Abstract
Objectives:
Parental PTSD increases children’s risk for emotional and behavioral problems. We examined parenting stress and parenting behavior quality as mediators of the relation between maternal PTSD and problematic child behaviors in a sample at high risk for trauma exposure. We also examined whether child sex moderated this association.
Method:
Participants were 141 African-American mother-child dyads (children aged 8–12). Mothers reported PTSD severity, parenting stress, and child behavior (externalizing, internalizing and emotional self-control). Parenting behavior quality (accounting for factors including parental warmth and engagement) was assessed from an observational parent-child interaction task.
Results:
Parenting stress, but not observed parenting behavior quality, mediated the relation between maternal PTSD severity and child behaviors. Child sex moderated this association, such that the effect was stronger for girls.
Conclusions:
Maternal PTSD may be associated with negative child behavior outcomes, and this relation appears to be mediated by increased parenting stress. Stress reducing interventions for parents with PTSD could improve child outcomes, especially for girls.
Keywords: PTSD, trauma, parenting stress, parent-child interaction, moderated mediation
Introduction
Recent research has elucidated the adverse effects of non-combat, civilian trauma—such as community violence, intimate partner violence, and natural disasters—on trauma survivors and their offspring (Gillespie et al., 2009; Jain, Davey-Rothwell, Crossnohere, & Latkin, 2018; Lang & Gartstein, 2017). This is especially relevant in low-income, urban, minority communities, where an estimated 90% of women experience at least one traumatic event during their lifetime, per DSM-IV criteria (Gillespie et al., 2009). Posttraumatic stress disorder (PTSD) is one potential psychopathological consequence of trauma exposure. PTSD is characterized by core symptoms of intrusion (e.g., flashbacks and nightmares), avoidance, negative changes in cognition and mood, and altered physiologic arousal (American Psychiatric Association, 2013). Approximately 10–20% of women exposed to trauma develop PTSD, with elevated rates—up to 46%—among low-income, minority, urban populations (Gillespie et al., 2009; Jain et al., 2018; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Many of these women are mothers, and research suggests that their trauma exposure can have negative consequences for their children, even if their children are not exposed to trauma themselves (Lang & Gartstein, 2017; Yehuda et al., 2014; Yehuda et al., 2005).
Multiple studies have found that children of parents with PTSD are at higher risk for developing depression, anxiety, behavioral problems, and PTSD (Lambert, Holzer, & Hasbun, 2014; Leen-Feldner, Feldner, Bunaciu, & Blumenthal, 2011; van Ee, Kleber, & Jongmans, 2016). Across 22 studies that assessed associations between parental PTSD and child outcomes, parental PTSD symptom severity was consistently associated with more child internalizing behaviors, such as depression and anxiety, and externalizing behaviors, such as aggression and impulsivity (van Ee et al., 2016). Similarly, a meta-analysis of 42 studies found that higher levels of parental PTSD symptoms were associated with more negative child psychological outcomes, including distress, anxiety, behavior problems, and PTSD (Lambert et al., 2014). There is also evidence that parental PTSD adversely impacts children’s emotion regulation capacity, such that children display decreased distress tolerance and increased emotional reactivity (Bosquet Enlow et al., 2011; Pat-Horenczyk et al., 2015; Samuelson & Cashman, 2008). The association between parental PTSD and adverse child behavioral outcomes has been observed in infants and young children (<5 years; Bosquet Enlow et al., 2011; Pat-Horenczyk et al., 2015), as well as in older children and adolescents (Samuelson & Cashman, 2008; Self-Brown et al., 2012).
Although a substantial body of evidence suggests a link between parental PTSD and adverse child outcomes, the relevant mechanisms of transmission are an area of active investigation. These mechanisms are likely multifactorial and could include genetic, neuroendocrine, and behavioral/environmental/socio-cultural pathways. One behavioral pathway by which parental PTSD could impact child outcomes is via direct effects of parental PTSD on parenting behaviors, such as sensitivity, protectiveness, and aggression. Studies have investigated this possibility using both parent report and observer ratings of parenting behaviors (Lambert et al., 2014; van Ee et al., 2016). Investigations that utilized parent report consistently point to significant negative associations between parental PTSD and parenting behavior quality (van Ee et al., 2016). For instance, mothers with PTSD endorse higher levels of psychological aggression toward their children (Chemtob, Gudino, & Laraque, 2013), and report using more physical aggression with their children compared to mothers without PTSD (Leen-Feldner et al., 2011). Additionally, increased maternal PTSD symptoms have been associated with higher self-reported child abuse potential (Cross et al., 2018). In contrast, several researchers have collected ratings of parenting behavior quality from independent observers and have found that parental PTSD is not associated with lower-quality parenting behavior, as measured in a laboratory setting (Koren-Karie, Oppenheim, & Getzler-Yosef, 2008; Muzik et al., 2017; Samuelson, Wilson, Padron, Lee, & Gavron, 2017). In particular, Samuelson and colleagues (2017) found that observed parenting behavior quality did not mediate the relations between maternal PTSD severity and child emotion regulation, internalizing, and externalizing behaviors in a sample of 52 dyads of mothers and their school-aged children. Possible explanations for these mixed results include differences in the sample characteristics, including child age, and the possibility that parents with PTSD might perceive and rate their own parenting behavior more harshly than parents without PTSD.
Parental PTSD has been proposed to have indirect effects on child outcomes through parenting stress. Samuelson and colleagues (2017) found that parenting stress mediated the relations between maternal PTSD severity and child behavior problems in 7–12 year old’s. Parenting stress is conceptualized as the parent’s negative feelings and stress that result from her or his assessment of both a) her or himself as a parent and b) how difficult s/he perceives the child to be (Abidin, 1990; Samuelson et al., 2017). Parenting stress may be influenced by sociocultural factors, such as race and ethnicity. Although there are limited studies that compare different ethnic or racial groups, some studies have reported on parenting stress within minority groups. For example, a study of African-American mothers from a low socioeconomic status (SES) population reported a positive correlation between neighborhood disturbance and parenting stress, and negative correlations between religiosity and parenting stress (Lamis et al., 2014). Parenting stress and trauma exposure may also adversely impact parental warmth, an important aspect of sensitive caregiving that can have broad effects on child and adolescent well-being (Davidov & Grusec, 2006; Lowe & Dotterer, 2013; Cross et al., 2016). Studies of school-age African-American children found that greater parental warmth is associated with better outcomes assessed in 12-year-old children, including less anxious/internalizing behavior (McCabe, Clark, & Barnett, 1999), higher self-esteem, and better academic outcomes (Lowe & Dotterer, 2013). Mothers with PTSD report more parenting stress than those without PTSD (Chemtob et al., 2013). This finding may be related to a parent’s need to manage her own PTSD symptoms and her role as a parent.
