Abstract
Objective
Different assessment tools are used to screen for joint hypermobility. One of the most commonly used tools is the Beighton score. However, the inclusion of the item “hands on floor” (HOF) has been questioned, as this maneuver is not a pure measure of the range of motion because it involves multiple joints and stretching of muscular structures. This study therefore aimed to determine the value of the HOF item to the Beighton score in children aged 6–11 years.
Methods
Exploratory research involved children in Grades 1–4 attending four different primary schools in South Africa. Children with a severe medical or neurological condition were excluded from the study. Hypermobility was determined as a score ≥5/8 on the Beighton score excluding the HOF item.
Results
A total of 460 children (median age 8.58 years [interquartile range, 7.33–9.50]) were tested, of which 34.57% were hypermobile. However, only 8.91% of all children scored positive on HOF. Although a significant association was found between HOF and the hypermobility classification (p=0.007), 86.16% of the hypermobile children could not place their hands flat on the floor. Internal consistency improved slightly when HOF was removed from the scale (α changed from 0.698 to 0.703), with a weak corrected item-total correlation (r=0.16). The specificity of the item HOF in identifying hypermobility is high (93.69%); however, the sensitivity is very low (13.84%).
Conclusion
This study does not show an additional value of the item HOF of the Beighton score in children.
Keywords: Child, joint instability, musculoskeletal system, range of motion
Introduction
The prevalence of joint hypermobility, the ability to move beyond the normal range of motion (ROM) in less than five joints (localized hypermobility) or more than five joints (generalized joint hypermobility [GJH]) (1), depends on age, gender, and ethnicity of the population (2–12). The population prevalence of GJH is estimated to be 10%–30%, with significantly higher rates among children, females, and Asian and African racial groups (5, 6, 9–12).
Pain, musculoskeletal disorders, a motor developmental delay, and motor coordination problems are often reported in children with GJH (13, 14), which may persist into adulthood (15). Therefore, diagnosis and management of hypermobility are of great importance.
Due to the variety of health professionals (pediatricians, rheumatologists, orthopedic surgeons, and physiotherapists) who are qualified to diagnose hypermobility, it is important to use valid, reliable and reproducible instruments to gain consensus and ensure the multidisciplinary approach when diagnosing and treating such patients (13, 14, 16).
Different diagnostic and screening tools are available to identify joint hypermobility and joint hypermobility syndrome: the Beighton score (17, 18), Bulbena/Barcelona criteria (19), Brighton criteria (20), Carter-Wilkinson criteria (2, 21), and Biro criteria (22, 23). The Beighton score, most commonly used worldwide (3, 5–7, 9–11, 13, 16, 17, 23–26), is an adaptation of the Carter-Wilkinson criteria (27), and it was originally developed for research related to joint hypermobility in the Ehlers-Danlos syndrome (18). Beighton and Horan (18) replaced the item “passive hyperextension of the fingers parallel to the extensor side of the forearm” of the Carter-Wilkinson criteria to “dorsiflexion of the 5th digit,” as they believed the former movement was too far-reaching for many subjects. They also replaced the item “passive dorsiflexion of the ankle and eversion of the foot” with “forward flexion of the trunk,” as small variations in movement of the ankle and foot were found in a normal population. Further, the Carter-Wilkinson criteria used a cut-off score of three positive items, including both the upper and lower limb, to define GJH (21). However, this scoring system was later adapted by Beighton et al. (17), for use in their epidemiological study of a South African population. Therefore, the Beighton scoring system, as used today, contains five items, with a score ranging from 0 to 9 (18). Items 1 to 4 are assessed bilaterally. Item 1 assesses passive dorsiflexion of the metacarpophalangeal joint, scoring positive when the 5th digit can move beyond 90° dorsiflexion. Item 2 is scored positively when the thumb can touch the flexor side of the forearm. Items 3 (elbow) and 4 (knee) assess the hyperextension of the joint with a positive score when the joint can be passively extended past 10°. Item 5 assesses the ability to reach for the floor with both hands, while the knees stay in extension. A positive score is attributed when the person can place both hands flat on the floor (18).
