Abstract
This study aims to explore the relationship between psychological distress and post-traumatic stress disorder among Chinese participants as the result of COVID-19 outbreak. This study was conducted within 1 month after COVID-19 appeared in China, it included 570 participants age from 14 to 35. The results indicated that 12.8% of all participants with the symptoms of post-traumatic stress disorder and the effects of psychological distress on post-traumatic stress disorder was mediated by negative coping style. Gender moderated the direct effect between psychological distress and post-traumatic stress disorder, which is a significant discovery for relevant departments to take further measures.
Keywords: COVID-19, negative coping style, psychological distress, PTSD, youths
Introduction
At the end of 2019, a series of cases of an unfamiliar type of pneumonia has been reported in Wuhan City, Hubei Province, China. It has been confirmed that this pneumonia is caused by a new type of coronavirus, which World Health Organization has officially named it 2019 novel coronavirus disease (Du et al., 2020). On 30 January 2020, the World Health Organization announced a public health emergency of international concern (PHEIC) (WHO, 2020). This public health emergency not only damages people’s physical health, but also have a significant impact on their mental health (Huang et al., 2020; Wang et al., 2020c). Psychological distress as a broader manifestation of mental health-related problems, which is characterized by symptoms of depression anxiety, stress-related concerns and it is known to continue to show severity (Drapeau et al., 2012). In previous studies, psychological distress mainly included related psychological problems such as depression, anxiety, and stress (Higuchi et al., 2016; O’Brien et al., 2016). In a survey with regard to the mental health of general population 2 weeks after the COVID-19 outbreak in China, which the result showed about one-third of participants reported moderate to severe level of anxiety (Wang et al., 2020a), and nearly 40.4% of the youth had a tendency to have psychological problems (Liang et al., 2020). Simultaneously, medical staff also showed signs of irritability, unwillingness to rest, and difficulties in emotion management and existential stress (Chen et al., 2020; Zaka et al., 2020). In addition, the impact of infectious diseases and microbial threats on mental health has become an important public health issue (Holloway et al 1997; Norwood et al., 2001). However, most of previous studies focused on the impacts of public health emergencies such as infectious diseases on the medical staffs who are diagnosed with post-traumatic stress disorder (PTSD) (Brooks et al., 2018; Kang et al., 2020), and less on the impacts of PTSD diagnoses among younger people with lower adaptive capacities and less mature cognitive abilities which make them vulnerable against psychological distresses (Cénat and Derivois, 2014). Thus, about within 1 month after COVID-19 occurred in China, we conducted this cross-sectional study to assess the mental state of young people who are diagnosed with PTSD due to this outbreak.
PSTD is a psychological disorder which can occur after people went through a traumatic experience such as earthquakes, hurricanes and SARS (Ding and Xia, 2014; Gonzalez et al., 2019; Mak et al., 2010). Its basic feature is the characteristic symptoms result from the exposure to a traumatic experience, or a personal tragic life event, or witness events involving death, injury or threat to the physical integrity of others (Lin et al., 2007). And people with PTSD also will be forced to relive the negative effect caused by traumatic event that gives them the disorder, which can cause dramatic changes in their cognition and mood, make them avoid trauma-related stimuli at all cost, these symptoms has an important impact on daily life and work of people (Farooqui et al., 2017; Sekiguchi et al., 2013). With the extremely high infection concerns, enough evidences has demonstrated COVID-19 was considered as a life-threatening public health emergency and a disease serious enough to cause PTSD. According to the cognitive model of PTSD, the negative emotions experienced by traumatized patients (such as fear, sadness, and anger) can cause them to adopt negative assessment as a way to deal with traumatic events, which may lead to PTSD. Furthermore, previous studies have shown that participants with higher level of psychological distress, such as anxiety, depression, and fear, are more likely to develop PTSD symptoms (Wang et al., 2020b; Xi et al., 2020). This may be because people fear injury and death, especially under unexpected and unprepared situations, which can create panic, fear, and tension (Xu et al., 2016). Since the events are unexpected, people will feel confused about their current situation, and they will be uncertain about their future (Yates and Stone, 1992). Furthermore, this uncertainty may cause psychological distress in people, which would result in huge psychological stress aggravating PTSD symptoms. Therefore, psychological distress is a predictor of PTSD. However, the mediating and moderating mechanisms underlying psychological distress and PTSD need further investigation.
Studies have shown that in the absence of other adaptive coping strategies, youths may use material coping as a negative coping style (NCS) to cope with psychological distress (Acierno et al., 1996; Pollice et al., 2011; Vlahov et al., 2002). In addition, numerous empirical studies also proved that adolescents who use NCS after experienced traumatic events such as earthquakes and hurricanes have a negative impact on their PTSD symptoms (Carr et al., 1995; Pina et al., 2008;), which may be a way to alleviate the symptoms of PTSD in youths with psychological distress. It was mainly reflected in the use of methods including denial, blaming, social withdrawal, and disengagement aim to avoid the problematic situations during and after emergencies (Zheng et al., 2012). Thus, this study proposed the hypothesis that NCS would mediate the association between psychological distress and PTSD.
