Abstract
Background: Covid-19 has started to spread within China since the end of December 2019. Despite government’s immediate actions and strict control, more and more people were infected every day. As such a contagious virus can spread easily and rapidly between people, the whole country was put into lockdown and people were forced into isolation. In order to understand the impact of Covid-19 on mental health well-being, Chinese researchers have conducted several studies. However, no consistent results were obtained. Therefore, a meta-analysis was conducted.
Methods: We searched Embase, PubMed, and Web of Science databases to find literature from December 2019 to April 2020 related to Covid-19 and mental health, among which results such as comments, letters, reviews and case reports were excluded. The incidence of anxiety and depression in the population was synthesized and discussed.
Results: A total of 27,475 subjects were included in 12 studies. Random effect model is used to account for the data. The results showed that the incidence of anxiety was 25% (95% CI: 0.19–0.32), and the incidence of depression was 28% (95% CI: 0.17–0.38). Significant heterogeneity was detected across studies regarding these incidence estimates. Subgroup analysis included the study population and assessment tools, and sensitivity analysis was done to explore the sources of heterogeneity.
Conclusions: Owing to the significant heterogeneity detected in studies regarding this pooled prevalence of anxiety and depression, we must interpret the results with caution. As the epidemic is ongoing, it is vital to set up a comprehensive crisis prevention system, which integrating epidemiological monitoring, screening and psychological crisis prevention and interventions.
Keywords: Mental health, Covid-19, Anxiety, Depression, Meta-analysis
Background
At the end of December, the first case of Covid-19 that a novel coronavirus, which could potentially cause acute infectious pneumonia, emerged from Wuhan, China. As early as 30th January 2020, WHO had declared it as a public health emergency of international concerns, and appealing for efforts to prevent this epidemic [1]. According to the National Health Commission of China, until 4th February 2020, there had been 24,324 people confirmed to be infected by Covid-19 across 31 provinces in Mainland China [2]. Due to its high infectiveness, widely and rapidly spread was inevitable. By 23rd April, there have been 84,302 confirmed cases in China. Globally, this figure has surged up to 2,510,122, including 172,241 deaths reported to WHO [3].
China, as the first nation struck by Covid-19, has taken unprecedented measure to control the virus. Three weeks into the epidemic, indoor facilities such as cinemas and shopping malls were closed, public transportation was suspended and communities were kept under close monitored. The whole country was in lockdown, over 50 million people were quarantined, including confirmed as well as suspected patients. Under this circumstance, people were prone to experience loneliness, anxiety and depression caused by social isolation and fear of being infected. The shortage of personal protective equipment and medical equipment had worsened the situation. Not only the general public was in distressed, healthcare professionals were one of the worst affected by supply shortages. They had to come to work and care for patients knowing that they were very likely to be infected due to insufficient protective equipment. Moreover, excessive workload and extreme working condition had undoubtedly added an enormous mental burden for front line workers. The similar situation during influenza outbreak were shown, researchers suggested that about 10–30% of the population concern or had some degree of concern about being exposed to the virus [4].
Given that no one fully understands the impact of Covid-19 outbreak has on mental health, many researches were conducted within China. According to researches, mental distress was detected within the nation. However, how significant the distress was varied dramatically. For example, according to Wang and Pan, the percentage of anxiety and depression was 28.8% and 16.5%, respectively [5]. Yet, another research revealed that 50.4% and 44.6% of all had symptoms of anxiety and depression [6]. As all available research data had presented to be very inconsistent, it would be useful to analyze the data provided, using an integrated approach to build a clear picture of the impact. To our knowledge, this is the first meta-analysis that identifies the impact of Covid-19 outbreak has on mental health.
Methods
Search Strategy
This study was performed according to the recommendations of the Moose [7]. Two reviewers independently searched the EMBASE, Web of Science and PubMed to obtain all potential researches, using keywords including Covid-19, mental health, depression, anxiety, depressive and stress. Reviewers also manually searched the references of selected articles to identify any relevant studies. Only English articles were included in this study.
