ABSTRACT
Telemedicine use in the field of wound care had been increasing in popularity when the novel coronavirus 2019 paralyzed the globe in early 2020. To combat the constraints of healthcare delivery during this time, the use of telemedicine has been further expanded. Though many limitations of telemedicine are still being untangled, the benefits of virtual care are being realized in both inpatient and outpatient settings. In this article, the advantages and disadvantages of telemedicine are discussed through two case examples that highlight the promise of implementation during and beyond the pandemic.
KEYWORDS: coronavirus, COVID-19, telehealth, telemedicine, wound care
INTRODUCTION
At the start of 2020, the world found itself grappling with an unprecedented global pandemic: the novel coronavirus 2019 (COVID-19). The first case in the US was discovered on January 20th in Washington State.1 Since then, the country has seen an exponential increase in the number of cases, reaching over 1.4 million as of May 16, 2020.2 With this, the medical community has quickly adapted to meet the needs of patients while balancing adherence to social distancing and containment practices. It has pushed many once-hesitant clinicians to adopt telemedicine, posing the question: will COVID-19 be the impetus for more widespread use of telemedicine?
Telemedicine is the remote delivery of healthcare via electronic communication tools such as smartphones or videoconferencing. Telemedicine visits have increased dramatically from 2005 to the present,3 with 76% of hospitals fully or partially implementing computerized telehealth systems as of 2017.4 At the same time, American patients are becoming more amenable to these changes in healthcare delivery, with a 2019 survey finding that 66% of consumers are willing to use telemedicine.5 More specifically, in the midst of the COVID-19 pandemic, population-level interest in telemedicine has increased dramatically as the number of COVID-19 cases in the US has risen.6
For wound care, telemedicine provides a particularly well-suited alternative to managing patients in person during and beyond the COVID-19 pandemic. Through photography and video-based communication, healthcare providers can obtain a detailed history, visually assess the wound, and answer any questions in a similar fashion to a face-to-face visit. These telemedicine practices can be applied to both inpatient and outpatient settings, with obvious advantages and disadvantages compared with traditional in-person medicine. Overall, virtual care grants patients access to timely and necessary wound management while preventing person-to-person spread of the virus, protecting both patients and providers.
The outpatient case exemplar included in this manuscript provided written authorization for publication of the accompanying images and case details. The inpatient case study has been anonymized to protect the identity of the patient.
LIMITATIONS OF TELEMEDICINE
When looking at the application of telecommunication to healthcare delivery, there are clear advantages and disadvantages (limitations) compared with traditional face-to-face medicine. Focusing first on the general limitations of telemedicine (Table 1), there are sometimes technological difficulties that arise when using computers, tablets, or smartphones.7,8 These glitches detract from the clinical visit and can cause inefficiencies in healthcare delivery. At the same time, it is important to acknowledge that many patients do not have access to the necessary infrastructure (eg, video-enabled devices or high-speed internet) to participate in telemedicine.
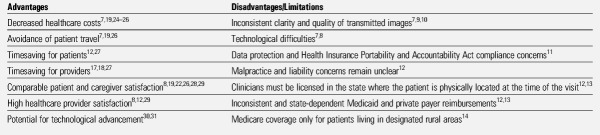
Table 1.
TELEMEDICINE ADVANTAGES AND DISADVANTAGES PRIOR TO COVID-19
The provider-patient relationship is seated in establishing a strong bond and human connection that ultimately builds trust. It is possible that telemedicine, through faulty photography, online messaging, or videoconferencing, can hinder the rapport that every clinician strives for. For example, there can be inconsistencies in the quality of transmitted images.7,9,10 Frequently, telemedicine makes use of patient-generated images, which vary in relation to clarity, lighting, position, background, and camera quality. If the images are too poor in quality for use, these factors can ultimately hinder the provider’s clinical decision-making.
In addition, telemedicine providers are responsible for patient data protection and Health Insurance Portability and Accountability Act (HIPAA) compliance at every step of the process. This requires protected electronic health records (EHRs) and secure videoconferencing systems, which can pose a challenge in a complex internet-driven world.11 However, telemedicine is largely uncharted territory, with little legal framework or case law to guide the standard of care in the delivery of remote health services. For this reason, malpractice and liability concerns for doctors and nurses remain unclear.12 For example, if an incomplete assessment is performed by a patient or their caregiver, and this influences the recommendations of a wound specialist, it can leave the practitioner open to liability.
