Abstract
Background
The first case of COVID-19 detected in Mexico was on the 27th of February 2020. On the 30th of April, 64 days after this first diagnosis, the number of patients had increased exponentially, reaching 19,224 confirmed cases and 1859 (9.67%) deaths. In response to this global outbreak, we summarize the current state of our understanding regarding COVID-19 in Mexico.
Methods
We obtained the data from the official website of the Ministry of Health in Mexico. The study period covered the 27th of February to the 30th of April 2020. The cases were confirmed using real-time reverse transcription-polymerase chain reaction assays, and we analyzed the epidemiological, demographic and clinical data.
Results
In Mexico, most cases of COVID-19 were located in Mexico City. The mean age of the patients was 46 years. Of the 12,656 confirmed cases, most infected individuals were between the ages of 30 and 59 years (65.85%), and there was a higher incidence rate for men (58.18%) than for women (41.82%). The patients who died had one or more comorbidities, mainly hypertension (45.53%), diabetes (39.39%) and obesity (30.4%). In the first 64 days of the epidemic, China had reported 80,304 cases, with a mortality rate of 3.66%.
Conclusions
Our results indicate the early transmission of COVID-19 in Mexico. The descriptive epidemiology shows similarities between the cases of COVID-19 in Mexico and those in China. In the same period of the epidemic curve, we observed a reduction in the number of confirmed cases of COVID-19 in Mexico and a higher mortality rate compared with that of China.
Keywords: Coronavirus, COVID-19, SARS-CoV-2, Mexico, Quarantine, Infection
Abstract
Antecedentes
El primer caso de COVID-19 se detectó en México el 27 de febrero de 2020. El 30 de abril, 64 días después de este primer diagnóstico, el número de pacientes aumentó exponencialmente, alcanzando un total de 19.224 casos confirmados y 1.859 (9,67%) fallecidos. En respuesta a este brote global, resumimos el estado actual del conocimiento sobre COVID-19 en México.
Métodos
Los datos se obtuvieron del sitio web oficial del Ministerio de Salud en México. El período analizado fue entre el 27 de febrero y el 30 de abril de 2020. Los casos se confirmaron mediante RT-PCR en tiempo real y se analizaron los datos epidemiológicos, demográficos y clínicos.
Resultados
La mayoría de los casos de COVID-19 se ubicaron en la Ciudad de México. La edad promedio de los pacientes fue de 46 años. De los 12.656 casos confirmados, el mayor número de infectados ocurre en el rango de edad entre 30 y 59 años (65,85%), y hubo una mayor incidencia en hombres (58,18%) que en mujeres (41,82%). Los pacientes fallecidos tenían una o múltiples comorbilidades, principalmente hipertensión (45,53%), diabetes (39,39%) y obesidad (30,4%). En los primeros 64 días de epidemia, China había reportado 80.304 casos con una tasa de mortalidad del 3,66%.
Conclusiones
Nuestros resultados indican la transmisión temprana de COVID-19 en México. La epidemiología descriptiva muestra las similitudes entre los casos de COVID-19 de México y China. En el mismo período de la curva epidémica, observamos en México una reducción en el número de casos confirmados de COVID-19 y una mayor tasa de mortalidad en comparación con China.
Palabras clave: Coronavirus, COVID-19, SARS-CoV-2, México, Cuarentena, Infección
Background
On the 31st of December 2019, China had a total of 26 cases and 1 death with a diagnosis of pneumonia of unknown etiology.1 These cases originated in the Huanan Seafood Wholesale Market of Wuhan.2 On the 7th of January 2020, the Chinese Center for Disease Control and Prevention identified the causal agent of the unknown pneumonia as a severe acute coronavirus related to severe acute respiratory syndrome (SARS), which was termed SARS-CoV-2, due to its similarity with SARS coronavirus (CoV), discovered in 2003.