Inclusion and Exclusion Criteria
Xin Ren and Wanli Huang reviewed the initial retrieved publications independently. The discrepancy was resolved through discussion by all reviewers. Studies that met the following criteria were included: (1) cross-sectional studies; (2) the nationality of the subjects is Chinese and age >18 years old; (3) used a standard instrument to assess for mental health conditions. However, articles had incomplete or unidentified data were excluded, as well as abstracts, reviews, case reports, letters and duplicate publications.
Quality Assessment and Data Extraction
Xin Ren and Wanli Huang reviewed each included article independently, using the 11-item checklist that was recommended by the Agency for Healthcare Research and Quality (AHRQ) [8]. An item would be scored ‘0’ if it was answered ‘NO’ or ‘UNCLEAR’ whereas ‘1’ will be given to the answer ‘YES’. Article quality was assessed as follows: low quality = 0–3; moderate quality = 4–7; high quality = 8–11. Differences in article quality were discussed to reach an agreeable final score. The following information was extracted: first author, publication time, the sample size, study population, assessment tools, and the number of people who had anxiety and depression.
Statistical Analysis
A random-effect model was used to estimate the pooled proportion of anxiety and depression. Statistical heterogeneity was considered to be present when p < 0.1 or I2 > 50%. Publication bias was evaluated visually by funnel plots and considered significant when p < 0.05 in either Begg’s test or Egger’s test. The subgroup analysis was carried out using the study population and assessment tools. STATA 14.0 software (Stata Corporation, College Station, TX, USA) was also used to conduct different analyses and all statistical tests.
Result
Search Results
Our initial search yielded 568 articles in total, 170 of which were removed for duplication. After screening titles and abstracts, further 378 items were taken away. Twenty articles were reviewed, among which 12 were included in this meta-analysis [5, 6, 9–18]. No further study was identified by manual search. The flow diagram of studies selection was shown in Fig. 1.
Fig. 1.
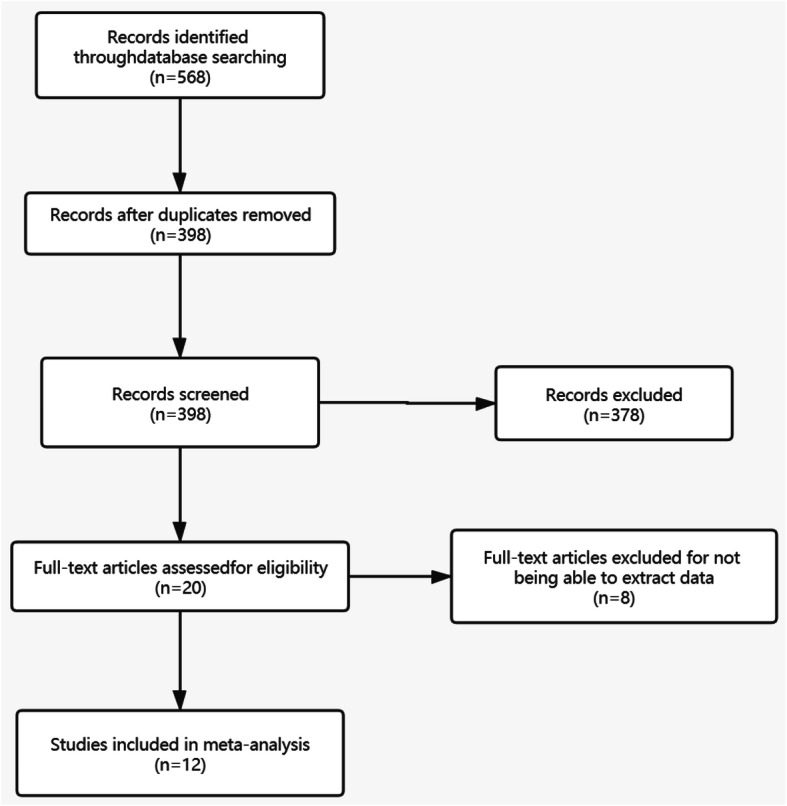
Flowchart of selection of studies for inclusion in meta-analysis
Study Characteristic
Twelve cross-sectional studies, with 27,475 subjects, met the inclusion criteria and were included for the final meta-analysis. Among the subjects, 21,377 were the general public and 6098 were healthcare professionals. The sample size of the studies ranged from 98 to 7236. Assessment tools used in the studies are list as follows: Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder (GAD-7), Self-Rating Anxiety Scale (SAS), Self-rating depression scale (SDS), Impact of Event Scale-Revised (IES-R), Hamilton Anxiety Scale (HAMA), Hamilton Depression Scale (HAMD) and The insomnia severity index (ISI). The main features of the 12 articles were summarized in Table 1. AHRQ scores suggested that all 12 studies scored at eight as high quality.