Other challenges posed by nascent telemedicine practices include insurance reimbursements for telemedicine visits, virtual check-ins, and e-visits. Medicaid and private payer reimbursements vary from state to state, with many hospitals relying on grants to fund telemedicine programs.12,13 The inconsistency in service requirements for each type of visit, and at what levels that visit will be compensated, is complicated for providers and patients alike. Prior to the COVID-19 pandemic, the Federal government stipulated that Medicare coverage of telemedicine was only for patients living in designated rural areas,14 which is only a small percentage of the US population. A final general caveat is the regulation that providers must be licensed in the state where the patient is physically located at the time of the virtual appointment.12,13 This poses a problem for patients who require care across state lines, unless the provider is also licensed or has reciprocal licensure in the patient’s specific state (compact states). However, during the current pandemic, these laws have been loosened, which is discussed further below.
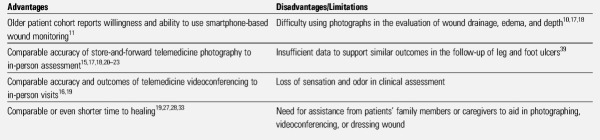
Wound Evaluation Considerations (Table 2)
Table 2.
TELEMEDICINE WOUND EVALUATION
Telemedicine may not be appropriate for initial wound assessment, complex wounds, or ischemic and/or deteriorating wounds. Challenges in comprehensive wound assessment using telemedicine can include the assessment of undermining, tunneling, temperature differences, and odor. Further, if the patient or caregiver cannot or will not perform needed wound care, then telemedicine may not be appropriate, and an in-person or in-office visit to evaluate a new level of care may be warranted. Education on proper wound care must be available and provided (if not already in place). In these cases, an in-office or emergent in-person visit may be necessary. Ultimately, telemedicine may be limited to established patients, stable wounds, and/or maintenance wounds.
The limitations of telemedicine specific to wound care are primarily related to the loss of some of the senses needed for clinical examination. Touch and odor are lost in telecommunication, although patients can be asked a set of clinical questions to circumvent this challenge. Most studies have shown that video and photographic evaluation of wounds are comparable to in-person assessments;15–23 however, these studies have also shown that the evaluation of wound drainage,10,17 edema,17 and depth18 are more difficult via these media. Patients also have the added challenge of photographing wounds in difficult locations, such as the sacrum. In these cases, there is often a need for assistance from a family member or caregiver to aid in the telecommunication or dressing changes. Many patients do not have this support at home, especially when social distancing guidelines are in place.
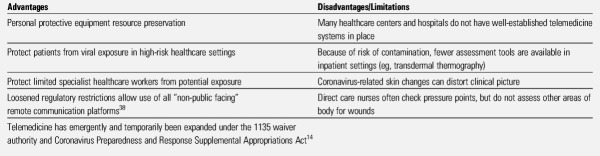
COVID-19 Considerations (Table 3)
Table 3.
TELEMEDICINE AND COVID-19
The pandemic has highlighted the intersection of wound care and telemedicine. In these times, the medical community has quickly adapted to fit the needs of an overburdened healthcare system. Large medical centers have focused on expanding their existing telemedicine systems to continue seeing patients; however, it is important to acknowledge that many healthcare centers do not have such established resources. Telemedicine programs require money, time, and training to implement, which may be impossible at a time when revenues are down, time is at a premium, and in-person training is difficult. Telemedicine is not necessarily a “quick fix” for all providers across the country.
ADVANTAGES OF TELEMEDICINE
Telemedicine has many general advantages compared with in-person medicine (Table 1). Numerous studies have cited the cost benefits of telemedicine, stemming from decreased travel, decreased staff nonproductive time, and increased efficiency of appointments.7,19,24–26 Michaud and colleagues’25 2018 systematic review of home-based telemedicine programs highlighted reduced costs in all of the included studies, although they cautioned that the extent of the savings required more inquiry.
In addition, telemedicine circumvents a major barrier for many patients: travel to and from healthcare centers.7,19,26 It allows remote delivery of services to those who are immobile, cannot drive, live in rural areas, or cannot drive or travel for other reasons. These virtual visits lead to a time-savings for both providers (eg, decrease downtime and inefficiencies) and patients (eg, decrease travel and wait times).12,17,18,27 These appointments also provide for those disadvantaged populations who can only take time during a scheduled break or are confined to their home during regular clinic hours because of a lack of adequate childcare. Overall, telemedicine has comparable patient8,19,22,26,28,29 and provider satisfaction8,12,29 in relation to face-to-face healthcare delivery.
