SUMMARY:
During the Severe Acute Respiratory Syndrome Coronavirus 2 (COVID-19) pandemic, neuroradiology practices have experienced a paradigm shift in practice, which affected everything from staffing, workflow, work volumes, conferences, resident and fellowship education, and research. This article highlights adaptive strategies that were undertaken at the epicenter of the outbreak in New York City during the past 4–6 weeks, as experienced by 5 large neuroradiology academic departments.
During the Severe Acute Respiratory Syndrome Coronavirus 2 (COVID-19) pandemic neuroradiology practices have been experiencing a paradigm shift in activities. This disruption has affected everything from staffing to workflow, work volumes, conferences, resident and fellowship education, and research. This article highlights some adaptive strategies that have been undertaken at the United States center of the outbreak in New York City during the past 4–6 weeks, as experienced by 5 large neuroradiology academic departments in New York City. The volume of COVID-19 cases seen at these institutions varies, but the numbers are staggering; while the system has not yet been overwhelmed, there are critical manpower, equipment, intensive care unit (ICU) bed, ventilator, and so forth deficiencies. The system has been taxed, and the medical community has found itself stressed to nearly the breaking point. These adaptive strategies are still relatively fluid but, in some areas, converging on consensus. As this is completed, the admission numbers at many institutions in New York City (NYC) are stabilizing and appearing to decrease, suggesting that a plateau has been reached, and if we are successful in the ongoing attempts at mitigation of the illness, the worst may be over.
Clinical Practice: Staffing
As cases of Severe Acute Respiratory Syndrome Coronavirus 2 (COVID-19) first appeared and then exponentially increased in the NYC metro area, it became clear to the population and finally to government figures that social distancing was required to “flatten the curve.” Academic neuroradiology practices began to limit the number of staff in reading rooms, and as the severity of the pandemic became clearer, many staff members were quickly transitioned to work from home. Many staff members already had at-home PACS, but some neuroradiologists with no at-home PACS were actually allowed to bring their hospital PACS workstation home. This required quick acquisition of many elements of support; hospital and departmental information technology (IT) support was sought because secure data links including virtual private networks, which needed to be established, and often home network upgrades were necessary. Sites reported that they were overwhelming their IT resources to get physicians “up and running” quickly. Most have experienced minimal difficulties with bandwidths available through commercial internet providers, though some hours are very busy with subsequent decreased network speeds.
Radiologists who currently do not do remote interpretation and are anticipating doing so in the immediate future should investigate their provider bandwidth availability and be proactive at obtaining adequate network speed. Sites anticipating a surge are advised to attend to off-site reading requirements (including increasingly scarce equipment such as monitors) as quickly as possible. Conversations with hospital/departmental IT staff are also best done early. The goal has been to keep radiologists healthy and functioning as providers and viable members of the patient-care team.
The number of radiologists required in the hospital setting is based on a number of considerations, including staffing for procedures, the presence for pharmaceutical/contrast administration, overseeing trainees still in-house, and the “visibility” of a radiologist in the hospital, a feature that is uniformly of value. Radiologists remain an essential element of the health care team, and maintaining a presence in the hospital at this time is critical; Working alongside our trainees, technologists, and other staff provides moral support and some functional advantages. The institutions represented here have widely varied approaches to staffing; some divided radiology staff into 2 groups working separately and distinctly (week on, week off), and others limited exposure of older and potentially more vulnerable physicians. All the institutions have tried to ensure that minimal staff were exposed and that necessary access is maintained. When clinical care conferences have continued, video conferencing has proved very reliable and an adequate replacement for in-person meetings. Secure video conferencing methods should be routinely available for this purpose.
Procedural volumes also declined; many biopsy and other outpatient procedures were determined to be nonurgent and of too great a risk for the patient to come to a facility. The necessity for inpatient lumbar punctures, angiography, and/or neurointerventional procedures remains, and either in-house coverage or on-call staff are available for urgent procedures.
Communication is of paramount concern. Our report is our final work product, the actionable result of the study, and must be immediately available and properly delivered. In-house services maintain a normal hospital reporting system, and obviously maintain the delivery of urgent examinations through direct communication with the involved clinical services, but a mirror system of communication must be maintained for off-site interpretation. Because of social distancing, clinical services staff may not access reading rooms with the same regularity as before; many sites have posted information outside reading rooms with all contact information for the radiology staff. Particularly difficult issues have resulted from “displaced” ICU beds and the accompanying staff, often moved to different locations, including previously unused floor space and, on occasion, field hospitals. New lines of communication have been established, but urgent communications from the radiology staff to these areas has proved problematic early on.