Table 1.
Characteristics of studies included in the meta-analysis
| Study | Study design | Age (mean ± sd) | Male (%) | Assessment tools | Cases (n) | Participants | Quality score |
|---|---|---|---|---|---|---|---|
| [5] | Cross-sectional | NA | 32.7 | IES, DASS | 1210 | General public | 8 |
| [6] | Cross-sectional | NA | 23.3 | PHQ-9, GAD-7, ISI, IES-R | 1257 | Healthcare professionals | 8 |
| [9] | Cross-sectional | 37.7 ± 14.0 | 40.3 | IES | 263 | General public | 8 |
| [10] | Cross-sectional | 32.31 ± 4.88 | 28.3 | SAS, GSES, PSQI, SASR, SSRS | 180 | Healthcare professionals | 8 |
| [11] | Cross-sectional | 32.71 ± 6.52 | 10 | SAS, SOS | 180 | Healthcare professionals | 8 |
| [12] | Cross-sectional | 34 ± 12 | 44.5 | SAS, SDS | 600 | General public | 8 |
| [13] | NA | NA | 30.35 | GAD-7 | 7143 | General public | 8 |
| [14] | Cross-sectional | 35.3 ± 5.6 | 45.4 | GAD-7, CES-D, PSQI | 7236 | General public | 8 |
| [15] | Cross-sectional | NA | 35.8 | PHQ-4, GAD-2, ISI, SCL-90 | 2182 | Healthcare professionals and general public | 8 |
| [16] | Cross-sectional | NA | 22.35 | HAMA, HAMD | 2299 | Healthcare professionals | 8 |
| [17] | Cross-sectional | 29.6 ± 12.69 | 34.7 | PHQ-9, GAD-7 | 98 | General public | 8 |
| [18] | Cross-sectional | 32.3 ± 10.0 | 32.3 | WHO-5, GAD-7 | 4827 | General public | 8 |
Overall Prevalence of Anxiety among the Population
The rate of anxiety within the population reported in nine studies ranged from 9% to 45% (Fig. 2). Meta-analytic pooling of these rates generated an overall prevalence of 25% (95% CI: 0.19–0.32, P = 0.00, I2 = 99.4%), which calculated by random-effects model (P < 0.05), with significant between-study heterogeneity exist (I2 = 99.4%). Hence, to find out the sources of heterogeneity, we used subgroup analysis (Table 2) to evaluate potential sources between the study population and assessment tools. First, the summarized proportion of non-medical staff was 24% (95% CI: 0.16–0.32), while medical staff was 27% (95% CI: 0.12–0.43). Second, the summarized proportion of anxiety assessed by GAD-7 scale was 36% (95% CI: 0.27–0.44). Anxiety evaluated by SAS scale and GAD-2 scale was 14% (95% CI: −0.01-0.30) and 11% (95% CI: 0.06–0.15), respectively. No evidence of publication bias was detected by the Begg’s test (p = 0.721) and the Egger’s test (p = 0.925). Sensitivity analysis was carried out to evaluate the influence of a single study on the results of this meta-analysis. We found that no significant changed was observed of 10 values when any one study was removed from this meta-analysis (Fig. 3).
Fig. 2.