Healthcare systems have only begun to scratch the surface of telemedicine’s benefits. The potential for technological advancement in the field is unbounded30,31 as medical devices and smartphones push the limits of what services can be delivered remotely (see the next section).32
Wound Evaluation Considerations
The current literature on wound evaluation via telemedicine is largely positive (Table 2). Numerous studies have shown that store-and-forward photography, a form of asynchronous communication in which a patient-provided image is stored in the EHR for the provider to view at a later time, to be accurate in wound assessment.15,17,18,20–23 Similarly, live videoconferencing has comparable accuracy and outcomes to in-person examination.16,19 There is also some evidence that telemedicine can provide an equal, or even shorter, time to healing than is seen with in-person clinical examinations.19,27,28,33 Combined, these studies support the expansion of telemedicine.
Telemedicine is most frequently delivered through smartphones and computers, devices that most Americans already have access to, adding no extra costs or hurdles before a patient begins use. However, many patients with wounds tend to be older adults with comorbid conditions, a population who may not be the most comfortable with smartphone and computer use. That said, Wiseman and colleagues found that this population not only has access to smartphones, but also is willing to use them for at-home wound monitoring.11 Essentially, the demographic of patients with chronic wounds are likely amenable to adopting telemedicine practices into their healthcare.
Looking at technological advancement from the perspective of wound care, smartphone health applications, wireless devices, and sensor-based technologies are already being applied to the field.34 Three-dimensional imaging35,36 and smartphone-enabled wound temperature monitoring34 are two examples currently being studied. Telemedicine has the potential to introduce these technologies into virtual visits as they become more readily accessible, which would allow for greater precision in the remote analysis of wounds and ultimately higher-quality care through expanded clinical information.
COVID-19 Considerations
The role of telemedicine has been previously discussed in the context of the medical response to national or global disasters.37 Since the beginning of the pandemic, there has been a surge in the use of telemedicine in response to COVID-19 (Table 3). The most intuitive benefit of this form of healthcare delivery is preventing exposure to the virus. In the outpatient setting, patients are understandably hesitant to visit high-risk hospital and healthcare settings, but still need care for their wounds or other nonemergent ailments. Conversely, healthcare workers and clinical specialists are vital resources who should not have to face unnecessary risk. Telemedicine enables nonemergent patients to be assessed by their providers without the risk of exposure. The same applies to the inpatient setting, where telecommunication can limit the number of healthcare workers entering patient rooms. This curtails potential infection and decreases the potential for spread among patients. Further, telemedicine can reduce the use of in-demand personal protective equipment (PPE).
Critically, the US government has noted the value in expanding telemedicine during this global crisis to preserve resources and contain the spread of the virus. Telemedicine has emergently and temporarily been expanded under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act.14 Under this legislation, the CMS has broadened access to telemedicine services in the hopes of relieving current stressors on the healthcare system. Medicare now can pay for telemedicine usage for all Medicare-covered patients in the US. These services are paid at the same rate as in-person visits and cover a multitude of providers including physicians, nurses, physician assistants, clinical social workers, and more. At the same time, the US Department of Health and Human Services has loosened HIPAA guidelines to allow providers to better serve patients during the COVID-19 pandemic, including the delivery of remote healthcare services via audio or video on private applications such as FaceTime (Apple Inc, Cupertino, California), Google Hangouts (Google Inc, Mountain View, California), Zoom (Zoom Video Communications Inc, San Jose, California), Skype (Skype Communications SARL, Luxembourg), or Facebook Messenger (Facebook Inc, Menlo Park, California).38
OUTPATIENT CLINICAL EXAMPLE: SURGICAL WOUND DEHISCENCE
A 42-year-old man who was managed by the authors’ wound center for nonhealing surgical wound dehiscence following abdominoplasty tested positive for COVID-19. The patient was receiving certified home healthcare agency (CHHA) services every week. Given this patient’s positive coronavirus status, he was scheduled for a telemedicine follow-up visit with a wound care specialist. At the time of the appointment, both the physician and patient logged into the video conference via a HIPAA-compliant secure EHR platform, where a standard history was taken (Figure 1).
Figure 1.