As radiology volumes declined and intensive care physician manpower became stressed, the issue of “redeployment” was raised. Within many systems, radiology trainees and staff were reassigned to clinical areas. The wisdom and utility of this as well as the potential broad-ranging ramifications of such reassignment are clearly beyond the realm of this brief report. These staff may be truly working above and beyond their expectations or training. House staff are more likely to be redeployed to clinical services, including ICUs, than faculty. At one institution, neuroradiologists have been part of a “Patient Liaison Team,” connecting with patients’ families for information and support. At other sites, neuroradiologists have performed clerical work as part of clinical teams in ICUs or floors. Other redeployment activities have included participation in workplace health and safety, telemedicine, and elective examination rescheduling teams.
Challenges
Determination of safe and appropriate in-house staffing requirements for residents, fellows, and attending physicians.
Management of consults.
Management of multidisciplinary tumor boards and clinical conferences.
Facilitation of off-site reading for radiologists who were not already equipped for this.
Management of hospital practice committee work/administrative responsibilities.
Active or impending “redeployment” of radiologists.
Recommendations
-
Keep in-house coverage to an appropriate minimum.
Balance concerns regarding the importance of the visibility of radiologist with the need to maintain physician health and well-being.
Ensure that radiologists reading on-site have personal protective equipment (PPE) and maintain appropriate distancing.
-
Maintain prompt, appropriate communication, which is essential.
Easily accessible contact information for all radiology staff, in-house and off-site.
Complete lists of contact information for in-house resources for off-site staff.
Use Microsoft Teams, Zoom, and similar virtual or video conferencing platforms for continuation of multidisciplinary conferences.
Maximize IT support staffing and ensure that IT contact information is readily available.
Recognize that redeployment requests and mandates have been highly variable and system-dependent.
Clinical Practice: Workflow
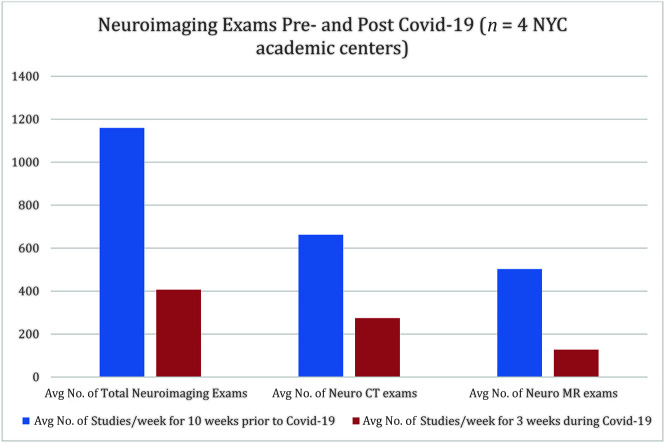
It quickly became apparent that it was unsafe to continue elective imaging, given the risk to patients, technologists, and staff. At 4 of the included academic institutions in the NYC area, the total volume of combined CT and MR neuroimaging cases for similar periods declined by an average of 65% (range, 51%–80.9%). More specifically, neurologic CT volume declined an average of 58.6% (range, 49.3%–72.6%). Neurologic MR imaging volume declined an average of 75% (range, 56.4%–88.6%). Stroke code CT-specific cases declined by 59.7% (range, 32.2%–73.8%) (Figs 1 and 2). Coincident with the reduced elective imaging volumes, there was a need for prioritization of emergent reads to help move patients in and out of increasingly crowded emergency departments.
Fig 1.
Chart demonstrates changes in the weekly average (Avg) of the total number of neuroimaging cases as well as changes in the weekly average of the total number of neurologic CT and MR imaging examinations. This compares weekly average volumes for 10 weeks before the NYC official shutdown to the 3 weeks following the shutdown at the height of the NYC pandemic.
Fig 2.