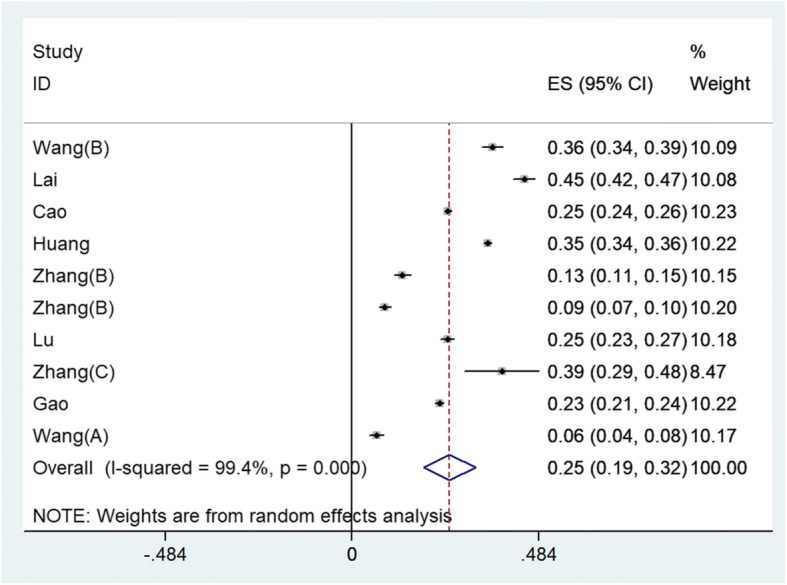
Summarized proportion of anxiety in overall population
Table 2.
Subgroup meta-analysis by study population and assessment tools for the summarized proportion of anxiety in overall population
| Variable | Summarized proportion | 95% CI | I2 | P value | Number of studies |
|---|---|---|---|---|---|
| Overall estimate | 0.25 | [0.19;0.32] | 99.4% | <0.01 | 9 |
| Study population | |||||
| General public | 0.24 | [0.16;0.32] | 99.5% | <0.01 | 7 |
| Health professionals | 0.27 | [0.12;0.43] | 99.4% | <0.01 | 3 |
| Assessment tools | |||||
| GAD-7 | 0.36 | [0.27;0.44] | 99.0% | <0.01 | 4 |
| SAS | 0.14 | [−0.01;0.30] | 99.5% | <0.01 | 2 |
| GAD-2 | 0.11 | [0.06;0.15] | 90.9% | <0.01 | 2 |
CI Confidence interval
Fig. 3.
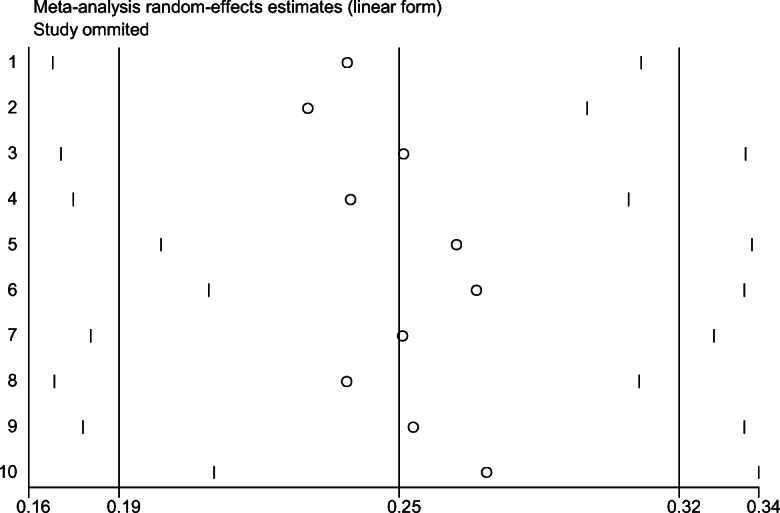
Sensitivity analysis of anxiety in overall population
Overall Prevalence of Depression among the Population
Eight of the 12 studies with 19,709 subjects were included for the meta-analysis for overall prevalence, which was 28% (95% CI: 0.17–0.38, P = 0.00, I2 = 99.7%) (Fig. 4). Subgroup analysis (Table 3) was used to identify possible sources of heterogeneity. The rate of depression was 29% (95% CI: 0.16–0.42) among the general public, whereas 25% (95% CI: 0.04–0.45) among healthcare professions. Additionally, studies conducted by different scales yielded different results of depression prevalence as follows: PHQ-9 scale was 50% (95% CI: 0.48–0.53), and PHQ-4 scale was 11% (95% CI: 0.08–0.13). To investigate the publication bias, we used Egger’s test (p = 0.594) and the Begg’s test (p = 0.348) to investigate the publication bias and the result revealed that such bias did not exist. Sensitivity analysis was carried out to evaluate the influence of individual study had on results of this meta-analysis. We found that no significant changed was observed of 9 values when any one study was removed from this meta-analysis (Fig. 5).
