Introduction
On the basis of recent changes to blood pressure (BP) guidelines1, some 46% of Americans (a further 31 million people) are now classified as having hypertension (BP ≥130/80 mmHg). This new classification recognizes the recent clinical trial evidence regarding the benefits of lower BP targets2 and, among other factors, emphasizes the importance of considering how non-pharmacological strategies (i.e., lifestyle modification) can be better incorporated into broader prevention messages3. In this context, and with conventional guidelines focusing on moderate-vigorous physical activity, there is unrealized potential for benefitting a large proportion of the at-risk population through broadening the range of physical activity options in ways that might be more amenable to lifetime adherence.
Although the benefits of a physically active lifestyle for overall cardiometabolic health – including BP control – are well known4–7, a large and growing proportion of the global population are physically inactive8, 9. Worksites, schools, homes and public spaces are physically engineered and socially arranged in ways that minimize regular movement and muscular activity, and maximize the time spent sitting. This is against a background of unprecedented demographic shifts associated with the aging of populations, with higher proportions experiencing more years of frailty, a range of chronic non-communicable diseases and risk factors, and poorer physical function and quality of life. Aside from contributing significantly to increases in healthcare costs, these combined factors represent a formidable set of clinical and public health challenges.
The contribution of low rates of participation in moderate-vigorous physical activity to the chronic disease burden has provided the impetus to explore the efficacy of physical activity options which are more amenable to lifetime adherence and that have broader population reach. In this regard, emerging strategies focusing on reducing and changing the patterns of sedentary behaviors (put simply, too much sitting) may have potential for lowering the incidence and prevalence of hypertension, as well as minimizing medication use in those already treated.
Through a hypertension lens, this review focuses on the potential health implications and some of the plausible counter-measures for the high volumes of prolonged sitting that now characterize modern lifestyles. We synthesize findings on the specific relationships of sedentary behavior with BP – which primarily are from observational and acute experimental studies – including a discussion on the relevant cardiovascular mechanisms. We also consider what will need to be better understood as a basis for evidence-based recommendations on sedentary time in the context of BP control, and identify evidence gaps for future research.
Sedentary Behavior: a Newly-Identified Element for Chronic Disease Risk and a Target for Management
Regular moderate-vigorous physical activity is well-established as an effective tool in the prevention and management of multiple chronic diseases, including hypertension4, 7. However, in recent years, sedentary behavior – defined as “any waking behavior characterized by an energy expenditure ≤1.5 metabolic equivalents (METs) while in a sitting or reclining posture” – has received increasing attention as a clinical and population health problem that is additional to insufficient moderate-vigorous physical activity10. Reasons for this new perspective around sedentary behavior largely stem from three key points (expanded upon below). For clarity and distinction, we refer to recommended amounts of moderate-to-vigorous intensity physical activity as ‘‘exercise’’ and use the terms “sitting” and “sedentary behavior” interchangeably throughout this paper7.
1) Modest uptake and adherence to exercise guidelines: Despite the multitude of potential health benefits derived from regular physical activity, population uptake is low. One-third of many adult populations (about 1.5 billion people globally) and four-fifths of adolescents do not adhere to minimum recommended levels of moderate-vigorous physical activity8. While leisure-related physical activity levels have tended to remain relatively steady over time, physical activity at work, in the domestic environment and in transportation have all decreased in recent decades8, 9. Sustained and growing concerns also exist around the limited uptake and adherence to exercise guidelines in longer-term trials11 and in accordance with national/global activity guidelines, particularly for older adults and in deconditioned/clinical populations8, 12–15.
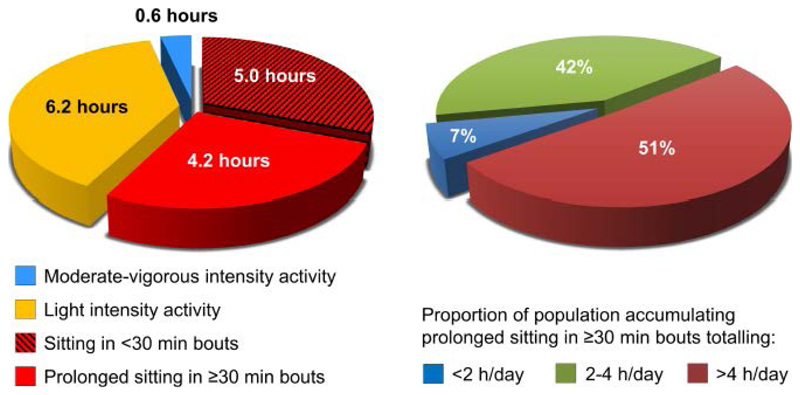
2) High volume of waking hours spent sedentary: In developed countries, and in the rapidly urbanizing populations of developing countries, sedentary behaviors have become the primary default behavioral option – inextricably embedded in work, school, transport, and leisure-time. Data obtained from studies using accelerometers, mainly from America and Australia, indicates that adults spend on average 55–70% of their waking hours (or over 8-10 hours/day) engaged in sedentary behaviors16–18. Furthermore, recent Australian-based data (AusDiab3) suggests that just under half of the ~9 hours of total sitting time (as measured by posture-sensitive accelerometers)19 is spent in prolonged unbroken bouts of greater than 30 minutes, and that just over half of all adults accumulated more than 4 hours per day of their sitting time in this manner (Figure 1).
Figure 1.
Unpublished data from the AusDiab3 cohort showing how a sub-sample of Australian adults (n=717, aged 36-80 years) allocate their physically-active and sitting time during waking hours on average (derived from both ActiGraph™ and ActivPAL™ activity monitors and normalized to 16 hours). These data highlight the high volumes of sitting time typically observed, and the proportion of people that accumulated sitting time in “prolonged” unbroken bouts (≥30 minutes). Note that moderate-vigorous intensity activity is calculated based on every minute of activity accumulated over the day (i.e. not just in “exercise” bouts of 10 min or more).
3) Evidence on the associations of total sedentary time, and its pattern of accumulation, with cardiometabolic risk: Prospective epidemiological evidence suggests that high volumes of sedentary time are associated with premature mortality and cardiometabolic risk biomarkers for type 2 diabetes, cardiovascular disease, and certain cancers. These deleterious associations are partly moderated by time spent in moderate-vigorous physical activity, but are particularly evident in those who undertake insufficient or no moderate-vigorous physical activity7, 20, 21. Furthermore, accumulating observational and experimental evidence indicates that specific patterns of sedentary time (i.e., whether sitting is undertaken in prolonged or regular intermittent bouts) may be differentially associated with a number of cardiometabolic risk biomarkers and premature mortality19, 22–25. For example, a recent large-scale observational study found that both total sedentary time and prolonged uninterrupted sedentary bouts were associated with an increased risk for all-cause mortality, after controlling for moderate-vigorous physical activity and traditional cardiovascular risk factors24. Another recent cross-sectional study, using inclinometer data from a subset of AusDiab3 participants (also see Figure 1 from the same cohort), showed that both greater amounts of sitting time and prolonged sitting time were deleteriously associated with waist circumference, BMI, HDL-cholesterol, triglycerides, 2-hour post-load glucose, and fasting plasma glucose23.
As a result, leading health agencies such as the American Heart Association26 and the American Diabetes Association27 have begun to acknowledge the likely clinical and population health impact of changing sedentary behaviors. Consideration of the mechanistic linkages of reducing and breaking up prolonged sitting with BP control and hypertension is highly relevant in this context. Indeed, evidence from epidemiologic observational studies and a new body of findings from acute experimental trials can provide helpful insights.