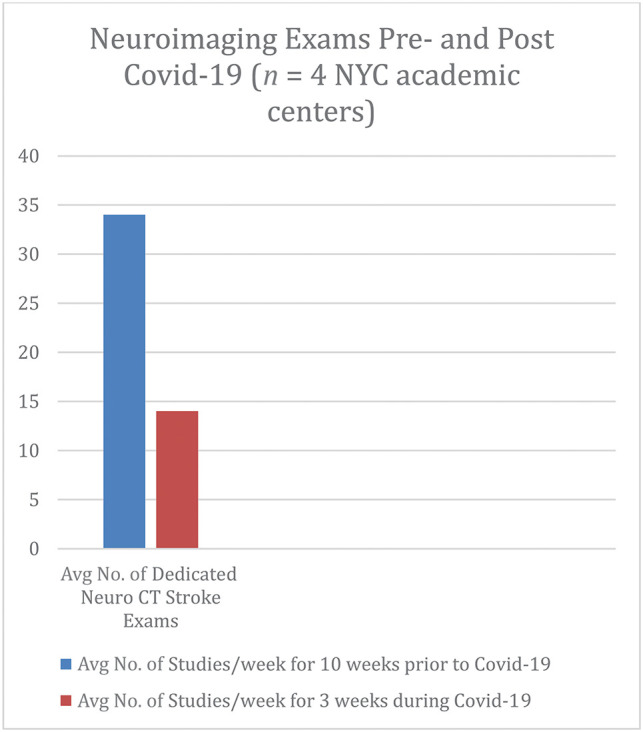
Chart demonstrates changes in weekly average (Avg) of the total number of designated “stroke code” cases. This compares weekly average volumes for 10 weeks before the NYC official shutdown to the 3 weeks following the shutdown at the height of the NYC pandemic.
Elements in the workflow are worthy of individual consideration, allowing for the potential revisions by government regulators. Our reception staff, nurses, and technologists are particularly affected by patient care changes in the era of COVID-19. Redeployment of nursing personnel to clinical units has removed nursing staff from radiology. Furloughs and layoffs have occurred. These staff can also become infected and require quarantine or hospitalization. All our institutions were aggressive early in reviewing patient examination lists and identifying and rescheduling nonurgent examinations. The radiologists’ review of these requests required much time, and rescheduling remains a work-in-progress. Protocols to manage scheduled and future examinations are being created or have already been instituted. Triage requires physician input; in many cases, additional communication with referrers is necessary to gauge the urgency if not evident from requisition and electronic medical record data. We have worked to maintain safe access to imaging for patients undergoing examinations to monitor and treat oncologic diagnoses.
There have been challenging issues in designating sites for patients with known COVID-19, and other sites for noninfected patients. While there may be some benefit to designating a site for only patients with known COVID-19, the incidence of asymptomatic and afebrile patients, who unknowingly are COVID-19 positive, is problematic at sites that intend to remain for noninfected patients. All staff will be properly equipped with PPE and will practice appropriate distancing. When patients arrive for scanning deemed urgent, sites have incorporated screening before patients can access imaging suites. Social distancing in waiting areas is reinforced. The discovery of a patient with potential COVID-19 on any scanner is a major issue; the patient must be isolated, staff may require quarantine, and the scanner must be cleaned by a defined protocol.
It has been observed that turnaround time data will definitely show a unique perturbation based on the COVID-19 pandemic. Declining volumes and staff reading in real-time are the cause. These have led to issues in workflow—some are positive, but others are not. A rapid turnaround time is good for patient care and particularly positive in the emergency department. However, the “urge” of attending staff to grab an examination from a worklist and read it (the “Hungry Hippos” analogy, Fig 3) has been evident. This clearly detracts from resident/fellow education. Allowing trainees to generate preliminary interpretations is a necessary part of training programs and should continue.
Fig 3.
This analogy and tweeted image are borrowed with the courtesy of Daniel Ortiz, MD, Summit Radiology Services, Cartersville, Georgia. ED indicates emergency department.
Challenges
Triage of previously scheduled and new requests for outpatient imaging.
Reduction in available technologists and support staff because of illness and quarantine following exposure or redeployment.
Machine/room contamination by known or later-discovered patients with COVID-19.
Absolute decline in case volumes in neuroradiology.
Recommendations
Continue to prioritize reading of emergency department studies; a low emergency department turnaround time helps providers move patients from this risky setting.
-
Create a protocol to manage outpatient imaging.
Every patient kept out of an imaging facility and in their homes is a potential “save” during this pandemic.
Assemble a radiologist team to triage elective outpatient studies.
-
Move all outpatient imaging out of hospitals and into imaging centers; reduce the number of operating imaging centers to reduce staffing requirements.