Fig. 4.
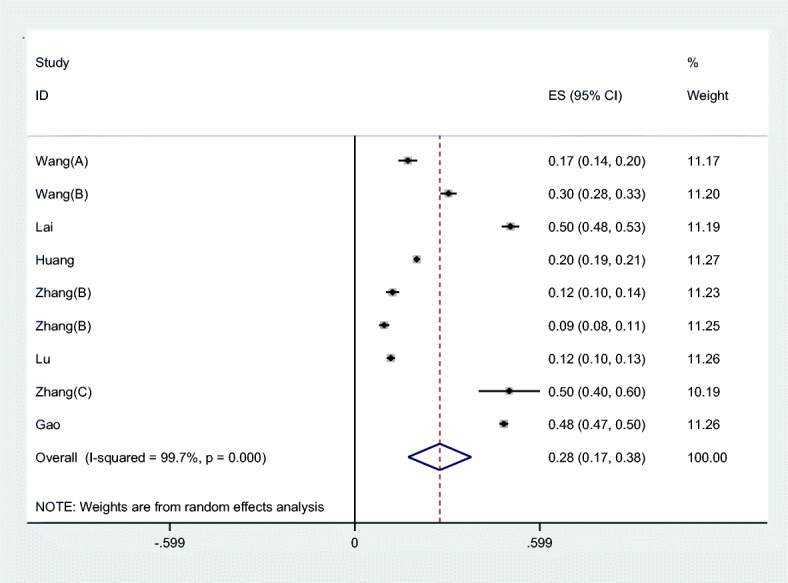
Summarized proportion of depression in overall population
Table 3.
Subgroup meta-analysis by study population and assessment tools for the summarized proportion of depression in overall population
| Variable | Summarized proportion | 95% CI | I2 | P value | Number of studies |
|---|---|---|---|---|---|
| Overall estimate | 0.28 | [0.17;0.38] | 99.7% | <0.01 | 9 |
| Study population | |||||
| General public | 0.29 | [0.16;0.42] | 99.7% | <0.01 | 6 |
| Health professionals | 0.25 | [0.04;0.45] | 99.7% | <0.01 | 3 |
| Assessment tools | |||||
| PHQ-9 | 0.50 | [0.48;0.53] | 93.4% | <0.01 | 2 |
| PHQ-4 | 0.11 | [0.08;0.13] | 74.8% | P = 0.047 | 2 |
CI Confidence interval
Fig. 5.
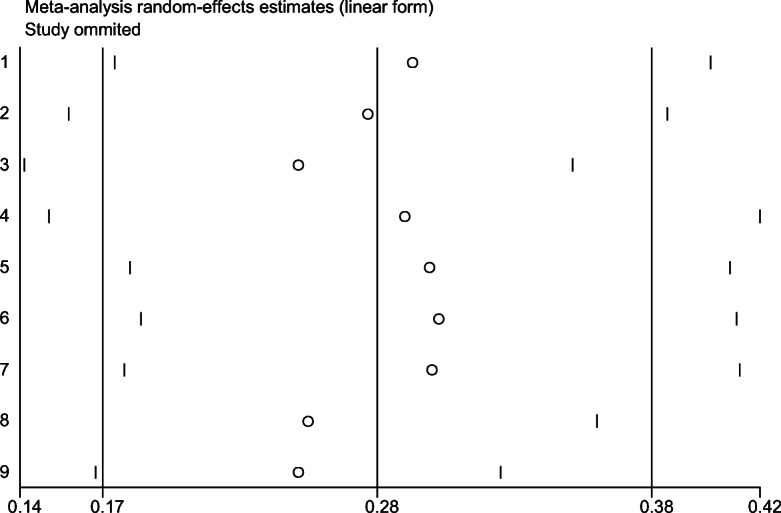
Sensitivity analysis of depression in overall population
Discussion
According to Robert G. Maunder, Severe Acute Respiratory Syndrome (SARS) should not be considered as mental health catastrophe. Since the virus would unlikely to mutate and patients would only become the source of infection when they were symptomatic, authorities had been able to identify cases efficiently and to isolate infected individuals [19], which limited spread of the disease and therefore had provided reassurance for people.