In addition, gender is an important biological determinant of vulnerability to psychosocial stress (Wang et al., 2007). There was no consistent conclusion regarding the relationship between gender and psychological distress and PTSD. Research indicates that compare to males, females show more PTSD symptoms (Kun et al., 2013; Qi et al., 2020). When an emergency occurs, women may be more vulnerable than men, less likely to use effective coping strategies, and tend to interpret PTSD negatively (Tolin and Foa, 2006). On the other hand, women are instinctively more sensitive to loss and stress, and therefore may develop negative emotions and PTSD symptoms (Dell’Osso et al., 2011). However, some studies have found that men have more PTSD diagnoses than women (Du et al., 2018; Liang et al., 2020), this may be because the men take more responsibility in taking care of the family (Guo et al., 2017), therefore show more symptoms of PTSD. These different results inspired us to further explore the relationship between gender, psychological distress and PTSD. Thus, this study proposes the hypothesis that the gender would moderate the direct association between the psychological distress and PTSD (Figure 1).
Figure 1.
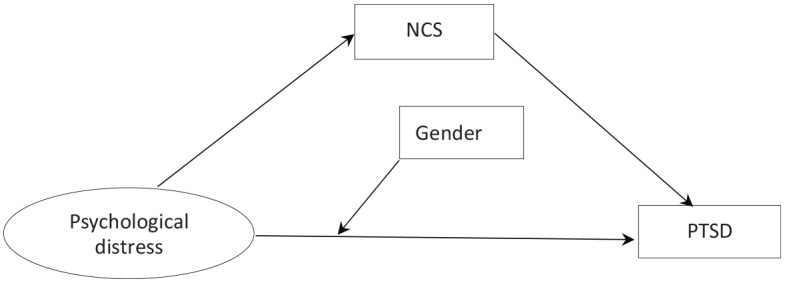
The conceptional framework of the moderated mediation model.
Method
Participants and procedures
A cross-sectional study was designed in the first month since COVID-19 outbreak hits China. The study took a snowball sampling approach to collect questionnaires remotely, targeting people age from 14 to 35. The questionnaires will be sent to participants through a well-known smartphone social network application called WeChat. Participants can share their questionnaires with their friends, who can then share with their friends, as a way to expand the sample size. Finally, approximately 600 questionnaires were collected from participants. After deleting the duplicate IDs and random questionnaires, this study collected a total of 570 valid questionnaires, the valid response rate was 95.0%. Before collecting the data, the participant was given an informed consent, and researchers received a verbal consent from the participant in return.
Measures
The PTSD Checklist-Civilian Version
The diagnosis of PTSD was done by using the PTSD Checklist-Civilian Version (PCL-C) (Weathers et al., 1993), which was designed to assess participants’ responses to traumatic experiences encountered in daily lives. The severity of PTSD symptoms was measured using a five-point Likert scale. The total score range from 17 to 85, with higher score indicates more serious symptomatological PTSD and participants with a cut-off score of 38 or higher were diagnosed with PTSD symptoms (Grubaugh et al., 2007). This scale was widely used to evaluate symptomatic PTSD of Chinese adolescents, with high reliability and validity (Yang et al., 2007). An early study using this threshold reported Cronbach’s alpha of the whole scale was 0.94 (Zhou et al., 2015). In this study, the Cronbach’s alpha of PCL-C was 0.943.
The General Health Questionnaire Scale
The psychological distress was measured using the General Health Questionnaire (GHQ-12) (Goldberg et al., 1997), which contains 12 items assessing participant’s mental health. It uses a four-point Likert scale, which higher score indicates higher degree of disturbance in the mind. The questionnaire has been proven with great reliability and validity, and it is commonly used by different Chinese research (Fares et al., 2016). Previous research has shown that the GHQ-12 coefficients ranged from 0.78 to 0.95 (Arnberg et al., 2012; Yusoff et al., 2010). In the present study, the Cronbach’s alpha of GHQ-12 was 0.79.
Simplified Copying Style Questionnaire
The Simplified Coping Style Questionnaire (SCSQ) (Xie, 1998) was a 20-item self-report scale, including two sub-scales: positive coping (12 items) and negative coping (eight items). Each item options ranged from 0 (never) to 3 (very frequently), and the scores on corresponding sub-scale indicates the level of coping strategy everyone possesses, this study selects the subscale of negative coping style in this questionnaire. Previous study has showed that the Cronbach’s alpha of negative coping was 0.78 (Lin et al., 2020). In the present study, the Cronbach’s alpha of negative coping was 0.83.