This type of virus causes disease in animals and humans, which can be respiratory infections, such as the common cold, or more acute infections, such as Middle East respiratory syndrome (MERS)-CoV and SARS-CoV.3 Generally, the viruses can be found in animal reservoirs: MERS-CoV is transmitted from camels to humans, whereas SARS-CoV is transmitted from exotic animals. Bats are suspected to be the reservoir for SARS-CoV-2, although this has not been completely verified.[4], [5], [6], [7] The World Health Organization (WHO) named this disease coronavirus disease 2019 (COVID-19).[8], [9] On the 11th of March, 2020, COVID-19 was declared a pandemic.[10], [11]
It has been reported that COVID-19 can be transmitted from person to person through direct contact with an infected individual or when an individual coughs or sneezes, creating tiny droplets that remain suspended in the air travelling up to approximately 1.8 m. Virus transmission has also been detected through contact with contaminated surfaces or fomites.[12], [13], [14]
The most common symptoms of COVID-19 infection are sore throat, fatigue, dry cough, myalgia and fever. Some patients also experience headache, vomiting, hemoptysis, diarrhea, dyspnea, sputum production and lymphopenia.[15], [16] These symptoms can appear within 5.2 days, the mean incubation time for the coronavirus.17
Most patients have recovered spontaneously, and some presented nonsevere pneumonia. Individuals with fatal complications can develop pulmonary edema, organ failure, severe pneumonia, septic shock and acute respiratory distress syndrome. Deaths resulting from coronavirus occur after a mean delay of 14 days after contracting the infection (range, 6–41 days).18
The number of infections caused by COVID-19 continues to grow quickly. As of the 30th of April 2020, COVID-19 has infected 3,090,445 people worldwide and has caused the deaths of 217,769, only 4 months after the first diagnosed case. At this point in the pandemic, governments are attempting to prevent the spread of infection among the population by restricting mobility.
To confront this worldwide health problem, we need transparency and the exchange of information between nations to evaluate the characteristics of this new disease.[19], [20] In response to this worldwide outbreak, we summarize the current state of knowledge on COVID-19 in Mexico up to April 2020. This information is valuable for understanding the expansion of the disease and the effect of containment measures in Mexico.
Materials and methods
Data source
Data on the confirmed cases and deaths due to COVID-19 infection in Mexico were obtained from the official website of the Mexican Ministry of Health through the Directorate General of Epidemiology. These data are analyzed by the The Institute for Diagnosis and Epidemiological References (Instituto de Diagnóstico y Referencia Epidemiológica).
The study period covered the 27th of February to the 30th of April 2020. Our data include the notification dates for all confirmed cases, suspected cases and deaths, the symptom onset date, whether the case was local transmission, of imported origin or contact with the imported case, and the mortality rate distribution by sex and age (Table 1 ).
Table 1.
Total number of confirmed and suspected cases and deaths as of the 30th of April 2020, as well as the distribution of cases and the mortality rate by sex and age.
| [0,1–9]Results of COVID-19 tests | ||||||||
|---|---|---|---|---|---|---|---|---|
| [0,1–2]Tests performed = 87,372 |
[0,3–5]Confirmed cases = 19,224 |
[0,6–7]Negative cases = 52,628 |
[0,8–9]Suspected cases 15,520 |
|||||
| [0,1–5]Confirmed cases = 19,224 |
[0,6–9]Deaths = 1,859 |
|||||||
| Age group, years | Cases n = 19,244 | %Total cases | Men n = 11,186 | Women n = 8,038 | Deaths n = 1,859 | Deaths % Age group | Men n = 1,280 | Women n = 579 |
| 0–4 | 94 | 0.49 | 57 | 37 | 4 | 4.26 | 2 | 2 |
| 5–9 | 61 | 0.32 | 29 | 32 | 0 | 0.00 | 0 | 0 |
| 10–14 | 95 | 0.49 | 49 | 46 | 0 | 0.00 | 0 | 0 |
| 15–19 | 175 | 0.91 | 95 | 80 | 0 | 0.00 | 0 | 0 |
| 20–24 | 627 | 3.26 | 352 | 275 | 6 | 0.96 | 2 | 4 |
| 25–29 | 1558 | 8.10 | 840 | 718 | 23 | 1.48 | 14 | 9 |
| 30–34 | 1972 | 10.26 | 1076 | 896 | 36 | 1.83 | 34 | 2 |
| 35–39 | 2191 | 11.40 | 1259 | 932 | 75 | 3.42 | 52 | 23 |
| 40–44 | 2238 | 11.64 | 1280 | 958 | 130 | 5.81 | 99 | 31 |
| 45–49 | 2333 | 12.14 | 1376 | 957 | 210 | 9.00 | 159 | 51 |
| 50–54 | 2127 | 11.06 | 1306 | 821 | 225 | 10.58 | 168 | 57 |
| 55–59 | 1795 | 9.34 | 1055 | 740 | 242 | 13.48 | 163 | 79 |
| 60–64 | 1333 | 6.93 | 804 | 529 | 217 | 16.28 | 145 | 72 |
| 65–69 | 1071 | 5.57 | 654 | 417 | 255 | 23.81 | 168 | 87 |
| 70–74 | 658 | 3.42 | 437 | 221 | 166 | 25.23 | 117 | 49 |
| 75–79 | 466 | 2.42 | 274 | 192 | 130 | 27.90 | 76 | 54 |
| 80–84 | 249 | 1.30 | 139 | 110 | 83 | 33.33 | 44 | 39 |
| 85–89 | 121 | 0.63 | 67 | 54 | 38 | 31.40 | 23 | 15 |
| 90–94 | 44 | 0.23 | 27 | 17 | 13 | 29.55 | 10 | 3 |
| 95–99 | 12 | 0.06 | 6 | 6 | 5 | 41.67 | 3 | 2 |
| 100–104 | 4 | 0.02 | 4 | 0 | 1 | 25.00 | 1 | 0 |
Definitions
A confirmed case is defined as a positive result for the COVID-19 laboratory test, which consists of the real-time reverse transcription-polymerase chain reaction assay. A suspected case is defined as a case that meets 2 of the following criteria: fever, radiographic evidence of pneumonia, low or normal white blood cell count or low lymphocyte count. An asymptomatic case is defined as a patient with confirmed COVID-19 with normal body temperature or minor discomfort.
