Abstract
In metal-peptide interactions, cations form stable complexes through bonds with coordinating groups as side chains of amino acids. These compounds, among other things, exert a wide variety of antimicrobial activities through structural changes of peptides upon metal binding and redox chemistry. They exhibit different mechanisms of action (MOA), including the modification of DNA/RNA, protein and cell wall synthesis, permeabilization and modulation of gradients of cellular membranes. Nowadays, the large increase in antibiotic resistance represents a crucial problem to limit progression at the pandemic level of the diseases that seemed nearly eradicated, such as tuberculosis (Tb). Mycobacterium tuberculosis (Mtb) is intrinsically resistant to many antibiotics due to chromosomal mutations which can lead to the onset of novel strains. Consequently, the maximum pharmaceutical effort should be focused on the development of new therapeutic agents and antimicrobial peptides can represent a valuable option as a copious source of potential bioactive compounds. The introduction of a metal center can improve chemical diversity and hence specificity and bioavailability while, in turn, the coordination to peptides of metal complexes can protect them and enhance their poor water solubility and air stability: the optimization of these parameters is strictly required for drug prioritization and to obtain potent inhibitors of Mtb infections with novel MOAs. Here, we present a panoramic review of the most recent findings in the field of metal complex-peptide conjugates and their delivery systems with the potential pharmaceutical application as novel antibiotics in Mtb infections.
Keywords: metallopeptides, antimicrobial peptides, Mycobacterium tuberculosis, drug delivery
1. Introduction
Tuberculosis (Tb) is an airborne infectious disease caused by the bacillus Mycobacterium Tuberculosis (Mtb). Unfortunately, even though several therapies have been developed, tuberculosis still has a high incidence and mortality rate. Current drugs and vaccines have no significant impact on its control; indeed, Tb incidence rates are now higher than 25 years ago. According to the World Health Organization (WHO), every year, 10 million people get sick. Despite being a preventable and curable disease, 1.5 million/year die of Mtb infections, making it the world’s top infectious killer [1]. The emergence of drug-resistant Tb (multidrug-resistant (MDR-Tb) and extensively drug-resistant (XDR-Tb)) is considered a public health crisis, with several strains actually resistant to all available drugs [2]. The Mtb cell wall has a peculiar conformation that concurs to the onset of MDR, since it is characterized by features belonging both to Gram-positive and -negative cell envelopes: it has a peptidoglycan layer almost as thick as in Gram-positive bacteria and an outer layer composed by glycolipids similar to the external membrane of Gram-negative bacteria [3]. In detail, the mycobacterial wall is called a myco-membrane and presents an uncommon thickness, even though constituted of different layers, each with a different hydrophobicity, in dependence of the diverse composition of lipids and sugars. Indeed, moving from the external surface toward the inner cytoplasmic membrane, different structural polymers are observable: glycolipids, mycolic acids, arabinogalactans, peptidoglycans, and lipomannans [4]. Peptidoglycan and arabinogalactan are hydrophilic layers that prevent the passage of hydrophobic drugs and are covalently linked to an external layer of mycolic acids and wax-D (macromolecular peptidoglycolipids) moieties that in turn, being mainly hydrophobic, form a barrier that encumbers the penetration of hydrophilic molecules into bacteria [5]. Thus, the permeability of the wall is highly restricted and the antibiotics have difficulty passing through this barrier, and many antimicrobial compounds are active against mycobacteria only at high concentrations [6].
A promising field to answer to drug resistance in the pharmaceutical research is the development of novel and peptide-based compounds as therapeutic antibiotics. Often, peptides demonstrated elected compounds to target proper and difficult targets as protein complexes for their high specificity as well as recent and innovative synthetic strategies [7]. Several natural antimicrobial peptides (AMPs) have been identified over time and many improvements of their biological activity were achieved through their ad hoc chemical modifications. Among these variations, the coordination of the transition metal can be included: the presence of a metal ion can alter the AMP’s structure, but also provide redox action on targets; this strategy is also used to interfere with the metals belonging to bacteria. A crucial point in overcoming drug resistance is the full comprehension of the way of action of known drugs and how it can be improved by the presence of metal cofactors for the design of novel metal antibiotics based on natural AMPs. This review aims to discuss modified AMP structures and their MOAs, focusing on the potentialities of their therapeutic use in Tb infection.
Antimicrobial Peptides
AMPs are usually short peptide sequences endowed with a broad range of activity against both Gram-positive and -negative bacteria; many of them also show anti-biofilm activity [1,8] through inhibition of biofilm formation and adhesion or disruption of pre-formed biofilms and down-regulation of quorum-sensing factors. AMPs can exhibit remarkable levels of specificity and genetic variability at the level of single amino acids, can dramatically alter resistance to infection. The pharmacodynamics and MOAs of AMPs are much more favorable than those of conventional antibiotics for the prevention of resistance evolution [9].
Natural AMPs belong to the innate immune system in humans, animals and plants [10,11], they combat infections by influencing the host’s immune responses and limiting enhanced inflammation [12]: they can lead to bacterial cell death through both membranolytic and non-membranolytic mechanisms or the interaction with intracellular targets, such as DNA, RNA, and proteins. AMPs are characterized by both hydrophobic and hydrophilic domains and are typically short (less than 50 amino acid residues) and strong cationic character (for this, they are often called cationic antimicrobial peptides (CAMPs)) [12,13]: hence, the positive net charge ensures better interaction with negatively charged bacterial membranes. CAMPs can differ significantly in sequence and structure and are classified on the basis of their conformations [12]; usually, they accumulate at the cellular surface and, once a certain concentration is reached, they assemble on the bacterial membrane. In the barrel-stave model of the membrane penetration mechanism, peptides perpendicularly enter the membrane, promoting lateral peptide-peptide interactions. In this mechanism, the amphipathic structure of AMPs is crucial, since hydrophilic residues form the channels’ lumen, while the hydrophobic side establishes favorable interactions with lipoid membranes [14].
The main classes of CAMPs in vertebrates are defensins and cathelicidins. Defensins have a common β-sheet core stabilized with three disulfide bonds between six conserved cysteines and are subdivided into α-, β-, and θ-defensins on the basis of the linkages of Cys [12,15,16], while most cathelicidins are α-helical, amphipathic, with a hydrophobic surface that favors the interaction and perturbation of membranes with anionic surfaces [12]. Other cathelicidins comprise β-hairpin peptides (12–18 residues) and linear sequences (13–39 residues), that are involved into immunomodulation of the inflammatory response [17,18,19].
Several natural AMPs also demonstrated their antimicrobial activities against Mtb and, more recently, on the basis of investigated MOAs, many synthetic peptides have been designed and tested against various mycobacteria strains, providing improved and novel antimicrobial activities [20]. Several examples of both natural and chemically modified AMPs are reported in Table 1 [21]. Among the investigated models, the anti-mycobacterial compound produced by Pantoea dispersa W18 named pantocin wh-1 is a short peptide of 16 residues endowed with a cyclic structure, which demonstrated anti-Tb activity both in vitro and in vivo [22]. The screening of a library of small sequences (~10 amino acids) designed using a collection of 253 natural CAMPs active against Pseudomonas aeruginosa and optimized in silico provided several promising compounds with low toxic effects [23] against Mtb. Five of the most active sequences were modified by inserting cinnamic acid to the N-terminal side and then tested in vitro: they proved more effective against Mtb strains than unmodified parental peptides [24].
Table 1.
