Abstract
An unidentified pneumonia outbreak was first observed in Wuhan, the capital of Hubei Province, China, in December 2019. WHO officially named the disease, Coronavirus Disease 2019 (COVID-19), and declared it as pandemic on Mar 11, 2020. Globally, there are more than 3 million confirmed cases with nearly 200,000 deaths. Hence, we aimed to perform a systematic review and pooled analysis of the current published literature on COVID-19 to provide an insight on the epidemiological and clinical characteristics of COVID-19 patients. A systematic search of published peer-reviewed articles that reported cases with demographical and clinical features of real-time reverse transcriptase polymerase chain reaction (rRT-PCR)–confirmed SARS-CoV-2 infection using MOOSE guidelines was conducted from December 1, 2019, to April 27, 2020, and 50 eligible articles were included for the final analysis. Review articles, opinion articles, and letters not presenting original data as well as studies with incomplete information were excluded. We included a total of 6635 patients from 50 articles, with 54.5 % being male. The predominant symptoms were fever (80.3%), cough (64.2%), and fatigue/myalgia (36.5%) and other symptoms including dyspnea, chest pain, and sore throat. We also found patients with GI symptoms like diarrhea (9.2%) and nausea/vomiting (5.2%). Comorbidities were found in 3,435 (51.7%) patients with the most common being hypertension (22.67%) followed by diabetes mellitus (12.78%). COVID-19 pandemic is not only leading a huge burden on health care facilities but significant disruption in the world society. Patients with coexisting comorbidities are at higher risk and need more utilization of health care resources. As this virus is spreading globally, all countries have to join hands and prepare at all levels of human resources, infrastructure, and facilities to combat the COVID-19 disease.
Electronic supplementary material
The online version of this article (10.1007/s42399-020-00393-y) contains supplementary material, which is available to authorized users.
Keywords: COVID-19, coronavirus disease, SARS-CoV-2, 2019-nCoV, pandemic, outbreak, epidemiology
Introduction
An unidentified pneumonia outbreak was first observed in Wuhan, the capital of Hubei Province, China, in December 2019 [1, 2]. WHO officially named the virus Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) and the disease, Coronavirus Disease 2019 (COVID-19) [3], and on Mar 11, 2020, declared COVID-19 as pandemic [4]. As on 4 May, 2020, there were 3,435,894 confirmed cases globally with 239,604 deaths globally [5].
Coronavirus is an enveloped, non-segmented, positive-sense single-stranded RNA virus with genome size ranging from 26 to 32 kilobases (the largest known viral RNA genome) [6]. COVID-19 is mainly transmitted by droplets and contact with contaminated surfaces or objects, showing human-to-human transmission, family aggregation spread, and nosocomial infection [7]. It is worth noting that COVID-19 has a diverse clinical presentation, ranging from asymptomatic infection to mild respiratory illness to more severe complications of pneumonia, Acute Respiratory Distress Syndrome requiring intensive care unit (ICU) admission, and mechanical ventilation.
While current research is focusing on outcomes and vaccine-development and therapeutics for COVID-19, there remain gaps in our understanding of the natural history of this disease. Recently, published observational studies have provided insights on the epidemiology of this pandemic, but there are limitations in the sample sizes and geographical locations for any definitive conclusions. Hence, we sought to conduct a pooled analysis of the current literature on COVID-19 providing an insight on the epidemiological and clinical characteristics of 6635 patients globally, while also studying image findings and comorbidities.
Methods
Objectives
The primary aim of this study was to evaluate the epidemiological and clinical characteristics of COVID-19 patients while also highlighting the comorbidities and radiological findings.