The cases confirmed in the first FHS reports, up to the 7th of April 2020, were divided into 3 types: imported cases, imported contact and transmission and local infection. An imported case is an individual who has traveled to an affected area outside the country in the 14 days prior to the disease onset. Imported contact is an individual infected by direct contact with an imported case. Local infection is an individual with no history of infection due to importation. The index case, or patient zero, is an individual who is positive for COVID-19 with the earliest onset date in a specific setting.21
Temporary milestones and control measures
The first case (or index case) of COVID-19 in Mexico was detected on the 27th of February 2020 in Mexico City: a Mexican who had traveled to Italy and had mild symptoms. On the 28th of February, 2 more cases were confirmed: a 35-year-old Italian resident of Mexico City and a Mexican citizen from the state of Hidalgo who was in the state of Sinaloa. The 2 individuals had recently traveled to Italy. Phase 1 of COVID-19 in Mexico began that day. In this phase, the cases of infection were imported from abroad, and there were no cases of local infection. The number of people infected with the virus was small, and there were no strict health measures, except for efforts directed at disseminating preventive actions.
The fourth case was confirmed on the 29th of February 2020: a youth in the state of Coahuila who had recently traveled to Milan (Italy). On the 1st of March, a youth who studied in Italy was confirmed with COVID-19 in Tuxtla Gutiérrez, Chiapas, thereby reaching 5 cases. On the 6th of March, the sixth case was confirmed in the state of Mexico: a 71-year-old man who had traveled to Italy. The seventh case, confirmed on the 7th of March, was a 46-year-old man from Mexico City. On the 11th of March, the same day the WHO classified COVID-19 as a pandemic, 4 new cases were reported: 2 in Mexico City, 1 in Querétaro and 1 in the state of Mexico. The patients from Mexico City and Queretaro had returned from a trip to Spain, and their ages ranged from 30 to 41 years. The case from the state of Mexico was a 64-year-old woman who had recently traveled to the United States. Up to that date, 11 cases had been reported in Mexico.
On the 14th of March 2020, the Ministry of Public Education moved up the Holy Week vacations and extended them to a month, from the 23rd of March to the 20th of April for all educational institutions throughout the country.
On the 18th of March, 118 confirmed cases of COVID-19 were reported, a 26% increase compared with the previous day’s result (93 cases). That same day, the Secretary of Health confirmed the first death by COVID-19 in Mexico.
The federal government decreed the 24th of March as the start of phase 2 of the COVID-19 pandemic in Mexico, after recording the first local infections. In this phase, certain activities, mainly financial, were suspended, massive congregations were restricted, and the general population was advised to remain at home, especially those older than 60 years and those with diagnosed arterial hypertension, diabetes, heart or lung disease and induced or acquired immunosuppression, as well as pregnant and immediate postpartum women.