Data analysis
In this study, we conducted a descriptive analysis to describe the basic sociodemographic characteristics of participants, and a correlation analysis to verify the relationship between variables. We also used multiple linear regression analysis via SPSS 24.0 (IBM Corp) and a PROCESS macro to tests the mediating effect of NCS and the moderating effect of gender between psychological distress and PTSD. Finally, this study conducted 95% bootstrap confidence intervals (CI) based on 5000 bootstrapped samples, with the effects being significant when the results did not include zero. A significance level of p < 0.05 was used for all variables.
Results
Participant characteristics
As the result, the demographic characteristics of 570 participants are shown in Table 1. A total of 205 males (36.0%) and 365 females (64.0%) were included. The age range of all participants was between 14 and 35 years old. The majority of participants aged 21 to 30 years old (73.3%). As for the education level, a significant proportion of participants were undergraduates (78.2%), follow by master’s degree or above (13.9%). About 69.1% of all participants have a monthly income less than 2000 RMB. See Table 1 for more information.
Table 1.
Demographic characteristics of the participants (n = 570).
| Variables | n | % |
|---|---|---|
| Gender | ||
| Male | 205 | 36.0 |
| Female | 365 | 64.0 |
| Age | ||
| ⩽20 | 131 | 23.0 |
| 21–30 | 418 | 73.3 |
| ⩾31 | 21 | 3.7 |
| Educational level | ||
| High school or secondary school | 45 | 7.9 |
| Undergraduate or college | 446 | 78.2 |
| Master’s degree or above | 79 | 13.9 |
| Monthly income | ||
| ⩽2000 RMB | 394 | 69.1 |
| 2001–3000 RMB | 79 | 13.9 |
| 3001–4000 RMB | 44 | 7.7 |
| 4001–5000 RMB | 15 | 2.6 |
| ⩾5001 RMB | 38 | 6.7 |
Preliminary analyses
Table 2 presented the means, standard deviations and bivariate correlations of all study variables. The results indicated that both psychological distress and NCS had significant positive correlation with PTSD.
Table 2.
Descriptive statistics and correlation among variables.
| Variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Gender | 1 | |||
| The psychological distress | −0.07 | 1 | ||
| PTSD | −0.09* | 0.37** | 1 | |
| NCS | −0.09* | 0.16** | 0.28** | 1 |
| M | 1.64 | 11.73 | 27.32 | 19.53 |
| SD | 0.48 | 6.25 | 10.42 | 5.38 |
Gender was coded so that 1 = male and 2 = female.
p < 0.05; **p < 0.01.
Testing for mediation effect
This study used multiple liner regression analysis (Baron and Kenny, 1986) to test whether NCS mediate the association between the psychological distress and PTSD. In this study, the direct path coefficient from the psychological distress to PTSD was significant (B = 0.61, β = 0.37, p < 0.001), and the psychological distress was also significantly associated with NCS (B = 0.13, β = 0.15, p < 0.001). When we considered both the psychological distress and NCS as predictors of PTSD in the regression model, the path coefficients of the psychological distress on PTSD remained significant (B = 0.55, β = 0.33, p < 0.001). In addition, we used the PROCESS macro (Model 4) in SPSS and perform the bootstrap method to test the indirect effect (Preacher and Hayes, 2008). The results indicated that the psychological distress on PTSD through NCS was significant (95% CI = [0.02, 0.10]; excluding 0). Thus, this study indicated that NCS mediated the association between psychological distress and PTSD.
Testing for the moderated mediation effect
Before examining the moderated mediation analysis, all the variables were mean centered to minimize multicollinearity. Table 3 showed the detailed results. In Model 1, the psychological distress was positively related to PTSD (β = 0.35, p < 0.001). Gender did not relate to PTSD (β = −0.06, p > 0.05), but the interaction term between the psychological distress and gender was positively related to PTSD (β = −0.08, p < 0.05), which indicated that gender could moderate the association between psychological distress and PTSD. In Model 2, the main effect of psychological distress on NCS was significant (β = 0.15, p < 0.001), but this effect could not be moderated by the gender (β = −0.01, p > 0.05). In model 3, the main effect of NCS on PTSD was significant (β = 0.22, p < 0.001), however, this effect could not be moderated by the gender (β = −0.02, p > 0.05). Simple slope analyses were used to further analyze the moderate effect of gender on the relationship between psychological distress and PTSD (see Figure 2). The results indicated that psychological distress can be significantly associated with PTSD in males (βsimple = 0.71, t = 7.17, p < 0.001) and females (βsimple = 0.44, t = 5.25, p < 0.001). The effect of psychological distress on PTSD was higher in males than females.
Table 3.