Additional factors, including child sex and child trauma exposure, may also impact the relationship between parental PTSD and child outcomes (van Ee et al., 2016; Zahn-Waxler, Shirtcliff, & Marceau, 2008). Prior studies report that boys often show more externalizing behaviors than girls, even in the absence of trauma (Zahn-Waxler et al., 2008), while girls may respond to stressors with greater physiologic arousal than boys (Stevens, van Rooij, & Jovanovic, 2016). One study found that adult sons of parents with PTSD are more likely to display symptoms of PTSD than adult daughters of parents with PTSD (Zerach & Solomon, 2018). One potential source of sex differences is that the frontal cortex, which modulates emotion regulation and behavioral control, develops more slowly in school-age boys than girls (Zahn-Waxler et al., 2008). In addition, school-age girls tend to engage in play that is more relational and family-oriented, while boys tend to engage in more aggressive play, which may aggravate their parents’ PTSD symptoms (Zahn-Waxler et al., 2008). Child trauma exposure is another relevant factor, as children’s own exposure to trauma has been shown to impact their cognitive development and mental health (Enlow, Blood, & Egeland, 2013). These prior studies suggest that child sex and trauma exposure warrant further investigation regarding their role in the association between parental PTSD and children’s well-being.
The present study sought to replicate and extend the findings of Samuelson and colleagues (2017) in a larger sample of 141 dyads of mothers and children age 8–12 years old by: (1) examining associations between maternal PTSD severity and increased child externalizing, internalizing, and emotional self-control behaviors in an independent and larger sample of low-income, urban, minority mother-child dyads; (2) evaluating whether the impact of maternal PTSD on each of these child behaviors was mediated by parenting stress or observed parenting behavior quality (see Figure 1 for conceptual model); (3) ascertaining the moderating role of child sex; and (4) determining whether the associations remained significant when controlling for child trauma exposure. We hypothesized that, as Samuelson and colleagues (2017) found, (1) maternal PTSD severity would be associated with increased child externalizing, internalizing, and emotional self-control behaviors and (2) maternal parenting stress, but not observed parenting behavior quality, would mediate the impact of maternal PTSD on each of these child behaviors. We further hypothesized that (3) child sex would moderate the relation between maternal parenting stress and children’s emotional and behavioral functioning, with a greater effect in boys, as reported by Zerach and Solomon (2018) (see Figure 2 for conceptual model), and lastly (4) this moderated mediation would not change when child trauma exposure was added to the model as a covariate, as Samuelson and colleagues (2017) found that parental PTSD affected child outcomes even when controlling for the child’s own trauma exposure (see Figure 3 for conceptual model). To our knowledge, this is the first moderated mediation study of parental PTSD, parenting stress, and child behavior outcomes that tests for sex differences in these associations.
Figure 1. Mediation Model of Total Parenting Stress as a Mediator Between Maternal PTSD Symptoms and Child Behavioral Outcomes.
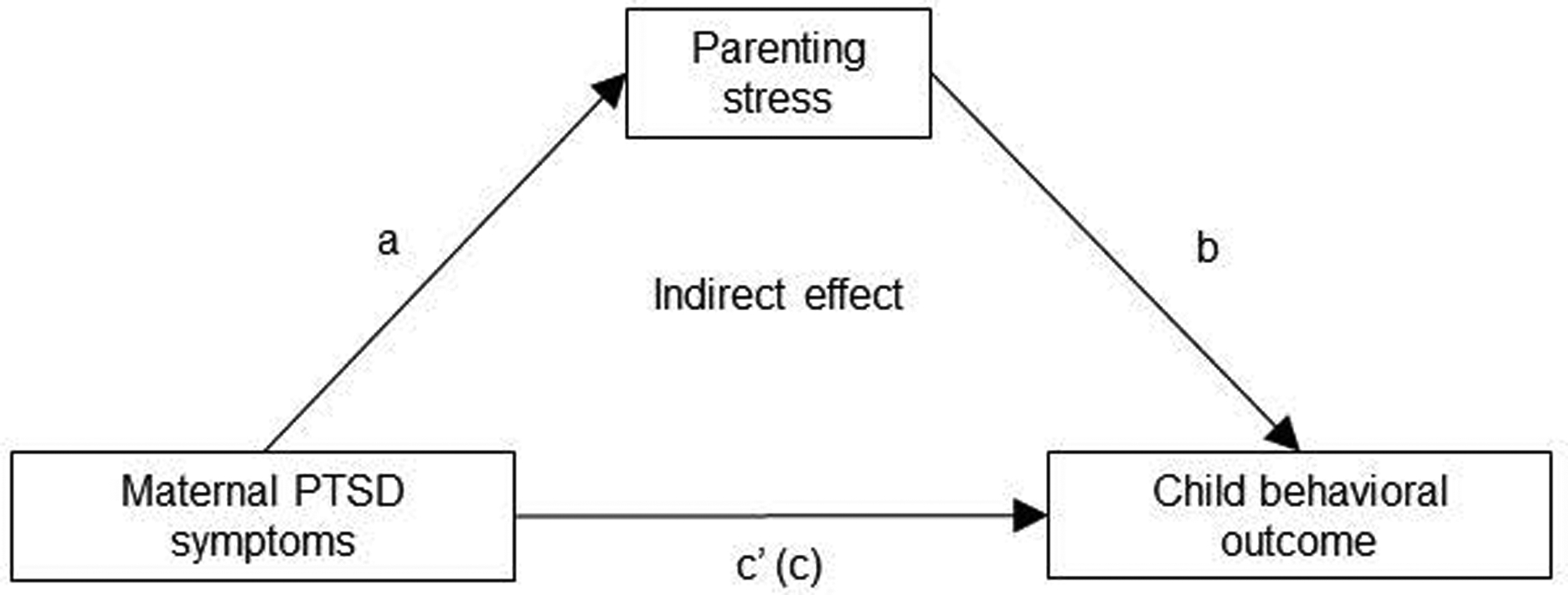
Note. Path c’ is the direct effect. Path c is the total effect. Analyses were conducted separately for each of the child behavioral outcomes: externalizing behavior, internalizing behavior and emotional self-control. Results are shown in Table 3.
Figure 2. Moderated Mediation Model of Parenting Stress as a Mediator Between Maternal PTSD and Child Behavior Outcomes, with Child Sex as a Moderator.