Starting the 26th of March, nonessential activities of the federal government were suspended, except those related to the departments of safety, health, energy and sanitation. The recommendations include sneezing etiquette, constant washing of hands and continuous disinfection of public-use areas. Individuals who have symptoms and have been confirmed with COVID-19 have to use face masks to avoid infecting other people. Medical care personnel should wear the necessary personal protection equipment to avoid infection when identifying patients at risk and when inside medical facilities.7
On the 30th of March, the government issued a national health emergency in Mexico, given the progression of confirmed cases and deaths by the disease. This resulted in the establishment of additional measures for its prevention and control, such as the immediate suspension of nonessential activities in all financial sectors of the country for 1 month, up to the 30th of April.[22], [23]
On the 21st of April 2020, phase 3 of COVID-19 was assumed to have begun in Mexico, given that there was already evidence of active outbreaks and propagation in the country, with more than a thousand cases. During this phase, the nonessential activities of the public, private and social sector were suspended, and the National Healthy Distance Day was extended to the 30th of May.24
Results
Since the first case on the 27th of February 2020, to the 30th of April 2020, COVID-19 has spread throughout Mexico. To date, 87,372 diagnostic tests have been conducted throughout the country. Of these, 19,224 have resulted positive, and another 15,520 diagnostic tests from suspected cases are still being analyzed. The total number of deaths during the study period was 1859.
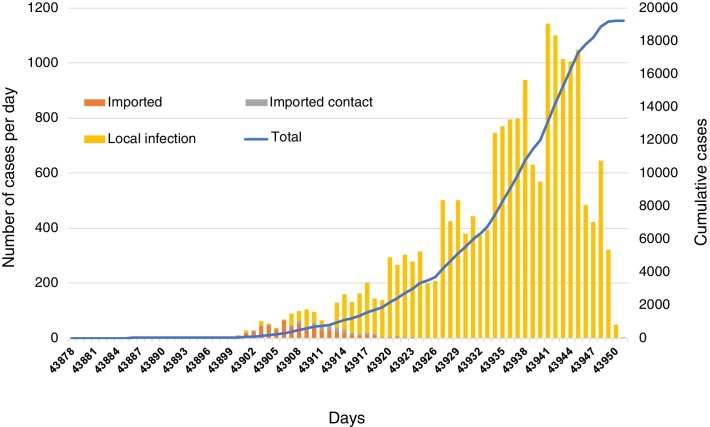
The analysis of the demographic characteristics of the 19,224 confirmed patients in Mexico showed that 746 (3.88%) patients were imported cases from Italy, Germany, Spain, United States, France, Great Britain, Turkey, Peru, Switzerland, Netherlands, Czech Republic, Colombia, China, Canada, Brazil, Argentina and Singapore. In total, there were 135 (0.70%) recorded cases of infection by direct contact with individuals reported as imported cases, and 18,343 (95.42%) cases had no history of contact with individuals who have traveled abroad and can therefore be defined as community or local infection (Fig. 1 ).
Figure 1.
Distribution of symptom onset for patients with confirmed COVID-19 through laboratory testing: imported cases (orange), imported contact cases (grey), local contact cases (yellow). The line in the figure shows the cumulative cases of COVID-19 between the 17th of February and the 30th of April 2020.
After the 13th of March, the number of local confirmed cases began to exceed the number of imported cases. Mexico also began to detect infections among healthcare personnel dedicated to treating people diagnosed with COVID-19 and in their treatment locations. It is clear that COVID-19 is an infection with a high degree of person-to-person propagation. Coupled with this, there are mild cases that are not reported due to presenting symptoms of a common cold or common infection. These individuals received no medical care and were not diagnosed.
Moreover, we have individuals with asymptomatic infection who act as unidentified transmitters of the infection. To date, the proportion of mild cases of COVID-19 and of asymptomatic infections is unknown, thereby hiding the virus’ true epidemic potential at this time. To quantify the actual reach of the virus, we would need to perform the largest number of tests possible.
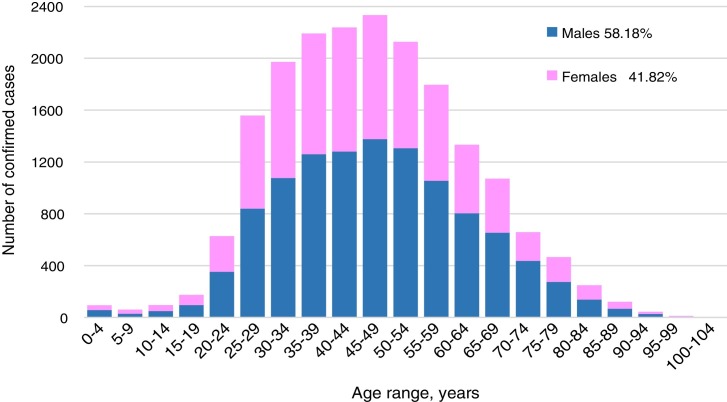
Fig. 2 shows the distribution of COVID-19 cases between men and women. Blue indicates the 11,186 (58.18%) confirmed cases in men, and pink indicates the 8038 (41.82%) cases confirmed in women. The patients’ mean age was 46 years, with a range of 0–104 years.