However, unlike typical respiratory viruses that are most contagious when a patient is symptomatic, Covid-19 was very different. A study looking into 94 Covid-19 patients has proved that human-to-human transmission can occur during the asymptomatic incubation period [20], which can be as long as 14 days. Alarmingly, according to a case reported by one Germany researcher and as well as studies conducted in China, people who suffered from subclinical or mild symptoms of the disease possessed the same viral load to patients who exhibited symptoms [21, 22]. In fact, 44% transmissions of the virus occurred before people got sick [20]. As a result, traditional containment measures struggle to be effective as expected. Although fatality rate was about 0.3–0.6%, because of its distinctive characteristic that make it so difficult to contain, Covid-19 should be recognized as health catastrophe that would cause people great and sudden sufferings [23].
According to Hall, R.C.W. et al., during the outbreak of an infection, people’s mental health would be affected profoundly and immensely [24]. For the general public, myths and misinformation about the virus, fueling health-related fears and concerns, together with shut down of infrastructures trigger a series of emotional stress response including anxiety and other negative emotions. Healthcare professionals, being exposed to this new and highly contagious pathogen, are heavily burdened with excessive workload, shortage of personal protection equipment and feeling lack of support. Some researchers have been done to find out how the Covid-19 outbreak affects people’s mental health. According to one research conducted by Cuiyan Wang et al., 16.5% of respondents (the general public) reported moderate to severe depressive symptoms, and 28.8% reported anxiety symptoms to the same extent [5]. Another study has shown that a depression rate of 17.7% and an anxiety rate of 6.33%. Furthermore, there were a lot more research data that had presented to be varied considerably in both rates [6, 25]. As a result, the study we conducted can help to identify the mental burden of the public and therefore, to improve future mental health care.
In this meta-analysis, the percentage of mental disturbance (anxiety and depression) was calculated, using data from 12 articles, including 27,475 individuals. Overall, the pooled prevalence of anxiety was 25%. Because of the high heterogeneity discovered in this article (I2 = 99.4%), we performed subgroup analysis, which included study population and assessment tools to identify the source of heterogeneity. Nevertheless, heterogeneity of both groups was over 50%. Sensitivity analysis found no significant changed was observed of 10 values when any one study was removed. No publication bias was discovered analyzed by the Begg’s test (p = 0.721) and the Egger’s test (p = 0.925). Besides, we also calculated the pooled prevalence of depression, which was 28%. Similarly, the heterogeneity was high as well, and subgroup analysis indicated that the result was higher than 50%. Sensitivity analysis revealed that after removing nine values, there was no significant changed observed. Egger’s test (p = 0.594) and the Begg’s test (p = 0.348) were carried out, but no publication bias was discovered. The results must be interpreted with caution because the significant heterogeneity was detected in studies.
We cannot identify if there is any different impact these infectious diseases had on mental health because there were relatively small numbers of articles that analyzed what was the influence SARS had on mental health, and even fewer articles analyzed the relationship between Middle East Respiratory Syndrome (MERS) and mental health. But fortunately, some researches of Post-SARS psychology had provided valuable information for governments and mental health organizations to prepare for the current outbreak. Authorities had paid crucial attention to maintain people’s well-being mentally and physically. For instance, hot-lines were set up to deal with the Covid-19 related issues, and handbooks with advice on how to look after individual mental health during the outbreak were given out [26]. Thanks to advanced technologies, daily updates of the disease and latest government advice and policies were accessible anytime online. Extensive information was made available to the general public to ease people’s anxiety. However, as a consequence of large-scale social isolation, people were not only worried about contracting the virus, they were also worried about their love ones [27]. The uncertainty of how the future would be and how those measures would affect the stability of society and the economy was causing lots of concerns.