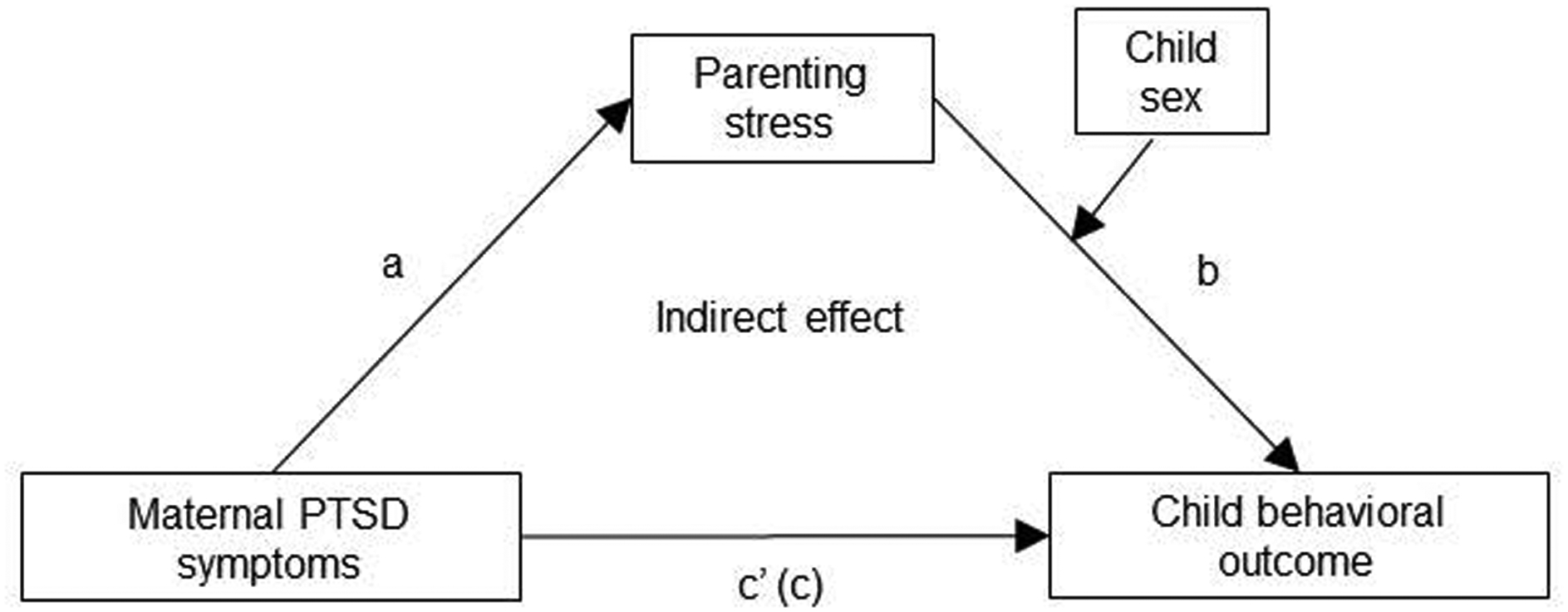
Note. Path c’ is the direct effect. Path c is the total effect. Analyses were conducted separately for each of the child behavioral outcomes: externalizing behavior, internalizing behavior and emotional self-control. Results are shown in Table 4a.
Figure 3. Moderated Mediation Model of Parenting Stress as a Mediator Between Maternal PTSD and Child Behavior Outcomes, with Child Sex as a Moderator, While Controlling for Child Trauma Exposure.
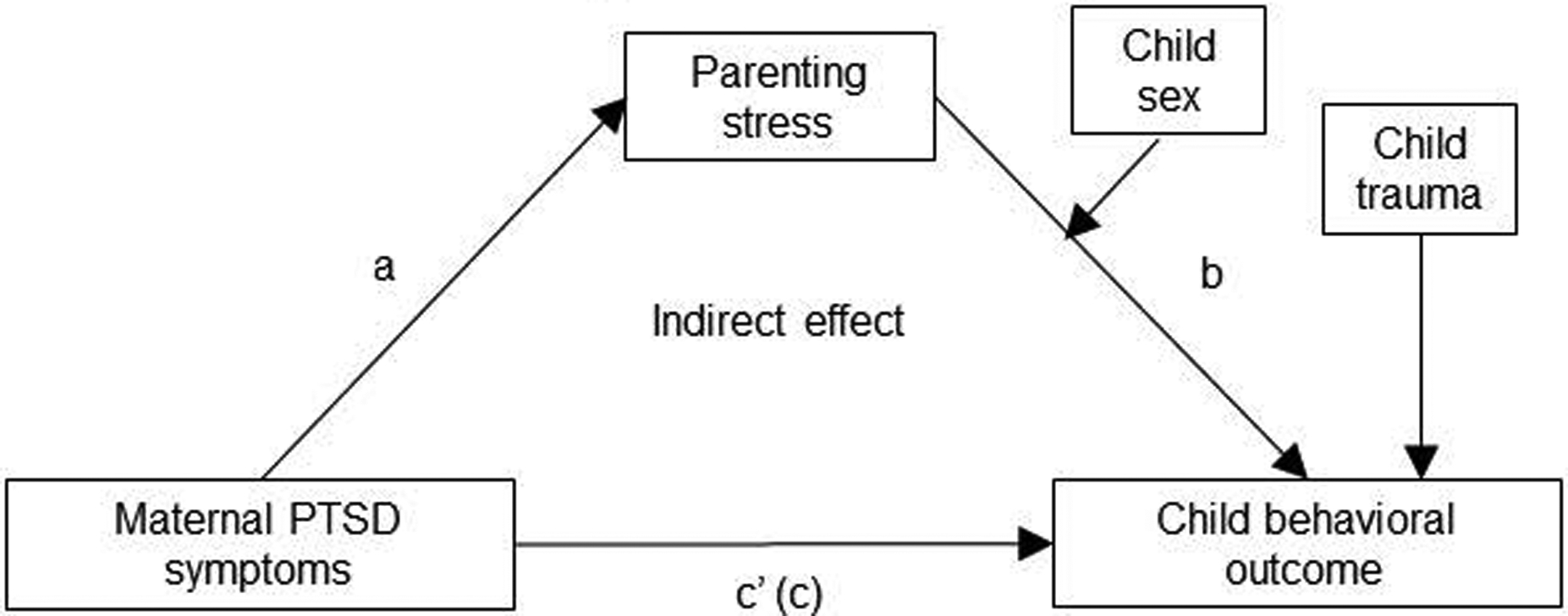
Note. Path c’ is the direct effect. Path c is the total effect. Analyses were conducted separately for each of the child behavioral outcomes: externalizing behavior, internalizing behavior and emotional self-control. Results are shown in Table 4b.
Methods
Participants
Participants were recruited from the waiting rooms of a large urban tertiary care center, in Atlanta, GA, which serves a low-income population with high trauma exposure (Jovanovic et al., 2011). The study included 141 African-American mother-child dyads; all mothers were their child’s legal guardian and primary caretaker. Exclusion criteria for mothers and children included intellectual disability, active psychosis, or autism, per parent report. The mothers were 21–58 years old (M = 34.1) and the children (46.8% female) were 8–12 years old (M = 9.6). The children’s age range matched that of the children in Samuelson and colleagues (2017). Dyads were primarily from single-parent households: 84.6% of the parents reported being single, divorced, widowed, or separated and 32.6% of the children had no contact with their father in the past year. Only 15.4% of the mothers/female caregivers reported being married (9.8%) or having a domestic partner (5.6%). The sample self-identified as African-American and low-income, with 79.9% of the mothers reporting a household monthly income < $2,000. Over 95% of the mothers reported one or more types of traumatic events in their lifetime. All procedures in this study were reviewed and approved by Emory University’s Institutional Review Board. Prior to participation, mothers provided informed consent and parental permission for their children to participate. Children provided verbal assent.