Testing the moderated mediation effect of psychological distress on PTSD.
| Independent variables | Model 1 (PTSD) |
Model 2 (NCS) |
Model 3 (PTSD) |
|||
|---|---|---|---|---|---|---|
| β | t | β | t | β | t | |
| The psychological distress | 0.35 | 9.01*** | 0.15 | 3.56*** | 0.33 | 8.56*** |
| Gender | −0.06 | −1.06 | −0.08 | −1.86 | −0.05 | −1.23 |
| The psychological distress × Gender | −0.08 | −2.01* | −0.01 | −0.09 | ||
| NCS | 0.22 | 5.48*** | ||||
| NCS × Gender | −0.02 | −0.71 | ||||
| R2 | 0.14 | 0.03 | 0.18 | |||
| F | 32.09*** | 5.86** | 32.42*** | |||
p < 0.05; **p < 0.01; ***p < 0.001.
Figure 2.
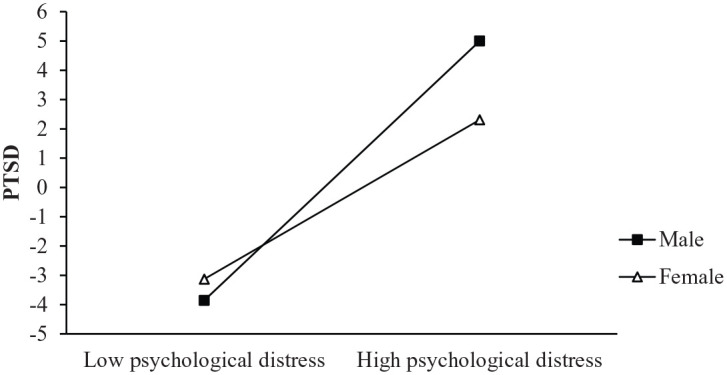
Gender moderates the effect of the psychological distress on PTSD.
In addition, this study conducted the PROCESS macro method (Model 5) to further analyze the moderation mediation, which was able to verify the above assumptions. The index of moderated mediation was –0.27 (SE = 0.13, 95%CI = [–0.526, –0.021]). Analysis of the moderation effect indicated that this path was significantly for males (95% CI = [0.515, 0.904]; excluding 0) and females (95% CI = [0.272, 0.599]; excluding 0), which tested the above assumption.
Discussion
In this study, we found that within 1 month after the occurrence of COVID-19 outbreak in China, the prevalence of PTSD was 12.8%, which was lower than a cross-sectional study of the prevalence of PTSD (22.3%) 1 month after the earthquake in Chengdu, Sichuan province, China (Lau et al., 2010) and also lower than PTSD (41%) reported by SARS patients 3 months after discharge (Kwek et al., 2006). However, in a 4-year follow-up study of discharged SARS patients, the result shows the reported cases of PTSD was 44.1% among all patients (Hong et al., 2009). And in a report from Italy, the prevalence of PTSD 8 years after the earthquake is only 0.5% (Priebe et al., 2011). The above differences in PTSD prevalence after a traumatic event may be due to the differences in research methods, culture, type and severity of the disaster, time interval measured after the disaster and diagnostic criteria (Liu et al., 2017). In addition, a systematic review demonstrated that the PTSD rate declined after disaster (Dai et al., 2016), but studies also pointed out that adolescents affected by traumatic events were prone to invasive thoughts such as sleep disorders, nightmares, and separation anxiety (Yule, 2001). Thus, this emphasizes that relevant government agencies should take measures aimed at the mental health of youths as soon as a public health emergency occurs. In addition, related preventive and clinical measures should also be applied to prevent and treat the damage of COVID-19 to participants’ health. A recent study suggested that COVID-19 can cause nervous system damage (Wu et al., 2020), and also indicated that the negative mental states (such as depression and anxiety) are relate to changes in the immune system (Rajkumar, 2020). Thus, from the perspective of psychoneuroimmunology, the immune system can be improved by eliminating daily psychological distress, maintaining good sleep quality, balancing nutrition intake, keeping a healthy lifestyle and exercising regularly. As the result, if people have strong immune systems, it can reduce the risk of COVID-19 infection (Kim and Su, 2020; Matias et al., 2020; Ng et al., 2018). Also, this study provides references that are significant for relevant clinical researches, and they can help psychiatrists to effectively identify the groups with mental health issues due to the COVID-19 outbreak (Zhou et al., 2013). After picking out people in need, psychological professionals can provide remote services like telephone and internet, which can speed up the development of technologies along the way, such as electronic consent forms and telemedicine (Smith et al., 2020).