Sedentary Behavior and BP Control
Measurement challenges
There are significant challenges in objective quantification of both physical activity patterns and blood pressure, which make relational investigations difficult28, 29. Most observational studies examining associations of sedentary behavior with BP and hypertension have typically relied on self-reported daily sitting or television/screen viewing time – methods that are susceptible to recall and response bias, social desirability, and under- or over-reporting28. Accelerometer-derived measures of movement and posture have been employed more recently to more “objectively” characterize sedentary and active behaviors, as they are less subject to the biases that are inherent to self-report. However, they are not without limitations. For example, these newer methods cannot determine the behavioral contexts (i.e., the location and purpose of these behaviors) and results may be influenced by wear-time differences, some activity misclassification (depending on device type/location), and data analysis approaches.
Particularly under conditions of normal daily living, BP measurement is associated with additional challenges. BP is an inherently labile parameter, with considerable temporal variation from heart beat to heart beat and across the 24-hour day. Thus, interpretation of a single time-of-day BP must be in a behavioral context which considers additional factors, such as dietary and fluid intake, physical activity, emotions, stress and drugs (including caffeine and nicotine). In addition, BP measurements can be dramatically affected by the “white coat” or “masked” effects in clinic/office settings, and is often measured under a variety of conditions (e.g., postures) with differing preceding rest periods. Although not without limitations, 24-hour ambulatory BP has better prognostic value than single office BP measurements, and is thus considered the reference standard to diagnose hypertension according to certain groups29.
The above measurement challenges likely contribute to variability in observational evidence on the associations of sedentary behavior with BP and hypertension (almost always assessed via resting office BP). Indeed, such evidence to date has been quite heterogeneous and inconsistent30–34, with relatively small mean effect sizes.
Observational evidence
In a recent systematic review and meta-analysis, Lee and Wong35 examined the associations of time spent in sedentary behaviors with BP in both adults and children. Of the 28 studies included in the meta-analysis (8 longitudinal, 20 cross-sectional), 10 assessed sedentary behavior via accelerometry and the remainder used self-report measures (i.e., television/screen viewing time, sitting time, or both). Results from this meta-analysis revealed that for each hour increase in self-reported sedentary behavior there was an associated small increase in systolic and diastolic BP of 0.06 (95% CI: 0.01-0.11) and 0.20 (0.10-0.29) mmHg, respectively. Additionally, for each hour increase in sedentary behavior there was a 2% elevation in risk for hypertension (OR=1.02, 95% CI: 1.003–1.03).
Interestingly, no significant associations were observed when sedentary time was assessed via accelerometry, although systolic BP was borderline significant at 0.10 (95% CI: -0.001 to 0.21, p=0.06) mmHg35. These discrepancies between the self-report and device-based exposure measures suggest either differences in measurement variability, validity and reliability (for both the sedentary behavior and the resting BP measures), poorer compliance with the use of the accelerometers (which has been shown to be lower in those with hypertension36), or that the disparity in timing of office BP measurements in relation to the active/sedentary behaviors and other factors (as mentioned previously) may also be important.
In one of the few observational studies to utilize both 7-day accelerometry and ambulatory BP measures, Hamer et al.,37 showed, in a sample of 216 middle-aged Black- and Caucasian-African school teachers with or at high risk of hypertension, that the positive associations of sedentary time with 24-hour BP (but not daytime or resting office BP) were primarily driven by the night-time readings. Further analyses showed that participants in the highest sedentary tertile were also more likely to be night-time ‘non-dippers’ (OR=2.11, 95% CI: 0.99–4.46, p=0.052) compared with those in the lowest sedentary tertile. These night-time specific BP findings for the more sedentary participants are intriguing, since ambulatory BP-derived sleep BP (presence/absence of dipping) tends to be a more stable BP measure, and is a stronger predictor of cardiovascular risk, independent of office BP or wake-time BP38. The findings could be due to elevated night-time sympathetic activation, which is consistent with the findings from one experimental study demonstrating higher plasma noradrenaline levels during prolonged sitting39. Alternatively, BP readings are generally more stable nocturnally. However, there is also the potential for measurement issues, since study participants were required to sleep in unfamiliar surroundings at the overnight clinical facility. Importantly, the study also showed that those who spent less daily time in light-intensity physical activity (the corollary of spending more time sedentary) had significantly higher 24 h ambulatory and daytime systolic and diastolic BP, as well as higher resting systolic BP.
It is thus difficult to draw any firm conclusions from the observational evidence to date. The question of whether sedentary behavior is an acute BP “stressor”, as distinct from other conventional risk factors which contribute to sustained BP elevation (e.g., age, obesity, diabetes), is difficult to disentangle. Ambulatory BP measures may be better suited for studying the patterning of BP on days characterized by periods of prolonged sitting. Thus further prospective study evidence using ambulatory BP methods, and with more detailed sensor-assessed measures of sitting patterns per se and their context, would be highly informative. Consideration of the specific population (e.g., normotensive and uncomplicated hypertension, medication) in these contexts will also be important.
Experimental evidence
Few studies have examined the effects of prolonged sitting on BP (see Supplementary Table S1 for a summary of the relevant acute studies published to date). Most studies39–45, but not all46, 47, have observed significant systolic or diastolic BP-lowering effects when prolonged sitting time has been reduced or interrupted (mostly with walking breaks, but also some with standing breaks), ranging from 1 to 16 mmHg in magnitude. However, the majority of studies have generally included BP as a secondary endpoint, which may limit the rigor and interpretability of the BP findings.
Although not an entirely consistent phenomenon, reductions in BP with activity-breaks in prolonged sitting have tended to be more modest in the physically active healthy-younger populations, but most pronounced in older, ‘at-risk’ populations and/or those with overt or pre-hypertension. For example, in inactive overweight/obese adults (over half of which were classed as having pre- hypertension or hypertension), interrupting sitting time with brief bouts of either light- or moderate-intensity walking significantly lowered resting systolic and diastolic BP by ~2–3 mmHg43. Similarly, reductions in resting systolic and diastolic BP of significantly greater magnitude (mean ↓14-16 and ↓8-10 mmHg respectively) were shown when sitting was interrupted with either light-intensity walking or with simple resistance activities in adults with type 2 diabetes (of which 88% were also hypertensive)39. These latter two laboratory-based studies support the contention that the magnitude of BP-lowering by interrupting sitting time, or the BP-increase with prolonged uninterrupted sitting, may be greater in hypertensive compared to normotensive groups. Moreover, BP-reductions in these two studies were established on top of standard antihypertensive medications.