This study had several limitations. Firstly, the sample size of this meta-analysis was relatively small. As a result, the unknown risk of bias caused by incomplete data could constrain our results. Secondly, the data collected by QR code or link in these studies only demonstrated the figures of people who concern about mental health but not those who have no interested in joining this kind of surveys. People who have no interested in mental health would not join the studies. Since most data were collected via online platforms or smartphone applications, older people would have troubles to take part in. The statistic can only reflect the mental status of the people who have access to the Internet or smartphone. Thirdly, not all the studies had collected data about subjects’ social status and incomes, which also affect their ability and perception when experiencing psychological distress. Fourthly, it is notable that studies included in this meta-analysis used entirely self-report inventories as assessment tools, which had an inconsistent sensitivity and specificity for detecting anxiety and depressive symptoms. Instruments such as the SCL-90 have low specificity, although it is a cost-effective instrument, particularly in epidemiological surveys. Finally, some studies reported the response rate but did not contact the non-respondents for the reasons why they did not participate in the surveys. Therefore, those non-respondents were too stressed to respond or not interested in the surveys is hard to tell. These factors are partly responsible for the prospective heterogeneity source of pool prevalence of anxiety and depression. Much remain to be learned to cast light upon this phenomenon in the future.
Conclusion
In summary, our meta-analysis showed that the pooled prevalence of anxiety and depression was 25% and 28%, respectively. Given the fact that previous findings indicated both groups of people suffered from stress [9, 25], and healthcare professionals continue to experience substantial psychological distress, even 1–2 year after the SARS outbreak [28, 29], we should continue perfecting our psychological first aid system. As the epidemic is ongoing, not only the people but also our healthcare systems need to be prepared. This meta-analysis highlights the need for setting up a comprehensive crisis prevention system, which integrating epidemiological monitoring, screening and psychological interventions.
Acknowledgments
The authors thank Wanqi Huang for helping to revise this manuscript.
Availability of Data and Material
All data generated or analyzed in this study are available from the corresponding author for the reasonable request.
Biographies
Ms. Xin Ren
Xin Ren obtained a bachelor’s degree of clinical medicine from City College of Zhejiang University in 2013. She is now working as a doctor of the Psychosomatic department at the Tongde Hospital. Her main area of interest is mental health in the general population, particularly anxiety and depression.
Ms. Wanli Huang
Wanli Huang graduated from Central South University, Xiangya Medical College in 2010 and completed a master’s degree in psychopathology and mental health from Zhejiang University in 2013. Since 2013, she has worked in the department of psychiatry at Tongde Hospital of Zhejiang Province as a doctor. Her research interests are the pathogenesis and treatment of schizophrenia.
Ms. Huiping Pan
Huiping Pan is Vice Dean of Psychosomatic department at Tongde Hospital of Zhejiang Province. She has engaged in the clinical work of psychiatry for over 20 years. She has been involved in research on the treatment of psychosis, the biological effects of antipsychotics and how to integrate traditional Chinese and western medicine to treat the side effects of antipsychotic drugs.
Ms. Tingting Huang
Tingting Huang graduated from Zhejiang Chinese Medical University and now works in the Psychosomatic Department of Tongde Hospital of Zhejiang. Her main research themes concentrate on how to alleviate side reactions of antipsychotics, using her knowledge about traditional Chinese medicine.
Ms. Xinwei Wang
Xinwei Wang graduated from Zhejiang Chinese Medical University, majored in psychopathology and mental health. Working as a doctor in the Psychosomatic Department of Tongde Hospital of Zhejiang, she currently devote herself to studying the evaluation of treatments and the biological risk factors for psychosis.
Mr. Yongchun Ma
Yongchun Ma graduated from the Institute of Mental Health at King’s College London. He is now the director of the Psychosomatic Department at the Tongde Hospital of Zhejiang Province. Engaging in research on psychosomatic diseases for a long time, he is a member of the Chinese Psychological Crisis Intervention Committee, the Academic Committee of Psychosomatic Medicine of Zhejiang Province and Chinese Psychological Consultant Professional Committee; Young member of Psychosomatic Medicine Branch of Chinese Medical Association and Zhejiang Psychiatric Medical Commission. He specialized in dealing with anxiety disorders and sleep disorders, combining medication and psychotherapy. Recently, his research focus on the subject of helping the students and workers get back to a functional life after recovery and looking into the possibility of establishing a Chinese model of mental rehabilitation.
Authors’ Contributions
Xin Ren and Wanli Huang – Participated in the conception and design of the study, performed the analysis, and wrote the manuscript.
Huiping Pan – Participated in the conception and design of the study, cleaning up the data.
Tingting Huang and Xinwei Wang – collected data.
Yongchun Ma – Participated in the conception and design of the study, collected data, and wrote the manuscript.