As expected, the effect of psychological distress on PTSD was mediated by NCS, which supported the initial hypothesis. In the study, the mediation analysis indicates that psychologically distressed adolescents are more likely to engage in negative coping strategies, which ultimately lead to PTSD (Vlahov et al., 2002). In addition, traumatic experiences cause people to experience more negative emotions, which in turn results in PTSD (Quan et al., 2020). People overwhelmed with negative emotions tend to choose negative behaviors like self-blame or avoid problems (Xiang et al., 2016), this may be because negative emotions have been theorized as an obstacle mechanism to affect NCS (Folkman and Lazarus, 1988). Such actions can further weaken people’s capability to deal with psychological distresses, which will eventually lead to mental illnesses like PTSD (D’Amico et al., 2013). Moreover, studies have also shown that the symptoms of PTSD and psychological distress have overlapping characteristics (Hurlocker et al., 2018), sharing common characteristics such as inattention, hypervigilance, and emotional disorders (Pacella et al., 2013), in which may be because the related symptoms didn’t occur in isolation (Borsboom and Cramer, 2013). Therefore, these results may help psychiatrists and psychologists to develop or take interventions that target specific symptoms of this relationship. When a public health emergency occurs, the local government should immediately provide relevant psychological interventions to help young people overcome negative emotional experiences, because early psychological interventions can help reduce the prevalence of PTSD (Zhou et al., 2013). On the other hand, during the COVID-19 outbreak, the government and other relevant agencies should encourage adolescents to take active coping styles, enhance their ability of learning from difficult situations and actively seek help from others who can protect them from PTSD (Liu et al., 2016).
Our study indicated that gender played a moderating role in the direct effect between the psychological distress and PTSD, which supported the hypothesis. With the increase of psychological distress, the prevalence of women PTSD increased significantly, but the prevalence of men PTSD increase more. From a biological perspective, gender is an important biological determinant of the vulnerability of psychological distress, and gender differences have been identified in the brains’ activation of stress. This may be because by examine the brain activity in response to physiological stresses, significant differences appear between men and women. When people try to cope with psychological distress, the activities of prefrontal lobe in males’ brains are asymmetric, meanwhile, the activities are mainly focus on limbic system for females. In brief, the results show men and women will choose different actions and coping strategies in response to when people try to cope with psychological distress (Wang et al., 2007). The reason may also be caused by the different coping styles during the study time, or it may be because women are more likely to show symptoms during emergencies, which can effectively reduce the chance of get PTSD (Du et al., 2018). In addition, social expectations related to gender roles may lead to differences (Tolin and Foa, 2006). In China, there may be such a basic rule that men are normally perceived as powerful figures who are dominant in status and rights (Chen et al., 2009), but this social trend may also bring more psychological distresses to men. During the occurrence of COVID-19, the Chinese government has implemented the strictest prevention and control measures, people need isolation at home to prevent infection, on the other hand, adult males will experience more psychological distress due to increasing financial pressures and loss of job opportunities. Such high stress situations can increase chances of getting PTSD in males. Therefore, this study suggests that corresponding measures should be taken based on the gender differences in the PTSD.
Limitations
Certain limitations of this study should be recognized. We examined only general psychopathology using the GHQ-12 rather than a specific mental health problem (such as depression and fear). Our study used a cross-sectional design, which cannot provide strong evidence for causality. Thus, further research should use a longitudinal design. In addition, our study is limited by sample size. In order to get more detailed results, larger and more universal sample groups are needed.
Conclusion
This study was conducted within 1 month of the COVID-19 emergency in China. In this study, 12.8% of participants were diagnosed with PTSD, which indicates the significance of the public health emergency. Government and other relevant agencies must take swift and systematic action to improve the mental health of youth. This study found that general mental health can be affected by PTSD through NCS, highlighting the moderating effect of gender on this association. The prevalence of PTSD in women increased significantly with psychological distress, but the prevalence of men PTSD increased even more. This study provides a reference for formulating psychological intervention measures to improve people’s mental health and psychological adaptability during the occurrence of COVID-19 and any similar pandemics in the future.
Acknowledgments
The author wish to thank his collaborators for their contribution to this study.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by International innovation team of Jilin University (2019GJTD06); research plan of youth development in Jilin Province–the effect of COVID-19 on adolescent mental health (2020jqy-018); research on the problems of COVID-19 of Jilin University (2020XGZX11).