Search Method and Strategy
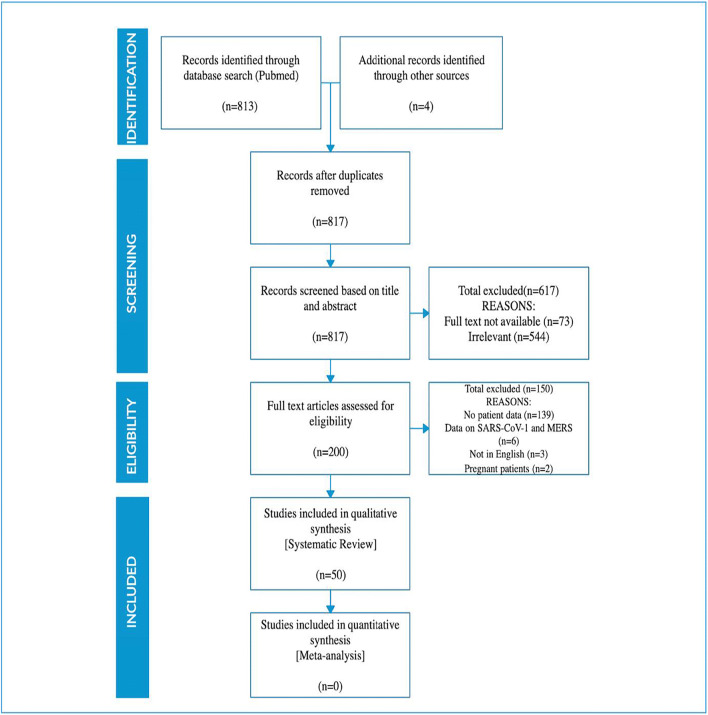
In order to evaluate the primary aim, we performed a systematic review of these observational studies, case series, and case reports according to PRISMA guidelines [8]. We searched the PubMed database for peer-reviewed published articles that reported cases with real-time reverse transcriptase polymerase chain reaction (rRT-PCR)–confirmed SARS-CoV-2 infection and have details on demographics, clinical symptoms, imaging features, and coexisting comorbidities. The database was searched from December 1, 2019, to April 27, 2020. The search was conducted using the following keyword/MESH terms: ((COVID-19[Title/Abstract]) OR coronavirus [Title/Abstract]) OR SARS-CoV- 2[Title/Abstract] OR 2019-nCoV [Title/Abstract]. All studies that had information on above mentioned characteristics in COVID-19 patients were included. Review articles, opinion articles, and letters or other articles with incomplete information and not presenting original data were excluded. Non-English literature, non-full text, and animal studies were also excluded. Abstracts were reviewed, and articles were retrieved accordingly. Two independent reviewers performed the search and literature screening (NK and HS), with disputes resolved by consensus following discussion with author (IG and RHK). For the ease of understanding, we used a flow diagram to describe literature search and study selection process in Fig. 1.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)
Data Collection
A prespecified data collection Excel sheet was used to collect the data relating to study characteristics of interest by two authors (NK and HS), and discrepancies were solved by a discussion with author (IG and RHK). The following study characteristics were extracted: publication year, country of origin, sample size, gender, clinical signs and symptoms, comorbidities, radiology findings, treatment utilized, and complications.
Statistical Analysis
All analysis was done in Excel and SAS 9.4. Percentages and means ± standard deviation (SDs) were calculated to describe the distributions of categorical and continuous variables, respectively.
Results
Our search resulted in 817 studies, out of which 617 non-human studies, non-full text and articles with non-English language information were excluded. Two hundred full-text studies were screened and assessed for eligibility; 150 studies with insufficient clinical information were excluded. The final analysis included 50 articles including observational studies, case series, and case reports, presented in Supplementary Table, including a total of 6635 patients to study the pattern and variations in the clinical presentation of the COVID-19 disease. Our review included studies from various countries from across the globe, mainly from China followed by the USA, Germany, Italy, Vietnam, Thailand, Canada, Nepal, and Korea.
Epidemiological and Clinical Characteristics (Table 1)
Table 1.
Epidemiological and clinical characteristics of confirmed COVID-19 cases
| Variables | All patients (n = 6635) | |
|---|---|---|
| Total | Percentage (%) | |
| Clinical symptoms | ||
| Fever | 5325 | 80.3 |
| Cough | 4262 | 64.2 |
| Fatigue/Myalgia | 2422 | 36.5 |
| Sputum | 1671 | 25.2 |
| Shortness of breath | 1187 | 17.9 |
| Headache/dizziness | 859 | 12.9 |
| Sore throat | 635 | 9.6 |
| Diarrhea | 627 | 9.4 |
| Chills | 477 | 7.2 |
| Nausea/Vomiting | 343 | 5.2 |
| Nasal congestion | 209 | 3.1 |
| Loss of appetite | 132 | 2.0 |
| Rhinorrhea | 75 | 1.1 |
| Chest pain | 60 | 0.9 |
| Hemoptysis | 37 | 0.56 |
| Impaired consciousness | 25 | 0.38 |
| Rigors | 24 | 0.36 |
| Conjunctival congestion | 19 | 0.29 |
| Impaired taste | 12 | 0.18 |
| Impaired smell | 12 | 0.18 |
| Impaired vision | 3 | 0.05 |
| Ataxia | 1 | 0.02 |
| Seizures | 1 | 0.02 |
| Imaging findings | ||
| Computed tomography (CT) findings | 1655 | 24 |
| Comorbidities | ||
| Hypertension | 1504 | 22.67 |