Figure 2.
Distribution by age and sex of patients with laboratory-confirmed COVID-19 infection.
The lowest number of infections were in individuals younger than 14 years, given that they presented only 250 (1.3%) cases. Among the 15–29-year age group, 2360 (12.27%) cases were recorded. The largest number of infections occurred in the 30–59-year age group, with 12,656 (65.85%) cases, whereas the age range of 60–104 years had fewer cases (3958 cases; 20.58%).
Of the 19,224 patients reported to date, 11,637 (60.53%) were outpatients, which means that they were mild cases who did not require hospitalization and continued with the necessary care and isolation at home. A total of 7587 (39.47%) patients required hospitalization due to presenting severe signs. By the 30th of April, 1859 of these 7587 hospitalized patients had died and 5728 remained hospitalized. Of the hospitalized patients, 1785 were stable, 3068 had more severe symptoms and 875 were intubated with mechanical ventilation.
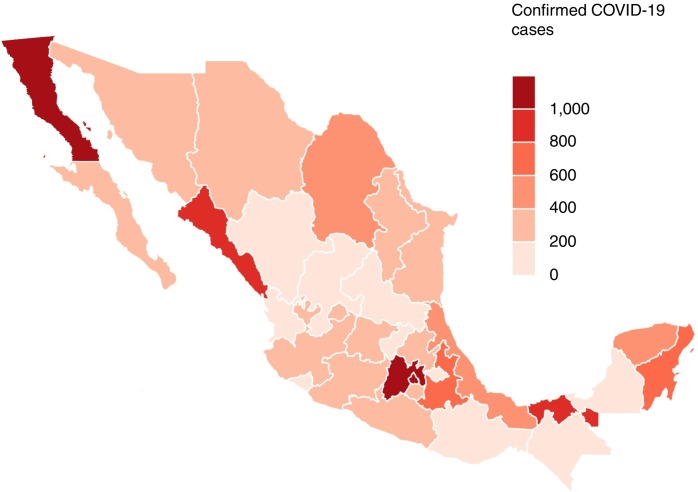
Fig. 3 shows a map of Mexico with its 32 states. Using the available information reported by the Mexican Ministry of Health, as of the 30th of April 2020, as reference, we can see that all states in Mexico reported COVID-19 infections. The states with the most reported cases were Mexico City (5209 confirmed infections), the state of Mexico (3130 cases) and Baja California (1557 cases). The states with the lowest numbers of reported COVID-19 cases in Mexico were Campeche and Nayarit with 93 confirmed cases, Zacatecas with 77, Durango with 66 and Colima with 27 cases. In addition to the measures implemented on a national scale, each state has the authority to establish additional measures to contain the propagation of COVID-19.
Figure 3.
Distribution of patients with laboratory-confirmed COVID-19 infection in Mexico by state.
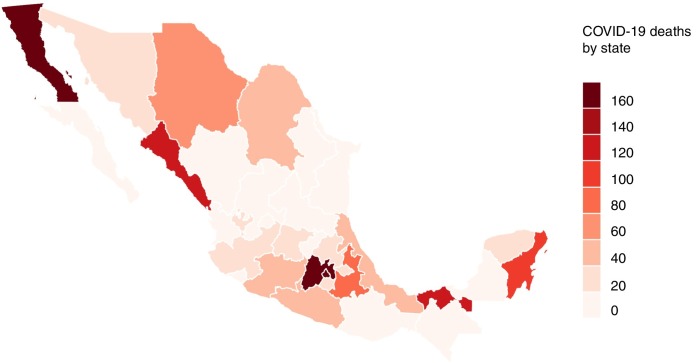
Fig. 4 shows the distribution in Mexico of the 1859 registered cases of deceased individuals from the start of the pandemic to the 30th of April 2020. Of these, 337 died in Mexico City, the most affected state, with the highest number of deaths due to the pandemic. The state of Mexico reported 239 deaths, and the states of Baja California, Sinaloa, Tabasco and Quintana Roo reported 220, 139, 125 and 116 deaths, respectively. The states that presented the lowest number of deaths were the state of Colima with 3 deaths, the state of Aguascalientes with 6 and the states of Chiapas, Durango and San Luis Potosi, with 7 deaths each.
