scores on the three latent profiles of the symptoms for PTSD (i.e. intrusion and avoidance) and GAD commodity (N = 1172).
The first profile was labeled as Moderate PTSD Profile (N = 756, 64.51%). Most participants in the profile scored between 7 and 14 on intrusion (N = 680, 89.95%) and avoidance (N = 638, 84.39%) and between 0 and 2 on GAD (N = 423, 55.95%). The second profile was labeled as Mild Comorbidity Profile (N = 274, 23.38%). Most participants in this profile scored higher than 14 on intrusion (N = 227, 82.85%) and 2 on GAD (N = 187, 68.25%). However, participants scored lower than 7 on avoidance (N = 227, 82.85%). The third profile, which was labeled as Severe Comorbidity Profile (N = 142, 12.11%), had most participants who scored higher than 14 on intrusion (N = 137, 96.48%) and avoidance (N = 87, 61.27%) and scored higher than 2 on GAD (N = 109, 76.76%).
3.3. Multivariate ANOVA (MANOVA) and three-step method for predictors
The characteristics of the three-profile solution revealed by MANOVA are shown in Table 4 . The scores of PTSD, intrusion, and avoidance in the Severe Comorbidity Profile were significantly higher than those in the two other profiles (p < 0.001). Although Mild Comorbidity Profile and Moderate PTSD Profile showed no significant differences in the total PTSD score (p > 0.05), the Mild Comorbidity Profile scored significantly higher on intrusion symptoms than the Moderate PTSD Profile (p < 0.001) but scored lower on avoidance symptoms (p < 0.001). Although the scores of GAD symptoms in Severe Comorbidity Profile and Mild Comorbidity Profile were significantly higher than those in Moderate PTSD Profile (p < 0.01), but the difference was not significant (p > 0.05). Although Severe Comorbidity Profile and Mild Comorbidity Profile showed no difference in the score of perceived threat (p > 0.05), their scores on intrusion symptoms were higher than those in Moderate PTSD Profile (p < 0.001). Severe comorbidity profile showed the highest score in stigma, and Moderate PTSD Profile showed the lowest score (p < 0.001).
Table 4.
Multivariate analysis of variance (MANOVA) for the symptoms for PTSD, GAD, and risk factors among the three profiles (N = 1172).
| 1 Moderate PTSD Profile (N = 756) |
2 Mild Comorbidity Profile (N = 274) |
3 Severe Comorbidity Profile (N = 142) |
F | ηp2 | Post-Hoc Comparison | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||||
| PTSD | 21.69 | 3.20 | 21.43 | 3.16 | 34.30 | 3.75 | 941.52*** | 0.62 | 1, 2 < 3 |
| Intrusion | 11.47 | 2.39 | 17.27 | 2.18 | 18.25 | 1.84 | 976.44*** | 0.63 | 1 < 2 < 3 |
| Avoidance | 10.22 | 2.72 | 4.16 | 2.70 | 16.05 | 3.04 | 940.83*** | 0.62 | 2 < 1 < 3 |
| GAD | 2.59 | 1.69 | 3.54 | 1.86 | 3.83 | 1.89 | 49.83*** | 0.08 | 1 < 2, 3 |
| Perceived Threat | 2.75 | 0.75 | 2.91 | 0.78 | 2.97 | 0.89 | 7.78*** | 0.01 | 1 < 2, 3 |
| Stigma | 1.75 | 0.65 | 1.63 | 0.64 | 2.06 | 0.90 | 19.09*** | 0.03 | 2 < 1 < 3 |
Note. ***p < 0.001.
A three-step method (Asparouhov and Muthén, 2014) was adopted to examine the association between latent profile membership and risk factors (i.e., perceived threat and stigma). Table 5 illustrates the results. Compared with Moderate PTSD Profile, individuals who perceived additional threats were likely to be classified into other profiles with increasingly serious symptoms (i.e., Mild Comorbidity Profile and Severe Comorbidity Profile, p < 0.01, odds ratio > 1). Meanwhile, individuals who perceived more stigma were more likely to be classified into Severe Comorbidity Profile (p < 0.001, odds ratio > 1), rather than Mild Comorbidity Profile (p < 0.05, odds ratio < 1). Compared with Mild Comorbidity Profile, individuals who perceived higher stigma were likely to be classified into Severe Comorbidity Profile (p < 0.001, odds ratio > 1).
Table 5.