Compliance with Ethical Standards
Conflict of Interest
Not applicable.
Code Availability
Not applicable.
Research Involving Human Participants and/or Animals
Not applicable.
Informed Consent
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xin Ren, Email: renxin831@outlook.com.
Wanli Huang, Email: pungpungli@outlook.com.
Huiping Pan, Email: 690514272@qq.com.
Tingting Huang, Email: 624450885@qq.com.
Xinwei Wang, Email: 421803982@qq.com.
Yongchun Ma, Email: 13735806542@163.com.
References
- 1.2019-nCoV outbreak is an emergency of international concern. [http://www.euro.who.int/en/health-topics/emergencies/pages/news/news/2020/01/2019-ncov-outbreak-is-an-emergency-of-international-concern]. (Access Feb 16, 2020). [DOI] [PMC free article] [PubMed]
- 2.Update on epidemic situation of novel coronavirus-infected pneumonia by 24:00 on Feb 4, 2020. [http://www.nhc.gov.cn/xcs/yqfkdt/202002/17a03704a99646ffad6807bc806f37a4.shtml] (Accessed Feb 5, 2020).
- 3.WHO Coronavirus Disease (COVID-19) Dashboard. [https://covid19.who.int/]. (Accessed Apr 22,2020).
- 4.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 8.Celiac Disease. Rockville: Agency for Healthcare Research and Quality (US); 2004. [https://www.ncbi.nlm.nih.gov/books/NBK35149/]. (Accessed Feb 5, 2020).
- 9.Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int J Environ Res Public Health. 2020;17(7):2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, Qin M, Huang H. Work stress among Chinese nurses to support Wuhan for fighting against the COVID-19 epidemic. J Nurs Manag. 2020; 10.1111/jonm.13014. [DOI] [PMC free article] [PubMed]
- 12.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2020:1–10. [DOI] [PubMed]
- 13.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: who will be the high-risk group? Psychol Health Med. 2020:1–12. [DOI] [PubMed]
- 15.Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, Min BQ, Tian Q, Leng HX, Du JL, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020:1–9. [DOI] [PMC free article] [PubMed]
- 16.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maunder RG. Was SARS a mental health catastrophe? Gen Hosp Psychiatry. 2009;31(4):316–317. doi: 10.1016/j.genhosppsych.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, Lau YC, Wong JY, Guan Y, Tan X, Mo X, Chen Y, Liao B, Chen W, Hu F, Zhang Q, Zhong M, Wu Y, Zhao L, Zhang F, Cowling BJ, Li F, Leung GM. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- 21.Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020; 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed]
- 22.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, Yu J, Kang M, Song Y, Xia J, Guo Q, Song T, He J, Yen HL, Peiris M, Wu J. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nishiura H, Kobayashi T, Yang Y, Hayashi K, Miyama T, Kinoshita R, Linton NM, Jung SM, Yuan B, Suzuki A, et al. The rate of underascertainment of novel coronavirus (2019-nCoV) infection: estimation using Japanese passengers data on evacuation flights. J Clin Med. 2020;9(2):419. doi: 10.3390/jcm9020419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hall RC, Hall RC, Chapman MJ. The 1995 Kikwit Ebola outbreak: lessons hospitals and physicians can apply to future viral epidemics. Gen Hosp Psychiatry. 2008;30(5):446–452. doi: 10.1016/j.genhosppsych.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, Yao L, Bai H, Cai Z, Xiang Yang B, Hu S, Zhang K, Wang G, Ma C, Liu Z. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dealing with stress, anxiety, and grief during COVID-19. [https://directorsblog.nih.gov/2020/04/07/dealing-with-stress-anxiety-and-grief-during-covid-19/]. (Accessed Apr 14, 2020).
- 28.Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, Fernandes CMB, Goldbloom DS, Gupta M, Hunter JJ, Hall LMG, Nagle LM, Pain C, Peczeniuk SS, Raymond G, Read N, Rourke SB, Steinberg RJ, Stewart TE, VanDeVelde-Coke S, Veldhorst GG, Wasylenki DA. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lancee WJ, Maunder RG, Goldbloom DS, Coauthors for the Impact of SS Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv. 2008;59(1):91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed in this study are available from the corresponding author for the reasonable request.