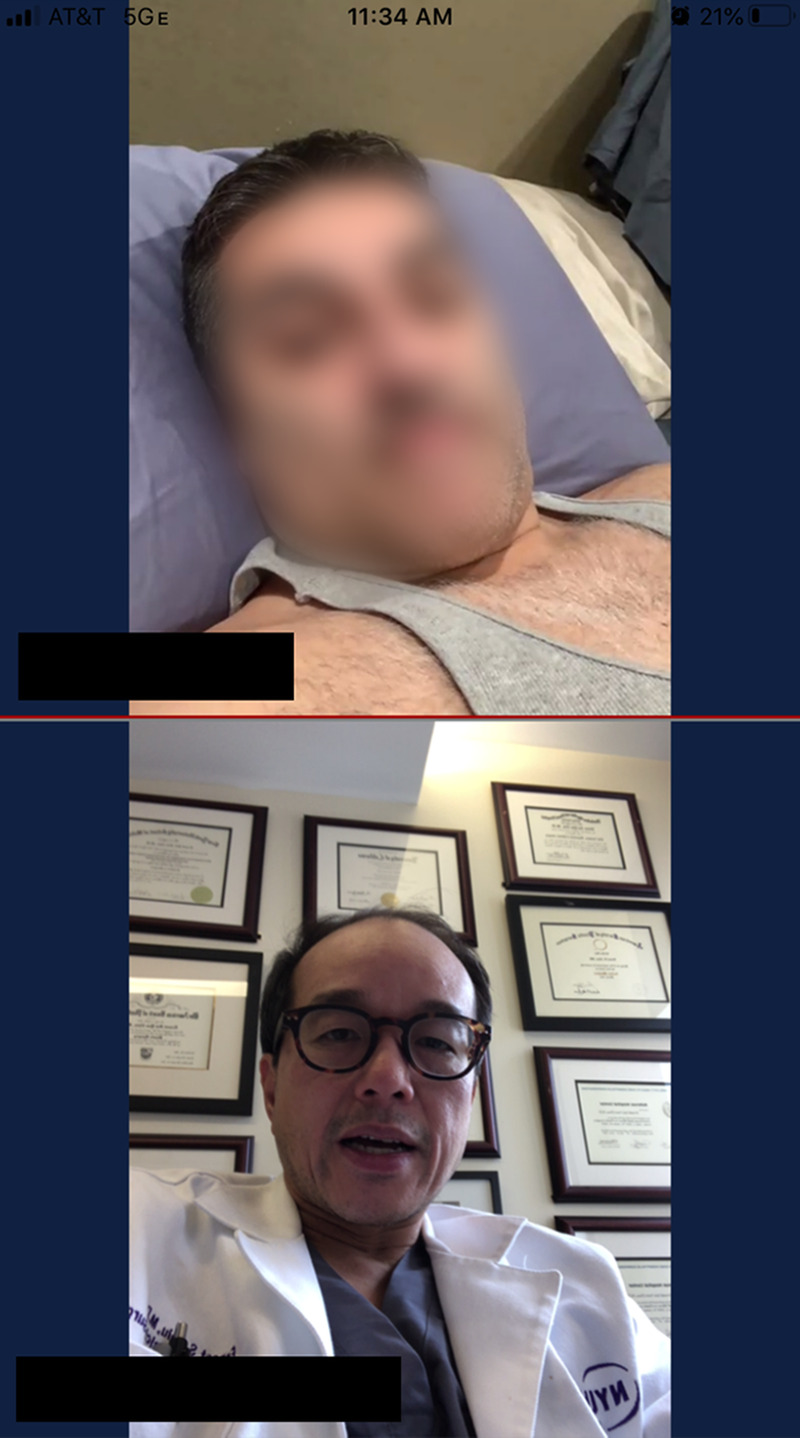
OUTPATIENT VIDEOCONFERENCE
Before the visit, the patient had been instructed to photograph the wound and send the image through the institution’s secure EHR (Figure 2). This allowed the medical team to preliminarily assess the wound before the scheduled video call. After the patient’s history was reviewed, he was instructed to take a video the wound with his wife’s assistance. This allowed the physician to assess the clinical appearance of the wound bed, including the color, location, and surrounding skin (Figure 3). In addition, the physician asked the patient a series of directed questions to further assess the wound. The wound dimensions were assessed using a standard 4-inch by 4-inch gauze sponge in lieu of a ruler (Figure 3). Similarly, the patient was instructed to use a sterile cotton-tipped applicator to approximate the wound depth. The physician further inquired about fever, site pain, exudate, tunneling, undermining, and odor. In this case, specific questions in conjunction with the photographed images clarified wound status.
Figure 2.
PATIENT-GENERATED SMARTPHONE PHOTOGRAPH
Figure 3.