Materials
Maternal PTSD symptom severity was assessed through the modified PTSD Symptom Scale (PSS; Foa & Tolin, 2000), a psychometrically valid 17-item self-report measure of current symptoms of PTSD, with scores ranging from 0 to 47. The PSS has been validated with the widely used measure of PTSD – the Clinician Administered PTSD Scale (CAPS; Foa & Tolin, 2000). The PSS begins with an inventory of traumatic experiences and participants are instructed not to continue if they have not experienced any traumatic event. The categorical presence of PTSD was determined based on DSM-IV A-E criterion responses to the PSS questionnaire (A, presence of trauma; B, presence of at least 1 intrusive symptom; C, presence of at least 3 avoidance / numbing symptoms; and D, presence of at least 2 hyperarousal symptoms; and E, present for at least 1 month). We summed the PSS frequency items to obtain a continuous measure of PTSD symptom severity. Parenting stress was measured through the Parenting Stress Index, Third Edition, Short Form (PSI; Abidin, 1995), a 36-item parent self-report measure of parenting stress with subscales for Parental Distress, Parent-Child Dysfunctional Interactions, and Difficult Child. The total parenting stress score is the sum of these subscales.
Children’s emotional self-control, internalizing, and externalizing behaviors were assessed using the Parent Rating Scales from the Behavioral Assessment System for Children, Second Edition (BASC-2; Reynolds & Kamphaus, 2004). Scores between 60 and 69 are considered at-risk and scores above 70 are considered clinically significant. The BASC-2 yields composite scores on two child psychopathology dimensions, externalizing and internalizing, and includes an emotional self-control scale. Child trauma exposure was assessed with the Traumatic Events Screening Inventory-Parent Report Revised (TESI-PRR), a 24-item parent-report measure of child exposure to potentially traumatic events, with the result ranging from 0–24 based on the number of trauma exposure types (Ghosh-Ippen et al., 2002).
Parenting behavior quality was measured through the Etch-A-Sketch Task, an observational interaction task that requires the parent and child to work cooperatively to succeed (Ginsburg, Grover, & Ialongo, 2005). The parent and child are given an Etch-A-Sketch board and instructed to copy a series of three designs of increasing complexity. Raters code their overall impression of the quality of the parent-child interaction on a 4-point scale, with higher numbers representing higher quality interactions. This rating is based on positive affect, negative affect, warmth, and degree of cooperation and reciprocity. These parenting dimensions are associated with the development of child anxiety (Ginsberg et al., 2005). All sessions were videotaped and later scored by trained, blinded coders. Training of each coder took approximately 20 hours and involved reviewing written and videotaped material and demonstrating ability to reliably score gold-standard videotaped sessions. To ensure inter-rater reliability, all interactions were taped and scored by two coders. Scores were considered reliable if they were within one point of each other. If the scores were not within one point of each other, coders re-watched and then discussed the tape, and either agreed on a consensus rating or contacted a senior coder to make the final determination (Ginsburg et al., 2005). Inter-rater reliability was assessed with Shrout & Fleiss Two-Way Random Models (Shrout & Fleiss, 1979); all coefficients were ≥ .72 (range = .72, .95), indicating good to excellent reliability.
Data Analytic Plan
All analyses were conducted with SPSS version 24. The significance of all statistical tests was evaluated at the α= .05 level. Independent t-tests assessed differences between the group variables by child sex. BASC-2 data were analyzed using age-normed t-scores. To determine if the variables of interest were associated, we tested for correlations between maternal PTSD, parenting behavior, parenting stress, child trauma, and child behavior (externalizing, internalizing, and emotional self-control). Mediation analyses were only conducted for maternal variables that were significantly associated with child behavior outcomes, as mediation is only appropriate when both the primary and mediator variables are significantly correlated with the outcome variable. These analyses were conducted using Hayes’ PROCESS macro, version 2.16.3 (Preacher & Hayes, 2004; Preacher & Hayes, 2008). Tests of mediation examined direction and significance of indirect effects in Hayes’ PROCESS macro using Model 4. We employed bootstrapping to determine the direction and significance of indirect mediation effects in smaller samples. This method uses 10,000 bootstrap samples to generate 95% confidence intervals (CI) around the effects, which are significant if the CI does not include 0.
To test whether mediation effects were dependent on the level of a moderator (child sex), the moderated mediation model shown in Figure 2 was used. Tests of moderated mediation were conducted in Hayes’ PROCESS macro using Model 14. All tests were conducted for each of the three child behavioral outcome variables. A significant moderated mediation effect was established when the 95% bias-corrected bootstrap CI of the index of moderated mediation did not contain 0. To test whether the moderated mediation effect remained significant when controlling for child trauma, the model in Figure 3 was used.
Results
Descriptive statistics for child and maternal measures are reported in Table 1. Results from the BASC-2 indicated that for externalizing symptoms 19.6% (n=28) of children were in the at-risk category and 11.9% (n=17) qualified as clinically significant. For internalizing symptoms 18.1% (n=25) were at-risk and 8.3% (n=13) were clinically significant. For emotional self-control, 16.7% (n=23) were at-risk and 9.7% (n=15) were clinically significant. Mothers exhibited PTSD symptoms; mean score on the PSS was 15.4 (SD = 13.5), and 36.2% met criteria for current PTSD. Maternal PTSD symptom severity, parenting stress, and child behavior (externalizing, internalizing, and emotional self-control) were not significantly different by child sex. Bivariate correlations indicated that maternal PTSD was positively correlated with higher parenting stress, child trauma exposure, externalizing behavior, internalizing behavior, and child emotional self-control (see Table 2; all ps < .01). Furthermore, parenting stress was positively correlated with all three child behavior variables and child trauma exposure (all ps < .01). Child trauma exposure was positively correlated with internalizing and externalizing behaviors (p < .01 and p < .05, respectively). Parenting behavior quality on the Etch-A-Sketch observational task was not significantly correlated with maternal PTSD or with any of the child behavior measures. Therefore, no further analyses using parenting behavior quality were conducted.
Table 1.
Descriptive Statistics for All Child and Maternal Measures (N = 141).
| Boys (n = 75) | Girls (n = 66) | |||
|---|---|---|---|---|
| Child variables | M | SD | M | SD |
| Age (years) | 9.8 | 1.5 | 9.4 | 1.4 |
| Externalizing | 55.2 | 11.3 | 58.0 | 13.4 |
| Internalizing | 53.0 | 11.6 | 53.3 | 11.7 |
| Emotional self-control | 52.1 | 10.5 | 54.1 | 12.1 |
| Trauma * | 67 | 3.3 | 5.8 | 2.9 |
| Maternal variables | ||||
| Age (years) | 34.7 | 7.5 | 33.5 | 7.8 |
| Maternal PTSD | 16.8 | 14.5 | 13.9 | 12.2 |
| Parenting stress + | 88.2 | 18.8 | 86.1 | 17.5 |
| Parenting behavior quality | 2.5 | 0.8 | 2.4 | 0.8 |
Note. Externalizing = Behavior Assessment System for Children-Second Edition (BASC-2) externalizing score; Internalizing = BASC-2 internalizing total score; Emotional self-control = BASC-2 emotional self-control score; Child Trauma = Traumatic Events Screening Inventory, Parent-report, total number of events; PTSD = posttraumatic stress disorder; Maternal PTSD = PSS total Score; Parenting Stress = PSI total score; Parenting Behavior Quality = Quality of interaction composite score on Etch-A Sketch task.
n = 130.
n = 138.
Table 2.
Correlations for All Variables.