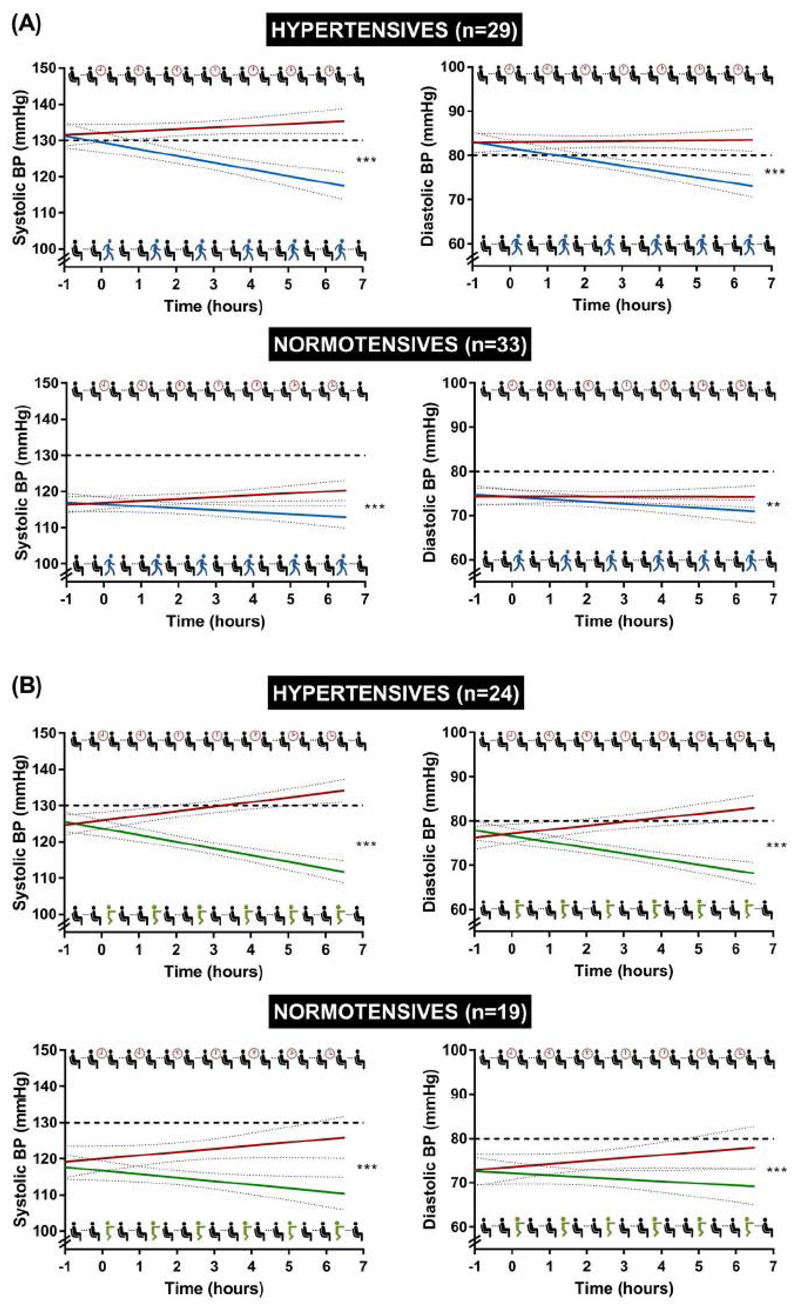
To further explore the hypothesis that those with hypertension may be more susceptible to BP elevation with prolonged sitting exposures, and/or derive more benefit from reducing and breaking up sitting time, we pooled data from four separate laboratory-based randomized cross-over trials. These studies examined the BP responses to prolonged uninterrupted sitting versus sitting interrupted by regular 2-3 minute walking breaks (Figure 2A) or by regular 3 minute simple resistance activity breaks (half-squats, calf raises, gluteal contractions and knee raises; Figure 2B) in overweight/obese adults with and without hypertension. Figure 2 and accompanying Supplementary Table S2 illustrate two key points:
-
(1)
that prolonged uninterrupted sitting appears to evoke increases in both systolic and diastolic BP in a manner proportional to the length of time spent sitting, and that the magnitude of these changes are generally greater and more clinically relevant in those with hypertension compared to normotensives;
-
(2)
and, that regular breaks in prolonged sitting with either light-walking breaks or simple resistance activity breaks reduces both systolic and diastolic BP by a greater magnitude for simple resistance activity breaks in both normotensive and hypertensive populations.
Figure 2.
Temporal changes in systolic and diastolic BP of pooled data from four separate crossover trials39, 43, 73, 85 employing similar experimental protocols in individuals with and without hypertension. (A) Lines represent line of best fit (with 95% CI, dotted lines) for uninterrupted sitting (red line) and sitting interrupted with short 2-3 minute walking breaks (blue line) every 20-30 minutes after a 1-hour steady-state period. (B) Lines represent line of best fit (with 95% CI, dotted lines) for uninterrupted sitting (red line) and sitting interrupted with short 3 minute simple resistance activities (green line) every 30 minutes after a 1-hour steady-state period. Hypertensive individuals defined by a combination of clinical diagnosis/medication use, or BP ≥130/80 mmHg at screening visit. Solid dashed line represents new US clinical thresholds for hypertension (>130/80 mmHg)1. Difference in slopes according to a linear mixed effect model adjusted for age, sex, BMI, treatment order and baseline values, ***P<0.001, **P=0.002 (see Supplementary Table S2 for further details on the statistical models/results).
The simple resistance activity breaks that have been employed in these recent trials were designed to provide an alternative option to walking breaks, which usually obliges a person to leave their immediate location. They require no specialized equipment and only small amounts of floor space. In addition, the compound/multi-joint nature of these activities engages a significant muscle mass in contractile activity, and when performed regularly, could increase functional capacity and insulin sensitivity through maintenance or increases in muscle mass and adaptations in metabolic enzymes. These factors may be particularly relevant for overweight and ageing populations with hypertension48, the vast majority of whom do not engage in sufficient moderate-vigorous nor muscle-strengthening activities, in accordance with national activity guidelines7, 49. If these findings are corroborated by further studies and in a chronic context, there are potential implications for future targeting and optimization of physical activity/sedentary behavior interventions in these populations groups.
Recent studies have also started to include more detailed ambulatory BP measures over consecutive days and while simulating “free-living” scenarios, which is providing insight into the sustained effects of sitting-reduction interventions. For example, Zeigler et al., showed that pre-hypertensive, overweight/obese adults accumulating 2.5 h of standing or light-intensity physical activity across the day equally reduced systolic and diastolic ambulatory BP both during and after working hours by ~3–4 mmHg45 and ~2-13 mmHg44 respectively, compared to a simulated 8 hour seated workday. Using a comparable design and measures, Bhammer et al.,41 also showed similar reductions in systolic, diastolic and mean arterial BP (~5-6 mmHg) with moderate-, but not vigorous-intensity walking breaks, but these effects were only observed in the evening after the intervention period (outside of the laboratory).
The accumulation of the experimental findings described above are congruent with previous literature regarding the equally beneficial impact of fractionized vs. continuous exercise bouts50–54, and the potential for a light-intensity physical activity ‘threshold’ for BP lowering55, 56, which may even be related to simple postural changes (i.e., sit-to-stand transitions) across the day. Further prospective and longer-duration intervention studies of this nature, in more free-living settings and with ambulatory BP measures, will be important in elucidating whether prolonged sitting per se induces BP elevation. They will also assist in determining the efficacy and specificity of interventions that reduce and break up prolonged sitting time using a range of light-to-moderate intensity activities.
Teasing apart the impact of other confounding and interacting factors of everyday living, such as dietary, stress and sleep patterns, will continue to be a challenge – and may require more tailored study designs and advanced measurement and analytical approaches. The timing of BP measurements relative to activity and dietary factors will also be important, with a combination of parallel ambulatory BP measurements to determine BP reactivity in real-time, and well-standardized resting and ambulatory BP measures taken after the intervention period, in order to determine chronic BP changes.