ORCID iD: Leilei Liang  https://orcid.org/0000-0003-4754-5430
https://orcid.org/0000-0003-4754-5430
References
- Acierno RA, Kilpatrick DG, Resnick HS, et al. (1996) Violent assault, posttraumatic stress disorder, and depression-risk factors for cigarette use among adult women. Behavior Modification 20(4): 363–384. [DOI] [PubMed] [Google Scholar]
- Arnberg FK, Hultman CM, Michel P-O, et al. (2012) Social support moderates posttraumatic stress and general distress after disaster. Journal of Trauma Stress 25(6): 721–727. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. (1986) The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology 51(6): 1173–1182. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO. (2013) Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology 9: 91–121. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Dunn R, Amlôt R, et al. (2018) Systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. Journal of Occuptional and Environmental Medicine 60(3): 248–257. [DOI] [PubMed] [Google Scholar]
- Carr VJ, Lewin TJ, Webster RA, et al. (1995) Psychosocial sequelae of the 1989 Newcastle earthquake: I. Community disaster experiences and psychological morbidity 6 months post-disaster. Psychological Medicine 25(3): 539–555. [DOI] [PubMed] [Google Scholar]
- Cénat JM, Derivois D. (2014) Assessment of prevalence and determinants of posttraumatic stress disorder and depression symptoms in adults survivors of earthquake in Haiti after 30 months. Journal of Affective Disorders 159: 111–117. [DOI] [PubMed] [Google Scholar]
- Chen QN, Liang MN, Li YM, et al. (2020) Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry 7(4): E15–E16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen ZX, Fiske ST, Lee TL. (2009) Ambivalent sexism and power-related gender-role ideology in marriage. Sex Roles 60(11–12): 765–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai WJ, Chen L, Lai ZW, et al. (2016) The incidence of post-traumatic stress disorder among survivors after earthquakes: A systematic review and meta-analysis. BMC Psychiatry 16: 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico S, Marano A, Geraci MA, et al. (2013) Perceived self-efficacy and coping styles related to stressful critical life events. PLoS One 8(7): e67571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell’Osso L, Carmassi C, Massimetti G, et al. (2011) Full and partial PTSD among young adult survivors 10 months after the L’Aquila 2009 earthquake: Gender differences. Journal of Affective Disorders 131(1–3): 79–83. [DOI] [PubMed] [Google Scholar]
- Ding C, Xia LX. (2014) Posttraumatic reactions to an earthquake: Multidimensional scaling profile analysis of adolescent survivors. Journal of Health Psychology 19(8): 1055–1065. [DOI] [PubMed] [Google Scholar]
- Drapeau A, Marchand A, Beaulieu-Prévost D. (2012) Epidemiology of psychological distress. Mental Illnesses-Understanding, Prediction and Control 69: 105–134. [Google Scholar]
- Du BL, Ma XZ, Ou XC, et al. (2018) The prevalence of posttraumatic stress in adolescents eight years after the Wenchuan earthquake. Psychiatry Research 262: 262–269. [DOI] [PubMed] [Google Scholar]
- Du ZW, Wang L, Cauchemez S, et al. (2020) Risk for transportation coronavirus disease from Wuhan to other cities in China. Emerging Infectious Diseases 26(5): 1049–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. (1988) Coping as a mediator of emotion. Journal of Personality and Social Psychology 54(3): 466–475. [PubMed] [Google Scholar]
- Fares J, Saadeddin Z, Al Tabosh H, et al. (2016) Extracurricular activities associated with stress and burnout in preclinical medical students. Journal of Epidemiology and Global Health 6: 177–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooqui M, Quadri SA, Suriya SS, et al. (2017) Posttraumatic stress disorder: A serious post-earthquake complication. Trends in Psychiatry and Psychotherapy 39(2): 135–143. [DOI] [PubMed] [Google Scholar]
- Goldberg DP, Gater R, Sartorius N, et al. (1997) The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychological Medicine 27(1):191–197. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Rasul R, Molina L, et al. (2019) Differential effect of Hurricane Sandy exposure on PTSD symptom severity: Comparison of community members and responders. Occupational and Environmental Medicine 76(12): 88–887. [DOI] [PubMed] [Google Scholar]
- Grubaugh AL, Elhai JD, Cusack KJ, et al. (2007) Frueh Screening for PTSD in public-sector mental health settings: The diagnostic utility of the PTSD checklist. Depression and Anxiety 24(2): 124–129. [DOI] [PubMed] [Google Scholar]
- Guo J, Fu MQ, Xing J, et al. (2017) Coping style and posttraumatic growth among adult survivors 8 years after the 2008 Wenchuan earthquake in China. Personality and Individual Differences 111: 31–36. [Google Scholar]
- Higuchi Y, Inagaki M, Koyama T, et al. (2016) A cross-sectional study of psychological distress, burnout, and the associated risk factors in hospital pharmacists in Japan. BMC Public Health 16: 534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway HC, Norwood AE, Fullerton CS, et al. (1997) The threat of biological weapons. Prophylaxis and mitigation of psychological and social consequences. JAMA 278(5): 425–427. [PubMed] [Google Scholar]