Figure 4.
Distribution of deaths by COVID-19 in Mexico by state.
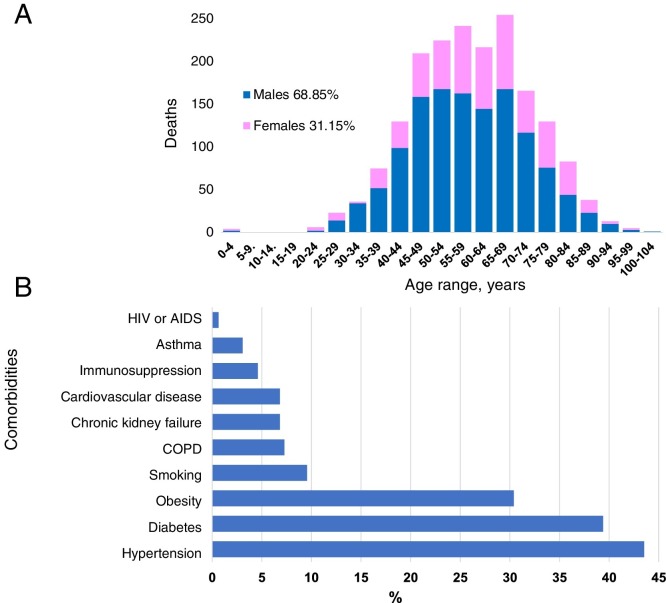
Fig. 5 a shows the age distribution for the individuals who died from COVID-19. The ages range from 0 to 104 years. Of the submitted cases, 68.85% were male and 31.15% were female. For the male sex, the largest mortality rate occurred for the 65–69 and 50–54-year age range, with 9.03% of the total deaths, followed by the 55–59 and 45–49-year ranges, with 8.76% and 8.55%, respectively. For the female sex, the age ranges with the highest mortality rates were the 65–69-year age range (4.67%) and the 55–59-year range (4.24%). The female sex presented 579 cases, thereby showing a lower lethality rate in women to date. At present, COVID-19 has a lethality rate of 9.67% in Mexico, which is higher than the worldwide rate of 7%.
Figure 5.
a) Age and sex distribution of deaths by COVID-19 in Mexico. b) Comorbidities presented in the individuals who died due to COVID-19 in Mexico.
Abbreviations: AIDS, acquired immune deficiency syndrome; COPD, chronic obstructive pulmonary disease; HIV, human immunodeficiency virus.
Fig. 5b presents the comorbidities of the 1859 patients who died in Mexico. Comorbidities increased the risk of complications in the cases with COVID-19. The patients who died had one or more comorbidities: 43.53% of those who died had hypertension; 39.39% had diabetes; 30.4% had obesity; 9.56% were smokers; 7.27% had chronic obstructive pulmonary disease; 6.82% had chronic renal failure and cardiovascular disease; 4.59% were immunosuppressed; 3.06% had asthma; and 0.64% had HIV or AIDS. A number of patients showed several comorbidities simultaneously, which made them more susceptible to severe disorders due to COVID-19.
Discussion
The present study describes the epidemiological characteristics of COVID-19 in Mexico between February and April 2020. In the study period, there were 19,224 confirmed cases and 1859 (9.67%) deaths. In terms of the demographic characteristics, there was a clear predominance of middle-aged patients (30–59 years of age) and a higher rate among men (68.85%). Among the deceased, the most predominant underlying diseases were hypertension, diabetes and obesity.
The comparison between Mexico and China of the epidemic’s characteristics in the first 64 days after diagnosing the index case reveal the following findings: the number of confirmed diagnoses in Mexico was 76% lower than in China, which counted 80,304 cases, and the number of deaths was 37% lower than that reported by China. However, the lethality rate in Mexico was 9.67%, whereas the rate in China was 3.66%.
The analysis of the confirmed data by country should be interpreted with caution, because it depends on the total number of tests performed on the population. Results differing from the actual situation could be generated if sufficient tests are not performed to estimate the number of infected people in a region, given that a large number of asymptomatic cases can be left out of the study, as well as people with mild symptoms or who died before the COVID-19 test was performed. However, the number of people who died from COVID-19 is a datum that allows us to measure the impact of the pandemic caused by SARS-CoV-2 on a particular region.
We can observe this impact by comparing the lethality rates between Mexico and China. Mexico presented a higher lethality rate than China, but the number of deaths was lower in 1087 cases, which means that the lethality rate varies with respect to the number of confirmed COVID-19 cases, with the number of tests performed on the population an important factor.