Examples of recently developed (2013–2020) natural and chemically modified Antimicrobial peptides (AMPs) against Tb.
| Natural Peptides | ||||
|---|---|---|---|---|
| AMP | Chemical Structure | Source | Activity | Mechanism of Action (MOA) |
| Pantocin wh-1 [22] | Cycle | Pantoea dispersa W18 | Mycobacterium smegmatis mc2 155, H37Ra mice | Unknown |
| Lassomycin [29] | Cycle | Lentzea kentuckyensis | Mtb and Mycobacterium avium subsp. paratuberculosis. | ATP-protease ClpC1P1P2 |
| Bacteriocin AS-48 [30] | Cycle | Enterococcus faecalis | H37Rv, H37Ra, BCG Pasteur 1173, Mt103, CDC1551, GC 1237, H37Rv phoP, SS18b, M. smegmatis mc2 155 | Disruption of cell membranes |
| Micrococcin P1 [35] | Thio-cycle | Staphylococci | H37Rv | Inhibition of protein synthesis |
| Teixobactin [36] | Iso-cycle | Eleftheria terrae (β-proteobacterium) | H37Rv | Inhibition of cell wall synthesis |
| Ecumicin [37] | Cycle | Nonomuraea spp. MJM5123 | H37Rv | Inhibition of ClpC1 |
| Rufomycin I/Ilamycin A [38] | Cycle | Streptomyces sp. (MJM3502), Streptomyces atratus (NRRL B-16927) | Mtb and Mycobacterium abscessus | Inhibition of ClpC1 |
| Synthetic Peptides | ||||
| Several cationic antimicrobial peptides (CAMPs) [23] | Cationic peptide rich in W and R | Peptide libraries | M. smegmatis mc2 6, H37Rv and Mycobacterium tuberculosis lux strain | Pore formation |
| Cinnamic acid (Cin+) CAMP1, 2, 3, 5, 7 [24] | N-terminally modified protein | Five de novo proteins designed from CAMPs [23] | H37Rv, Multi drug resistant Tubercolosis (MDR-Tb) | Pore formation |
| hBD consensus hBD10 [25] | Disulfide bonds | Human β-defensin (hBD) | Multi drug resistant (MDR) strains, H37Rv | Possible activity on Kv channels |
| NZX [26] | Cysteine-rich protein | Plectasin | BCG, H37Rv | Unknown |
| Vaejovis punctatus Antimicrobial peptide (VpAmp1.0, 2.0) [27] | Cycle, disulfide bond | Mexican scorpion Vaejovis punctatus | MDR strains, H37Rv | Cell lysis |
| Cyclohexyl griselimycin (CGM) [28] | Cycle | H37Rv, M. smegmatis mc2 155, | Inhibition of dnaN | |
| Vesicle associated membrane proteins (VAMP) α1, α2, α4 (VapBC30) [39] | α-helix | Fragments of VapBC30 | H37Rv | Inhibition of VapB30/VapC30 |
| d-LAK 120 [40] | D-amino acid derivative, α-helix | MDR strains |
|
|
| LL37-analogous peptide(LLAP) [41] | LL-37 | M. smegmatis | Inhibition of ATPase | |
| Synthetic AMPs (SAMPs-Dma) [42] | Dimethylamination and imidazolation | De novo designed | M. smegmatis mc2 155 |
|
| Innate defense regulators ((IDR)-1002, -HH2, IDR-1018) [43,44,45] | Macrophage chemotactic protein-1 (MCP-1) | H37Rv, MDR strains |
|
|
| RNAse (RN3) (1–45) (RN6) (1–45) (RN7) (1–45) [46,47] |
RNAse (RN)N-terminus | Mycobacterium vaccae; Mycobacterium aurum; M. smegmatis mc2 155; Mycobacterium bovis; bacillus Calmette-Guérin (BCG) |
|
|
| Peptide B (Pep-B) [48] | hBD-1 (H β-Defensin-1) | H37Rv |
|
|
| Synthetic cyclomarin A [49,50] | Cycle | Cyclomarin A | M. smegmatis, H37Rv | ClpC1 activity inhibition |
| Pandinin-2 (Pin2) based [51] | Short helix | Pandinin-2 | H37Rv | Disruption of cell membranes |
Two long synthetic peptides (~30 residues) designed using the β-defensin structure inhibited growth of the H37Rv and MDR Mtb strains, but they do not provide hemolytic effects on blood cells [25]. Furthermore, two plectasin derivatives named NZ2114 and NZX demonstrated anti-microbial activity in comparison with parental LL-37, a well-known cathelicidin sequence: NZX was the most effective, since it exhibited an inhibition grade of the mycobacterial growth of 74%, effectively killed Mtb in vitro, and decreased the bacterial load in vivo [26]. Two AMPs derived from the venom glands of the Mexican scorpion Vaejovis punctatus named VpAmp1.0 and VpAmp2.0 (19, 25 residues long) were reduced in size in several smaller synthetic peptides that effectively inhibited the growth of two clinically isolated strains of Mtb, including the MDR one, with low minimum inhibiting concentrations (MICs) [27]. Noticeably, several lucky studies outlined a clear MOA as in the case of optimized derivatives of griselimycin that proved highly active against Mtb both in vitro and in vivo by inhibiting the DNA polymerase sliding clamp dnaN [28]; conversely, lassomycin binds to an acidic region of the ATP-dependent Clp protease (ClpC1) and markedly stimulates its ATPase activity without stimulating catalyzed proteolysis (ClpP1P2), which is essential for the viability of Mtb [29].
Synergistic effects against Mtb strains between AMPs and conventional tuberculosis drugs were observed in several studies. Bacteriocin AS-48 produced by Enterococcus faecalis demonstrated interesting antimycobacterial activity alone that is enhanced if used in combination with a lysozyme or ethambutol [30]. Similarly, two synthetic 11-residue peptides derived from the Naja atra cathelicidin (ATRA-1A and ATRA-2) that bear variations of a repeated motif and one derived from the human β-defensin hBD3 (hBD3-Pep4) demonstrated synergistic effects with rifampicin (Rf), above all against Mycobacterium smegmatis [31].
More recently, a new therapeutic approach has emerged to treat tuberculosis, host-directed therapy (HDT), which aims to induce immune modulation. It involves agents that are not microbicides per se, but can additively or synergistically enhance activity of the anti-Tb drugs. HDT can be used to improve long-term functional outcomes of respiratory tract infections (RTIs), such as MDR-Tb [32]. For example, in a Tb infection, Mtb down-regulates the expression of LL-37 in human macrophages; this reduction can be counteracted by treating the infected macrophages with vitD3, phenylbutyrate (PBA), or their combination [33]. Indeed, 1,25(OH)2-vitamin D modulates cathelicidin and defensin gene expression in innate immune cells, such as monocytes and macrophages [34].
2. Metal-Based Antibiotic Therapeutic Agents
2.1. Antimicrobial Metal Complexes
Metal-based compounds represent promising potential new drugs for different diseases: cancer, neurodegeneration, and inflammation [52,53,54,55].
In the antimicrobial field, metal complexes associated with known AMPs often present different MOAs with respect to single peptides: the destruction of bacterial plasma membranes as well as hydrolytic or oxidative cleavage of nucleic acids promoted by metal-based compounds has garnered significant interest as a result of their broad range of application [56].
Nuclease function is involved in a variety of biological functions, including nucleic acid synthesis, recombination, regulation, processing, and degradation [57,58,59,60], hence the development of low molecular weight metal complexes as “artificial nucleases” is of crucial importance [61]. For most natural metallonucleases, Mg2+ is the best candidate ion due to its high natural availability and Lewis acidity, but several examples involving Zn2+, Ca2+, and other metals have been reported [62,63]: in these studies, the metal ion promotes hydrolysis of the nucleic acid phosphate backbone [64]. The rate of cleavage depends on the metal and on the formation of the metal-bound hydroxide nucleophilic intermediates. An alternative approach in the degradation of nucleic acids consists of an oxidative cleavage in the presence of redox-active ions through intermediates that produce reactive oxygen species (ROS) followed by electron transfer (ET) from the metal to molecular oxygen or peroxide. The oxidized metal is then reduced by ascorbate or dithiothreitol (DTT) to continue ROS formation, which typically abstracts hydrogen from the deoxyribose/ribose ring followed by spontaneous cleavage of C–C and C–O bonds (Figure 1A) [65]. Efficient synergy derives from DNA cleavage coupled to the inhibition of biofilm formation [66]. Recently, the ability of passivated gold nanoparticles (NPs) with multiple Ce4+ complexes on the surface of colloidal magnetic particles to degrade extracellular DNA (eDNA) and inhibit biofilm formation was reported [67].