- Hong X, Currier GW, Zhao XH, et al. (2009) Posttraumatic stress disorder in convalescent severe acute respiratory syndrome patients: A 4-year follow-up study. General Hospital Psychiatry 31(6): 546–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang CL, Wang YM, Li XW, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223): 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurlocker MC, Vidaurri DN, Cuccurullo LJ, et al. (2018) Examining the latent structure mechanisms for comorbid posttraumatic stress disorder and major depressive disorder. Journal of Affective Disorders 229: 477–482. [DOI] [PubMed] [Google Scholar]
- Kang LJ, Li Y, Hu SH, et al. (2020) The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry 7(3): e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SW, Su KP. (2020) Using psychoneuroimmunity against COVID-19. Brain, Behavior, and Immunity 87: 4–5. DOI: 10.1016/j.bbi.2020.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kun P, Tong X, Liu Y, et al. (2013) What are the determinants of post-traumatic stress disorder: Age, gender, ethnicity or other? Evidence from 2008 Wenchuan earthquake. Public Health 127(7): 644–652. [DOI] [PubMed] [Google Scholar]
- Kwek SK, Chew WM, Ong KC, et al. (2006) Quality of life and psychological status in survivors of severe acute respiratory syndrome at 3 months postdischarge. Journal of Psychosomatic Research 60(5): 513–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau JTF, Yu XN, Zhang JX, et al. (2010) Psychological distress among adolescents in Chengdu, Sichuan at 1 month after the 2008 Sichuan earthquake. Journal of Urban Health 87(3): 504–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang LL, Ren H, Cao RL, et al. (2020) The effect of COVID-19 on youth mental health. Psychiatric Quarterly. Epub ahead of print 21 April 2020. DOI: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CY, Peng YC, Wu YH, et al. (2007) The psychological effect of severe acute respiratory syndrome on emergency department staff. Emergency Medicine Journal 24(1): 12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JY, Su YA, Lv XZ, et al. (2020) Perceived stressfulness mediates the effects of subjective social support and negative coping style on suicide risk in Chinese patients with major depressive disorder. Journal of Affective Disorders 265: 32–38. [DOI] [PubMed] [Google Scholar]
- Liu DL, Chen H, Ma L, et al. (2017) Post-traumatic stress disorder and its predictors among bereaved Tibetan adolescents four years after the Yushu earthquake: A cross-sectional survey in China. Journal of Clinical Nursing 26(7–8): 1095–1105. [DOI] [PubMed] [Google Scholar]
- Liu DL, Fu LY, Jing Z, et al. (2016) Post-traumatic stress disorder and it’s predictors among tibetan adolescents 3 years after the high-altitude earthquake in China. Archives of Psychiatric Nursing 30(5): 593–599. [DOI] [PubMed] [Google Scholar]
- Mak IW, Chu CM, Pan PC, et al. (2010) Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. General Hospital Psychiatry 32(6): 590–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matias T, Dominski FH, Marks DF. (2020) Human needs in COVID-19 isolation. Journal of Health Psychology 25(7): 871–882. DOI: 10.1177/1359105320925149. [DOI] [PubMed] [Google Scholar]
- Yusoff MSB, Rahim AFA, Yaacob MJ. (2010) Prevalence and sources of stress among Universiti Sains Malaysia medical students. The Malaysian Journal Medical Sciences 17(1): 30–37. [PMC free article] [PubMed] [Google Scholar]
- Ng A, Tam WW, Zhang MW, et al. (2018) IL-1β, IL-6, TNF-α and CRP in elderly patients with depression or Alzheimer’s disease: Systematic review and meta-analysis. Scientific Reports 8(1): 12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norwood AE, Holloway HC, Ursano RJ. (2001) Psychological effects of biological warfare. Military Medicine 166(12): 27–28. [PubMed] [Google Scholar]
- O’Brien KS, Latner JD, Puhl RM, et al. (2016) The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite 102: 70–76. [DOI] [PubMed] [Google Scholar]
- Pacella ML, Hruska B, Delahanty DL. (2013) The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders 27(1): 33–46. [DOI] [PubMed] [Google Scholar]
- Pina AA, Villalta IK, Ortiz CD, et al. (2008) Social support, discrimination, and coping as predictors of posttraumatic stress reactions in youth survivors of Hurricane Katrina. Journal of Clinical Child and Adolescent Psychology 37(3): 564–574. [DOI] [PubMed] [Google Scholar]
- Pollice R, Bianchini V, Roncone R, et al. (2011) Marked increase in substance use among young people after L’Aquila earthquake. European Child & Adolescent Psychiatry 20(8): 429–430. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. (2008) Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods 40(3): 879–891. [DOI] [PubMed] [Google Scholar]
- Priebe S, Marchi F, Bini L, et al. (2011) Mental disorders, psychological symptoms and quality of life 8 years after an earthquake: Findings from a community sample in Italy. Social Psychiatry and Psychiatric Epidemiology 46(7): 615–621. [DOI] [PubMed] [Google Scholar]
- Qi J, Yang XM, Tan RY, et al. (2020) Prevalence and predictors of posttraumatic stress disorder and depression among adolescents over 1 year after the Jiuzhaigou earthquake. Journal of Affective Disorders 261: 1–8. [DOI] [PubMed] [Google Scholar]