Potential Physiological Mechanisms
Theoretical considerations
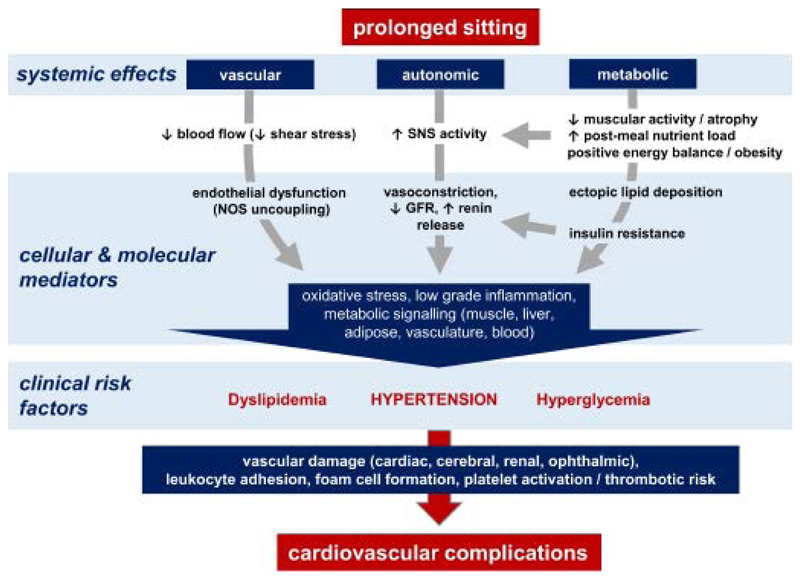
The potential underlying biological mechanisms by which a bout of prolonged sitting may acutely modulate BP are multiple, but ultimately must result from alterations in cardiac output and/or total peripheral resistance. In this context, mechanisms are likely to predominantly affect total peripheral resistance, and to include metabolic, autonomic and direct vascular mechanisms (Figure 3).
Figure 3.
Hypothesized mechanisms by which prolonged sitting may influence risk for hypertension and cardiovascular complications. Systemic reductions in metabolic demand and blood flow, and elevated sympathetic nervous system (SNS) activity, may evoke concurrent decrements in insulin sensitivity and vascular function, promoting oxidative stress and low-grade inflammatory cascades. When prolonged sitting is habitual, these factors likely contribute to the development of hyperglycemia, dyslipidemia and hypertension, promoting vascular damage and progression towards serious cardiovascular complications. GFR, glomerular filtration rate. NOS, nitric oxide synthase.
The concept that metabolism controls blood flow and thus drives pressure is a potentially important consideration with respect to understanding how prolonged sitting might modulate BP. Prolonged sitting is characterized by low energy expenditure or metabolic demand, as measured by indirect57, 58 and whole-room calorimetry59, where the average energy cost of common sedentary behaviors (reclining, watching television, reading, and typing on a computer) are narrowly banded around ~1.0 MET, even in the postprandial state59. Metabolic demand is the key determinant of blood flow in all tissues, with multiple mechanisms linking the metabolic requirements of tissues in terms of oxygen and substrates (glucose and fatty acids), to blood supply.
As described above, metabolic demand is low during prolonged sitting. Consequently, vasodilatory metabolites, including adenosine, are correspondingly low and the caliber of capillaries is therefore minimized. It would be expected that low metabolic demand would result in closure of precapillary sphincters and the shutdown of nutritive capillary beds (Figure 4). Capillary closure as a result of low metabolic demand within muscles reduces the pressure differential with upstream feed arteries, thus reducing blood flow via simple hemodynamics. As a consequence, vascular shear stress is reduced, promoting vasoconstriction through associated endothelial mediators (i.e., reduced nitric oxide and increased endothelin-1). Low metabolic demand therefore has the potential to increase peripheral resistance and drive BP up through effects at multiple levels of the vascular tree. A seated posture creates bends and constrictions in major blood vessels of the lower limbs, particularly under the thighs60. Such effects may result in simple mechanical increases in peripheral resistance, but also promote turbulent blood flow patterns, which may have acute and chronic consequences for blood flow and pressure regulation61, 62.
Figure 4.
Hypothesised vascular mechanisms by which prolonged sitting may impact on blood pressure in contrast to sitting interrupted by regular active breaks. During prolonged sitting (left side): (a) low metabolic/ATP demand within muscles results in low levels of vasodilator metabolites, constriction of pre-capillary arterioles, and closure of precapillary sphincters. This in turn results in blood being shunted through metarterioles. (b) Reduced pressure differential between capillaries and upstream muscular (distributing) arteries reduces blood flow and endothelial shear stress, promoting vasoconstriction through associated endothelial mediators (i.e., reduced nitric oxide and increased endothelin-1), and (c) reduced calibre of resistance arterioles, increasing peripheral resistance and BP. During brief 2-3 minute activity bouts during prolonged sitting (right side): (d) increased metabolic/ATP demand within muscles results in upregulation of vasodilator metabolites, dilation of precapillary arterioles and relaxation of precapillary sphincters, promoting flow through nutritive capillaries. (e) The greater pressure differential between capillaries and upstream muscular (distributing) arteries increases blood flow and endothelial shear stress, promoting vasodilation through associated endothelial mediators, and (f) increased calibre of resistance arterioles, reducing peripheral resistance and BP. Previously observed alterations in circulating noradrenaline (NA) during these two states are also depicted, along with endothelin-1 (ET-1) and nitric oxide bioavailability (NO), for which the evidence is only preliminary.
A further consideration is that increased hydrostatic pressure and reduced venous return (i.e. via insufficient calf muscle pump activity) while seated also leads to fluid accumulation in the lower limbs that is proportional to the time spent sitting63–65. This fluid accumulation during the day likely shifts rostral overnight and is hypothesized to predispose or exacerbate obstructive sleep apnea – particularly in those with congestive heart failure or at increased risk for obstructive apnea66–68 – which has been associated with nocturnal hypertension and non-dipping BP patterns67. Significant peripheral edema may also have implications for night-time BP elevation via carotid baroreceptor unloading (due to increased interstitial pressure), reduced baroreceptor afferent activity, and therefore a reflex increase in efferent sympathetic activity – but these mechanistic links remain untested in the context of prolonged sitting.
Over time, habitual physical inactivity and high volumes of prolonged sitting are likely to result in weight gain, muscle atrophy, vascular rarefaction (reducing vascular volume), endothelial damage and stiffening of large arteries, potentially contributing to sustained elevation in peripheral resistance and hypertension. In this context, controlled chronic studies are required, in order to better understand any such longer-term structural and functional changes.
Given that prolonged sitting occurs over hours, concurrent behaviors are integral to the consideration of mechanistic influences on BP. Foremost among these is food intake, which will induce a higher nutrient load in the context of prolonged sitting, where muscular activity and hence energy expenditure are relatively low. The exaggerated elevations in circulating glucose and insulin levels documented to occur with prolonged sitting in association with feeding would be expected to cause sympathoexcitation and noradrenaline release from arterial nerve terminals. This represents another plausible pathway which may contribute to BP elevation during a bout of prolonged sitting.
A final issue to consider is that physical activity-induced muscle contraction, whether through multiple breaks in sitting or via a continuous bout, will have opposing effects on mechanisms associated with prolonged sitting by promoting energy metabolism and vasodilation.
The autonomic effects of brief activity bouts are more complex. While systolic BP, in particular, increases acutely during the performance of an activity (predominantly due to resting BP between a day of prolonged sitting and a day of prolonged sitting interrupted by brief activity bouts may be related to:
-
(1)
increases in BP from baseline mediated by prolonged sitting, and
-
(2)
decreases in BP from baseline mediated by activity bouts.
While the physiological basis of the proposed mechanisms described above is sound, their validity requires testing in controlled laboratory studies which consider real-world behaviors, including food intake and stress that are present in different contexts (e.g., at work, during transportation, in leisure time).