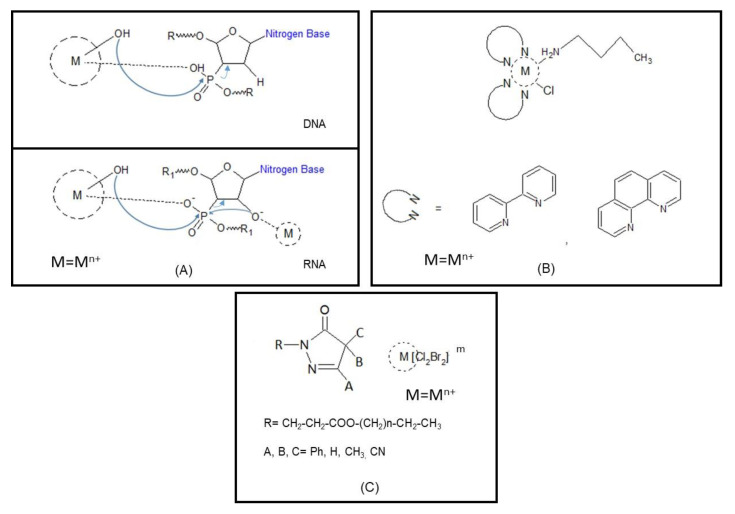
Figure 1.
Schematic representation of DNA/RNA cleavage catalyzed by metal complexes; arrows indicate the nucleophilic attack and leaving groups during substitution, Mn+ = mostly divalent cations (A) assisted by metallosurfactants with bidentate N,N ligands (B), and (C) with different substituents, Mn+ = mostly in octahedral and tetrahedral coordination geometry, m = the net charge of the complex, including surfactant contribution.
Metal complexes with amphiphilic character called metallosurfactants exhibit precise properties: they present long alkyl chains (hydrophobic part) and metal ions coordinate, mostly, ligands with nitrogen donors (hydrophilic fragment). Due to the presence of different functional regions, they can be soluble both in water and non-polar solvents and can be adsorbed both at fat/water or air/water interfaces; and, as other surfactants, they can self-assemble to form aggregates after reaching the critical aggregation concentration (cac) [68]. Interestingly, metal complexes with amphiphilic molecules demonstrated ability to penetrate cells more easily than the ligands alone [69]: in these, donor atoms present high electron density increasing the hydrophobicity of the system, thus the adsorption on the lipidic cell walls occurs with less difficulty, allowing easy passage through the bacterial membrane. An excellent example is related to antimicrobial Co3+ complexes bearing as ligands N,N-donor ligands, such as ethylenediamine (en), bipyridine (bipy), phenanthroline (phen), or triethylenetetramine (trien), with a long chain amine ligand (Figure 1B). These metallosurfactants demonstrated ability to bind DNA and to inhibit growth of some bacterial and fungal species [70].
Similarly, square planar complexes of different ions including long alkyl chains with amine functionalities aiding the formation of bilayers or metallomicelles demonstrated activity against various pathogenic microorganisms: hemolysis assay demonstrated different toxicities (Fe > Ni > Co) at concentrations below the critical micelle concentration (cmc) [71]. Pyrazolinone and pyrazolone moieties as surfactants were coordinated through an ester bond with long alkyl chains and Sn and Cu were used as counter ions (Figure 1C): while the cationic surfactants themselves already showed moderate antibacterial activity as salts, an important increase in activity was achieved (Sn > Cu). The authors correlate the activity of the metal complexes with their electronegativity with respect to a single molecule [72]. Also, benzaldehyde derivatives condensed with amines with long alkyl chains demonstrated a modest activity against Gram-positive and -negative bacteria strains as well as fungi; this activity resulted in the mobility increased by complexation of transition metal ions, in particular, of Co, Cu, and Mn. Similarly, in these complexes, the high electron density within the ligand increased the hydrophobicity of the molecules if coordinated to metal ions [73].
2.2. Metal-Antimicrobial Peptides
Among metal complexations of AMPs, an intensely explored motif is Amino Terminal Cu(II)- and Ni(II)(ATCUN), a Cu2+- and Ni2+-binding sequence with an XXH stretch usually as an amino terminal, where X is any amino acid [74]. Piscidins are a family of AMPs found in the teleosts; two of them, P1 (FFHHIFRGIVHVGKTIHRLVTG) and P3 (FIHHIFRGIVHAGRSIGRFLTG), are linear peptides that exhibit broad antibacterial activity, although their MOAs are quite different [75,76]: in detail, P3 proved less toxic to mammalian cells and more active on biofilms and persister cells. The ATCUN motif is Phe-Phe-His- for P1 and Phe-Ile-His- for P3 and binds Cu2+ and Ni2+ ions with high affinity: the α-amine group, the two amide nitrogens of the backbone, and the δ-nitrogen of the third His form the ligand field with a planar coordination geometry [77]. Both P1 and P3 cross bacterial membranes and co-localize with intracellular DNA, but P3 is more condensing to DNA, while P1 is more membrane-active, and the bactericidal effects of P3 are enhanced in the presence of Cu2+ caused by the formation of radicals (superoxide O2, hydroxyl radical HO) that nick DNA [78]. Interestingly, progressive loss of the plasmid supercoiled form pUC19 and an increase of the nicked and linearized forms of DNA were outlined during the time-dependent cleavage of the plasmid incubated with P3 in the presence of H2O2 and ascorbic acid [76].
More recently, in a study related to the Clostridioides difficile infection, a hospital-acquired disease highly resistant to multiple classes of antibiotics, it has been pointed out that P1, P3 activities strongly depend on the anaerobic conditions corroborating the hypothesis related to the formation of radical species during their MOA [79]. Ovispirin 3 (OV-3) is a synthetic AMP derived from the sheep myeloid antimicrobial peptide (SMAP-29) [80], a cathelicidin member, with antimicrobial activity against a variety of pathogens [81,82]. Metallopeptide analogs of OV-3 exhibited DNA/RNA binding and nucleasic activity in vitro and higher antimicrobial activity with lower MIC values towards Escherichia coli [83].
The ATCUN motif also naturally occurs in histatin-5 (Hst-5) [84], a 24-residue sequence found in saliva that binds Cu2+ with a dissociation constant KD in the picomolar range [85], or hepcidin (Hpc-25), a 25-residue peptide involved in iron homeostasis for which KD has a micromolar value [86]. Hst-5 is a conformationally dynamic peptide, with bioactive forms preferentially stabilized by zinc interactions that make it responsive to the coordination of other divalent metal ions, with distinct copper and zinc sites [87]. At the same time, Hpc-25 was identified as the main iron regulator in the human body through the binding to the iron exporter ferroportin: the N-terminus of Hpc is responsible for this interaction and with the same motif, in turn, it is able to bind Cu and Ni enhancing its antimicrobial power [88]. Other examples of an ATCUN sequence are Asp–Ala–His in serum albumin (HSA) and Gly–His–Lys present in several wound-healing factors: encouraging reported results open the way to add a high-affinity Cu-binding site to almost any peptide or protein by chemical or recombinant approaches [89]. Noticeably, XXH motifs have already been grafted to short AMPs (such as anoplin or buforin), which act by interacting with the cell membrane [90] or inhibiting intracellular targets, revealing a powerful strategy to increase their biological activity [91].
Sub5 is a short synthetic AMP derived from the screening of substitution library of bactenecin 2 [92] and the addition of an ATCUN motif to Sub5 showed a 2- to 3-fold increase in antimicrobial activity for a variety of microbes, with MICs and KD values of DNA7RNa binding in the low micromolar range [93]. On the other hand, several other systems intrinsically need the presence of metal ions: mucin 7 (named MUC7 or MG2) is a salivary protein whose fragments exhibited strong antimicrobial activities acting as a natural multicomponent protector of organisms against pathogens; its MOA implies the presence of metals. Recently, several shorter versions of Sub5, 12-mer peptides containing both or alternatively His3 and His8 for the coordination to metals were investigated against bacterial and fungal strains revealing activity against Enterococcus faecalis and Staphylococcus epidermidis enhanced upon Cu2+ or Zn2+ addition. Coordination studies revealed the formation of mainly mononuclear complexes in a solution in which the binding affinity appeared inversely proportional to the antimicrobial properties indicating a tunable balance between KD and MIC values [94].