TELEVIDEO WOUND EVALUATION
Using the virtually-obtained history and physical examination combined with the physician’s clinical judgement, the physician instructed the patient on an appropriate dressing and its proper application, including how to maintain aseptic technique at home (Figure 3). Wound care orders were prescribed and endorsed to the CHHA, including how to provide wound care and monitor for deterioration of wound status through weekly wound measurements. The CHHA also continued education through “teach-back” of appropriate wound dressing. The CHHA subsequently ordered the materials for the patient.
The patient was scheduled for a follow-up telehealth visit per the clinic’s pre-existing guidelines (every 2 weeks). The patient and caregiver were educated to contact the clinic for any signs of deterioration or any concerns via the EHR communication tool or by calling the clinic directly. This information was provided verbally and in the EHR after-visit summary. In addition, the patient was informed that written materials would be provided via the US Postal Service if he could not access the EHR materials.
INPATIENT CLINICAL EXAMPLE: PRESSURE INJURY AND COVID-19
A 72-year-old woman with a past medical history of noninsulin-dependent diabetes mellitus and hypertension presented to an urgent care center with obesity, cough, fever, and progressive shortness of breath on exertion. Upon referral to the ER, she demonstrated severe acute hypoxemic respiratory failure and was diagnosed with COVID-19. She was intubated and a nasogastric tube was placed to provide enteral feeding. Her hospital course was significant for Escherichia coli pneumonia, acute nephrotic syndrome, septic shock requiring IV antibiotics, vasopressors, and respirator use. The patient was noted to have dual incontinence, which was managed using hygiene and an external female urinary incontinence device.
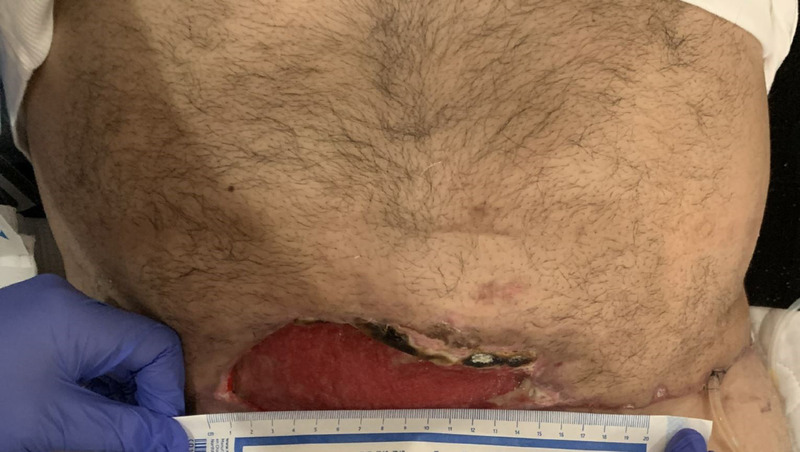
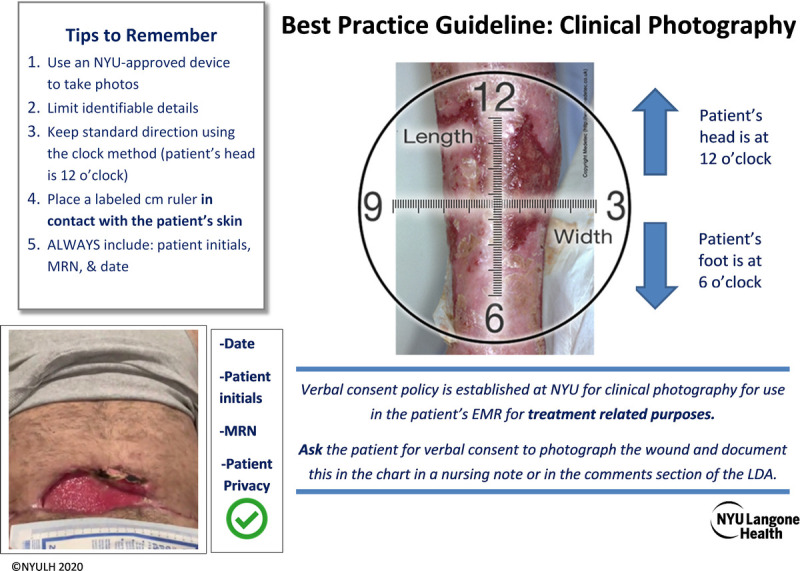
Two weeks later, direct care staff assessed the patient as having altered skin integrity of the buttocks presenting as a “pink, irregularly bordered partial-thickness wound.” They took clinical photographs of the region according to best practice guidelines (Figure 4). The wound, ostomy, and continence (WOC) nursing service regularly audits the EHR reporting tool and during one of these reviews noted documentation of a “pressure injury” for this patient. (This method allows any pressure injuries that are recorded by the direct care staff to be reviewed by WOC specialists for accuracy and as a method of checks and balances in case a notification is omitted.) The WOC nursing service then reviewed the full chart, including the patient’s physical examination, past medical history, goals of care, past surgical history, medications, recent social history, pertinent laboratory tests and imaging, and clinical course after admission. Upon evaluation of the clinical photograph, the WOC team noted the patient had a well-localized sacral full-thickness wound with regular wound borders, scant serosanguinous exudate, intact normopigmentated periwound, no undermining or tunneling, and open wound edges. Half of the wound bed had soft, brown, adherent necrotic tissue and half comprised moist, red, granular tissue. Per the nursing report, there was no foul odor, although this finding was questionable given the staff were wearing full PPE during the evaluation. There were remnants of intact nonblanchable violaceous discoloration at the wound borders consistent with an evolved deep-tissue pressure injury. This diagnosis also was consistent with the clinical presentation and history of events—intubation, nasogastric tube feeds, and so on.