Evidence
As noted earlier, the body of evidence on the mechanisms by which prolonged sitting may impact BP is in its infancy. While there are significant challenges to understanding the chronic BP effects in this context, acute physiological studies are providing some evidence to support the theoretical concepts discussed above. A number of studies have convincingly documented a prolonged sitting-induced increase in accumulation of extra-vascular fluid in the legs63, 65–68 and a decline in leg flow-mediated dilation and/or shear stress measured in the superficial femoral70–73 and popliteal74, 75 arteries. These effects can be mitigated by various interventions promoting increased metabolic demand, muscle pump activity, and/or vasodilation, including frequent short low-intensity activity breaks72, 73, static standing74, fidgeting70, calf/lower leg exercises while sitting68, 76, bouts of cycling74 or walking71 and heating75.
Direct measurement of vasoactive mediators (neurotransmitters and endothelium-derived factors) is challenging, since blood levels do not accurately reflect the physiologically relevant concentrations within the vasculature, and because some (e.g., nitric oxide) have very short half-lives. There is however some evidence for elevation in vasoconstrictor mediators in response to prolonged sitting. In patients with type 2 diabetes, Dempsey et al., observed an 11-18% increase in circulating noradrenaline in association with BP elevations of 10/5 mmHg during prolonged sitting39. These effects were mitigated by a magnitude similar to that typically achieved with pharmacological treatments if sustained77, by interrupting prolonged sitting with brief bouts of light-intensity walking or simple resistance activities. It is also interesting that these effects were present even though 67% of participants in this study were medicated for hypertension and took their medications on the experimental days.
The expected downstream effects of sympathetic activation, including on the reninangiotensin-aldosterone system, are yet to be studied in the context of prolonged sitting. Vasoactive endothelium-derived mediators are also likely important in the context of prolonged sitting exposures (see Figures 3 and 4), but evidence on these and other such mechanistic candidates is currently lacking. As previously mentioned, downregulation of nitric oxide due to shear stress reductions is probable. In addition, there is consistent evidence that prolonged sitting increases insulin resistance relative to regular activity breaks, particularly in those who have type 2 diabetes25. Insulin resistant states are associated with marked impairments in insulin-mediated vasodilatation and capillary perfusion of skeletal muscle, through endothelial mechanisms involving impaired nitric oxide bioavailability78 and endothelin-1 upregulation79–81. Indeed, a recent study in overweight/obese adults showed that endothelin-1 levels are higher during a bout of prolonged sitting compared with sitting interrupted every 30 minutes by three minutes of simple resistance activities; however, prolonged sitting per se did not elevate endothelin-173. Insulin may also promote the expression of pro-atherogenic mediators including the intracellular adhesion and vascular cell adhesion molecules82. Taken together, it could be speculated that prolonged sitting-induced shear stress reduction, combined with impairments in lower limb arterial function and dilation71, 72, 83 and the above CVD risk factors, may promote a pro-atherogenic environment. However, further investigations are required in order to elucidate the specific vascular mechanisms relevant to prolonged sitting, and its interruption by short activity breaks.
Mechanisms – summary
Preliminary evidence suggests that the BP-relevant effects of prolonged sitting include reduction in conduit vessel flow and elevation in vasoactive mediators. Theoretical considerations indicate that these effects are likely driven by metabolic demand and capillary caliber, but studies to date have not extended to the microvessels. The mechanisms contributing to the effects of habitual prolonged sitting on BP over an extended (chronic) period are indeterminate and will be challenging to investigate. Current knowledge of the cellular and molecular mediators of vascular pathophysiology would implicate chronic low grade inflammation and oxidative stress, as well as structural effects promoting vascular stiffening84 as intermediaries between acute hemodynamic changes and manifestations of clinical hypertension (Figure 3).
Summary and Future Directions
Through a hypertension lens, we have highlighted potential new clinical and population health implications of sedentary behavior; also synthesizing the available evidence on prolonged sitting with respect to BP control. In this context, we have discussed the plausible mechanisms and the associated emerging evidence. While there are notable gaps in the currently available research literature on sedentary behavior and BP, accumulating experimental evidence points to the potential importance of reducing and breaking up prolonged sitting for BP control, particularly in those who are more ‘at risk’, prehypertensive or hypertensive.
These findings reemphasize the major role that all aspects along the human movement continuum – from sedentary behavior through to moderate-vigorous physical activity – can play in influencing overall health and cardiovascular function. Initial evidence also hints that prolonged sitting per se may exert both direct and indirect effects on BP; however, much still remains to be understood and clarified. This area of research may be particularly important in the context of the recently revised US guidelines for the diagnosis, treatment, and management of hypertension2, which now recognize the vital importance of incorporating lifestyle approaches into broader clinical and population health messages. In this context, we can offer some new directions for future research:
Longer-term exposures and interventions
There remains an urgent need for more chronic experimental trials and intervention-study evidence from real-world settings such as clinics and workplaces – with high quality BP measures as primary outcomes, sufficient controls, and adequate sample sizes/statistical power to detect changes. Such evidence will be required to determine the composition of sitting-reduction interventions that will have the largest impact on BP control and hypertension risk, and whether BP changes can be sustained over longer periods. This would also contribute to the elucidation of potential mechanisms by which both acute and longer-term interventions interrupting prolonged sitting may reduce BP.
More advanced measurement tools and analytic methods
To fully understand the interrelationships between sedentary behavior, physical activity and BP, it is crucial to have high-quality and accurate measures of both the exposure and the outcome. The integration of data from devices that are able to accurately assess both posture and activity patterns/intensities in real-time, alongside both office and ambulatory BP measures, should be emphasized in future research. Additionally, analytical techniques such as isotemporal substitution modelling and compositional data analysis will allow researchers to better account for the inevitable interdependencies and interactions between sedentary behaviors, physically active behaviors and sleep across the 24-hour day.
Identifying the optimal doses, patterning and timing of sedentary behaviors
Although there is acute evidence that reducing and breaking up prolonged sitting time with a range of light-moderate intensity activities may be beneficial for BP control, much less is known about the specific dose-related and patterning effects of these behaviors. The ‘ideal’ balance between sedentary behavior and physical activity for BP control is yet to be defined. Questions still remain around the optimal durations and thresholds of prolonged sitting time for BP control, and what range of postural or activity perturbations from sitting (i.e., frequency, type/mode, duration, timing and intensity) can produce the most benefit. These questions are inevitably complex, as the “ideal” patterning of sedentary and physical activity behaviors is likely to be based on the requirements, context, and activity/health status of the subpopulation, rather than a “one size fits all” approach. As such, more in-depth examination of the behavioral targets and feasibility to change in different populations will be informative in optimizing future intervention efforts.
Mechanisms, contexts and interacting effects
Evidence on the relative and/or integrated importance of the physiological states considered earlier in mediating the potential detrimental effects of prolonged sitting remains limited. Identifying the relevant mechanisms associated with prolonged sitting exposures, along with their relevant contexts and settings (e.g., workplace, leisure, transportation, TV/screen time), will be important in providing an informed basis for clinical guidelines and public health targets. With this in mind, the impact on BP of reducing and breaking up prolonged sitting may interact with specific phenotypes, including but not limited to: gender, menopausal status, adiposity, age, ethnicity, genetic profiles, sleep, dietary habits, smoking, alcohol intake, medications, current cardiorespiratory fitness and baseline physical activity levels, and populations with or at increased risk of chronic diseases. In the future, delivery of both broad-based preventive messages, as well as tailored programs for particular ‘at risk’ groups, will help maximize population-health benefits, while minimizing the likelihood of ineffective approaches. Put simply: how, why and where is it important to change sitting time, and in whom?