Although the Beighton score is the most frequently used screening tool, no clear universal cut-off score is defined to identify hypermobility in children and adults (3, 5–7, 9–11, 13, 16, 17, 23–26). Further, only a few studies investigated the validity and reliability of the Beighton score, presenting mixed results (3, 16, 19, 24). In the study of Ferrari et al. (3), the Beighton score was compared to the Lower Limb Assessment Score (LLAS) in three groups of children (normomobile, possible hypermobile, and known hypermobile). The Beighton score was unable to differentiate between these groups. However, an agreement between both assessment tools was found in 69% of the cases; particularly in the group with known hypermobility, a strong agreement was found between the LLAS and Beighton score (in 80% of the cases). This could indicate that the Beighton score can identify children with general hypermobility, but that the LLAS is preferred over the Beighton score when identifying lower limb joint hypermobility (3). A review by Remvig et al. (16) concluded that the Beighton score is a reproducible tool, particularly when used by experienced rheumatologists. However, further studies are needed to ascertain its validity and determine its sensitivity and specificity. Smits-Engelsman et al. (24) investigated the validity of the Beighton score by comparing it with a “standardized joint mobility protocol” (which assessed the passive ROM of eight different joints). They found that the Beighton score was a valid tool for measuring GH when items were measured with a goniometer. Finally, the study by Bulbena et al. (19) reported a high predictive and concurrent validity of the Beighton, Carter-Wilkinson, and Rotés-Querol criteria.
The separate items of the Beighton score have not been analyzed in the literature. A few studies reported scores for the separate Beighton score items within a pediatric population, revealing that the item HOF is less often scored positive in children compared to the other items (5, 11, 26). It can be hypothesized that the item HOF measures more than single joint hypermobility, as the movement is comparable to a sit-and-reach test, which is influenced by the hamstrings length, spinal mobility, hip joint ROM, and anthropometric characteristics (28–30). Therefore, it is unclear whether HOF has a place within the Beighton score, as all other items are single joint ROM measurements.
This study therefore aims to determine whether the HOF item provides an additional value to the Beighton score. The item will be considered to have an additional value if (I) the internal consistency decreases when the item is removed from the test, (II) a moderate correlation (≥0.20) is obtained for the corrected item-total correlation between the Beighton score items, and (III) high sensitivity and specificity are found (>80%).
Methods
This study used a cross-sectional exploratory study design, assessing children at one point in time. Ethical approval to conduct this research was granted by the University of Cape Town Human Research Ethics Committee (ref: 556/2014). Further approval was obtained from the Western Cape Department of Education; and parent and children provided their consent/assent to take part in the study.
Participants
Children aged 6–11 years attending Grades 1–4 in four different mainstream primary schools in Cape Town, South Africa, were enrolled in the study. Children identified as having any medical or neurological problems (based on parental reports) were excluded from the study. All children eligible for the study, who returned signed consent and assent forms, were enrolled in the study. A sample of convenience was used. All children included in this study were of Black African or mixed ancestry.
Hypermobility assessment
This study used a cut-off score of ≥5/9 on the Beighton score to determine hypermobility. Description of the Beighton score can be found in the introduction. To analyze the usefulness of the item HOF, the item was removed from the total Beighton score, referred to as the ROM score. This score only includes the scores of the elbow, knee, thumb, and 5th digit, giving a total maximum score of 8. The cut-off score for identification of hypermobility was set at ≥5/8.
Procedure
Data were collected in a separate classroom, during school hours. Children performed other movement tests prior to the assessment of the Beighton score, which provided a generalized but non-standardized warm-up session. The procedure was explained verbally to all children prior to testing. Testing was conducted by trained pediatric physiotherapists. Children did not wear shoes when the HOF item was tested, and the tested joints were free of clothes to maintain accuracy. A goniometer was used to measure the items “dorsiflexion of the 5th digit beyond 90°,” “elbow extension beyond 10°,” and “extension of the knees beyond 10°” to prevent observational bias. Handedness was not recorded during the test procedure.
Statistical analysis
Data were analyzed using the IBM Statistical Package for the Social Sciences software version 25.0 (IBM SPSS Corp.; Armonk, NY, USA). Normality of the data was tested using the Shapiro-Wilk test. The children’s descriptive information is presented as the mean and standard deviation (SD) or median and interquartile range (IQR), depending on data distribution. Frequency tables and percentages were used together with the Pearson Chi-squared test to analyze associations and frequencies. Further, the Cronbach α was calculated to determine internal consistency with corrected item-total correlation. Finally, the specificity and sensitivity of the HOF item has been analyzed, using the receiver operator characteristic (ROC) curve. The significance level was set at 0.05.