Moreover, biophysical studies strongly aid the definition of MOAs, for example, bacitracin A, a cyclic peptide produced by Bacillus subtilis and licheniformis, exhibited the ability to bind to diverse divalent metals with potential different effects [95]: the Mn–bacitracin complex showed enhanced inhibition of microbial growth of Gram-positive Staphylococcus aureus and Enterococcus spp., but also a potent SOD-like (superoxide dismutase) activity suggesting the ability to continue functioning under stress. The crystal structure of the Zn2+ complex exhibited an octahedral coordination geometry in which ligands are constituted by the N-terminus of the peptide, Glu4, and thiazoline nitrogen [96]. Dermicidin is secreted from eccrine sweat glands and proteolytically processed into two fragments, dermicidin-1 and 1-L (DCD-1 and DCD-1L), active against E. coli, Enterococcus faecalis, and S. aureus. Circular Dichroism (CD) studies revealed that peptide fragments adopt α-helical conformations both in sodium dodecyl sulfate (SDS) [97] and TFE (2,2,2-trifluoroethanol) and oligomerization was observed for DCD-1L in a process stabilized by the Zn2+ ion, suggesting that it could also occur in vivo [98,99].
Furthermore, clavanin A (VFQFLGKIIHHVGNFVHGFSHVF), a 23-residue AMP that shows an α-helical conformation in a hydrophobic environment, exhibited a wide range of antimicrobial functions that are mainly exerted through liposome permeabilization and appeared enhanced upon the coordination of Zn2+ to His17 and His21 [100].
On the other hand, transition metals appear essential nutrients for pathogens and mammals through “nutritional immunity” that limits their availability [101]. Furthermore, hosts are also able to secrete antimicrobial peptides, such as microplusin, psoriasin, and calprotectin, that inhibit bacterial infection through metal binding.
Microplusin structurally presents three disulfide bonds and five α-helices and is active against Gram-positive bacteria, but not Gram-negative ones. This can be justified by different physiological levels of copper; indeed, the addition of copper changes its effects toward Micrococcus luteus and Cryptococcus neoformans, suggesting that it functions by sequestering copper from pathogens [102]. Calprotectin is a member of the S100 family that undergoes heterodimerization through the coordination of metal ions, above all, of zinc and manganese, but more recently, it has been demonstrated that calprotectin’s activity and metal binding can be further influenced by the presence of calcium, which improves the affinity for both zinc and manganese [103].
An unusual, but essential for Mtb cytochrome P450 metallo-enzyme (CYP) named CYP121A1 catalyzes the oxidative coupling of two tyrosine residues in the substrate cyclodityrosine (cYY) to generate a C−C bond: this process seems to be strictly related to the biosynthesis of glycopeptide antibiotics, such as vancomycin and teicoplanin. CYP121 is not found in other microorganisms and appears a valid target for the development of specific agents against Mtb [104].
2.3. Antibiotic Metal Complexes in Mtb Treatment
Over the last years, the metal coordination of the antibiotics already known has been pursued to overcome problems connected to impeding ways: the recent studies with Mtb demonstrated that metal complexes of isoniazid act preferentially against drug-resistant strains [105]. Similarly, a class of functionalized 1,8-disubstituted cyclam metal derivatives displays (i) low micromolar activity against MDR-Mtb, (ii) no toxicity to human cells, and (iii) inhibition of intracellular growth [106]. Derivatives of 1,8-naphthalimide bearing two pendent groups as ligands produced a series of metal complexes endowed with micromolar antimycobacterial activity: most lead compounds contain a metal ion (Cu2+ or Zn2+) coordinated to the macrocycle [106] (Figure 2A).
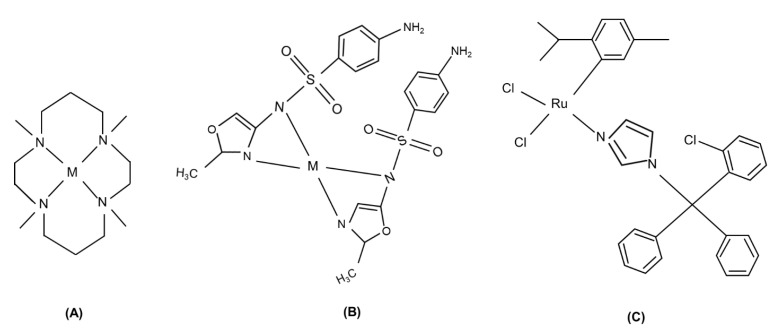
Figure 2.
Several examples of metal-drug complexes: (A) cyclam derivatives, M = Mn+, (B) sulfonamide complexes, M = Mn+, (C) ruthenium-clotrimazole metal complex.
Sulfadoxine is a sulfonamide used in combination with pyrimethamine to treat malaria caused by the Plasmodium falciparum parasite [107]. Pyrimethamine and sulfadoxine target two enzymes that are crucial to the parasitic folate biosynthetic pathway, i.e., dihydrofolate reductase (DHFR) and dihydropteroatesynthetase (DHPS). With respect to this, cobalt, copper, nickel, and zinc complexes of the sulfonamide 4-[(E)-(5-bromo-2-hydroxyphenyl)methylidene]-amino-N-(4,6-dimethyl-pyrimidinyl)benzenesulfonamide revealed moderate to significant antibacterial activity against one or more bacterial strains and good antifungal activity [108] (Figure 2B).
Several ruthenium complexes containing the 2-pyridinecarboxylic acid anion (picolinate) already demonstrated potential anti-Tb activity [109,110]; more recently, novel arene Ru, cyclopentadienyl (Cpx) Rh and Ir complexes containing an N,N’-chelated pyridylimino or quinolylimino ligand functionalized with the sulfadoxine were tested: in these complexes, the imino and pyridyl/quinolyl nitrogens provided an N,N-chelation site for the metal and exhibited potent antiplasmodial activity with IC50 values in the low micromolar range. An increase in the size of both the Cpx ligand and the aromatic imino substituent increased hydrophobicity and antiplasmodial activity [111].
Sulfonamide copper complexes presented antibacterial activity; their general formula is as follows: [Cu(sulfa−)2(N^N)], where sulfa is the anionic form of a sulfonamide ligand (sulfameter (mtrH) or sulfadimethoxine (sdmx)) and N^N is bipy or phen; they exhibit different geometry and oligomeric state depending on ligand hindrance and demonstrated the ability to bind DNA [112] and good anti-Mtb activity in the micromolar range [113].
Clotrimazole (CTZ) an old antifungal agent with high efficacy and minimal side effects [114], showed antitumoral effects and lower cytotoxicity in complex with ruthenium (RuCl2(CTZ)2)in comparison with platinum complexes [115]. Recently, different Ru/phosphine/diimine complexes demonstrated a promising activity against Mtb; in particular, three new complexes with the general formula [RuCl(CTZ)(bipy)(P-P)]PF6, where P-P can be 1,2-bis(diphenylphos-phino)ethane, 1,4-bis(diphenylphosphino)butane, and 1,1′-bis(diphenylphosphino)ferrocene, were analyzed. These complexes generated hydrophobic interactions with proteins and DNA causing anti-Mtb activity with the MIC values equivalent or enhanced if compared to free CTZ, cycloserine, gentamicin, tobramycin, and clarithromycin [116], (Figure 2C).
Similar good results were obtained by diphosphine-derivative Ru-complexes; bis(diphenylphosphino)amines are donor ligands containing a single nitrogen atom between two phosphorus atoms (P-N-P) able to form a quaternary chelating ring for a metal center with the following general formula: [RuCl(η6-p-cymene)(P-NR-P)]X, where R can be = CH2Py, CH2Ph, Ph, p-tol, and X = PF6− or BF4−. In the antimicrobial mechanism against Mtb, a crucial role appeared exerted by the basicity of the amines, which can affect the donor ability of the P-N-P ligands [117].
Ternary copper complexes with the general formula Cu(N-O)(N-N)(ClO4)2, in which N-O = 4-fluorophenoxyacetic acid hydrazide (4-FH) or 4-nitrobenzoic hydrazide (4-NH) and N-N = phen, 4–4′-dimethoxy-2-2′-bipyridine (dmb) or bipy demonstrated interesting antimicrobial activity: they displayed an octahedral distorted geometry around the copper ion in which both ligands are coordinated in a bidentate mode, (N-O) and (N-N). CD analysis revealed their ability to bind DNA [118] to explain their MOAs and, in comparison with similar compounds containing aromatic diimine ligands (N-N), they appeared the most active [118,119,120].