Keep technologists/other staff to a minimum and enforce appropriate quarantine practices.
Maintain appropriate PPE and precautions for all staff and patients.
Define protocol for machine/room cleaning after contamination by patients with COVID-19.
In hospital and outpatient centers, when possible, designate scanners or sites for patients under investigation.
Assign a smaller number of primary/backup readers and instruct others to do nonclinical (research, teaching, administrative) work.
Resident and Fellow Education
Because minimizing radiologists physically at the hospital was necessary, multiple challenges ensued regarding continuing resident and fellow education. An initial move to remove as many residents as possible from the hospital setting was followed by a “redeployment” of physicians, with residents and fellows reassigned to clinical service. This redeployment resulted in confusion and anxiety among house staff and interfered with their availability to participate in educational radiology activities. Additionally, postponement of American Board of Radiology examinations has changed the learning paradigm for senior residents.
Much of radiology learning has been “shoulder-to-shoulder” case review with an attending physician, as well as didactic teaching, case review, and unknown case presentations. This form of education has been largely halted. Trainee numbers in the reading rooms have diminished, and social distancing has interfered with traditional training methods. The dispersal of staff and residents necessitates video conferencing.
Staff have quickly become familiar with video conferencing for teaching. While not a perfect system, it does at least allow widely spread trainees to be involved and the educational mission of the system to continue. Trainees have also requested a more permanent archive of the material; providing a PDF or other augmented text file of lectures allows the material to be durable and residents who may be redeployed to have access to the material. Some sites have also recorded lectures. On-line teaching materials are also available.
The decrease in volume may impact resident training. As previously mentioned, staff taking cases from clinical worklists that were previously preliminarily reviewed by a trainee is an issue. Encouraging staff to allow the normal workflow in clinical areas seems an unusual problem, but clearly staff feel pressure to be active and turn examinations around quickly. Trainees benefit from case review and formulating an opinion; this system should be maintained if possible.
Challenges
Continuing resident/fellow conferences via online or video conferencing.
Providing enhanced opportunities for on-line education.
Mitigating the impact of reduced case volume on resident and fellow education.
Mitigating the impact of redeployment on resident/fellow education and well-being.
Recommendations
Move resident and fellow teaching conferences to on-line video conference formats (Zoom, Skype, and so forth).
Revise existing syllabi for continued on-line learning to maintain levels of medical student/resident/fellow training.
Encourage attendings to allow residents/fellows to provide standard preliminary interpretations, while facilitating turnaround times.
Be consistent in communication between training program directors and trainees, which is essential to ensure ongoing learning and reduce stress.
Research
In a dystopian fashion, COVID-19 has presented a research opportunity for imaging physicians and a huge roadblock to ongoing or planned research. Institutional review boards have typically been receptive to COVID-19 research (active clinical outcomes practices that combine “learning” as well as “doing” treatments), advocated data collection for subsequent retrospective analyses, and are remaining active during this time to allow researchers the opportunity to begin studies. On the other hand, institutional review boards have prohibited other unrelated ongoing research protocols that involve healthy controls in the hospital/clinic setting from continuing. Clinical trials that involve administration of drugs on a defined schedule, particularly in oncologic care, have largely continued.
Many institutions have moratoriums on sharing electronic medical records with other institutions. This policy clearly stems from the past inadvertent release of PHI and existing legislation to protect confidential patient data, but the restriction can also have deleterious effects. For example, if all NYC academic centers wanted to share the electronic medical records of patients with COVID-19 for the development of artificial intelligence (AI) algorithm tools for triage or outcomes research, this collaboration would be highly restricted at present.
Some centers have instituted special review institutional review board panels to handle any COVID-19–related research in an effort to centralize the process and avoid repetition (and potentially link up like-minded projects), to prevent overwhelming institutional review boards. At least 2 institutions are using an expedited process for any clinical or translational research related to COVID-19, particularly drug trials. Some institutions have also used a blanket institutional review board for data collection on all patients with COVID-19 performed across their network to ease collaboration and reduce the workload on institutional review boards.
It is impossible to over emphasize the value of ongoing communications among providers, researchers, associated staff, and patients and research subjects during this time. A clear discussion among those involved with ongoing research during a potential hiatus is a necessity. Departments are also in a position to leverage downtime from clinical activities to the benefit of research; additional academic and/or nonclinical time that can be used to complete research, apply for grants, and so forth is of immense value to academic physicians.