Results
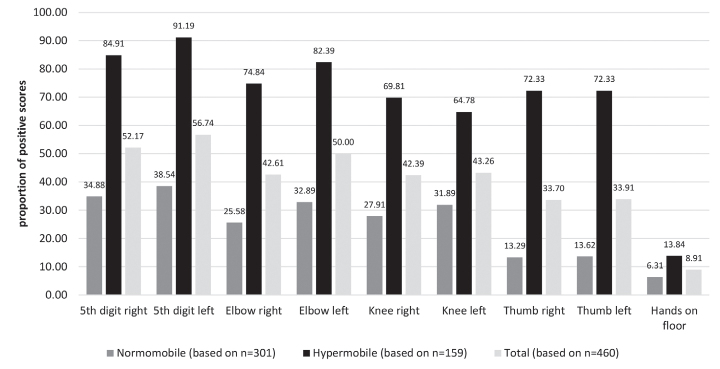
A total of 460 children were enrolled in the study (median [IQR] age of 8.58 [7.33–9.50] years, 233 boys and 227 girls). Table 1 presents the participants’ characteristics. All data, except the height in centimeters, were skewed. An overview of the frequency of positive scores per item is presented in Figure 1. Frequencies for the four bilateral items ranged from 33.70% to 56.74%; however, only 8.91% of children scored positive on the HOF item.
Table 1.
Characteristics of participants.
| Characteristic | Male | Female | Total |
|---|---|---|---|
| N | 233 (50.65%) | 227 (49.35%) | 460 |
| Age (year), median (IQR) | 8.67 (7.33–9.50) | 8.58 (7.42–9.50) | 8.58 (7.33–9.50) |
| Weight (kg), median (IQR) | 27.50 (23.60–31.70) | 28.50 (23.10–33.10) | 27.75 (23.50–32.35) |
| Height (cm), mean (SD) | 130.15 (9.28) | 130.21 (9.80) | 130.18 (9.53) |
| Beighton score (≥5/9) | |||
| - Normomobile, n (%) | 150 (64.38) | 144 (63.44) | 294 (63.91) |
| - Hypermobile, n (%) | 83 (35.62) | 83 (36.56) | 166 (36.09) |
| ROM score (≥5/8) | |||
| - Normomobile, n (%) | 152 (65.24) | 149 (65.64) | 301 (65.43) |
| - Hypermobile, n (%) | 81 (34.76) | 78 (34.36) | 159 (34.57) |
IQR: interquartile range; N: number of participants; ROM: range of motion; SD: standard deviation.
Figure 1.
Proportion of positive scores on the Beighton items per ROM category (based on the ROM score ≥5/8 indicating hypermobility) and of the total population.
A significant association is found between the item HOF and mobility classified based on the ROM score (χ2=7.26; df=1; p=0.007). However, 86.16% (137/159) of the hypermobile children were unable to place the palms of the hands flat on the floor (Figure 1).
The Cronbach α of the entire 9-item score (α= 0.698) changed slightly when the HOF item was removed from the dataset (α=0.703). Furthermore, a low item-total correlation coefficient was found between the HOF item and other items of the score (Table 2). And finally, ROC revealed an area under the curve of 0.54 (p=0.184), with a high specificity of the HOF item (93.69%), but a low sensitivity (13.84%).
Table 2.
Item-total correlation for the Beighton score items.
| Item | Item-Total Correlation |
|---|---|
| Dorsiflexion 5th digit right | 0.42 |
| Dorsiflexion 5th digit left | 0.43 |
| Elbow right | 0.41 |
| Elbow left | 0.40 |
| Knee right | 0.32 |
| Knee left | 0.23 |
| Thumb right | 0.48 |
| Thumb left | 0.47 |
| Hands on floor | 0.16 |
Discussion
The aim of this study was to determine whether the HOF item adds additional value to the Beighton score in children. The current study’s results suggest that the HOF item shows very little discriminative value as only seven children shifted from the category hypermobile to normomobile when the item was removed from the screening tool (with the ROM cut-off score ≥5/8). Further, the internal consistency increased slightly when the item was removed from the test, and a very weak item-total correlation was found between HOF and the other items of the score. The ROC analysis also revealed a very poor diagnostic ability of the item HOF.