An interesting antimicrobial compound endowed with potential is the 8-hydroxyquinoline (8HQ): recently, a high-throughput screening identified ~200 8HQ derivatives exhibiting micromolar MIC values against Mtb; this activity appeared to be enhanced by its ability to chelate metal ions as Cu2+ in a 1:1 complex [121].
More in general, copper is able to enhance the antimicrobial activity of other basic antibiotics, such as viomycin and capreomycin, which are the most effective agents against MDR-Tb. The Cu–viomycin complex is stabilized by H-bonds able to induce helical conformation into the peptide and is able to cause strong DNA degradation [122]; this mechanism is associated with the modulation of the antigenomic delta ribozyme catalytic activity [123].
Similarly, copper is able to enhance the antimicrobial activity of isoniazids (INH) that represent the most commonly used drugs in Tb [124]: in the study of related MOAs, they exhibited the ability to form lipophilic vehicles for the delivery of the undamaged INH moiety into bacteria [125].
Four INH–copper complexes with different INH derivatives, such as 2-pyridinecarboxaldehydeisonicotinoyl hydrazone (HPCIH) 2-acetylpyridine-(HAPIH), 2-pyridineformamide-(HPAmIH), and pyrazineformamide-(HPzAmIH), exhibited different and controversial performance towards Mtb [125]; the same compounds coordinated to Ag+ did not exhibit substantial enhancement of the anti-Mtb activity [126].
Very recent promising results have been obtained by a novel class of Cu and Co compounds containing benzohydroxamate as a ligand: the investigated compounds interact with the enzyme urease, which is crucial for the bacillus survival in the intraphagosomal environment [127].
Furthermore, Pd complexes with capreomycin (C), kanamycin (K), and ofloxacin (Ofx) have been characterized: NMR studies revealed that in the C–Pd compound, different species are present and the tetra hydropyrimidinic is the prevalent one: for K–Pd, proton nuclear magnetic resonance (1HNMR) spectra present an overall broadness indicating that two Pd ions can contemporarily or singularly bind two different sites, similar to the Ofx–Pd complex [128]. Ferrocene derivatives appear to have a great impact as antiproliferative compounds in breast cancer and infections [129]: they generate ROS due to the presence of the redox-active Fe2+ [130]: recently, nine different isonicotinyl and pyrazinyl ferrocenyl-based complexes have been characterized and analyzed and only mononuclear complexes exhibited antimicrobial action against Tb [131].
3. Delivery Systems for Antibacterial Compounds in Tb
Various drug delivery systems have been exploited over the last years in the therapeutic strategies related to Tb: metal NPs of Ni, Ag, Au [132,133], metal complexes of antibiotics [134], as well as polymers with antimicrobial properties, both decorated with AMPs and not. This latter strategy has the advantage to combine synergistically the effects of bioactive polymer matrices with drugs [135,136,137].
Most of used delivery nanosystems summarized in Table 2 include liposomes, metal/polymeric/multifunctional NPs, dissolvable hydrogel microneedles [138,139]. For example, liposomes composed of both lipidic and aqueous fractions are used for the delivery of amphiphilic molecules, while multifunctional NPs (based on silver, titanium, gold) are applied to entrap, couple, or adsorb AMPs combining their antimicrobial activity with that of the peptides [140].
Table 2.
Most common antimicrobial delivery systems.
| Cargo System | Antimicrobial Compound | Bacteria |
|---|---|---|
| Liposomes | LL-37 | Escherichia coli [141], Pseudomonas aeruginosa [176] |
| Ni NPs | LL-37 | General Bacteria [142] |
| Au NPs | Surfactin, lactoferrin | Staphylococcus aureus and E. coli [98,144] |
| Ag NPs | Silver | Mycobacterium bovis, Mtb [146,177] |
| Micro and nano-emulsions | Ru complexes | Mtb [147,148,149,150,151] |
| Folate/mannose-conjugated NPs | Ga3* complexes, Rf | Mtb [156] |
| Polymeric NPs | CTZ, Rf | Mtb [159,160] |
| Dissolvable microneedles | Ag85B | Mtb [166] |
| Self-assembly nanoparticles | KSL peptide | Staphylococcus epidermidis, aureus |
The LL-37 peptide, once encapsulated in lipid nanostructures [141] or coated onto magnetic Ni NPs, maintained its antimicrobial activities with longer times of action [142]; Au and Ag [143] NPs conjugated with both thioalkenes and lipo-surfactin or lactoferrin exhibited enhanced antimicrobial activities with respect to peptides alone [98,144]; in these studies, NPs seemed to aid the contact of AMPs with bacterial membranes [98,145] causing DNA damage through the production of ROS [146].
Ru/phosphine/diimine complexes, lichexanthone derivates, 1,2,3-triazole analogues of carbohydrate, Co/sulfonamide, Ag and Au/2-(2-thienyl)benzothiazole complexes exhibited an in vitro activity against resistant Mtb strains [147,148,149,150,151], but quickly degraded in cellular contexts [109,152,153]; furthermore, their entrapment in microemulsions [154] and nanomicelles [155] enhanced their bioavailability. Different types of Ga3* complexes and rifampicin (Rf) in folate- or mannose-conjugated NPs were prepared in such a way as to enhance targeting of Mtb-infected macrophages [156].
More recently, the incorporation of Rf and the encapsulation into Ag NPs on the CS-g-(CA-MA-PZA) (amphiphilic chitosan-grafted-(acetyl alcohol-maleic anhydride-pyrazinamide) polymer has been carried out: these multi-drug delivery systems demonstrated the ability to enhance biocompatibility and cytotoxic effects on the cells [157]. More in general, the combination of polymeric NPs with antimicrobial inorganic systems is widely investigated: metal-based poly(lactic-co-glycolic acid) (PLGA) nanostructures were used to provide new properties to PLGA derivatives, such as antimicrobial, photo-thermal, magnetic, and bioimaging properties [158]. For example, the polyethylene glycol (PEG-PLGA/magnetite (γ-Fe2O3)) co-assembled with the antibiotic cotrimoxazole resulted in an excellent delivery system for the release of a drug via an external magnetic impulse [159]. Similarly, Au-conjugated PLGA-PEG-succinate-PEG-PLGA NPs assembled with Rf exhibited a time-controlled release useful for a long-term personalized therapy [160] and, similarly, Rf–Cu complexes were assembled in several structures with PEGs of different length [161].
Biodegradable multimetallic microparticles (MMPs) containing Ag and ZnO NPs were coated with Rf and successfully used for pulmonary delivery of anti-tubercular drugs to the endosomal system of Mtb-infected macrophages [162]. Furthermore, the combination of Rf with curcumin (CUR) in dual-loaded NPs demonstrated improved mycobacterial clearances [163]. On the other hand, multifunctional drug delivery systems Fe3O4/chitosan/isoniazid magnetic NPs with optimized size, excellent loading capacity, good magnetic properties, nontoxicity, and pH-triggered drug release property appeared applicable for tuberculosis treatment with excellent magnetic sensitivity and sustained release [164].
An innovative strategy is represented by polymeric dissolvable structures known as microneedles: they are able to create small holes in the stratum corneum to improve drug diffusion into the dermis joining the transdermal delivery ability of hypodermic needles with the advantages of dermal patches (safe and painless) [139,165]. Recently, hyaluronate (HA) microneedles have been investigated as possible vaccines against Tb; they allow for a time-dependent release of the Ag85B protein of Mtb, inducing a greater immune response in comparison with an intramuscular injection [166].
Similarly, self-assembly structures of peptides [167,168,169,170,171,172] improve stability and pharmacokinetic properties of AMPs and better internalize in host cells by endocytosis after conversion into vesicles [173]. Examples of this strategy are Linocin M18 and Lactacin F, which spontaneously form particles of 20–50 nm, or Iturin A, which is able to self-associate in vesicles of 150 nm in size [174]. On the other hand, there is the cationic peptide KSL capable of self-encapsulating into NPs retaining its antimicrobial activity for a long time against Staphylococcus epidermidis and Staphylococcus aureus bacteria [175].