Results of 3-step LPA model with three latent profiles of the symptoms for PTSD (i.e. intrusion and avoidance) and GAD commodity (N = 1172).
| Severe Comorbidity Profile (vs. Moderate PTSD Profile) |
Mild Comorbidity Profile (vs. Moderate PTSD Profile) |
Severe Comorbidity Profile (vs. Mild Comorbidity Profile) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | OR | B | SE | OR | B | SE | OR | |
| Perceived Threat | 0.45** | 0.16 | 1.57 | 0.33** | 0.11 | 1.39 | 0.12 | 0.17 | 1.13 |
| Stigma | 0.69*** | 0.16 | 1.99 | −0.33* | 0.14 | 0.72 | 1.02*** | 0.19 | 2.78 |
Note: OR = Odds ratio.
* p < 0.05, ** p < 0.01, ***p < 0.001.
4. Discussion
In this study, LPA was adopted to investigate the comorbidity patterns of the symptoms for PTSD and GAD among children and adolescents who are susceptible to COVID-19 from Hubei, Mainland China. The results identified a three-profile solution of the symptoms for PTSD and GAD symptoms comorbidity that included Moderate PTSD, Mild Comorbidity, and Severe Comorbidity. The MANOVA results showed that the scores of PTSD, intrusion, avoidance, GAD, perceived threat, and stigma were different among the three profiles. Perceived threat and stigma can significantly distinguish Severe Comorbidity Profile from the two other profiles.
Moderate PTSD profile included participants who exhibited moderate levels of intrusion and avoidance but no evident symptom of anxiety. Participants in Mild Comorbidity Profile showed severe intrusion, mild avoidance, and evident anxiety symptoms. The participants who showed severe intrusion, severe avoidance, and evident anxiety symptoms were included in the Severe Comorbidity Profile. The current research confirmed the presence of comorbidity of the symptoms for PTSD and GAD among children and adolescents who are susceptible to COVID-19. The symptoms for PTSD and GAD should be evaluated to identify cases with different comorbidity patterns when screening the mental health of children and adolescents. The results can contribute to evidence-based social work and target psychological intervention.
The differentiating roles of perceived threat and stigma in the distinct comorbid patterns of the symptoms for PTSD and GAD have been discovered. Participants with higher perceived threat were more likely to enter comorbid profiles (i.e., Mild Comorbidity Profile and Severe Comorbidity Profile) than the Moderate PTSD Profile. Therefore, reducing threats perceived by people at risk of infection to a credible (i.e., not over- or understated) level while informing them of effective disease response strategies cannot only promote healthy behavior (Peters et al., 2013, Taylor, 2019) but also reduce the incidence of the comorbidity of PTSD and GAD symptoms. Participants who perceived a higher level of stigma were more likely to fall into Severe Comorbidity Profile and Moderate PTSD Profile than Mild Comorbidity Profile. One possible explanation is that perceived courtesy stigma may serve as a vulnerability factor for the severity of avoidance symptoms. Avoidance often occurs in the face of stress (Batey and Furnham, 2006). A review of 4256 samples from 21 related studies on internalizing stigma and avoidance found that individuals who internalize general stigma associated with the disease into their own personal stigmatizing beliefs may feel lonely and become highly avoidant (Abiri, Oakley, Hitchcock, & Hall, 2016). Therefore, measures should be taken to reduce the public stigma of potential COVID-19 infections. Potential COVID-19 infections should be intervened to reduce perceived stigma and internalization of stigma. These findings suggest that reducing the perceived threat should be emphasized in treatment and intervention for people in comorbid profiles of the symptoms for PTSD and GAD while reducing the perceived stigma is the focus of treatment and intervention for individuals with high levels of avoidance symptoms.
Two studies adopted the person-centered approach (i.e., LPA) to explore the comorbidity of PTSD and GAD in children and adolescents exposed to natural disasters. Lai et al. (2015) reported a comorbidity profile presenting a high level of GAD symptoms and a moderate level of PTSD, accounting for 37.17% in their sample. The current study further revealed the two sub-profiles of comorbidity of the symptoms for PTSD and GAD, namely, Mild Comorbidity (23.38%) and Severe Comorbidity (12.11%). By contrast, the comorbidity rates of PTSD and GAD in children and adolescents who experienced a natural disaster was 42.78%, as determined via the variable-centered method (Marthoenis et al., 2019). The rates of comorbid GAD determined via the variable-centered method in adult samples with diagnosed PTSD were 45.78% and 69.05% for the victims of serious motor vehicle accidents and intimate partner violence (Beck, Jones, Reich, Woodward, & Cody, 2015). The differences between person-centered and variable-based statistical methods, between adult and juvenile samples, and between natural and non-natural disaster traumas may affect the analysis of the comorbidity rate. Therefore, further comparative studies should be carried out to explore specific factors affecting the comorbidity rate.