Although a significant relation was found between HOF and hypermobility (based on the ROM score), 85.6% of the hypermobile children could not place the palms of their hands flat on the floor. In addition, HOF scored positive in the least number of participants with only 8.6% of all children (normomobile and hypermobile) able to reach for the floor. Hypermobile children were able to put the hands flat on the floor more often (13.84%) than normal mobile children (6.31%). However, all the other items reached percentages of 64.78%–91.19% in the hypermobile group. This is related to the high specificity and low sensitivity found for the item HOF.
The low number of participants being able to reach for the floor in our study is in line with the study by Hasija et al. (11); however, the authors found a higher percentage (17%) of the participants being able to reach the floor than in the current study. Quatman et al. (26) also found that the HOF item was least often scored positive within the pre-pubertal and pubertal groups, but this discrepancy disappeared in their post-pubertal group. The study by Lamari et al. (31) also found a low percentage (14%) of children scoring positive on the HOF item; however, they found that the item “extension of the knees” scored even lower (12.5%). The lower percentage of children who can place the palms of their hands on the floor in our study could be attributed to the anatomical leg length difference between ethnic groups. A shorter leg length is found in Caucasian populations compared to African populations (32), which might explain why the children in our study struggled to place their palms on the floor. Also, developmental changes in body segments need to be taken into consideration. The growth rate of the long bones, and therefore the limbs, is higher in young children than the growth rate of the trunk and head, which continues until puberty (33). During adolescence, the growth rate of the trunk surpasses the rate of the limbs to develop a more adult-like appearance (33).
The current study was conducted in South Africa, in a low socio-economic, Black African and mixed ancestry community. African and Indian populations have been found to be more flexible than Caucasian populations (34, 35), which makes it impossible to make generalizations about other ethnic groups.
More research is warranted to determine the additional value of the HOF item, particularly investigation into the different confounding factors, such as the muscle length, leg-length-to-trunk ratio, and the arm length and spinal mobility in different ethnic groups. Currently the Beighton score only includes one lower limb item “extension of the knees beyond 10°.” Adding another easy-to-measure lower limb item could increase test consistency and diagnostic value. Therefore, we recommend replacing the HOF item with passive dorsiflexion of the ankle beyond 25°, similarly to the original item in the Carter-Wilkinson criteria (21), with a cut-off value based on a study conducted by Smits-Engelsman et al. (24). However, further investigation about this item and the cut-off value is warranted. Also, further analysis should be done on the validity and reliability of the different items of the Beighton score, to determine whether this tool can be used as a screening test for GJH in different ethnic and age groups.
Based on our results, the HOF item does not add additional value to the Beighton score in children of Black African and mixed ancestry. The body composition and the various confounding factors (assessing not merely ROM) are most likely affecting the outcome of the HOF item in children. Hence, the clinical relevance of this item to assess hypermobility in children is questionable, suggesting the use of the Beighton score without the HOF item in this population. Investigating the replacement of the item with, for example, passive dorsiflexion of the ankle is recommended.
Main Points.
Most children struggle to place their hands flat on the floor while standing, whether they are hypermobile or not.
Children who can place their hands on the floor while standing are more likely to have generalized hypermobility (high specificity).
Children who fail to put their hands on the floor while standing are not all normomobile (low sensitivity).
The item HOF of the Beighton score does not have additional value in identifying children with hypermobility.
Acknowledgment
We would like to thank the pediatric physiotherapists involved in the testing of the children. We also thank Prof Peter Beighton for comments on the earlier version of this paper.
Footnotes
Content of this journal is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Ethics Committee Approval: Ethics committee approval was received for this study from the University of Cape Town Human Research Ethics Committee (ref: 556/2014).