Conclusion and Recommendations
In closing, further evidence is still required to inform the efficacy and specificity of sedentary behavior recommendations for clinical practice, and for public health policies aiming to reduce the burden of hypertension. Nonetheless, with the ubiquity of sedentary behaviors and the challenges for many in adhering to structured exercise guidelines, it is appropriate to advise: “Move More, Sit Less, More Often” to improve BP control26, 27. Importantly, such advice should continue to be viewed as complementary in the context of other health behaviors, such as the promotion of regular moderate-vigorous physical activity, improving dietary and sleep habits, and minimizing stress. In addition to improving other risk factors associated with inactivity, a “whole-of-day” approach to reducing sitting time and increasing daily incidental movement may prove useful in its own right for improving BP control – particularly in ‘at risk’ populations and for those already managing hypertension. Such a strategy may also be an acceptable “gateway” for those who are physically inactive and highly sedentary, overweight/obese, elderly, deconditioned, and/or unable or reluctant to add/transition directly into structured exercise.
Supplementary Material
Acknowledgement
We thank Andrew Plant (www.andrewplant.com) for contributions to the artwork in Figure 4.
Sources of Funding
PD, NO, DD and BK are supported by National Health and Medical Research Council of Australia (NHMRC) Research Fellowships (#1142685, #1003960, #1078360 & #1059454) and by the Victorian Government’s Operational Infrastructure Support program.
Footnotes
Disclosures
None.
References
- 1.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Wright JT, Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Godlee F. Pills are not the answer to unhealthy lifestyles. BMJ. 2018;362 [Google Scholar]
- 4.Diaz KM, Shimbo D. Physical activity and the prevention of hypertension. Curr Hypertens Rep. 2013;15:659–68. doi: 10.1007/s11906-013-0386-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huai P, Xun H, Reilly KH, Wang Y, Ma W, Xi B. Physical activity and risk of hypertension: a meta-analysis of prospective cohort studies. Hypertension. 2013;62:1021–6. doi: 10.1161/HYPERTENSIONAHA.113.01965. [DOI] [PubMed] [Google Scholar]
- 6.Liu X, Zhang D, Liu Y, et al. Dose-Response Association Between Physical Activity and Incident Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. Hypertension. 2017;69:813–20. doi: 10.1161/HYPERTENSIONAHA.116.08994. [DOI] [PubMed] [Google Scholar]
- 7.2018 Physical Activity Guidelines Advisory Committee Scientific Report. 2018 https://health.gov/paguidelines/second-edition/report.aspx.
- 8.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U, Lancet Physical Activity Series Working G Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–57. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 9.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13:659–80. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN) - Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saida T, Juul Sorensen T, Langberg H. Long-term exercise adherence after public health training in at-risk adults. Ann Phys Rehabil Med. 2017;60:237–43. doi: 10.1016/j.rehab.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Kohl HW, 3rd, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- 13.Heath GW, Parra-Perez D, Sarmiento-Duenas OL, Anderson LB, Owen N, Goenka S, Brownson RC. Evidence-based physical activity intervention: Lessons from around the globe. Lancet. 2012;380:272–81. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hallal PC, Bauman AE, Heath GW, Kohl HW, Lee IM, Pratt M. Physical activity: more of the same is not enough. Lancet. 2012;380:190–1. doi: 10.1016/S0140-6736(12)61027-7. [DOI] [PubMed] [Google Scholar]
- 15.Knuth AG, Hallal PC. Temporal trends in physical activity: a systematic review. J Phys Act Health. 2009;6:548–59. doi: 10.1123/jpah.6.5.548. [DOI] [PubMed] [Google Scholar]
- 16.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167:875–81. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hagstromer M, Troiano RP, Sjostrom M, Berrigan D. Levels and patterns of objectively assessed physical activity--a comparison between Sweden and the United States. Am J Epidemiol. 2010;171:1055–64. doi: 10.1093/aje/kwq069. [DOI] [PubMed] [Google Scholar]
- 18.Dempsey PC, Owen N, Biddle SJ, Dunstan DW. Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Curr Diab Rep. 2014;14:522. doi: 10.1007/s11892-014-0522-0. [DOI] [PubMed] [Google Scholar]
- 19.Healy GN, Winkler EA, Owen N, Anuradha S, Dunstan DW. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur Heart J. 2015;36:2643–9. doi: 10.1093/eurheartj/ehv308. [DOI] [PubMed] [Google Scholar]
- 20.Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, Alter DA. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162:123–32. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 21.Ekelund U, Brown WJ, Steene-Johannessen J, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2018 doi: 10.1136/bjsports-2017-098963. Online First: 10 July. [DOI] [PubMed] [Google Scholar]
- 22.Chastin SF, Egerton T, Leask C, Stamatakis E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity (Silver Spring) 2015;23:1800–10. doi: 10.1002/oby.21180. [DOI] [PubMed] [Google Scholar]
- 23.Bellettiere J, Winkler EAH, Chastin SFM, Kerr J, Owen N, Dunstan DW, Healy GN. Associations of sitting accumulation patterns with cardio-metabolic risk biomarkers in Australian adults. PLoS One. 2017;12:e0180119. doi: 10.1371/journal.pone.0180119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diaz KM, Howard VJ, Hutto B, et al. Patterns of Sedentary Behavior and Mortality in U.S. Middle-Aged and Older Adults: A National Cohort Study. Ann Intern Med. 2017;167:465–75. doi: 10.7326/M17-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dempsey PC, Owen N, Yates TE, Kingwell BA, Dunstan DW. Sitting Less and Moving More: Improved Glycaemic Control for Type 2 Diabetes Prevention and Management. Curr Diab Rep. 2016;16:114. doi: 10.1007/s11892-016-0797-4. [DOI] [PubMed] [Google Scholar]
- 26.Endorsed by The Obesity S. Young DR, Hivert MF, et al. Sedentary Behavior and Cardiovascular Morbidity and Mortality: A Science Advisory From the American Heart Association. Circulation. 2016;134:e262–79. doi: 10.1161/CIR.0000000000000440. [DOI] [PubMed] [Google Scholar]
- 27.Colberg SR, Sigal RJ, Yardley JE, et al. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care. 2016;39:2065–79. doi: 10.2337/dc16-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE. Measurement of adults' sedentary time in population-based studies. Am J Prev Med. 2011;41:216–27. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siu AL. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778–86. doi: 10.7326/M15-2223. [DOI] [PubMed] [Google Scholar]