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Maternal PTSD | - | .28** | .22** | .22* | .37** | .44** | −.01 |
| 2. Parenting stress | - | .59** | .55** | .43** | .29** | −.00 | |
| 3. Child emotional self-control | - | .75** | .45** | .12 | .04 | ||
| 4. Child externalizing | - | .46** | .23* | −.12 | |||
| 5. Child internalizing | - | .47** | .01 | ||||
| 6. Child trauma | - | .06 | |||||
| 7. Parenting behavior quality | - |
Note. Statistical significance indicated as
p < .05 or
p < .01.
Maternal PTSD = PSS total score; Parenting stress = PSI total score; Child emotional self-control = Behavior Assessment System for Children-Second Edition (BASC-2) emotional self-control content scale score; Child externalizing = BASC-2 externalizing total score; Child internalizing = BASC-2 internalizing total score; Child trauma = Traumatic Events Screening Inventory for Children total score; Parenting behavior quality = Quality of interaction composite score on Etch-A Sketch task.
The mediation and moderated mediation analyses were conducted separately for the three child behavioral outcomes: externalizing behavior, internalizing behavior and emotional self-control. Parenting stress fully mediated the association between maternal PTSD and child externalizing behavior (Figure 1; Table 3). The indirect effect of parenting stress was significant, B = 0.14, 95% CI [.05, .24], whereas the direct effect of maternal PTSD was not significant after accounting for parenting stress. In the second model, child sex significantly moderated the indirect effect of parenting stress on externalizing behavior, B = −22.54, p = .01. This effect was larger for girls, B = 0.20, 95% CI [.08, .35], than for boys, B = 0.09, 95% CI [.03, .17] (Figure 2; Table 4a). These effects remained significant after controlling for child trauma exposure (Figure 3; Table 4b).
Table 3.
Path Coefficients for Simple Mediation Relations by Parental Stress in the Relationship Between Maternal PTSD Symptoms and Child Behavioral Outcomes.
| Child Behavior | a | b | c | c’ | Indirect effect |
|---|---|---|---|---|---|
| Externalizing | 0.38* | 0.36* | 0.18* | 0.05 | 0.14* |
| Internalizing | 0.38* | 0.23* | 0.31* | 0.22* | 0.09* |
| Emotional Self Control | 0.38* | 0.35* | 0.18* | 0.04 | 0.13* |
Note. Table corresponds to Figure 1. Results are reported as unstandardized coefficients. Significance of indirect effects is based on 95% confidence intervals rather than p–values. Statistically significant effects indicated with *.
Table 4.
Path Coefficients for Moderated Mediation Relations with Parenting Stress as a Mediator and Child Sex as a Moderator of the Relationship Between Maternal PTSD Symptoms and Child Behavioral Outcomes (Table 4a) and with Child Trauma Included as a Covariate (Table 4b).
| Child Behavior | a | b (boys) | b (girls) | c’ | Indirect effect (boys) | Indirect effect (girls) | Main effect of sex | Covariate: Child trauma |
|---|---|---|---|---|---|---|---|---|
| a. | ||||||||
| Externalizing | 0.38* | 0.24* | 0.53* | 0.06 | 0.09* | 0.20* | −22.54* | — |
| Internalizing | 0.38* | 0.19* | 0.27* | 0.23* | 0.07* | 0.10* | −5.21 | — |
| Emotional self-control | 0.38* | 0.27* | 0.46* | 0.06 | 0.10* | 0.18* | −13.54+ | — |
| b. | ||||||||
| Externalizing | 0.29* | 0.22* | 0.54* | 0.03 | 0.06* | 0.15* | −25.49* | 0.27 |
| Internalizing | 0.29* | 0.15* | 0.27* | 0.13+ | 0.04+ | 0.08* | −9.59 | 1.19* |
| Emotional self-control | 0.29* | 0.28* | 0.48* | 0.08 | 0.08* | 0.14* | −14.82* | −0.33 |
Parenting stress partially mediated the association between maternal PTSD and child internalizing behavior (Figure 1; Table 3). The indirect effect of parenting stress was significant, B = 0.09, 95% CI [.03, .17], and the direct effect of maternal PTSD remained significant, B = .23, 95% CI [.09, .36], after accounting for parenting stress. In the second model, child sex did not moderate this indirect effect, B = −5.21, p = .55 (Figure 2; Table 4a). When child trauma was included as a covariate in the model it was significantly associated with increased internalizing behaviors, B = 1.19, 95% CI [.56, 1.81], but did not change the overall pattern of results: both the direct effect of maternal PTSD and the indirect effect of parenting stress remained significant (Figure 3; Table 4b).
Parenting stress fully mediated the association between maternal PTSD and child emotional self-control behavior (Figure 1; Table 3). The indirect effect of parenting stress was significant, B = .13, 95% CI [.05, .22], whereas the direct effect of maternal PTSD was not significant after accounting for parenting stress. In the second model, the indirect effect of parenting stress on externalizing behavior was marginally moderated by child sex, B = −13.54, p = .08. This indirect effect was larger for girls, B = .18, 95% CI [.07, .30], than for boys, B = .10, 95% CI [.04, .18] (Figure 2; Table 4a). This pattern of effects remained after controlling for child trauma exposure (Figure 3; Table 4b).
Discussion
In this study we examined associations between maternal PTSD and child behavior outcomes in one of the largest samples of mother-child dyads that included an observational measure of parenting behavior quality to date. We report that parenting stress, but not observed parenting behavior, mediated the association between maternal PTSD and children’s externalizing, internalizing, and emotional self-control behavior, thereby replicating the finding of Samuelson and colleagues (2017) in a larger sample of low-income, urban, African-American women and their school-aged children ages 8–12 years old. Moreover, we demonstrate the importance of child sex in moderating this relationship, such that parenting stress had a larger effect on girls’ externalizing and emotional self-control behavior. These findings were not influenced by child trauma exposure. These results provide novel information about factors influencing the intergenerational transmission of trauma within predominantly single-parent African-American families.
The positive association between maternal PTSD and parenting stress was hypothesized given that PTSD symptoms include numbness, hypervigilance, negative cognitions and mood, which could interfere with common parenting tasks like being receptive to the needs of a child and tolerating a child’s distress. Our finding is consistent with several prior studies that report parental PTSD impacts children via increasing parenting stress (Cao, Powers, Cross, Bradley, & Jovanovic, 2017; Chemtob et al., 2013; Samuelson et al., 2017). Notably, two studies found no association between parental PTSD and parenting stress (Lang, Gartstein, Rodgers, & Lebeck, 2010; Salloum, Stover, Swaidan, & Storch, 2015). The discrepancy between our findings and those of Lang and colleagues (2010) likely reflects differences in the samples: majority Caucasian versus African-American participants, infants versus school-aged (8–12 year old) children, and higher SES and lower trauma exposure relative to our sample. Mothers with infants may have different parenting stressors than mothers of school-age children (for example, stressors related to the need to soothe and feed a baby), and these groups may not be readily comparable. Interestingly, Salloum and colleagues (2015) tested parents of children in a similar age range and of comparable SES; however, their sample was 79% Caucasian and their measure of parental PTSD was dichotomous (yes/no) whereas we used a continuous measure of PTSD symptoms, which may capture the association with parenting stress levels more accurately.