In this respect, the number of diagnostic tests that Mexico conducts is 0.69 tests for every 1000 inhabitants,25 whereas in China, the estimated number is 3 tests for every 1000 inhabitants. Mexico is in last place in the number of tests conducted to identify COVID-19 among the 36 member countries of the Organization for Economic Cooperation and Development (OECD),26 which represents a limitation in the ability to identify asymptomatic cases and accurately estimate the number of infected individuals.
It is important to mention that diagnostic tests are our window into the pandemic and help us observe how the virus propagates in a certain area. It is therefore of utmost importance to increase the number of diagnostic tests in Mexico. This lack of testing might explain the higher lethality rate in Mexico, a finding that could at first view give an erroneous impression of the impact of the COVID-19 pandemic in Mexico: if we compare the data on deaths 64 days after the first diagnosed case, there would be a lower impact in Mexico.
In terms of the control measures to mitigate the outbreak of the COVID-19 pandemic, the government of China, specifically the local government of Wuhan, suspended all travel within the city, isolating the population by means of a mandatory quarantine on the 23rd of January 2020. They took these measures 24 days after the start of the outbreak, and by that date there were already 571 cases of COVID-19. In Mexico, the federal government began suspending certain financial activities, restricting mass congregations and recommending home protection for the general population on the 24th of March, 26 days after the start of the outbreak, with 405 reported cases. It is worth mentioning that at the time the measures for preventing and containing the propagation of COVID-19 were implemented, Mexico had 166 fewer cases than China, i.e., 29% fewer. There is evidence that approximately 60% of the Mexican population follow the measures taken by the federal government in the established quarantine; however, this percentage varies dramatically from one population to the next.
This study presented the characteristics of COVID-19 in Mexico 64 days after the first confirmed case in the country. The data for performing the analysis shown in the graphs are the data officially submitted by the Mexican Ministry of Health. These data are taken from the symptom onset date and are recorded according to the patients’ statements. The initial or mild symptoms might therefore have gone unnoticed, which could hinder the determination of the exact incubation time for COVID-19.
The pandemic caused by SARS-CoV-2 is still active in Mexico. Specific data on the propagation speed and lethality of the outbreak in Mexico is therefore still not available. To control the outbreak, we need to conduct the largest number of tests possible to obtain more accurate results: the early determination and investigation of the epidemiological characteristics of new infectious diseases is essential for limiting their transmission through prevention and control.
Moreover, the financial impact on the population due to the travel restriction measures is an important factor that needs to be taken into account. An extended period of quarantine or the emergence of new outbreaks could result in serious financial complications on a national scale.
Conclusion
COVID-19 constitutes a worldwide health emergency. Up to the 30th of April 2020, rigorous efforts have been undertaken worldwide to contain the virus by means of mandatory quarantines in some countries. To date, 4 months after the onset of the virus, there are 3,090,445 laboratory confirmed cases of COVID-19 worldwide, and more than 217,769 people have died from the infection. The rapid growth in the number of infections worldwide is therefore highly concerning.
The first case of COVID-19 detected in Mexico was on the 27th of February 2020. Sixty-four days after the first diagnosed case, the number of cases had increased rapidly, following an exponential growth trend. As of the 30th of April 2020, the total number of cases of COVID-19 in Mexico was 19,224, including 1,859 deaths.
There is no doubt that more research is needed to help define the precise mechanism of person-to-person transmission. It is clear that the pandemic potential of COVID-19 requires rigorous surveillance and continuous monitoring to accurately track outbreaks, as well as their evolution, transmissibility and pathogenicity. The abovementioned factors are of considerable importance because they can define the actual lethality rate, which can vary according to various characteristics, such as the mean age of the population, sex, comorbidities present (which often vary from country to country) and the quantity of tests performed on the population. It is therefore important that information on the virus flows from nation to nation so as to measure the impact that this virus can have in the future.
In response to this worldwide outbreak, we have summarized the current state of knowledge on COVID-19 in Mexico up to April 2020. This information is valuable for understanding the spread of the disease and the effect of containment measures in Mexico.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Footnotes
Please cite this article as: Suárez V, Suarez Quezada M, Oros Ruiz S, Ronquillo De Jesús E. Epidemiología de COVID-19 en México: del 27 de febrero al 30 de abril de 2020. Rev Clin Esp. 2020;220:463–471.