4. Conclusions and Future Perspectives
The identification of new therapeutic strategies to counteract infections is the main challenge in medicine as recently pointed out by the wide spread of COVID-19 [178].
To address the drug resistance experienced in Tb infection, innovative strategies should explore the compounds alternative to current ones, but also combine new leads with non-standard delivery systems. Antimicrobial peptides can be considered valid candidates in the fight against Mtb, since they present unique features, especially for their highly specific MOAs that reflect into nano/micromolar KD values toward their targets. But bacterial invasions are often very difficult to eradicate and the use of a high concentration of antibiotics has to be discouraged for their toxicity. The lack of newly discovered antibiotics prompt pharmaceutical research to enlarge the explored chemical diversity and metal-based antibiotics represent a wide and partially unknown world. In this review, we tried to outline the far-reaching impact of metal complexes on antibiotic drug discovery processes and also their potential use in combination with AMPs in Mtb infections. Metal-based compounds can be very versatile per se: their multiple MOAs due to different inertness of complexes and the tuning effects exerted by different coordination geometries both in redox and hydrophobicity features can pave the way to unexplored intervention ways. Anyway, to date, no metal-drug complexes have been approved by the FDA specifically for Mtb treatment, even if several transition metal compounds such as auranofin or ganite are FDA-approved drugs for other diseases and demonstrate a certain activity against Mtb [110]. In this context, the simultaneous optimization of cargo systems for the delivery of innovative antibiotics will lead to the identification of revolutionary treatments also increasing their market access.
Author Contributions
Conceptualization, D.M.; writing–original draft preparation, D.M., C.D.N., and I.D.B.; writing–review and editing, D.M., C.D.N., and I.D.B.; visualization, A.D.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by POR CAMPANIA FESR 2014/2020, “Combattere la resistenza tumorale: piattaforma integrata multidisciplinare per un approccio tecnologico innovativo alle oncoterapie-Campania Oncoterapie”, Project No. B61G18000470007.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.World Health Organization . Global Tuberculosis Control. World Health Organization; Geneva, Switzerland: 2011. World Health Organization global tuberculosis control report 2009. [Google Scholar]
- 2.Gandhi N.R., Nunn P., Dheda K., Schaaf H.S., Zignol M., Van Soolingen D., Jensen P., Bayona J. Multidrug-resistant and extensively drug-resistant tuberculosis: A threat to global control of tuberculosis. Lancet. 2010;375:1830–1843. doi: 10.1016/S0140-6736(10)60410-2. [DOI] [PubMed] [Google Scholar]
- 3.Maitra A., Munshi T., Healy J., Martin L.T., Vollmer W., Keep N.H., Bhakta S. Cell wall peptidoglycan in Mycobacterium tuberculosis: An Achilles’ heel for the TB-causing pathogen. FEMS Microbiol. Rev. 2019;43:548–575. doi: 10.1093/femsre/fuz016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dulberger C.L., Rubin E.J., Boutte C.C. The mycobacterial cell envelope–A moving target. Nat. Rev. Microbiol. 2019;18:1–13. doi: 10.1038/s41579-019-0273-7. [DOI] [PubMed] [Google Scholar]
- 5.Smith T., Wolff K.A., Nguyen L. Molecular biology of drug resistance in Mycobacterium tuberculosis. Curr. Top. Microbiol. Immunol. 2013;374:53–80. doi: 10.1007/82_2012_279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodriguez C.A., Papanastasiou E.A., Juba M., Bishop B. Covalent modification of a ten-residue cationic antimicrobial peptide with levofloxacin. Front. Chem. 2014;2:71. doi: 10.3389/fchem.2014.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.La Manna S., Di Natale C., Florio D., Marasco D. Peptides as therapeutic agents for inflammatory-related diseases. Int. J. Mol. Sci. 2018;19:2714. doi: 10.3390/ijms19092714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Somma A., Moretta A., Canè C., Cirillo A., Duilio A. Antimicrobial and Antibiofilm Peptides. Biomolecules. 2020;10:652. doi: 10.3390/biom10040652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazzaro B.P., Zasloff M., Rolff J. Antimicrobial peptides: Application informed by evolution. Science. 2020;368:eaau5480. doi: 10.1126/science.aau5480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown-Elliott B.A., Nash K.A., Wallace R.J. Antimicrobial susceptibility testing, drug resistance mechanisms, and therapy of infections with nontuberculous mycobacteria. Clin. Microbiol. Rev. 2012;25:545–582. doi: 10.1128/CMR.05030-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao X., Wu H., Lu H., Li G., Huang Q. LAMP: A database linking antimicrobial peptides. PLoS ONE. 2013;8:e66557. doi: 10.1371/journal.pone.0066557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mookherjee N., Anderson M.A., Haagsman H.P., Davidson D.J. Antimicrobial host defence peptides: Functions and clinical potential. Nat. Rev. Drug Discov. 2020;19:311–332. doi: 10.1038/s41573-019-0058-8. [DOI] [PubMed] [Google Scholar]
- 13.Craik D.J., Fairlie D.P., Liras S., Price D. The future of peptide-based drugs. Chem. Biol. Drug Design. 2013;81:136–147. doi: 10.1111/cbdd.12055. [DOI] [PubMed] [Google Scholar]
- 14.Henderson J.M., Waring A.J., Separovic F., Lee K.Y.C. Antimicrobial peptides share a common interaction driven by membrane line tension reduction. Biophys. J. 2016;111:2176–2189. doi: 10.1016/j.bpj.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morrison G.M., Semple C.A., Kilanowski F.M., Hill R.E., Dorin J.R. Signal sequence conservation and mature peptide divergence within subgroups of the murine β-defensin gene family. Mol. Biol. Evol. 2003;20:460–470. doi: 10.1093/molbev/msg060. [DOI] [PubMed] [Google Scholar]
- 16.Semple C.A., Rolfe M., Dorin J.R. Duplication and selection in the evolution of primate β-defensin genes. Genome Biol. 2003;4:R31. doi: 10.1186/gb-2003-4-5-r31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Harten R.M., Van Woudenbergh E., Van Dijk A., Haagsman H.P. Cathelicidins: Immunomodulatory antimicrobials. Vaccines. 2018;6:63. doi: 10.3390/vaccines6030063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zanetti M. Cathelicidins, multifunctional peptides of the innate immunity. J. Leukoc. Biol. 2004;75:39–48. doi: 10.1189/jlb.0403147. [DOI] [PubMed] [Google Scholar]
- 19.Mookherjee N., Rehaume L.M., Hancock R.E. Cathelicidins and functional analogues as antisepsis molecules. Expert Opin. Ther. Targets. 2007;11:993–1004. doi: 10.1517/14728222.11.8.993. [DOI] [PubMed] [Google Scholar]
- 20.Shukla P. Applied Microbiology and Bioengineering: An Interdisciplinary Approach. Academic Press; Cambridge, MA, USA: 2018. [Google Scholar]
- 21.Yathursan S., Wiles S., Read H., Sarojini V. A review on anti-tuberculosis peptides: Impact of peptide structure on anti-tuberculosis activity. J. Pept. Sci. 2019;25:e3213. doi: 10.1002/psc.3213. [DOI] [PubMed] [Google Scholar]