- Quan LJ, Zhen R, Yao BX, et al. (2020) Traumatic exposure and posttraumatic stress disorder among flood victims: Testing a multiple mediating model. Journal of Health Psychology 25(3): 283–297. [DOI] [PubMed] [Google Scholar]
- Rajkumar RP. (2020) Ayurveda and COVID-19: Where psychoneuroimmunology and the meaning response meet. Brain, Behavior, and Immunity 87: 8–9. DOI: 10.1016/j.bbi.2020.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekiguchi A, Sugiura M, Taki Y, et al. (2013) Brain structural changes as vulnerability factors and acquired signs of post-earthquake stress. Molecular Psychiatry 18(5): 618–623. [DOI] [PubMed] [Google Scholar]
- Smith K, Ostinelli E, Cipriani A. (2020) Covid-19 and mental health: a transformational opportunity to apply an evidence-based approach to clinical practice and research. Evidence Based Mental Health 23(2): 45–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. (2006) Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychology Bulletin 132(6): 959–992. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Galea S, Resnick H, et al. (2002) Increased use of cigarettes, alcohol, and marijuana among Manhattan, New York, residents after the September 11th terrorist attacks. American Journal of Epidemiology 155(11): 988–996. [DOI] [PubMed] [Google Scholar]
- Wang CY, Pan RY, Wan XY, et al. (2020. a) Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. International Journal of Environmental Research and Public Health 17(5): 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JJ, Korczykowski M, Rao H, et al. (2007) Gender difference in neural response to psychological stress. Social Cognitive and Affective Neuroscience 2(3): 227–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang WC, Wu XC, Lan XY. (2020. b) Rumination mediates the relationships of fear and guilt to posttraumatic stress disorder and posttraumatic growth among adolescents after the Ya’an earthquake. European Journal of Psychotraumatology 11(1): 1704993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YB, Zhao XD, Feng Q, et al. (2020. c) Psychological assistance during the coronavirus disease 2019 outbreak in China. Journal of Health Psychology 25(6): 733–737. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, et al. (1993) The PTSD checklist: Reliability, validity, and diagnostic utility. International Society for Traumatic Stress Studies 2: 90–92. [Google Scholar]
- World Health Organization (2020) Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV). Available at: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov).
- Wu YS, Xu XL, Chen ZJ, et al. (2020) Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain, Behavior, and Immunity 87: 18–22. DOI: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xi YJ, Yu H, Yao YM, et al. (2020) Post-traumatic stress disorder and the role of resilience, social support, anxiety and depression after the Jiuzhaigou earthquake: A structural equation model. Asian Journal of Psychiatry 49: 101958. [DOI] [PubMed] [Google Scholar]
- Xiang YH, Wang RF, Jiang YQ, et al. (2016) Relationships among personality, coping style, and negative emotional response in earthquake survivors. Social Behavior and Personality 44(3): 499–508. [Google Scholar]
- Xie YN. (1998) The initial exploration of reliability and validity of simplified coping styles questionnaire. Chinese Journal of Clinical Psychology 6: 114–115. [Google Scholar]
- Xu JP, Dai JZ, Rao RQ, et al. (2016) The association between exposure and psychological health in earthquake survivors from the Longmen Shan Fault area: The mediating effect of risk perception. BMC Public Health 16: 417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X-Y, Yang H-A, Liu Q-G, et al. (2007) The research on the reliability and validity of PCL-C and influence factors. Chinese Journal of Health Psychology 15(1): 6–9. [Google Scholar]
- Yates JF, Stone ER. (1992) Risk appraisal. Risk-taking Behavior 92: 49–85. [Google Scholar]
- Yule W. (2001) When disaster strikes–the need to be “wise before the event”: Crisis intervention with children and adolescents. Advances in Mind-Body Medicine 17(3): 191–196. [DOI] [PubMed] [Google Scholar]
- Zaka A, Shamloo SE, Fiorente P, et al. (2020) COVID-19 pandemic as a watershed moment: A call for systematic psychological health care for frontline medical staff. Journal of Health Psychology 25(7): 883–887. DOI: 10.1177/1359105320925148. [DOI] [PubMed] [Google Scholar]
- Zheng YH, Fan F, Liu XC, et al. (2012) Life events, coping, and posttraumatic stress symptoms among Chinese adolescents exposed to 2008 Wenchuan Earthquake, China. PLoS One 7(1): e29404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou XB, Kang L, Sun XL, et al. (2013) Prevalence and risk factors of post-traumatic stress disorder among adult survivors six months after the Wenchuan earthquake. Comprehensive Psychiatary 54(5): 493–499. [DOI] [PubMed] [Google Scholar]
- Zhou XB, Song H, Hu M, et al. (2015) Risk factors of severity of post-traumatic stress disorder among survivors with physical disabilities one year after the Wenchuan earthquake. Psychiatry Research 228(3): 468–474. [DOI] [PubMed] [Google Scholar]