- 30.Aadahl M, Kjaer M, Jorgensen T. Influence of time spent on TV viewing and vigorous intensity physical activity on cardiovascular biomarkers. The Inter 99 study. Eur J Cardiovasc Prev Rehabil. 2007;14:660–5. doi: 10.1097/HJR.0b013e3280c284c5. [DOI] [PubMed] [Google Scholar]
- 31.Beunza JJ, Martinez-Gonzalez MA, Ebrahim S, Bes-Rastrollo M, Nunez J, Martinez JA, Alonso A. Sedentary behaviors and the risk of incident hypertension: the SUN Cohort. Am J Hypertens. 2007;20:1156–62. doi: 10.1016/j.amjhyper.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Healy GN, Dunstan DW, Salmon J, Shaw JE, Zimmet PZ, Owen N. Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc. 2008;40:639–45. doi: 10.1249/MSS.0b013e3181607421. [DOI] [PubMed] [Google Scholar]
- 33.Jakes RW, Day NE, Khaw KT, et al. Television viewing and low participation in vigorous recreation are independently associated with obesity and markers of cardiovascular disease risk: EPIC-Norfolk population-based study. Eur J Clin Nutr. 2003;57:1089–96. doi: 10.1038/sj.ejcn.1601648. [DOI] [PubMed] [Google Scholar]
- 34.Sidney S, Sternfeld B, Haskell WL, Jacobs DR, Jr, Chesney MA, Hulley SB. Television viewing and cardiovascular risk factors in young adults: the CARDIA study. Ann Epidemiol. 1996;6:154–9. doi: 10.1016/1047-2797(95)00135-2. [DOI] [PubMed] [Google Scholar]
- 35.Lee PH, Wong FK. The association between time spent in sedentary behaviors and blood pressure: a systematic review and meta-analysis. Sports Med. 2015;45:867–80. doi: 10.1007/s40279-015-0322-y. [DOI] [PubMed] [Google Scholar]
- 36.Lee PH, Macfarlane DJ, Lam TH. Factors associated with participant compliance in studies using accelerometers. Gait Posture. 2013;38:912–7. doi: 10.1016/j.gaitpost.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 37.Hamer M, Bruwer EJ, de Ridder JH, Swanepoel M, Kengne AP, Cockeran M, Malan L. The association between seven-day objectively measured habitual physical activity and 24 h ambulatory blood pressure: the SABPA study. J Hum Hypertens. 2017;31:409–14. doi: 10.1038/jhh.2016.93. [DOI] [PubMed] [Google Scholar]
- 38.Hermida RC, Ayala DE, Fernandez JR, Mojon A, Smolensky MH. Hypertension: new perspective on its definition and clinical management by bedtime therapy substantially reduces cardiovascular disease risk. Eur J Clin Invest. 2018;48:e12909. doi: 10.1111/eci.12909. [DOI] [PubMed] [Google Scholar]
- 39.Dempsey PC, Sacre JW, Larsen RN, et al. Interrupting prolonged sitting with brief bouts of light walking or simple resistance activities reduces resting blood pressure and plasma noradrenaline in type 2 diabetes. J Hypertens. 2016;34:2376–82. doi: 10.1097/HJH.0000000000001101. [DOI] [PubMed] [Google Scholar]
- 40.Barone Gibbs B, Kowalsky RJ, Perdomo SJ, Taormina JM, Balzer JR, Jakicic JM. Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J Hypertens. 2017;35:2411–8. doi: 10.1097/HJH.0000000000001463. [DOI] [PubMed] [Google Scholar]
- 41.Bhammar DM, Sawyer BJ, Tucker WJ, Gaesser GA. Breaks in Sitting Time: Effects on Continuously Monitored Glucose and Blood Pressure. Med Sci Sports Exerc. 2017;49:2119–30. doi: 10.1249/MSS.0000000000001315. [DOI] [PubMed] [Google Scholar]
- 42.Champion RB, Smith LR, Smith J, Hirlav B, Maylor BD, White SL, Bailey DP. Reducing prolonged sedentary time using a treadmill desk acutely improves cardiometabolic risk markers in male and female adults. J Sports Sci. 2018;36:2484–91. doi: 10.1080/02640414.2018.1464744. [DOI] [PubMed] [Google Scholar]
- 43.Larsen RN, Kingwell BA, Sethi P, Cerin E, Owen N, Dunstan DW. Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutr Metab Cardiovasc Dis. 2014;24:976–82. doi: 10.1016/j.numecd.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 44.Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Effects of Standing and Light-Intensity Activity on Ambulatory Blood Pressure. Med Sci Sports Exerc. 2016;48:175–81. doi: 10.1249/MSS.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 45.Zeigler ZS, Swan PD, Bhammar DM, Gaesser GA. Walking workstation use reduces ambulatory blood pressure in adults with prehypertension. J Phys Act Health. 2015;12(Suppl 1):S119–27. doi: 10.1123/jpah.2013-0487. [DOI] [PubMed] [Google Scholar]
- 46.Bailey DP, Locke CD. Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J Sci Med Sport. 2015;18:294–8. doi: 10.1016/j.jsams.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 47.Younger AM, Pettitt RW, Sexton PJ, Maass WJ, Pettitt CD. Acute moderate exercise does not attenuate cardiometabolic function associated with a bout of prolonged sitting. J Sports Sci. 2016;34:658–63. doi: 10.1080/02640414.2015.1068435. [DOI] [PubMed] [Google Scholar]
- 48.Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58:950–8. doi: 10.1161/HYPERTENSIONAHA.111.177071. [DOI] [PubMed] [Google Scholar]
- 49.Bennie JA, Pedisic Z, van Uffelen JG, et al. Pumping Iron in Australia: Prevalence, Trends and Sociodemographic Correlates of Muscle Strengthening Activity Participation from a National Sample of 195,926 Adults. PLoS One. 2016;11:e0153225. doi: 10.1371/journal.pone.0153225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Angadi SS, Weltman A, Watson-Winfield D, Weltman J, Frick K, Patrie J, Gaesser GA. Effect of fractionized vs continuous, single-session exercise on blood pressure in adults. J Hum Hypertens. 2010;24:300–2. doi: 10.1038/jhh.2009.110. [DOI] [PubMed] [Google Scholar]
- 51.Bhammar DM, Angadi SS, Gaesser GA. Effects of fractionized and continuous exercise on 24-h ambulatory blood pressure. Med Sci Sports Exerc. 2012;44:2270–6. doi: 10.1249/MSS.0b013e3182663117. [DOI] [PubMed] [Google Scholar]
- 52.Miyashita M, Burns SF, Stensel DJ. Accumulating short bouts of brisk walking reduces postprandial plasma triacylglycerol concentrations and resting blood pressure in healthy young men. Am J Clin Nutr. 2008;88:1225–31. doi: 10.3945/ajcn.2008.26493. [DOI] [PubMed] [Google Scholar]
- 53.Miyashita M, Burns SF, Stensel DJ. Accumulating short bouts of running reduces resting blood pressure in young normotensive/pre-hypertensive men. J Sports Sci. 2011;29:1473–82. doi: 10.1080/02640414.2011.593042. [DOI] [PubMed] [Google Scholar]
- 54.Park S, Rink LD, Wallace JP. Accumulation of physical activity leads to a greater blood pressure reduction than a single continuous session, in prehypertension. J Hypertens. 2006;24:1761–70. doi: 10.1097/01.hjh.0000242400.37967.54. [DOI] [PubMed] [Google Scholar]
- 55.Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA. American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004;36:533–53. doi: 10.1249/01.mss.0000115224.88514.3a. [DOI] [PubMed] [Google Scholar]
- 56.Thompson PD, Crouse SF, Goodpaster B, Kelley D, Moyna N, Pescatello L. The acute versus the chronic response to exercise. Med Sci Sports Exerc. 2001;33:S438–45; discussion S52-3. doi: 10.1097/00005768-200106001-00012. [DOI] [PubMed] [Google Scholar]
- 57.Judice PB, Hamilton MT, Sardinha LB, Zderic TW, Silva AM. What is the metabolic and energy cost of sitting, standing and sit/stand transitions? Eur J Appl Physiol. 2016;116:263–73. doi: 10.1007/s00421-015-3279-5. [DOI] [PubMed] [Google Scholar]