As hypothesized, there was no significant association between maternal PTSD and observed parenting behavior quality. This finding is consistent with both Samuelson and colleagues (2017) and Koren-Karie and colleagues (2008), who also found no association between parental PTSD and parenting behavior in parents of school-aged children. In contrast, most studies that report significant relations between maternal PTSD and observed parenting behavior quality have examined mothers of infants or preschool-age children (Levendosky, Huth-Bocks, Shapiro, & Semel, 2003; Lieberman, Van Horn, & Ozer, 2005; Schechter et al., 2010). Younger children may require more parental involvement and control than older children, which could account for these disparate findings (Waite & Creswell, 2015). The divergent pattern of results for younger versus older children suggests that maternal PTSD could impact parenting behavior more or less during different developmental windows, which may be an important target for future investigation. It is also possible that the parenting behavior task, which has been validated in dyads with parents who reported anxiety disorders, was less effective at capturing a range of the parenting behaviors of interest (warmth, cooperation, positive and negative affect) within this population (Ginsburg et al., 2005). Our finding that parenting stress appeared to impact child outcomes despite no difference in observed parenting behaviors supports the idea that parenting stress is separate from observed behavior, and includes the internal experience of parenting, as well as the ability of a parent to experience joy from their child and to tolerate their child’s distress (Abidin, 1995; Mackler et al., 2015).
Our finding that child sex moderated the mediating role of parenting stress in the relationship between maternal PTSD and child externalizing behavior and emotional self-control is novel. Although there was no overall difference in levels of parenting stress or externalizing behavior between girls and boys, higher parenting stress was related to more externalizing behavior in girls. This was unexpected given that female sex is typically associated with lower levels of externalizing behavior (Zahn-Waxler et al., 2008) and fewer parenting difficulties (Willinger, Diendorfer-Radner, Willnauer, Jorgl, & Hager, 2005). One potential explanation is that girls may be more affected than boys by their mothers’ PTSD symptoms and stress, perhaps due to increased identification with their mothers, or increased maternal identification with their daughters. Cross and colleagues (2016) found that mothers with a history of childhood sexual abuse displayed decreased warmth towards their school-age daughters, but not sons. They suggested that mothers may demonstrate more emotional numbing and distance from a child who reminds them of themselves (i.e. of the same sex and age range) when they experienced their abuse. An alternative explanation is that externalizing behavior and emotional self-control difficulties are less common in school-age female children, and are thus considered more problematic when they occur (Zahn-Waxler et al., 2008). Our findings suggest that it is important to consider sex differences when treating traumatized mothers and their children.
This study aligns with findings that parental PTSD symptoms are associated with more negative child outcomes and adds information about behavioral mechanisms that may contribute to this relation. These findings should be viewed in the context of other established mechanisms of transmission of traumatic stress. More than 20 candidate genes, the majority of which are involved in the fear response pathway, have been identified as being involved in the heritability of PTSD (Ryan, Chaudieu, Ancelin, & Saffery, 2016). Alterations in hypothalamic pituitary adrenal axis functioning have been seen in both infants of trauma-exposed mothers (Danielson, Hankin, & Badanes, 2015; Yehuda et al., 2005) and adult offspring of parents with PTSD (Yehuda et al., 2014). Increased sympathetic nervous system activation has been seen in the school-aged children of trauma-exposed mothers (Jovanovic et al., 2011). Given these findings, it is possible that the offspring of parents with PTSD may have a shared genetic liability that contributes to behavioral problems, independent of behavioral pathways. Future studies should investigate potential interactions between genetic, neuroendocrine, behavioral, and environmental pathways in the intergenerational transmission of trauma.
The present study had several limitations. First, this is a cross-sectional study, and thus it cannot address change across time, directionality, or causality. There is evidence that use of a transactional model would better take into account the reciprocal relationship between parental factors and child behavior; Mackler and colleagues (2015) found that a longitudinal transactional model was a more appropriate fit to assess parenting stress and child externalizing behavior, when compared to a direct effects model (Samuelson et al., 2017; van Ee et al., 2015). Future studies should move towards utilizing transactional models to better incorporate the bi-directional influence of child behavior on parental factors.
A second limitation was our reliance on parental report of child behaviors rather than direct observation or child self-report, which might have produced different results. However, our use of parent report is consistent with widely used methods in this field, and is appropriate given that school-aged children’s self-report of behavior problems may be less reliable (Grills & Ollendick, 2003). We considered the possibility that mothers with PTSD viewed and rated their children’s behavior more harshly than parents without PTSD, which could confound our results; however, this was assessed in a meta-analysis of 41 studies on PTSD and parenting and that association was not found (Lambert et al., 2014). Future research in this area could be strengthened by the addition of another report of child behavior, such as by a teacher, or another caregiver. A third limitation was our measurement of parenting behavior, which was completed during a 15 minute task, did not capture a full range of parenting behaviors, and utilized a macro-rather than micro-level coding procedure. A fourth limitation was that we measured PTSD according to DSM-IV criteria rather than the current DSM-5 definition; the DSM-5 had not been published at the time that this study was developed. Finally, due to characteristics of this sample and our study design, we were not able to directly address the impact that fathers might have on these mother-child dynamics. Research into the link between PTSD and parenting stress has been conducted almost exclusively with mothers and children, and it is not clear that our findings would generalize to father-child dyads. Future research would benefit from the inclusion of high-quality observational measures of parent and child behavior, assessment of PTSD using DSM-5 criteria, and incorporation of information about the family context beyond the mother-child dyad, particularly in regards to the presence of fathers or other caregivers.
In spite of these limitations, our results enrich the account of how maternal PTSD impacts children. Importantly, we examined associations between maternal PTSD and important child behavioral outcomes in a sample of African-American mother-child dyads within one of the largest observational studies to date. There is limited empirical research on this population, which is impacted by multiple risk factors: low SES, discrimination, and high levels of trauma exposure. We found that parenting stress mediates the association between maternal PTSD and children’s externalizing, internalizing, and emotional self-control behavior problems. Therefore, our study adds to the limited literature on parenting stress in African-American dyads; although other studies have found factors that increase parenting stress in low SES AA women (Lamis et al., 2014), these did not examine child outcomes or compare different racial groups. Although not focused on PTSD and trauma, a recent study of caregivers of children with autism compared resilience and parenting stress between African-American, Hispanic, and white families found that parenting stress was highest in the African-Americans emphasizing potential for increased risk (Kim, Dababnah, & Lee, 2019).
We also extended findings from prior studies by reporting that child sex moderates these relationships, such that the effect was larger in girls. In addition, we report that observed parenting behavior is not significantly associated with parental PTSD symptom severity or child behavior. Together, these findings indicate that maternal PTSD primarily impacts child behavior by increasing parenting stress, and that this might affect girls more than boys. These results add to our understanding of behavioral mechanisms of intergenerational transmission of trauma within a population that is impacted by high levels of trauma exposure and socio-economic adversity, and may therefore experience unusually high levels of parenting stress. Our findings highlight the need for interventions designed to ameliorate parenting stress within this population in order to improve outcomes for children.