In this study, intrusion and avoidance were found to be negatively correlated. In particular, Mild Comorbidity Profile includes respondents who reported severe intrusion symptoms but mild avoidance symptoms. This controversial result was also found in previous studies. McCall and Resick (2003) interviewed 20 Kalahari Bushmen (a radical non-Western culture, 10 male and 10 female) who were exposed to domestic violence. All the participants met multiple criteria for the diagnosis of intrusion symptoms, but only one to eight participants met several criteria for avoidance symptoms to varying degrees. Soysa (2013) compared PTSD symptoms among Sri Lankan (nonwestern culture) children who were exposed to war (30 male, 30 female; aged 9–16 years) and the 2004 tsunami (30 male, 30 female; aged 12–14 years). A total of 80% of the war subjects met the intrusion criteria, but only 23% met the avoidance criteria., A total of 85% tsunami subjects met the intrusion criteria, but only 23% met the avoidance criteria. These results may be related to culture. The diagnostic criteria for PTSD have been operationalized primarily in a Euro-American, Western, and industrialized contexts (Marsella, Friedman, Gerrity, & Scurfield, 1996). Whether the diagnostic criteria for PTSD include culture-universal and -specific responses should be further explored (Hinton and Lewis-Fernández, 2011).
This work is a rapid and timely study that was conducted during the outbreak of COVID-19 in Mainland China. However, this work also has limitations. First, when the present study was designed, COVID-19 was only spreading in China. Therefore, the results should not be extended to a wider population. Given the panic and damage caused by the spread of COVID-19 worldwide, the situation became increasingly threatening. Similar studies from other countries and regions were expected to confirm our findings. Second, the symptoms for PTSD appeared after exposure to the trauma. However, as time goes by, the course of them changed. The duration of the symptoms for PTSD (ranging from 3 days to 1 month) is a response pattern of acute stress disorder, while the response pattern of PTSD cannot be diagnosed until it lasts >1 month (American Psychological Association, 2013). The present data were collected 7–14 days after Wuhan declared a lockdown strategy. As the lockdown continued, negative psychological conditions (e.g., fear, depression, boredom, and anxiety) developed among individuals (Brooks et al., 2020). Whether additional severe symptoms for PTSD developed as the psychosomatic condition changed should be further studied. Therefore, a longitudinal database will be established in the next 3–12 months to continue the corresponding research and investigate the occurrence, development, and underlying mechanism of PTSD. Third, many personal (e.g., resilience) (Ying, Wu, Lin, & Jiang, 2014) and environmental conditions (e.g., social support) (Han et al., 2019) that might have an important impact on the development of PTSD and GAD were not included in this study. These possible factors should be included in future studies to help practitioners improve their protective measures for reducing comorbidities.
During the outbreak of COVID-19, epidemiological features, fast transmission patterns, and quarantine can lead to mental health problems, such as feelings of boredom, loneliness, and fear among patients and susceptible individuals. Thus, timely mental health care is urgently needed (Xiang et al., 2020). These findings were expected to help social workers, psychologists, and policymakers to make the evidence-based and targeted decision about interventions that may benefit children and adolescents who are susceptible to COVID-19.
CRediT authorship contribution statement
Yumei Li: Conceptualization, Methodology, Formal analysis, Writing - original draft. Wenjie Duan: Conceptualization, Methodology, Visualization, Writing - review & editing, Supervision, Project administration. Zheng Chen: Investigation, Data curation, Resources.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The study was sponsored by East China University of Science and Technology Supporting Funds for Scientific Research, Strengths-Based Interventions in Multiple Contexts (PI: Prof. Wenjie Duan).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.childyouth.2020.105235.