Figure 4.
CLINICAL PHOTOGRAPHY BEST PRACTICE GUIDELINES
© NYULH 2020. Reprinted with permission.
The WOC team had several recommendations:
fecal incontinence containment using an internal fecal management system
regular skin assessment at least once per shift
continued risk assessment to individualize the plan of care
turning and repositioning based on the patient’s clustered care
offloading of the sacral area at all times using positioning devices such as wedges and pillows
further moisture management using a low-air loss integrated specialty mattress with kinetic therapy and continuous lateral rotational therapy for pulmonary toileting
comprehensive nutrition evaluation and supplementation to support wound healing
In this case exemplar, a comprehensive wound assessment and appropriate interventions were achieved in conjunction with direct care staff. Telemedicine limited additional potential exposures and inadvertent spread of the virus while preserving PPE resources. If the providers had not achieved a thorough wound assessment from the clinical photographs and documentation, an in-person visit would have been considered using proper safety precautions.
DISCUSSION AND CURRENT RECOMMENDATIONS
Even before the onset of this pandemic, the benefits of telemedicine had been continuously publicized: from cost7,19,24–26 and time savings12,17,18,27 to equal or even better health outcomes.19,27,28,33 Limitations in the form of technological glitches7,8 and uncertainty in future legal11,12 and insurance12–14 regulation of telemedicine do exist. New regulations have temporarily lifted some of these barriers, however.
In the outpatient setting, telecommunications allow those with chronic wounds to continue receiving high-quality care from the comfort and safety of their own homes. Strategies for successful management of wounds via telemedicine in the outpatient setting include:
Instruct patients to verify their smartphone or video-enabled device is working before the start of the telemedicine visit.
Ask patients to have the wound(s) ready to be examined, with the dressings removed, for the time of the appointment.
Obtain a thorough patient history to assess key wound attributes that are otherwise lost through telecommunication (eg, sensation, odor, wound depth, fever).
Provide guidelines for patients to optimize smartphone-generated wound photographs.
Be resourceful in wound evaluation. Consider using household items to approximate wound dimensions and collaborate with patients to elicit a full history and physical examination.
In the inpatient clinical example, the same principles of telemedicine were applied. The wound care team could evaluate the patient using telemedicine by way of chart review and review of clinical photography. The success of telemedicine was contingent upon complete documentation by the providers and the nursing staff, availability of a clinical photograph, and collaboration with the direct care staff when information was missing or when additional clarity was necessary. In this case example, the wound, ostomy, and continence nursing team could clinically assess and manage a pressure injury in a patient with COVID-19 solely using store-and-forward telemedicine communication without risking additional clinician and patient exposure to the virus. In the process, this also preserved vital PPE.
For inpatient wound care telemedicine, there are a few key principles and recommendations that are vital to its success:
Obtain consent from the patient for clinical photography. In the event the patient cannot consent (eg, intubated and sedated), a healthcare proxy can be contacted by the clinician and asked during the daily update to the family.
Clinical photographs of wounds, either patient-generated or staff-generated, must be of sufficient quality with as much standardization (lighting, background, angle, distance, etc.) as possible. Care should be taken to include a ruler for scale in all photos.
Establish strong communication with the nursing staff assessing patients’ wounds.
Educate team members on the use of telemedicine technologies and EHRs.
Create a template for wound assessment to ensure consistency and efficiency in evaluation. This is especially relevant during the COVID-19 pandemic to care for high-volume patient loads with limited specialist availability.