Clinical Impact Statement.
Parental PTSD increases children’s risk for emotional and behavioral problems. We examined behavioral factors that may drive this association, specifically, maternal stress and parenting quality. We studied 141 low-income African-American mother-child dyads; most had high trauma exposure and were in single-parent households. We found that parenting stress, but not observed parenting behavior quality, contributed to the association between maternal PTSD severity and child behaviors, and this effect was stronger for girls.
Acknowledgments
This research was supported by grants from the National Institute of Health, MH100122, MH111682, and HD071982.
References
- Abidin R (1990). Introduction to the special issue: The stresses of parenting. Journal of Clinical Child Psychology, 19(4), 298–301. doi: 10.1207/s15374424jccp1904_1 [DOI] [Google Scholar]
- Abidin R (1995). Parenting stress index, third edition: professional manual. Odessa, FL: Psychological Assessment Resources, Inc. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC [Google Scholar]
- Bosquet Enlow M, Kitts RL, Blood E, Bizarro A, Hofmeister M, & Wright RJ (2011). Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behavior and Development, 34(4), 487–503. doi: 10.1016/j.infbeh.2011.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao M, Powers A, Cross D, Bradley B, & Jovanovic T (2017). Maternal emotion dysregulation, parenting stress, and child physiological anxiety during dark-enhanced startle. Developmental Psychobiology, 59(8), 1021–1030. doi: 10.1002/dev.21574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemtob CM, Gudino OG, & Laraque D (2013). Maternal posttraumatic stress disorder and depression in pediatric primary care: association with child maltreatment and frequency of child exposure to traumatic events. JAMA Pediatrics, 167(11), 1011–1018. doi: 10.1001/jamapediatrics.2013.2218 [DOI] [PubMed] [Google Scholar]
- Cross D, Kim YJ, Vance LA, Robinson G, Jovanovic T, & Bradley B (2016). Maternal child sexual abuse is associated with lower maternal warmth toward daughters but not sons. Journal of Child Sex Abuse, 25(8), 813–826. doi: 10.1080/10538712.2016.1234532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross D, Vance LA, Kim YJ, Ruchard AL, Fox N, Jovanovic T, & Bradley B (2018). Trauma exposure, PTSD, and parenting in a community sample of low-income, predominantly African American mothers and children. Psychological Trauma: Theory, Research, Practice, and Policy, 10(3), 327–335. doi: 10.1037/tra0000264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson CK, Hankin BL, & Badanes LS (2015). Youth offspring of mothers with posttraumatic stress disorder have altered stress reactivity in response to a laboratory stressor. Psychoneuroendocrinology, 53, 170–178. doi: 10.1016/j.psyneuen.2015.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidov M, & Grusec JE (2006). Untangling the links of parental responsiveness to distress and warmth to child outcomes. Child Development, 77(1), 44–58. doi: 10.1111/j.1467-8624.2006.00855.x [DOI] [PubMed] [Google Scholar]
- Enlow MB, Blood E, & Egeland B (2013). Sociodemographic risk, developmental competence, and PTSD symptoms in young children exposed to interpersonal trauma in early life. Journal of Traumatic Stress, 26(6), 686–694. doi: 10.1002/jts.21866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, & Tolin DF (2000). Comparison of the PTSD Symptom Scale-Interview Version and the Clinician-Administered PTSD scale. Journal of Traumatic Stress, 13(2), 181–191. doi: 10.1023/A:1007781909213 [DOI] [PubMed] [Google Scholar]
- Ghosh Ippen C, Ford J, Racusin R, Acker M, Bosquet K, Rogers C, Edwards J Trauma Events Screening Inventory-Parent Report Revised. San Francisco: The Child Trauma Research Project of the Early Trauma Network and The National Center for PTSD Dartmouth Child Trauma Research Group; 2002. [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, … Ressler KJ (2009). Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry, 31(6), 505–514. doi: 10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg G, Grover R, & Ialongo N (2005). Parenting Behaviors Among Anxious and Non-Anxious Mothers: Relation with Concurrent and Long-Term Child Outcomes. Child & Family Behavior Therapy, 26(4). doi: 10.1300/j019v26n04_02 [DOI] [Google Scholar]
- Grills AE, & Ollendick TH (2003). Multiple informant agreement and the anxiety disorders interview schedule for parents and children. Journal of the American Academy of Child and Adolescent Psychiatry, 42(1), 30–40. doi: 10.1097/00004583-200301000-00008 [DOI] [PubMed] [Google Scholar]
- Jain KM, Davey-Rothwell M, Crossnohere NL, & Latkin CA (2018). Post-Traumatic Stress Disorder, Neighborhood Residency and Satisfaction, and Social Network Characteristics among Underserved Women in Baltimore, Maryland. Women’s Health Issues, 28(3), 273–280. doi: 10.1016/j.whi.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovanovic T, Smith A, Kamkwalala A, Poole J, Samples T, Norrholm SD, … Bradley B (2011). Physiological markers of anxiety are increased in children of abused mothers. Journal of Child Psychology and Psychiatry, 52(8), 844–852. doi: 10.1111/j.1469-7610.2011.02410.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives Of General Psychiatry, 52(12), 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kim I, Dababnah S, & Lee J (2019). The Influence of Race and Ethnicity on the Relationship between Family Resilience and Parenting Stress in Caregivers of Children with Autism. Journal Autism Dev Disord. Epub. doi: 10.1007/s10803-019-04269-6. [DOI] [PubMed] [Google Scholar]
- Koren-Karie N, Oppenheim D, & Getzler-Yosef R (2008). Shaping children’s internal working models through mother-child dialogues: the importance of resolving past maternal trauma. Attachment & Human Development, 10(4), 465–483. doi: 10.1080/14616730802461482 [DOI] [PubMed] [Google Scholar]
- Lambert JE, Holzer J, & Hasbun A (2014). Association between parents’ PTSD severity and children’s psychological distress: a meta-analysis. Journal of Traumatic Stress, 27(1), 9–17. doi: 10.1002/jts.21891 [DOI] [PubMed] [Google Scholar]
- Lamis DA, Wilson CK, Tarantino N, Lansford JE, & Kaslow NJ (2014). Neighborhood disorder, spiritual well-being, and parenting stress in African American women. Journal of Family Psychology, 28(6):769–78. doi: 10.1037/a0036373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ, & Gartstein MA (2017). Intergenerational transmission of traumatization: Theoretical framework and implications for prevention. Journal of Trauma & Dissociation, 1–14. doi: 10.1080/15299732.2017.1329773 [DOI] [PubMed] [Google Scholar]