Appendix A. Information about participant responses to individual items (N = 1172).
| Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|
| PTSD_1 | 0 | 5 | 2.87 | 1.44 |
| PTSD_2 | 0 | 5 | 1.45 | 1.42 |
| PTSD_3 | 0 | 5 | 2.36 | 1.62 |
| PTSD_4 | 0 | 5 | 1.72 | 1.50 |
| PTSD_5 | 0 | 5 | 1.57 | 1.46 |
| PTSD_6 | 0 | 5 | 2.27 | 1.56 |
| PTSD_7 | 0 | 5 | 2.00 | 1.55 |
| PTSD_8 | 0 | 5 | 1.68 | 1.49 |
| GAD_1 | 0 | 3 | 1.07 | 0.91 |
| GAD_2 | 0 | 3 | 1.11 | 1.04 |
| Perceived Threat_1 | 1 | 5 | 2.03 | 1.16 |
| Perceived Threat_2 | 1 | 5 | 2.04 | 1.17 |
| Perceived Threat_3 | 1 | 5 | 2.36 | 1.19 |
| Perceived Threat_4 | 1 | 5 | 3.50 | 1.35 |
| Perceived Threat_5 | 1 | 5 | 2.53 | 1.15 |
| Perceived Threat_6 | 1 | 5 | 2.84 | 1.24 |
| Perceived Threat_7 | 1 | 5 | 3.43 | 1.27 |
| Perceived Threat_8 | 1 | 5 | 3.03 | 1.33 |
| Stigma_1 | 1 | 4 | 1.87 | 0.88 |
| Stigma_2 | 1 | 4 | 1.69 | 0.78 |
| Stigma_3 | 1 | 4 | 1.49 | 0.67 |
| Stigma_4 | 1 | 4 | 1.52 | 0.68 |
| Stigma_5 | 1 | 4 | 1.58 | 0.75 |
Note: PTSD = Posttraumatic stress disorder. GAD = Generalized anxiety disorder symptoms.
PTSD subscales: intrusion (PTSD_1, PTSD_3, PTSD_6, and PTSD_7) and avoidance (PTSD_2, PTSD_4, PTSD_5, and PTSD_8). Perceived Threat subscales: susceptibility (Perceived Threat_1–Perceived Threat_4) and severity (Perceived Threat_5–Perceived Threat_8).
Appendix B. Supplementary material
The following are the Supplementary data to this article:
References
- Abiri S., Oakley L.D., Hitchcock M.E., Hall A. Stigma related avoidance in people living with severe mental illness (smi): Findings of an integrative review. Community Mental Health Journal. 2016;52(3):251. doi: 10.1007/s10597-015-9957-2. [DOI] [PubMed] [Google Scholar]
- Adler N.E., Epel E.S., Castellazzo G., Ickovics J.R. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, white women. Health Psychology. 2000;19(6):586–592. doi: 10.1037/0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- American Psychological Association . 5th ed. American Psychiatric Association; 2013. Diagnostic and statistical manual of mental disorders dsm-5. [Google Scholar]
- Angermeyer M.C., Schulze B., Dietrich S. Courtesy stigma. Social Psychiatry and Psychiatric Epidemiology. 2003;38(10):593–602. doi: 10.1007/s00127-003-0680-x. [DOI] [PubMed] [Google Scholar]
- Asparouhov T., Muthén B. Auxiliary variables in mixture modeling: Three-step approaches using mplus. Structural equation modeling: a multidisciplinary journal. 2014;21(3):329–341. doi: 10.1080/10705511.2014.915181. [DOI] [Google Scholar]
- Batey M., Furnham A. Creativity, intelligence, and personality: A critical review of the scattered literature. Genetic, Social, and General Psychology Monographs. 2006;132(4):355–429. doi: 10.3200/MONO.132.4.355-430. [DOI] [PubMed] [Google Scholar]
- Beck J.G., Jones J.M., Reich C.M., Woodward M.J., Cody M.W. Understanding the role of dysfunctional post-trauma cognitions in the co-occurrence of posttraumatic stress disorder and generalized anxiety disorder: Two trauma samples. Behaviour Research and Therapy. 2015;70:23–31. doi: 10.1016/j.brat.2015.04.011. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinese Center for Disease Control and Prevention (2020, June 30). Covid-19 outbreak distribution. http://2019ncov.chinacdc.cn/2019-nCoV/.