Challenges
Handling enormous volumes of data that are being generated on patients with COVID-19.
Avoiding potential exposures of research subjects.
Maintaining viability of ongoing research work.
Recommendations
Departments and organizations must collect a wide range of data on patients with COVID-19 in a systematic data-mineable fashion.
Ongoing clinical trials using imaging should ideally be segregated from interaction with potentially infected outpatients or hospitalized patients.
Organize/communicate with other institutions with experience with the disease to pool findings.
Communicate with patients in active studies to keep them enrolled.
Avoid loss of data in longitudinal studies as practicable.
Use downtime to complete ongoing projects to the extent possible and increase academic productivity.
Conferences and Meetings
As expected, during the pandemic, many planned meetings have been cancelled, postponed, or are being held in a “virtual” format. Most health care networks have restricted travel related to business. Several institutions ruled that physicians with scheduled time away for meetings that were canceled were unable to reschedule the time as work time and were bound to take the time off though travel was prohibited; this ruling was to avoid the expected backlog of travel and conference time when meetings are again scheduled and may overlap with the expected volume rebound of imaging studies that have been postponed. There is discussion of continued restrictions on vacation and meeting time allowances at some institutions after the “curve is flattened,” again because of the expected rebound. These restrictions may impact attendance at future meetings. If restrictions to travel remain in place, neither speakers nor participants may be able to attend. It is not possible for large meetings to nimbly change venues in response to a rapidly changing pandemic, and there is no guarantee that air travel will resume with normal schedules.
The disruption of academic meetings is a small part of this problem, but one that may have real economic repercussions. Attendance at and involvement in large medical meetings are an important element in academic advancement and promotion and tenure. The potential economic benefit to cities hosting meetings is also considerable. A large number of medical meetings (American Roentgen Ray Society, American Society of Neuroradiology, European Society of Head and Neck Radiology, among others) have either canceled their planned physical meetings, are attempting virtual meetings, or are postponing their meetings until later and hopefully achievable dates.
The virtual meeting plan has had numerous advocates, but issues remain with nondedicated time to attend a virtual meeting while still working on a clinical service. Data security and privacy are concerns with virtual meetings. The infamous “Zoom bomb” has been widely reported in the press and can be disruptive as well as a security concern. Prerecorded lectures as well as conferencing platforms are means of carrying out the educational mission of a meeting, and discussions can be via on-line platforms. Interruptions obviously occur and can be catastrophic, depending on where in the chain they occur, but are fortunately relatively uncommon. Some organizations have relied on podcasts and other digital formats to perform their academic missions, some with relative success. Canceled meetings are an anathema to organizations that benefit from the interactions and activities of these meetings, to say nothing of the potential loss of revenue. Postponing a meeting can lead to a less-than-optimal rescheduling, overlap with other meetings also being rescheduled, and pose the additional risk of a second or third wave of COVID-19.
Challenges
Planning in advance to attend meetings in late summer or fall that are in jeopardy of cancellation.
Scheduling future time away, which will be difficult with multiple other staff similarly looking at future meeting times, work volume rebounds, manpower requirements, and so forth.
Planning future meetings given the new COVID-19 reality.
Maintaining security with virtual meeting content.
Recommendations
Be proactive and plan a virtual meeting backup in anticipation of disruptions from local disease outbreaks, economic impact, and work-related restrictions on employee movement.
Condense meetings to a 1-day virtual workshop/on-line forum with restricted participation or make meeting lectures available on-line.
Provide security for virtual meeting content.
Physician Well-Being
There is omnipresent stress in an environment where an unseen pathogen is seemingly “stalking” you. Radiologists are often tagged as “loners” but, in fact, practice in constant communication with others: staff, technologists, nurses, and trainees. Staff who have typically been close to one another, surrounded by other staff and trainees, interacting with these individuals as a part of their practice, now find themselves sheltered in place at home, reading remotely. There are no lunch breaks, no shared time for coffee, and minimal interactions with anyone. Limited hospital manpower reserves also added another stress to radiologists: the uncertainty of being “redeployed” or reassigned to an area of medicine where they are minimally competent or untrained. Morale has definitely declined.
Physicians previously proud of their clinical volumes may be “out of the loop” and acutely aware of the lack of productivity forced on them. Many of us have seen an aggressive approach to worklists: taking cases from lists when the examinations were not completed and staff taking cases before trainees have an opportunity to review them.