- Lang AJ, Gartstein MA, Rodgers CS, & Lebeck MM (2010). The impact of maternal childhood abuse on parenting and infant temperament. Journal of Child and Adolescent Psychiatric Nursing, 23(2), 100–110. doi: 10.1111/j.1744-6171.2010.00229.x [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Bunaciu L, & Blumenthal H (2011). Associations between parental posttraumatic stress disorder and both offspring internalizing problems and parental aggression within the National Comorbidity Survey-Replication. Journal of Anxiety Disorders, 25(2), 169–175. doi: 10.1016/j.janxdis.2010.08.017 [DOI] [PubMed] [Google Scholar]
- Levendosky AA, Huth-Bocks AC, Shapiro DL, & Semel MA (2003). The impact of domestic violence on the maternal-child relationship and preschool-age children’s functioning. J Family Psychology, 17(3), 275–287. doi: 10.1037/0893-3200.17.3.275 [DOI] [PubMed] [Google Scholar]
- Lieberman AF, Van Horn P, & Ozer EJ (2005). Preschooler witnesses of marital violence: predictors and mediators of child behavior problems. Development and Psychopathology, 17(2), 385–396. doi: 10.1017/s0954579405050182 [DOI] [PubMed] [Google Scholar]
- Loew K, & Dotterer A (2013). Parental Monitoring, Parental Warmth, and Minority Youths’ Academic Outcomes: Exploring the Integrative Model of Parenting. Journal of Youth and Adolescence, 42(9), 1413–1425. doi: 10.1007/s10964-013-9934-4 [DOI] [PubMed] [Google Scholar]
- Mackler JS, Kelleher RT, Shanahan L, Calkins SD, Keane SP, & O’Brien M (2015). Parenting Stress, Parental Reactions, and Externalizing Behavior From Ages 4 to 10. Journal of Marriage and Family, 77(2), 388–406. doi: 10.1111/jomf.12163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe KM, & Clark R (1999). Family protectivefactors among urban African American youth. Journal of Clinical ChildPsychology, 28(2), 137–150. doi: 10.1207/s15374424jccp2802_2 [DOI] [PubMed] [Google Scholar]
- Muzik M, Morelen D, Hruschak J, Rosenblum KL, Bocknek E, & Beeghly M (2017). Psychopathology and parenting: An examination of perceived and observed parenting in mothers with depression and PTSD. Journal of Affective Disorders, 207, 242–250. doi: 10.1016/j.jad.2016.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pat-Horenczyk R, Cohen S, Ziv Y, Achituv M, Asulin-Peretz L, Blanchard TR, … Brom D (2015). Emotion regulation in mothers and young children faced with trauma. Infant Mental Health Journal, 36(3), 337–348. doi: 10.1002/imhj.21515 [DOI] [PubMed] [Google Scholar]
- Preacher K, & Hayes A (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Beh Res Methods, Instruments, and Computers, 36, 717–731. [DOI] [PubMed] [Google Scholar]
- Preacher K, & Hayes A (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, Instruments, and Computers, 40, 879–891. doi: 10.3758/brm.40.3.879 [DOI] [PubMed] [Google Scholar]
- Reynolds CR, & Kamphaus RW (2004). Behavior Assessment System for Children-Second Edition (BASC-2). Circle Pines, MN: American Guidance Service, Inc; 2004. [Google Scholar]
- Ryan J, Chaudieu I, Ancelin ML, & Saffery R (2016). Biological underpinnings of trauma and post-traumatic stress disorder: focusing on genetics and epigenetics. Epigenomics, 8(11), 1553–1569. doi: 10.2217/epi-2016-0083 [DOI] [PubMed] [Google Scholar]
- Salloum A, Stover C, Swaidan V, & Storch E (2015). Parent and child PTSD and parent depression in relation to parenting stress among trauma-exposed children. Journal of Child and Family Studies, 24(5), 1203–1212. doi: 10.1007/s10826-014-9928-1 [DOI] [Google Scholar]
- Samuelson KW, & Cashman C (2008). Effects of Intimate Partner Violence and Maternal Posttraumatic Stress Symptoms on Children’s Emotional and Behavioral Functioning. Journal of Emotional Abuse, 8(1–2), 139–153. doi: 10.1080/10926790801986007 [DOI] [Google Scholar]
- Samuelson KW, Wilson CK, Padron E, Lee S, & Gavron L (2017). Maternal PTSD and Children’s Adjustment: Parenting Stress and Emotional Availability as Proposed Mediators. Journal of Clinical Psychology, 73(6), 693–706. doi: 10.1002/jclp.22369 [DOI] [PubMed] [Google Scholar]
- Schechter DS, Willheim E, Hinojosa C, Scholfield-Kleinman K, Turner JB, McCaw J, … Myers MM (2010). Subjective and objective measures of parent-child relationship dysfunction, child separation distress, and joint attention. Psychiatry, 73(2), 130–144. doi: 10.1521/psyc.2010.73.2.130 [DOI] [PubMed] [Google Scholar]
- Self-Brown S, LeBlanc MM, David K, Shepard D, Ryan K, Hodges A, & Kelley ML (2012). The impact of parental trauma exposure on community violence exposed adolescents. Violence and Victims, 27(4), 512–526. doi: 10.1891/0886-6708.27.4.512 [DOI] [PubMed] [Google Scholar]
- Shrout PE, & Fleiss JL (1979). Intraclass correlations: uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428. doi: 10.1037//0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- Stevens JS, van Rooij SJ, & Jovanovic T (2016). Developmental Contributors to Trauma Response: The Importance of Sensitive Periods, Early Environment, and Sex Differences. Current Topics in Behavioral Neurosciences. doi: 10.1007/7854_2016_38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ee E, Kleber RJ, & Jongmans MJ (2016). Relational Patterns Between Caregivers With PTSD and Their Nonexposed Children: A Review. Trauma, Violence, & Abuse, 17(2), 186–203. doi: 10.1177/1524838015584355 [DOI] [PubMed] [Google Scholar]
- Waite P, & Creswell C (2015). Observing Interactions between Children and Adolescents and their Parents: The Effects of Anxiety Disorder and Age. Journal of Abnormal Child Psychology, 43(6), 1079–1091. doi: 10.1007/s10802-015-0005-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willinger U, Diendorfer-Radner G, Willnauer R, Jorgl G, & Hager V (2005). Parenting stress and parental bonding. Journal of Behavioral Medicine, 31(2), 63–69. doi: 10.3200/BMED.31.2.63-72 [DOI] [PubMed] [Google Scholar]
- Yehuda R, Daskalakis NP, Lehrner A, Desarnaud F, Bader HN, Makotkine I, … Meaney MJ (2014). Influences of maternal and paternal PTSD on epigenetic regulation of the glucocorticoid receptor gene in Holocaust survivor offspring. American Journal of Psychiatry, 171(8), 872–880. doi: 10.1176/appi.ajp.2014.13121571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R, Engel SM, Brand SR, Seckl J, Marcus SM, & Berkowitz GS (2005). Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. The Journal of Clinical Endocrinology & Metabolism, 90(7), 4115–4118. doi: 10.1210/jc.2005-0550 [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Shirtcliff EA, & Marceau K (2008). Disorders of childhood and adolescence: gender and psychopathology. Annual Review of Clinical Psychology, 4, 275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358 [DOI] [PubMed] [Google Scholar]
- Zerach G, & Solomon Z (2018). Gender differences in posttraumatic stress symptoms among former prisoners of wars’ adult offspring. Anxiety, Stress, & Coping, 31(1), 21–31. doi: 10.1080/10615806.2017.1368835 [DOI] [PubMed] [Google Scholar]