CONCLUSIONS
The COVID-19 pandemic has quickly brought telemedicine to the forefront of care, with healthcare providers using this tool to provide safe and efficient care during a time of uncertainty. In the field of wound care this is a welcomed change. As technology evolves, the benefits of telemedicine continue to compound as limitations are reconciled. Telemedicine use during the COVID-19 pandemic is an intuitive strategy to contain the spread of the virus while protecting healthcare workers. As COVID-19 healthcare policies become better defined in the coming months, telemedicine will likely remain an integral part of wound care assessment and monitoring. It expedites care, eliminates travel time, expands access to care, and increases patient satisfaction. Accordingly, even after the pandemic is over, the authors feel that the field of wound care is ready to expand telemedicine use.
REFERENCES
- 1.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020;382(10):929–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19): Cases in the U.S. April 17, 2020. www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Last accessed May 16, 2020.
- 3.Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA 2018;320(20):2147–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Hospital Association. Fact Sheet: Teleheath: Advancing Health in America. February 19, 2019. https://www.aha.org/system/files/2019-02/fact-sheet-telehealth-2-4-19.pdf. Last accessed May 16, 2020.
- 5.American Well. Telemedicine Index: 2019 Consumer Survey. August 2019. https://static.americanwell.com/app/uploads/2019/07/American-Well-Telehealth-Index-2019-Consumer-Survey-eBook2.pdf. Last accessed May 16, 2020.
- 6.Hong YR, Lawrence J, Williams D, Jr, Mainous A., III Population-level interest and telemedicine capacity of us hospitals in response to COVID-19: cross-sectional analysis of google search and national hospital survey data. JMIR Public Health Surveill 2020;6(2):e18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clegg A, Brown T, Engels D, et al. Telemedicine in a rural community hospital for remote wound care consultations. J Wound Ostomy Continence Nurs 2011;38:301–4. [DOI] [PubMed] [Google Scholar]
- 8.Yenikomshian HA, Lerew TL, Tam M, Mandell SP, Honari SE, Pham TN. Evaluation of burn rounds using telemedicine: perspectives from patients, families, and burn center staff. Telemed J E Health 2019;25(1):25–30. [DOI] [PubMed] [Google Scholar]
- 9.Bloemen EM, Rosen T, Cline Schiroo JA, et al. Photographing injuries in the acute care setting: development and evaluation of a standardized protocol for research, forensics, and clinical practice. Acad Emerg Med 2016;23(5):653–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiseman JT, Fernandes-Taylor S, Gunter R, et al. Inter-rater agreement and checklist validation for postoperative wound assessment using smartphone images in vascular surgery. J Vasc Surg Venous Lymphat Disord 2016;4(3):320–8.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiseman JT, Fernandes-Taylor S, Barnes ML, Tomsejova A, Saunders RS, Kent KC. Conceptualizing smartphone use in outpatient wound assessment: patients' and caregivers' willingness to use technology. J Surg Res 2015;198(1):245–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim PT, Falcone RA., Jr The use of telemedicine in the care of the pediatric trauma patient. Semin Pediatr Surg 2017;26(1):47–53. [DOI] [PubMed] [Google Scholar]
- 13.Sood A, Granick MS, Trial C, et al. The role of telemedicine in wound care: a review and analysis of a database of 5,795 patients from a mobile wound-healing center in Languedoc-Roussillon, France. Plast Reconstr Surg 2016;138(3 Suppl):248S–56S. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare & Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. March 17, 2020. www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Last accessed May 16, 2020.