References
- 1.Ren L., Wang Y., Wu Z., Xiang Z.C., Guo L., Xu T. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J. 2020;133:1015–1024. doi: 10.1097/CM9.0000000000000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J Med Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bogoch A., Watts A., Thomas-Bachli C., Huber C., Kraemer M.U., Kamran K. Pneumonia of unknown etiology in Wuhan, China: potential for international spread via commercial air travel. J Trav Med. 2020;27 doi: 10.1093/jtm/taaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. CDC 2019 Novel Coronavirus (2019-nCoV) Frequently Asked Questions and Answers. https://www.cdc.gov/coronavirus/2019-ncov/faq.html.
- 5.Health Alert Network (HAN). CDC HAN Archive-00426. https://emergency.cdc.gov/han/han00426.asp.
- 6.Centers for Disease Control and Prevention. CDC 2019 Novel Coronavirus (2019-nCoV) Situation Summary. https://www.cdc.gov/coronavirus/2019-ncov/summary.html.
- 7.Palacios Cruz M., Santos E., Velázquez Cervantes M.A., León Juárez M. COVID-19, una emergencia de salud pública mundial. Rev Clin Esp. 2020 doi: 10.1016/j.rce.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO). Novel Coronavirus (2019-nCoV) Situation Reports situation reports, https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf.
- 9.Zhang J., Yan K., Ye H., Lin J., Zheng J.J., Cai T. SARS-CoV-2 turned positive in a discharged patient with COVID-19 arouses concern regarding the present standard for discharge. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization (WHO). Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov).
- 11.World Health Organization. (WHO) Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020, https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-atthe-media-briefing-on-covid-19---11-march-2020.
- 12.Centers for Disease Control and Prevention. 2019 Novel Coronavirus (2019-nCoV) Situation Summary. https://www.cdc.gov/coronavirus/2019-ncov/summary.html.
- 13.Centers for Disease Control and Prevention. 2019 Novel Coronavirus (2019-nCoV) Transmission. https://www.cdc.gov/coronavirus/2019-%20ncov/about/transmission.html.
- 14.Centers for Disease Control and Prevention, 2019 Coronavirus Disease 2019 Transcript for CDC Media Telebriefing. https://wwwdev.cdc.gov/media/releases/2020/s0215-Diamond-Princess-Repatriation.html.
- 15.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graham Carlos W., Dela Cruz C.S., Cao B., Pasnick S., Jamil S. Novel Wuhan (2019-nCoV) coronavirus. Am J Respir Crit Care Med. 2020;201:7–8. doi: 10.1164/rccm.2014P7. [DOI] [PubMed] [Google Scholar]
- 17.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang W., Tang J., Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol. 2020;92:441–447. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization (WHO). Novel Coronavirus (2019-nCoV) Situation Reports. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200430-sitrep-101-covid-19.pdf?sfvrsn=2ba4e093_2.
- 20.Secretaría de Salud (SSA). Aviso Epidemiológico - Casos de infección respiratoria asociados a Coronavirus (COVID-19). https://www.gob.mx/cms/uploads/attachment/file/544683/UIES-APV-Pandemia-COVID19-SARSCoV2-v08-31Mar2020.pdf.
- 21.World Health Organization (WHO). Protocolo de investigación de los primeros casos y sus contactos directos (FFX)de la enfermedad por Coronavirus 2019 (COVID-19). https://www.who.int/docs/default-source/coronaviruse/covid-19-master-ffx-protocol-v2-sp-web.pdf?sfvrsn=7ad940f_8.
- 22.Secretaría de Salud (SSA). Técnico Diario Nuevo Coronavirus en el Comunicado Mundo (COVID-19). https://www.gob.mx/salud/documentos/coronavirus-covid-19-comunicado-tecnico-diario-238449.
- 23.Secretaría de Salud (SSA). Casos Confirmados a enfermedad por COVID-19. https://www.gob.mx/salud/documentos/coronavirus-covid-19-comunicado-tecnico-diario-238449.
- 24.Secretaría de Salud (SSA). Comunicado inicia la fase 3 por Covid-19. https://coronavirus.gob.mx/2020/04/21/inicia-la-fase-3-por-covid-19/.
- 25.Oxford Martin School, to understand the global pandemic, we need global testing–the Our World in Data COVID-19 Testing dataset. https://ourworldindata.org/coronavirus-testing.
- 26.OECD, Testing for COVID-19: A way to lift confinement restrictions. https://read.oecd-ilibrary.org/view/?ref=129_129658-l62d7lr66u&title=Testing-for-COVID-19-A-way-to-lift-confinement-restrictions.