- 22.Teng T., Li X., Zhang L., Li Y. Identification and Characterization of pantocin wh-1, a Novel Cyclic Polypeptide Produced by Pantoea dispersa W18. Molecules. 2020;25:485. doi: 10.3390/molecules25030485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramón-García S., Mikut R., Ng C., Ruden S., Volkmer R., Reischl M., Hilpert K., Thompson C.J. Targeting Mycobacterium tuberculosis and other microbial pathogens using improved synthetic antibacterial peptides. Antimicrob. Agents Chemother. 2013;57:2295–2303. doi: 10.1128/AAC.00175-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silva S., Santos-Silva A., Da Costa J.M.C., Vale N. Potent cationic antimicrobial peptides against Mycobacterium tuberculosis in vitro. J. Glob. Antimicrob. Resist. 2019;19:132–135. doi: 10.1016/j.jgar.2019.04.018. [DOI] [PubMed] [Google Scholar]
- 25.Rodriguez A., Pedersen M.Ø., Villegas E., Rivas-Santiago B., Villegas-Moreno J., Amero C., Norton R.S., Corzo G. Antimicrobial activity and structure of a consensus human β-defensin and its comparison to a novel putative hBD10. Proteins Struct. Funct. Bioinf. 2020;88:175–186. doi: 10.1002/prot.25785. [DOI] [PubMed] [Google Scholar]
- 26.Tenland E., Krishnan N., Rönnholm A., Kalsum S., Puthia M., Mörgelin M., Davoudi M., Otrocka M., Alaridah N., Glegola-Madejska I. A novel derivative of the fungal antimicrobial peptide plectasin is active against Mycobacterium tuberculosis. Tuberculosis. 2018;113:231–238. doi: 10.1016/j.tube.2018.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramírez-Carreto S., Jiménez-Vargas J.M., Rivas-Santiago B., Corzo G., Possani L.D., Becerril B., Ortiz E. Peptides from the scorpion Vaejovis punctatus with broad antimicrobial activity. Peptides. 2015;73:51–59. doi: 10.1016/j.peptides.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 28.Kling A., Lukat P., Almeida D.V., Bauer A., Fontaine E., Sordello S., Zaburannyi N., Herrmann J., Wenzel S.C., König C. Targeting DnaN for tuberculosis therapy using novel griselimycins. Science. 2015;348:1106–1112. doi: 10.1126/science.aaa4690. [DOI] [PubMed] [Google Scholar]
- 29.Gavrish E., Sit C.S., Cao S., Kandror O., Spoering A., Peoples A., Ling L., Fetterman A., Hughes D., Bissell A. Lassomycin, a ribosomally synthesized cyclic peptide, kills Mycobacterium tuberculosis by targeting the ATP-dependent protease ClpC1P1P2. Chem. Biol. 2014;21:509–518. doi: 10.1016/j.chembiol.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aguilar-Pérez C., Gracia B., Rodrigues L., Vitoria A., Cebrián R., Deboosère N., Song O.-R., Brodin P., Maqueda M., Aínsa J.A. Synergy between circular bacteriocin AS-48 and ethambutol against Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2018;62:e00359-18. doi: 10.1128/AAC.00359-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gupta K., Singh S., Van Hoek M.L. Short, synthetic cationic peptides have antibacterial activity against Mycobacterium smegmatis by forming pores in membrane and synergizing with antibiotics. Antibiotics. 2015;4:358–378. doi: 10.3390/antibiotics4030358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rao M., Ligeiro D., Maeurer M. Precision medicine in the clinical management of respiratory tract infections including multidrug-resistant tuberculosis: Learning from innovations in immuno-oncology. Curr. Opin. Pulm. Med. 2019;25:233–241. doi: 10.1097/MCP.0000000000000575. [DOI] [PubMed] [Google Scholar]
- 33.Ahmed S., Raqib R., Guðmundsson G.H., Bergman P., Agerberth B., Rekha R.S. Host-Directed Therapy as a Novel Treatment Strategy to Overcome Tuberculosis: Targeting Immune Modulation. Antibiotics. 2020;9:21. doi: 10.3390/antibiotics9010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Golpour A., Bereswill S., Heimesaat M.M. Antimicrobial and immune-modulatory effects of vitamin D provide promising antibiotics-independent approaches to tackle bacterial infections–lessons learnt from a literature survey. Eur. J. Microbiol. Immunol. 2019;9:80–87. doi: 10.1556/1886.2019.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Degiacomi G., Personne Y., Mondésert G., Ge X., Mandava C.S., Hartkoorn R.C., Boldrin F., Goel P., Peisker K., Benjak A. Micrococcin P1–A bactericidal thiopeptide active against Mycobacterium tuberculosis. Tuberculosis. 2016;100:95–101. doi: 10.1016/j.tube.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 36.Ling L.L., Schneider T., Peoples A.J., Spoering A.L., Engels I., Conlon B.P., Mueller A., Schäberle T.F., Hughes D.E., Epstein S. A new antibiotic kills pathogens without detectable resistance. Nature. 2015;517:455–459. doi: 10.1038/nature14098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gao W., Kim J.-Y., Chen S.-N., Cho S.-H., Choi J., Jaki B.U., Jin Y.-Y., Lankin D.C., Lee J.-E., Lee S.-Y. Discovery and characterization of the tuberculosis drug lead ecumicin. Org. Lett. 2014;16:6044–6047. doi: 10.1021/ol5026603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choules M.P., Wolf N.M., Lee H., Anderson J.R., Grzelak E.M., Wang Y., Ma R., Gao W., McAlpine J.B., Jin Y.-Y. Rufomycin targets ClpC1 proteolysis in Mycobacterium tuberculosis and M. abscessus. Antimicrob. Agents Chemother. 2019;63:e02204-18. doi: 10.1128/AAC.02204-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee I.-G., Lee S.J., Chae S., Lee K.-Y., Kim J.-H., Lee B.-J. Structural and functional studies of the Mycobacterium tuberculosis VapBC30 toxin-antitoxin system: Implications for the design of novel antimicrobial peptides. Nucleic Acids Res. 2015;43:7624–7637. doi: 10.1093/nar/gkv689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kwok P.C.L., Grabarek A., Chow M.Y., Lan Y., Li J.C., Casettari L., Mason A.J., Lam J.K. Inhalable spray-dried formulation of D-LAK antimicrobial peptides targeting tuberculosis. Int. J. Pharm. 2015;491:367–374. doi: 10.1016/j.ijpharm.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 41.Chingaté S., Delgado G., Salazar L.M., Soto C.-Y. The ATPase activity of the mycobacterial plasma membrane is inhibited by the LL37-analogous peptide LLAP. Peptides. 2015;71:222–228. doi: 10.1016/j.peptides.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 42.Sharma A., Pohane A.A., Bansal S., Bajaj A., Jain V., Srivastava A. Cell penetrating synthetic antimicrobial peptides (SAMPs) exhibiting potent and selective killing of Mycobacterium by targeting its DNA. Chem. A Eur. J. 2015;21:3540–3545. doi: 10.1002/chem.201404650. [DOI] [PubMed] [Google Scholar]
- 43.Huante-Mendoza A., Silva-García O., Oviedo-Boyso J., Hancock R.E., Baizabal-Aguirre V.M. Peptide IDR-1002 inhibits NF-κB nuclear translocation by inhibition of IκBα degradation and activates p38/ERK1/2-MSK1-dependent CREB phosphorylation in macrophages stimulated with lipopolysaccharide. Front. Immunol. 2016;7:533. doi: 10.3389/fimmu.2016.00533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mansour S.C., De la Fuente-Núñez C., Hancock R.E. Peptide IDR-1018: Modulating the immune system and targeting bacterial biofilms to treat antibiotic-resistant bacterial infections. J. Pept. Sci. 2015;21:323–329. doi: 10.1002/psc.2708. [DOI] [PubMed] [Google Scholar]
- 45.Rivas-Santiago B., Castañeda-Delgado J.E., Santiago C.E.R., Waldbrook M., González-Curiel I., León-Contreras J.C., Enciso-Moreno J.A., Del Villar V., Mendez-Ramos J., Hancock R.E. Ability of innate defence regulator peptides IDR-1002, IDR-HH2 and IDR-1018 to protect against Mycobacterium tuberculosis infections in animal models. PLoS ONE. 2013;8:e59119. doi: 10.1371/journal.pone.0059119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arranz-Trullén J., Lu L., Pulido D., Bhakta S., Boix E. Host antimicrobial peptides: The promise of new treatment strategies against tuberculosis. Front. Immunol. 2017;8:1499. doi: 10.3389/fimmu.2017.01499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pulido D., Torrent M., Andreu D., Nogués M.V., Boix E. Two human host defense ribonucleases against mycobacteria, the eosinophil cationic protein (RNase 3) and RNase 7. Antimicrob. Agents Chemother. 2013;57:3797–3805. doi: 10.1128/AAC.00428-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sharma R., Saikia U.N., Sharma S., Verma I. Activity of human beta defensin-1 and its motif against active and dormant Mycobacterium tuberculosis. Appl. Microbiol. Biotechnol. 2017;101:7239–7248. doi: 10.1007/s00253-017-8466-3. [DOI] [PubMed] [Google Scholar]