- Cho S., Przeworski A., Newman M.G. Chapter 12 - pediatric generalized anxiety disorder. In: Compton S.N., Villabø M.A., Kristensen H., editors. Pediatric anxiety disorders. Academic Press; 2019. pp. 251–275. [Google Scholar]
- Elrggal M.E., Karami N.A., Rafea B., Alahmadi L., Al Shehri A., Alamoudi R.…Cheema Evaluation of preparedness of healthcare student volunteers against middle east respiratory syndrome coronavirus (mers-cov) in makkah, saudi arabia: A cross-sectional study. Journal of Public Health. 2018;26(6):607–612. doi: 10.1007/s10389-018-0917-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau C.A., de la Torre-Luque A. Comorbidity profile of mental disorders among adolescents: A latent class analysis. Psychiatry Research. 2019;278:228–234. doi: 10.1016/j.psychres.2019.06.007. [DOI] [PubMed] [Google Scholar]
- Fiorillo D., Sabatini F. Quality and quantity: The role of social interactions in self-reported individual health. Social Science & Medicine. 2011;73(11):1644–1652. doi: 10.1016/j.socscimed.2011.09.007. [DOI] [PubMed] [Google Scholar]
- Geng F., Zhou Y., Liang Y., Zheng X., Li Y., Chen X., Fan F. Posttraumatic stress disorder and psychiatric comorbidity among adolescent earthquake survivors: A longitudinal cohort study. Journal of Abnormal Child Psychology. 2019;47(4):671–681. doi: 10.1007/s10802-018-0462-2. [DOI] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the covid-19 pandemic and lockdown. Psychiatry Research. 2020;113264 doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han K.-M., Park J.Y., Park H.E., An S.R., Lee E.H., Yoon H.-K., Ko Y.-H. Social support moderates association between posttraumatic growth and trauma-related psychopathologies among victims of the sewol ferry disaster. Psychiatry Research. 2019;272:507–514. doi: 10.1016/j.psychres.2018.12.168. [DOI] [PubMed] [Google Scholar]
- Hinton D.E., Lewis-Fernández R. The cross-cultural validity of posttraumatic stress disorder: Implications for dsm-5. Depression and Anxiety. 2011;28(9):783–801. doi: 10.1002/da.20753. [DOI] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during covid-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joffe H. Public apprehension of emerging infectious diseases: Are changes afoot? Public Understanding of Science. 2011;20(4):446–460. doi: 10.1177/0963662510391604. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Monahan P.O., Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lai B.S., Kelley M.L., Harrison K.M., Thompson J.E., Self-Brown S. Posttraumatic stress, anxiety, and depression symptoms among children after hurricane katrina: A latent profile analysis. Journal of Child and Family Studies. 2015;24(5):1262–1270. doi: 10.1007/s10826-014-9934-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T.F., Yeung N.C.Y., Yu X.N., Zhang J.X., Mak W.W.S., Lui W.W.S., Zhang J.X. Validation of the Chinese version of the children's revised impact of event scale (cries) among Chinese adolescents in the aftermath of the sichuan earthquake in 2008. Comprehensive Psychiatry. 2013;54(1):83–90. doi: 10.1016/j.comppsych.2012.06.007. [DOI] [PubMed] [Google Scholar]
- Lee S., Chan L.Y.Y., Chau A.M.Y., Kwok K.P.S., Kleinman A. The experience of sars-related stigma at amoy gardens. Social Science & Medicine. 2005;61(9):2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Xu Y., Sun Y., Dumenci L., Seedat S. Measuring hiv stigma at the family level: Psychometric assessment of the Chinese courtesy stigma scales (ccsss) PloS One. 2014;9(3) doi: 10.1371/journal.pone.0092855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.J., Bao Y., Huang X., Shi J., Lu L. Mental health considerations for children quarantined because of covid-19. The Lancet Child & Adolescent Health. 2020;4(5):347–349. doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L.…Liu W. Prevalence and predictors of ptss during covid-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Research. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y., Mendell N.R., Rubin D.B. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. doi: 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- Marsella A.J., Friedman M.J., Gerrity E.T., Scurfield R.M. Ethnocultural aspects of ptsd: Some closing thoughts. In: Marsella A.J., Friedman M.J., Gerrity E.T., Scurfield R.M., editors. Ethnocultural aspects of posttraumatic stress disorder: Issues, research, and clinical applications. American Psychological Association; 1996. pp. 529–538. [DOI] [Google Scholar]
- Marsh H.W., Lüdtke O., Trautwein U., Morin A.J.S. Classical latent profile analysis of academic self-concept dimensions: Synergy of person- and variable-centered approaches to theoretical models of self-concept. Structural Equation Modeling: A Multidisciplinary Journal. 2009;16(2):191–225. doi: 10.1080/10705510902751010. [DOI] [Google Scholar]