- 58.Mansoubi M, Pearson N, Clemes SA, et al. Energy expenditure during common sitting and standing tasks: examining the 1.5 MET definition of sedentary behaviour. BMC Public Health. 2015;15:516. doi: 10.1186/s12889-015-1851-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Newton RL, Jr, Han H, Zderic T, Hamilton MT. The energy expenditure of sedentary behavior: a whole room calorimeter study. PLoS One. 2013;8:e63171. doi: 10.1371/journal.pone.0063171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Padilla J, Fadel PJ. Prolonged sitting leg vasculopathy: contributing factors and clinical implications. Am J Physiol Heart Circ Physiol. 2017;313:H722–H8. doi: 10.1152/ajpheart.00326.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thosar SS, Bielko SL, Wiggins CC, Wallace JP. Differences in brachial and femoral artery responses to prolonged sitting. Cardiovasc Ultrasound. 2014;12:50. doi: 10.1186/1476-7120-12-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thosar SS, Johnson BD, Johnston JD, Wallace JP. Sitting and endothelial dysfunction: the role of shear stress. Med Sci Monit. 2012;18:RA173–80. doi: 10.12659/MSM.883589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mittermayr M, Fries D, Gruber H, et al. Leg edema formation and venous blood flow velocity during a simulated long-haul flight. Thromb Res. 2007;120:497–504. doi: 10.1016/j.thromres.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 64.Pottier M, Dubreuil A, Monod H. The effects of sitting posture on the volume of the foot. Ergonomics. 1969;12:753–8. doi: 10.1080/00140136908931092. [DOI] [PubMed] [Google Scholar]
- 65.Winkel J, Jorgensen K. Evaluation of foot swelling and lower-limb temperatures in relation to leg activity during long-term seated office work. Ergonomics. 1986;29:313–28. doi: 10.1080/00140138608968267. [DOI] [PubMed] [Google Scholar]
- 66.Redolfi S, Yumino D, Ruttanaumpawan P, Yau B, Su MC, Lam J, Bradley TD. Relationship between overnight rostral fluid shift and Obstructive Sleep Apnea in nonobese men. Am J Respir Crit Care Med. 2009;179:241–6. doi: 10.1164/rccm.200807-1076OC. [DOI] [PubMed] [Google Scholar]
- 67.White LH, Bradley TD, Logan AG. Pathogenesis of obstructive sleep apnoea in hypertensive patients: role of fluid retention and nocturnal rostral fluid shift. J Hum Hypertens. 2015;29:342–50. doi: 10.1038/jhh.2014.94. [DOI] [PubMed] [Google Scholar]
- 68.Singh B, Yadollahi A, Lyons O, Alshaer H, Bradley TD. The effect of sitting and calf activity on leg fluid and snoring. Respir Physiol Neurobiol. 2017;240:1–7. doi: 10.1016/j.resp.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 69.Floras JS, Sinkey CA, Aylward PE, Seals DR, Thoren PN, Mark AL. Postexercise hypotension and sympathoinhibition in borderline hypertensive men. Hypertension. 1989;14:28–35. doi: 10.1161/01.hyp.14.1.28. [DOI] [PubMed] [Google Scholar]
- 70.Morishima T, Restaino RM, Walsh LK, Kanaley JA, Fadel PJ, Padilla J. Prolonged sitting-induced leg endothelial dysfunction is prevented by fidgeting. Am J Physiol Heart Circ Physiol. 2016;311:H177–82. doi: 10.1152/ajpheart.00297.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Restaino RM, Holwerda SW, Credeur DP, Fadel PJ, Padilla J. Impact of prolonged sitting on lower and upper limb micro- and macrovascular dilator function. Exp Physiol. 2015;100:829–38. doi: 10.1113/EP085238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Thosar SS, Bielko SL, Mather KJ, Johnston JD, Wallace JP. Effect of prolonged sitting and breaks in sitting time on endothelial function. Med Sci Sports Exerc. 2015;47:843–9. doi: 10.1249/MSS.0000000000000479. [DOI] [PubMed] [Google Scholar]
- 73.Grace M, Climie RE, Wheeler MJ, et al. Prolonged uninterrupted sitting impairs vascular function and increases biomarkers of atherosclerotic risk in overweight adults (Abstract) American College of Sports Medicine. 2018;49:S111. [Google Scholar]
- 74.Morishima T, Restaino RM, Walsh LK, Kanaley JA, Padilla J. Prior exercise and standing as strategies to circumvent sitting-induced leg endothelial dysfunction. Clin Sci (Lond) 2017;131:1045–53. doi: 10.1042/CS20170031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Restaino RM, Walsh LK, Morishima T, Vranish JR, Martinez-Lemus LA, Fadel PJ, Padilla J. Endothelial dysfunction following prolonged sitting is mediated by a reduction in shear stress. Am J Physiol Heart Circ Physiol. 2016;310:H648–53. doi: 10.1152/ajpheart.00943.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Noddeland H, Winkel J. Effects of leg activity and ambient barometric pressure on foot swelling and lower-limb skin temperature during 8 h of sitting. Eur J Appl Physiol Occup Physiol. 1988;57:409–14. doi: 10.1007/BF00417985. [DOI] [PubMed] [Google Scholar]
- 77.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338 doi: 10.1136/bmj.b1665. b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Keske MA, Dwyer RM, Russell RD, et al. Regulation of microvascular flow and metabolism: An overview. Clin Exp Pharmacol Physiol. 2017;44:143–9. doi: 10.1111/1440-1681.12688. [DOI] [PubMed] [Google Scholar]
- 79.Reynolds LJ, Credeur DP, Manrique C, Padilla J, Fadel PJ, Thyfault JP. Obesity, type 2 diabetes, and impaired insulin-stimulated blood flow: role of skeletal muscle NO synthase and endothelin-1. J Appl Physiol (1985) 2017;122:38–47. doi: 10.1152/japplphysiol.00286.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cardillo C, Campia U, Bryant MB, Panza JA. Increased activity of endogenous endothelin in patients with type II diabetes mellitus. Circulation. 2002;106:1783–7. doi: 10.1161/01.cir.0000032260.01569.64. [DOI] [PubMed] [Google Scholar]
- 81.Muniyappa R, Sowers JR. Role of insulin resistance in endothelial dysfunction. Rev Endocr Metab Disord. 2013;14:5–12. doi: 10.1007/s11154-012-9229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Montagnani M, Golovchenko I, Kim I, et al. Inhibition of phosphatidylinositol 3-kinase enhances mitogenic actions of insulin in endothelial cells. J Biol Chem. 2002;277:1794–9. doi: 10.1074/jbc.M103728200. [DOI] [PubMed] [Google Scholar]
- 83.McManus AM, Ainslie PN, Green DJ, Simair RG, Smith K, Lewis N. Impact of prolonged sitting on vascular function in young girls. Exp Physiol. 2015 doi: 10.1113/EP085355. [DOI] [PubMed] [Google Scholar]
- 84.Germano-Soares AH, Andrade-Lima A, Meneses AL, et al. Association of time spent in physical activities and sedentary behaviors with carotid-femoral pulse wave velocity: A systematic review and meta-analysis. Atherosclerosis. 2018;269:211–8. doi: 10.1016/j.atherosclerosis.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 85.Larsen RN, Kingwell BA, Robinson C, et al. Breaking up of prolonged sitting over three days sustains, but does not enhance, lowering of postprandial plasma glucose and insulin in overweight and obese adults. Clin Sci (Lond) 2015;129:117–27. doi: 10.1042/CS20140790. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.