| Diabetes mellitus | 848 | 12.78 |
| Cigarette smoking | 309 | 4.66 |
| Cardiovascular disease | 254 | 3.83 |
| Pulmonary disease | 170 | 2.56 |
| Cerebrovascular disease | 73 | 1.10 |
| Malignancy | 70 | 1.06 |
| Chronic kidney disease | 66 | 0.99 |
| Gastrointestinal disease | 53 | 0.79 |
| Hepatitis B | 51 | 0.77 |
| Immunosuppression | 15 | 0.23 |
| Obstructive sleep apnea | 11 | 0.17 |
| HIV infection | 3 | 0.05 |
| Alcohol consumption | 2 | 0.03 |
| Organ transplant | 2 | 0.03 |
Out of 6635 confirmed COVID-19 patients, there was higher percentage of male patients (3617 (54.5%)) than female (3007 (45.3%)) and children (11 (0.2%)). In regard to clinical presentation, fever was the most common symptom, seen in 5325 (80.3%) patients, followed by cough (4262 (64.2%)), fatigue/myalgia (2422 (36.5%)), sputum production (1671 (25.2%)), and dyspnea (1187 (17.9%)). Lesser common symptoms include diarrhea in (627 (9.2%)) patients, followed by chills in (477 (7.2%)) patients, followed by nausea/vomiting (343 (5.2%)), nasal congestion (209 (3.1%)), loss of appetite (132 (2.0%)), and rhinorrhea (75 (1.1%)).
Computed tomography (CT) scan was performed on 1655 patients (24.9%), mainly revealed ground glass opacities in the majority of the patients. Few patients showed imaging features of pleural effusion and consolidation involving one or multiple lobes. Most common co-morbidities were hypertension 1504 (22.67%) followed by diabetes mellitus (848 (12.78%)), smoking (309 (4.66%)), pre-existing cardiovascular disease (254 (3.83%)), pulmonary disease (170 (2.56%)), and cerebrovascular disease (73 (1.10%)).
Discussion
Over the past five months, more than 5 million COVID-19 cases have been confirmed across the globe with nearly 300,000 deaths globally [9]. COVID-19 is a new clinical disease and an emerging condition alarming the preparedness at different levels. This pandemic urges continuous efforts in various fields of epidemiology, therapeutic and diagnosis, and preventive medicine globally [10, 11]. In setting of COVID-19 outbreak, many critical questions have arisen regarding disease severity ranging from asymptomatic to mildly symptomatic, to severe requiring ICU admission, to death [12]. Hence, in this systematic review and pooled analysis of 6635 confirmed COVID-19 cases from across the world, we have summarized critical information regarding epidemiology, clinical symptoms, radiology findings, and coexisting comorbidities of new COVID-19 infectious disease to have greater knowledge of the evolving pandemic.
In our pooled analysis, the most common symptoms of COVID-19 include fever, cough, fatigue/myalgia, sputum, and dyspnea along with other clinical symptoms. These findings of our study align with initial studies from China [2, 13, 14] and was also observed in all the studies included in this study including case series and case reports. The frequency of fever in COVID-19 is similar to SARS and MERS [15]; however, diarrhea is reported in 20–25% of SARS and MERS patients [16], but in our study only 9.2% patients had reported diarrhea. Our study findings are consistent with Rodriguez-Morales et al. [17] metanalysis of 635 patients, who reported 6.3% of COVID-19 patients with diarrhea. Furthermore, few COVID-19 patients may have mild symptoms, which can be easily overlooked [18], and few patients may be asymptomatic, which makes it difficult to detect and isolate such carriers on time, further making it difficult to contain the spread [19]. Interestingly, some of the rare presenting symptoms in our cohort include rhinorrhea, hemoptysis, chest pain, loss of smell, loss of taste, and raising suspicion of COVID-19 disease. Majority of the study patients had co-existing comorbidities, with most common being hypertension, diabetes, and cardiovascular disease. Early identification of such high-risk patients will help in better utilization of health care resources for more severe COVID-19 patients.