- Marthoenis M., Ilyas A., Sofyan H., Schouler-Ocak M. Prevalence, comorbidity and predictors of post-traumatic stress disorder, depression, and anxiety in adolescents following an earthquake. Asian Journal of Psychiatry. 2019;43:154–159. doi: 10.1016/j.ajp.2019.05.030. [DOI] [PubMed] [Google Scholar]
- McCall G.J., Resick P.A. A pilot study of ptsd symptoms among kalahari bushmen. Journal of Traumatic Stress. 2003;16(5):445–450. doi: 10.1023/a:1025702326392. [DOI] [PubMed] [Google Scholar]
- Meiser-Stedman R., McKinnon A., Dixon C., Boyle A., Smith P., Dalgleish T. A core role for cognitive processes in the acute onset and maintenance of post-traumatic stress in children and adolescents. Journal of Child Psychology and Psychiatry. 2019;60(8):875–884. doi: 10.1111/jcpp.13054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo P.K.H., Lau J.T.F., Yu X., Gu J. A model of associative stigma on depression and anxiety among children of hiv-infected parents in China. AIDS and Behavior. 2015;19(1):50–59. doi: 10.1007/s10461-014-0809-9. [DOI] [PubMed] [Google Scholar]
- Nylund K.L., Asparouhov T., Muthén B.O. Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- Perrin S., Meiser-Stedman R., Smith P. The children's revised impact of event scale (cries): Validity as a screening instrument for ptsd. Behavioural and Cognitive Psychotherapy. 2005;33(4):487–498. doi: 10.1017/S1352465805002419. [DOI] [Google Scholar]
- Peters G.-J.-Y., Ruiter R.A.C., Kok G. Threatening communication: A critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychology Review. 2013;7(sup1):S8–S31. doi: 10.1080/17437199.2012.703527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaswamy V., Desarbo W.S., Reibstein D.J., Robinson W.T. An empirical pooling approach for estimating marketing mix elasticities with pims data. Marketing Science. 1993;12(1):103–124. doi: 10.1287/mksc.12.1.103. [DOI] [Google Scholar]
- Ren S.-Y., Gao R.-D., Chen Y.-L. Fear can be more harmful than the severe acute respiratory syndrome coronavirus 2 in controlling the corona virus disease 2019 epidemic. World Journal of Clinical Cases. 2020;8(4):652–657. doi: 10.12998/wjcc.v8.i4.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soysa C.K. War and tsunami ptsd responses in sri lankan children: Primacy of reexperiencing and arousal compared to avoidance-numbing. Journal of Aggression, Maltreatment & Trauma. 2013;22(8):896–915. doi: 10.1080/10926771.2013.824056. [DOI] [Google Scholar]
- Taylor S. Scholars Publishing; Cambridge: 2019. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. [Google Scholar]
- Trickey D., Siddaway A.P., Meiser-Stedman R., Serpell L., Field A.P. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review. 2012;32(2):122–138. doi: 10.1016/j.cpr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Vartti A.M., Oenema A., Schreck M., Uutela A., de Zwart O., Brug J., Aro A.R. Sars knowledge, perceptions, and behaviors: A comparison between finns and the dutch during the sars outbreak in 2003. International Journal of Behavioral Medicine. 2009;16(1):41. doi: 10.1007/s12529-008-9004-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Eriksen Benros M. Covid-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Zou J., Luo J., Liu H., Yang Q., Ouyang Y.…Lin Q. Mental health symptoms among rural adolescents with different parental migration experiences: A cross-sectional study in China. Psychiatry Research. 2019;279:222–230. doi: 10.1016/j.psychres.2019.03.004. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2020a). Coronavirus disease (covid-19) outbreak situation. Retrieved March 22 from https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- World Health Organization (2020b). How does covid-19 spread? Retrieved March 21 from https://www.who.int/news-room/q-a-detail/q-a-coronaviruses.
- World Health Organization (2020c). What is covid-19? Retrieved March 21 from https://www.who.int/news-room/q-a-detail/q-a-coronaviruses.
- Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C.C. Evaluating latent class analysis models in qualitative phenotype identification. Computational Statistics & Data Analysis. 2006;50(4):1090–1104. doi: 10.1016/j.csda.2004.11.004. [DOI] [Google Scholar]
- Ying L., Wu X., Lin C., Jiang L. Traumatic severity and trait resilience as predictors of posttraumatic stress disorder and depressive symptoms among adolescent survivors of the wenchuan earthquake. PLoS ONE. 2014;9(2) doi: 10.1371/journal.pone.0089401. e89401-e89401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo W., Choi D.-H., Park K. The effects of sns communication: How expressing and receiving information predict mers-preventive behavioral intentions in south korea. Computers in Human Behavior. 2016;62:34–43. doi: 10.1016/j.chb.2016.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.