Informed Consent: Written informed consent was obtained from patients and the parents of the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - L.C., G.F., B.S.E.; Design - L.C., G.F., B.S.E.; Supervision - L.C., G.F., B.S.E.; Resources - G.F., B.S.E.; Materials - G.F., B.S.E.; Data Collection and/or Processing - L.C., G.F., B.S.E.; Analysis and/or Interpretation - L.C.; Literature Search - L.C.; Writing Manuscript - L.C.; Critical Review - L.C., G.F., B.S.E.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Castori M, Tinkle B, Levy H, Grahame R, Malfait F, Hakim A. A framework for the classification of joint hypermobility and related conditions. Am J Med Genet Part C Semin Med Genet. 2017;175:148–57. doi: 10.1002/ajmg.c.31539. [DOI] [PubMed] [Google Scholar]
- 2.Subramanyam V, Janaki KY. Joint hypermobility in South Indian children. Indian Pediatr. 1996;33:771–2. [PubMed] [Google Scholar]
- 3.Ferrari J, Parslow C, Lim E, Hayward A. Joint hypermobility: The use of a new assessment tool to measure lower limb hypermobility. Pediatr Rheumatol. 2005;23:413–20. [PubMed] [Google Scholar]
- 4.Remvig L, Jensen DV, Ward RC. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: Review of the literature. J Rheumatol. 2007;34:804–9. [PubMed] [Google Scholar]
- 5.Qvindesland A, Jónsson H. Articular hypermobility in Icelandic 12-year-olds. Rheumatology. 1999;38:1014–6. doi: 10.1093/rheumatology/38.10.1014. [DOI] [PubMed] [Google Scholar]
- 6.Rikken-Bultman DG, Wellink L, van Dongen PW. Hypermobility in two Dutch school populations. Eur J Obstet Gynecol Reprod Biol. 1997;73:189–92. doi: 10.1016/S0301-2115(97)02745-0. [DOI] [PubMed] [Google Scholar]
- 7.Seow CC, Chow PK, Khong KS. A study of joint mobility in a normal population. Ann Acad Med Singapore. 1999;28:231–6. [PubMed] [Google Scholar]
- 8.Santos MC, Azevêdo ES. Generalised joint hypermobility and black admixture in school children in Bahia, Brazil. Am J Phys Anthr. 1981;55:43–6. doi: 10.1002/ajpa.1330550107. [DOI] [PubMed] [Google Scholar]
- 9.El-Garf A, Mahmoud G, Mahgoub E. Hypermobility among Egyptian children: Prevalence and features. J Rheumatol. 1998;25:1003–5. [PubMed] [Google Scholar]
- 10.Van der Giessen LJ, Liekens D, Rutgers KJM, Hartman A, Mulder PGH, Oranje AP. Validation of Beighton Score and prevalence of connective tissue signs in 773 Dutch children. J Rheumatol. 2001;28:2726–30. [PubMed] [Google Scholar]
- 11.Hasija R, Khubchandani R, Shenoi S. Joint hypermobility in Indian children. Clin Exp Rheumatol. 2008;26:146–50. [PubMed] [Google Scholar]
- 12.Schweiter G. Laxity of metacarpophalangeal joints of fingers and interphalangeal joint of the thumb: A comparative inter-racial study. S Afr Med J. 1970;44:246–9. [PubMed] [Google Scholar]
- 13.Adib N, Davies K, Grahame R, Woo P, Murray KJ. Joint hypermobility syndrome in childhood. A not so benign multisystem disorder? Rheumatology. 2005;44:74–50. doi: 10.1093/rheumatology/keh557. [DOI] [PubMed] [Google Scholar]
- 14.Simmonds JV, Keer RJ. Hypermobility and the hypermobility syndrome. Man Ther. 2007;12:298–309. doi: 10.1016/j.math.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Grahame R. Time to take hypermobility seriously (in adults and children) Rheumatology. 2001;40:485–7. doi: 10.1093/rheumatology/40.5.485. [DOI] [PubMed] [Google Scholar]
- 16.Remvig L, Jensen DV, Ward RC. Are diagnostic criteria for general joint hypermobility and benign joint hypermobility syndrome based on reproducible and valid tests? A review of the literature. J Rheumatol. 2007;34:798–803. [PubMed] [Google Scholar]
- 17.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32:413–8. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Jt Surg. 1969;51:444–53. doi: 10.1302/0301-620X.51B3.444. [DOI] [PubMed] [Google Scholar]