COVID-19 disease may have clinical course similar to SARS. However, case–control studies are required to better understand the clinical evolution of the disease [20]. During the initial stage its presentation is similar to SARS coinciding with the recent viral load data reported by the Zou et al. [21]. As the disease progress, SARS-CoV-2 affects lower respiratory tract as seen on CT scan of our patient cohort with majority having bilateral ground-glass opacities in the peripheries and mostly in the posterior aspects of lungs. A proportion of patients also exhibit consolidative changes. According to the published literature till date, COVID-19 patients may have typical imaging features including ground-glass opacities, consolidation, enlarged lymph nodes, and cavitating nodules. These lesions can be peripheral or bilateral but help in screening of suspected cases, knowledge of extent of the disease, and managing of the severe cases [22].
Most of our study findings are consistent with first metanalysis published by Rodriguez-Morales et al., which included articles until February 23, 2020 [17]. Hence, our study findings have added to the existing literature of epidemiology, clinical characteristics, and common coexisting comorbidities. The biggest strength of our study is that the results are robust due to the pooled analysis of large sample size of 6635 patients after combining all the studies globally. However, our study has few limitations. The clinical data in our study results are mainly from published studies in China. Hence, there is need for more research data from other geographical locations like the USA, Spain, Italy, and others which have faced the surge of the pandemic to explicate the spectrum of the disease and complications in patients with COVID-19 and its associated outcomes based on the large sample size and representing global population.
Conclusion
This systematic review and pooled analysis of the current literature on COVID-19 provide insight on the epidemiological characteristics and clinical manifestation of the disease with wide range of typical and atypical manifestations of the disease. We also focused on the comorbidities associated with COVID-19 patients, which can help clinicians in early screening of high-risk patients and wise utilization of health care resources in these patients to prevent more severe disease. With the pandemic unfolding, research is the need of the hour. Even with massive amounts of publications, there remain gaps in the understanding of the natural history of the disease. Hence, there is still need for more extensive studies with short- or long-term follow up assessments and with large sample sizes from different countries facing the pandemic other than China to have good characterization of the course of this new COVID-19 disease.
Electronic supplementary material
(DOCX 96 kb)
Author contributions
NK conceived of the idea. NK, IG, and HS reviewed the literature and collected the data with the help of RK, AA, and AH. NK and IG performed biostatistical analysis with the help of UP. HS and RK formulated the tables. NK, IG, HS, RK, AA, and AH wrote the main draft of the manuscript with support of UP and PM. PM supervised the project.
Compliance with Ethical Standards
Conflict of Interest
We declare no competing interests. The authors report no disclosures relevant to the manuscript.
Informed Consent
The data used in this study are publicly available and de-identified database thus informed consent or IRB approval was not needed for this study.
Footnotes
This article is part of the Topical Collection on Covid-19
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/s0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naming the coronavirus disease (COVID-19) and the virus that causes it. World Health Organization. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. Accessed 2020 March 23.
- 4.Coronavirus disease 2019 (COVID-19) Situation Report – 51 World Health Organization. March 11, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10. Accessed March 15 2020.
- 5.COVID-19 CORONAVIRUS PANDEMIC. Worldometer. 2020. https://www.worldometers.info/coronavirus/. Accessed May 4 2020.
- 6.Li G, Fan Y, Lai Y, Han T, Li Z, Zhou P, et al. Coronavirus infections and immune responses. J Med Virol. 2020;92. 10.1002/jmv.25685. [DOI] [PMC free article] [PubMed]
- 7.Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19 CORONAVIRUS PANDEMIC. Worldometer. 2020. https://www.worldometers.info/coronavirus/. Accessed May 20 2020.
- 10.Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paules CI, Marston HD, Fauci AS. Coronavirus infections—more than just the common cold. Jama. 2020. 10.1001/jama.2020.0757. [DOI] [PubMed]
- 12.Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19—studies needed. N Engl J Med. 2020;382(13):1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 13.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/s0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yin Y, Wunderink RG. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology (Carlton, Vic) 2018;23(2):130–137. doi: 10.1111/resp.13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/s0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yaqian M, Lin W, Wen J, Chen G. Clinical and pathological characteristics of 2019 novel coronavirus disease (COVID-19): a systematic review. medRxiv. 2020;2020.02.20.20025601. 10.1101/2020.02.20.20025601.
- 19.Wang F-S, Zhang C. What to do next to control the 2019-nCoV epidemic? Lancet. 2020;395(10222):391–393. doi: 10.1016/S0140-6736(20)30300-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Srikantiah P, Charles MD, Reagan S, Clark TA, Pletz MW, Patel PR, et al. SARS clinical features, United States, 2003. Emerg Infect Dis. 2005;11(1):135–138. doi: 10.3201/eid1101.040585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am J Roentgenol. 2020;214(5):1072–1077. doi: 10.2214/ajr.20.22976. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 96 kb)