The issue of ego and well-being is personal. Finding a way to keep in touch with friends, colleagues, and acquaintances during this period requires effort. How one chooses to engage with others is not the issue; remained engaged with others is the issue. Phone, e-mail, texts, video chats, and so forth are viable. It is a good time to refresh old friendships. If you are a social media fan, the platforms are varied and can be useful, but clearly using social media to air issues with hospital administration, fellow staff, or others can be a potential landmine. A few moments to review hospital or system policies regarding social media can be valuable, particularly if one is frustrated and irritated. Outlets to reduce stress are also a personal issue, but as long as the outlet is not ultimately deleterious, whatever works for you is likely good. A widely held opinion echoed recently is that a crisis serves to pinpoint many hidden system problems. A useful means to handle that stress is to identify those problems and work to find solutions. An administration that openly and frequently communicates with the physicians contributes to a more positive view of the situation, reduces uncertainty, and lessens stress.
Stress that seems unbearable needs to be recognized as a problem, and help should be sought. Many of our systems have engaged support services and mental health professionals and made them available. There is no shame in seeking help for an issue that is so widely disruptive to society as we have known it.
Challenges
Lack of social interactions.
Stress and anxiety over work, health, and society.
Loss of productivity in the workplace.
Guilt.
Recommendations
Find ways to interact.
Know your institutional policies regarding media when discussing or providing opinions on administration decisions or practices.
Find useful/creative/constructive outlets to reduce stress.
Alert staff to signs of excessive stress and anxiety; facilitate access to behavioral health services when they are needed.
Work locally to address shortcomings in pandemic re-sponses. Some have advocated a “postpandemic” committee to review concerns and provide recommendations. Well-conceived and organized plans may move beyond local or regional to national significance. A “pandemic panel” to address all issues identified for improving the ability of physicians to express concerns through the American College of Radiology, Radiological Society of North America, American Society of Neuroradiology, or other organizations may be a useful outcome of this event.
Keep open communication lines between administration to staff. This is of paramount importance.
Long-Term Plan (Aftermath)
The isolation and its consequences will clearly end, and a return to normalcy in work and life will occur, though with differences, both expected and unexpected. Gearing up the medical imaging world will take time but is expected to return to prepandemic levels with a significant pent-up demand that could generate considerably increased short-term volumes. Social distancing and other factors may influence our practices for some time. The other mitigating factor here is the increase in unemployment, with loss of medical benefits that some may encounter. With the pandemic having exposed some weaknesses in the current imaging methodology, changes can be expected in the way we work. Off-site imaging has clearly proved its efficacy.
Challenges
Anticipated increase in workload when imaging returns.
Expected period when no/minimal travel or meetings will be allowed, given this potential period of increased volumes.
Recommendations
Sites may contemplate extended hours and increased availability for imaging services after restrictions are lifted.
Practices will likely increase access to PACS resources in-home and off-site.
Physicians will need to have flexibility in time-off schedules
Conclusions
Dealing with COVID-19 remains a work in progress, but there is a consensus that during surge periods, radiology departments will need to keep most staff off-site working from remote workstations, maintain but minimize their presence at hospitals for procedures and consults, minimize outpatient imaging for safety, maintain education of trainees, gather data on the disease to hopefully facilitate treatment of this ongoing episode or future pandemics, and enhance connectivity within the neuroradiology department and with neurologists, neurosurgeons, and head and neck surgeons by all means available to maintain patient care. When the pandemic worsened, systems have not hesitated to use deployment to either remote or clinical work as the volume of work in the more seriously affected areas reached a threshold by which staffing and subsequently patient care were challenged. We acknowledge our clinical colleagues who have faced this pandemic directly; they are truly performing a service that is of astounding risk and scope. We also acknowledge our radiology colleagues who have been reassigned to clinical areas to provide, in some cases, direct care to patients with this disease. Neuroradiology remains a critical support service for our clinical colleagues and for patients hospitalized with COVID-19.
ACKNOWLEDGMENTS
We extend special thanks to Keith Hentel, MD (Weill Cornell Medical College, NewYork-Presbyterian Hospital, New York City).
ABBREVIATIONS:
- ICU
intensive care unit
- IT
information technology
- NYC
New York City
- PPE
personal protective equipment
- PHI
protected health information