- 19.Bulbena A, Duro J, Porta M, Faus S, Vallescar R, Martin-Santos R. Clinical assessment of hypermobility of joints: Assembling criteria. J Rheumatol. 1992;19:115–22. [PubMed] [Google Scholar]
- 20.Graham R, Bird H, Child A. The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome (BJHS) J Rheumatol. 2000;27:1777–9. [PubMed] [Google Scholar]
- 21.Carter C, Wilkinson J. Persistent joint laxity and congenital dislocation of the hip. J Bone Jt Surg. 1964;46:40–5. doi: 10.1302/0301-620X.46B1.40. [DOI] [PubMed] [Google Scholar]
- 22.Biro F, Gewanter H, Baum J. The hypermobility syndrome. Paediatrics. 1983;72:701–6. [PubMed] [Google Scholar]
- 23.Verhoeven JJ, Tuinman M, Van Dongen PWJ. Joint hypermobility in African non-pregnant nulliparous women. Eur J Obstet Gynecol Reprod Biol. 1999;82:69–72. doi: 10.1016/S0301-2115(98)00182-1. [DOI] [PubMed] [Google Scholar]
- 24.Smits-Engelsman B, Klerks M, Kirby A. Beighton score: A valid measure for generalized hypermobility in children. J Pediatr. 2011;158:119–123. e4. doi: 10.1016/j.jpeds.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 25.Jansson A, Saartok T, Werner S, Renström P. General joint laxity in 1845 Swedish school children of different ages: Age- and gender-specific distributions. Acta Paediatr. 2004;93:1202–6. doi: 10.1111/j.1651-2227.2004.tb02749.x. [DOI] [PubMed] [Google Scholar]
- 26.Quatman CE, Ford KR, Myer GD, Paterno MV, Hewett TE. The effects of gender and maturational status on generalized joint laxity in young athletes. J Sci Med Sport. 2008;11:257–63. doi: 10.1016/j.jsams.2007.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beighton P, Grahame R, Bird H. Hypermobility of Joints. 4th ed. London: Springer-Verlag; 2012. pp. 11–26. [DOI] [Google Scholar]
- 28.Cornbleet SL, Woolsey NB. Assessment of hamstring muscle length in school-aged children using the sit-and-reach test and the inclinometer measure of hip joint angle. Phys Ther. 1996;76:850–5. doi: 10.1093/ptj/76.8.850. [DOI] [PubMed] [Google Scholar]
- 29.Chillón P, Castro-Piñero J, Ruiz JR, Soto VM, Carbonell-Baeza A, Dafos J, et al. Hip flexibility is the main determinant of the back-saver sit-and-reach test in adolescents. J Sports Sci. 2010;28:641–8. doi: 10.1080/02640411003606234. [DOI] [PubMed] [Google Scholar]
- 30.Mayorga-Vega D, Merino-Marban R, Viciana J. Criterion-related validity of sit-and-reach tests for estimating hamstring and lumbar extensibility: A meta-analysis. J Sports Sci Med. 2014;13:1–14. doi: 10.4100/jhse.2014.91.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lamari NM, Chueire AG, Cordeiro JA. Analysis of joint mobility patterns among preschool children. Sao Paulo Med J. 2005;123:119–23. doi: 10.1590/S1516-31802005000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deurenberg P, Deurenberg-Yap M. Validity of body composition methods across ethnic population groups. Acta Diabetol. 2003;40:246–9. doi: 10.1007/s00592-003-0077-z. [DOI] [PubMed] [Google Scholar]
- 33.Huelke DF. An overview of anatomical considerations of infants and children in the adult world of automobile safety design. Annu Proc Assoc Adv Automot Med. 1998;42:93–113. [Google Scholar]
- 34.Harris H, Joseph J. Variations in extension of the metacarpo-phalangeal and interphalangeal joints of the tumb. J Bone Jt Surg. 1949;31:547–59. doi: 10.1302/0301-620X.31B4.547. [DOI] [PubMed] [Google Scholar]
- 35.Birrell F, Adebajo A, Hazleman B, Silman A. High prevalence of joint laxity in West Africans. Br J Rheumatol. 1994;33:56–9. doi: 10.1093/rheumatology/33.1.56. [DOI] [PubMed] [Google Scholar]