- 15.Chen CH, Young TH, Huang CH, et al. Patient-centered wound teleconsultation for cutaneous wounds: a feasibility study. Ann Plast Surg 2014;72:220–4. [DOI] [PubMed] [Google Scholar]
- 16.Van Dillen C, Silvestri S, Haney M, et al. Evaluation of an off-the-shelf mobile telemedicine model in emergency department wound assessment and management. J Telemed Telecare 2013;19:84–8. [DOI] [PubMed] [Google Scholar]
- 17.Trovato MJ, Scholer AJ, Vallejo E, et al. eConsultation in plastic and reconstructive surgery. Eplasty 2011;11:e48. [PMC free article] [PubMed] [Google Scholar]
- 18.Murphy RX, Jr, Bain MA, Wasser TE, Wilson E, Okunski WJ. The reliability of digital imaging in the remote assessment of wounds: defining a standard. Ann Plast Surg 2006;56(4):431–6. [DOI] [PubMed] [Google Scholar]
- 19.Téot L, Geri C, Lano J, Cabrol M, Linet C, Mercier G. Complex wound healing outcomes for outpatients receiving care via telemedicine, home health, or wound clinic: a randomized controlled trial. Int J Low Extrem Wounds 2019;1534734619894485. [DOI] [PubMed] [Google Scholar]
- 20.Zarchi K, Haugaard VB, Dufour DN, Jemec GBE. Expert advice provided through telemedicine improves healing of chronic wounds: prospective cluster controlled study. J Invest Dermatol 2015;135(3):895–900. [DOI] [PubMed] [Google Scholar]
- 21.Boccara D, Bekara F, Soussi S, et al. Ongoing development and evaluation of a method of telemedicine: burn care management with a smartphone. J Burn Care Res 2018;39(4):580–4. [DOI] [PubMed] [Google Scholar]
- 22.Segura-Sampedro JJ, Rivero-Belenchón I, Pino-Díaz V, et al. Feasibility and safety of surgical wound remote follow-up by smart phone in appendectomy: a pilot study. Ann Med Surg (Lond) 2017;21:58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Heide J, Vroegh CJ, Szili Torok T, et al. Get the picture: a pilot feasibility study of telemedical wound assessment using a mobile phone in cardiology patients. J Cardiovasc Nurs 2017;32(2):E9–15. [DOI] [PubMed] [Google Scholar]
- 24.American Hospital Association. The promise of telemedicine for hospitals, health systems, and their communities. Washington, DC: American Hospital Association, 2015;1–12. [Google Scholar]
- 25.Michaud TL, Zhou J, McCarthy MA, Siahpush M, Su D. Costs of home-based telemedicine programs: a systematic review. Int J Technol Assess Health Care 2018;34(4):410–8. [DOI] [PubMed] [Google Scholar]
- 26.Liu YM, Mathews K, Vardanian A, et al. Urban telemedicine: the applicability of teleburns in the rehabilitative phase. J Burn Care Res 2017;38(1):e235–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Le Goff-Pronost M, Mourgeon B, Blanchère JP, Teot L, Benateau H, Dompmartin A. Real-world clinical evaluation and costs of telemedicine for chronic wound management. Int J Technol Assess Health Care 2018;34(6):567–75. [DOI] [PubMed] [Google Scholar]
- 28.Vowden K, Vowden P. A pilot study on the potential of remote support to enhance wound care for nursing-home patients. J Wound Care 2013;22:481–8. [DOI] [PubMed] [Google Scholar]
- 29.Wilkins EG, Lowery JC, Goldfarb S. Feasibility of virtual wound care: a pilot study. Adv Skin Wound Care 2007;20(5):275–8. [DOI] [PubMed] [Google Scholar]
- 30.Jiang Z, Ardywibowo R, Samereh A, et al. A roadmap for automatic surgical site infection detection and evaluation using user-generated incision images. Surg Infect (Larchmt) 2019;20(7):555–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bowling FL, Paterson J, Ndip A. Applying 21st century imaging technology to wound healing: an Avant-Gardist approach. J Diabetes Sci Technol 2013;7(5):1190–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bhavnani SP, Narula J, Sengupta PP. Mobile technology and the digitization of healthcare. Eur Heart J 2016;37(18):1428–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilbright WA, Birke JA, Patout CA, Varnado M, Horswell R. The use of telemedicine in the management of diabetes-related foot ulceration: a pilot study. Adv Skin Wound Care 2004;17(5 Pt 1):232–8. [DOI] [PubMed] [Google Scholar]
- 34.Shamloul N, Ghias MH, Khachemoune A. The utility of smartphone applications and technology in wound healing. Int J Low Extrem Wounds 2019;18(3):228–35. [DOI] [PubMed] [Google Scholar]
- 35.Wang G, Xiang W, Pickering M. A cross-platform solution for light field based 3D telemedicine. Comput Methods Programs Biomed 2016;125:103–16. [DOI] [PubMed] [Google Scholar]
- 36.Pavlovčič U, Jezeršek M. Handheld 3-dimensional wound measuring system. Skin Res Technol 2018;24(2):326–33. [DOI] [PubMed] [Google Scholar]
- 37.Lurie N, Carr BG. The role of telemedicine in the medical response to disasters. JAMA Intern Med 2018;178(6):745–6. [DOI] [PubMed] [Google Scholar]
- 38.U.S. Department of Health and Human Services. Notification of Enforcement Discretion for Telemedicine Remote Communications During the COVID-19 Nationwide Public Health Emergency. March 30, 2020. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. Last accessed May 16, 2020.