- 49.Barbie P., Kazmaier U. Total synthesis of cyclomarin A, a marine cycloheptapeptide with anti-tuberculosis and anti-malaria activity. Org. Lett. 2016;18:204–207. doi: 10.1021/acs.orglett.5b03292. [DOI] [PubMed] [Google Scholar]
- 50.Kiefer A., Bader C.D., Held J., Esser A., Rybniker J., Empting M., Müller R., Kazmaier U. Synthesis of new cyclomarin derivatives and their biological evaluation towards Mycobacterium tuberculosis and Plasmodium falciparum. Chem. A Eur. J. 2019;25:8894–8902. doi: 10.1002/chem.201901640. [DOI] [PubMed] [Google Scholar]
- 51.Rodríguez A., Villegas E., Montoya-Rosales A., Rivas-Santiago B., Corzo G. Characterization of antibacterial and hemolytic activity of synthetic pandinin 2 variants and their inhibition against Mycobacterium tuberculosis. PLoS ONE. 2014;9:e101742. doi: 10.1371/journal.pone.0101742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Florio D., Iacobucci I., Ferraro G., Mansour A.M., Morelli G., Monti M., Merlino A., Marasco D. Role of the Metal Center in the Modulation of the Aggregation Process of Amyloid Model Systems by Square Planar Complexes Bearing 2-(2′-pyridyl) benzimidazole Ligands. Pharmaceuticals. 2019;12:154. doi: 10.3390/ph12040154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marasco D., Messori L., Marzo T., Merlino A. Oxaliplatin vs. cisplatin: Competition experiments on their binding to lysozyme. Dalton Trans. 2015;44:10392–10398. doi: 10.1039/C5DT01279A. [DOI] [PubMed] [Google Scholar]
- 54.Florio D., Malfitano A.M., Di Somma S., Mügge C., Weigand W., Ferraro G., Iacobucci I., Monti M., Morelli G., Merlino A. Platinum (II) O, S Complexes Inhibit the Aggregation of Amyloid Model Systems. Int. J. Mol. Sci. 2019;20:829. doi: 10.3390/ijms20040829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kanayama Y., Tsuji T., Enomoto S., Amano R. Multitracer screening: Brain delivery of trace elements by eight different administration methods. Biometals. 2005;18:553–565. doi: 10.1007/s10534-005-4775-6. [DOI] [PubMed] [Google Scholar]
- 56.Yu Z., Cowan J.A. Metal complexes promoting catalytic cleavage of nucleic acids–Biochemical tools and therapeutics. Curr. Opin. Chem. Biol. 2018;43:37–42. doi: 10.1016/j.cbpa.2017.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lirussi L., Antoniali G., Scognamiglio P.L., Marasco D., Dalla E., D’Ambrosio C., Arena S., Scaloni A., Tell G. Cleavage of the APE1 N-Terminal Domain in Acute Myeloid Leukemia Cells Is Associated with Proteasomal Activity. Biomolecules. 2020;10:531. doi: 10.3390/biom10040531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Burra S., Marasco D., Malfatti M.C., Antoniali G., Virgilio A., Esposito V., Demple B., Galeone A., Tell G. Human AP-endonuclease (Ape1) activity on telomeric G4 structures is modulated by acetylatable lysine residues in the N-terminal sequence. DNA Repair. 2019;73:129–143. doi: 10.1016/j.dnarep.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Poletto M., Malfatti M.C., Dorjsuren D., Scognamiglio P.L., Marasco D., Vascotto C., Jadhav A., Maloney D.J., Wilson III D.M., Simeonov A. Inhibitors of the apurinic/apyrimidinic endonuclease 1 (APE1)/nucleophosmin (NPM1) interaction that display anti-tumor properties. Mol. Carcinog. 2016;55:688–704. doi: 10.1002/mc.22313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Poletto M., Vascotto C., Scognamiglio P.L., Lirussi L., Marasco D., Tell G. Role of the unstructured N-terminal domain of the hAPE1 (human apurinic/apyrimidinic endonuclease 1) in the modulation of its interaction with nucleic acids and NPM1 (nucleophosmin) Biochem. J. 2013;452:545–557. doi: 10.1042/BJ20121277. [DOI] [PubMed] [Google Scholar]
- 61.Mancin F., Scrimin P., Tecilla P., Tonellato U. Artificial metallonucleases. Chem. Commun. 2005;20:2540–2548. doi: 10.1039/b418164f. [DOI] [PubMed] [Google Scholar]
- 62.Dupureur C.M. Roles of metal ions in nucleases. Curr. Opin. Chem. Biol. 2008;12:250–255. doi: 10.1016/j.cbpa.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 63.Baum D., Silverman S.K. Deoxyribozymes: Useful DNA catalysts in vitro and in vivo. Cell. Mol. Life Sci. 2008;65:2156–2174. doi: 10.1007/s00018-008-8029-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mancin F., Scrimin P., Tecilla P. Progress in artificial metallonucleases. Chem. Commun. 2012;48:5545–5559. doi: 10.1039/c2cc30952a. [DOI] [PubMed] [Google Scholar]
- 65.Jiang Q., Xiao N., Shi P., Zhu Y., Guo Z. Design of artificial metallonucleases with oxidative mechanism. Coord. Chem. Rev. 2007;251:1951–1972. doi: 10.1016/j.ccr.2007.02.013. [DOI] [Google Scholar]
- 66.Joyner J.C., Hodnick W., Cowan A.S., Tamuly D., Boyd R., Cowan J. Antimicrobial metallopeptides with broad nuclease and ribonuclease activity. Chem. Commun. 2013;49:2118–2120. doi: 10.1039/c3cc38977d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen Z., Ji H., Liu C., Bing W., Wang Z., Qu X. A Multinuclear Metal Complex Based DNase-Mimetic Artificial Enzyme: Matrix Cleavage for Combating Bacterial Biofilms. Angew. Chem. Int. Ed. 2016;55:10732–10736. doi: 10.1002/anie.201605296. [DOI] [PubMed] [Google Scholar]
- 68.Schattschneider C., Kettenmann S.D., Hinojosa S., Heinrich J., Kulak N. Biological activity of amphiphilic metal complexes. Coord. Chem. Rev. 2019;385:191–207. doi: 10.1016/j.ccr.2018.12.007. [DOI] [Google Scholar]
- 69.Walker G.W., Geue R.J., Sargeson A.M., Behm C.A. Surface-active cobalt cage complexes: Synthesis, surface chemistry, biological activity, and redox properties. Dalton Trans. 2003;15:2992–3001. doi: 10.1039/b302230g. [DOI] [Google Scholar]
- 70.Kumar R.S., Arunachalam S. Synthesis, micellar properties, DNA binding and antimicrobial studies of some surfactant–cobalt (III) complexes. Biophys. Chem. 2008;136:136–144. doi: 10.1016/j.bpc.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 71.Kaur G., Garg P., Kaur B., Chaudhary G.R., Kumar S., Dilbaghi N., Hassan P., Gawali S.L. Cationic double chained metallosurfactants: Synthesis, aggregation, cytotoxicity, antimicrobial activity and their impact on the structure of bovine serum albumin. Soft Matter. 2018;14:5306–5318. doi: 10.1039/C8SM00535D. [DOI] [PubMed] [Google Scholar]
- 72.Witthayapanyanon A., Phan T.T., Heitmann T.C., Harwell J.H., Sabatini D.A. Interfacial properties of extended-surfactant-based microemulsions and related macroemulsions. J. Surfactants Deterg. 2010;13:127–134. doi: 10.1007/s11743-009-1151-5. [DOI] [Google Scholar]
- 73.Negm N., Zaki M. Structural and biological behaviors of some nonionic Schiff-base amphiphiles and their Cu (II) and Fe (III) metal complexes. Colloid. Surf. B Biointerfaces. 2008;64:179–183. doi: 10.1016/j.colsurfb.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 74.Pinkham A.M., Yu Z., Cowan J. Attenuation of West Nile Virus NS2B/NS3 protease by amino terminal copper and nickel binding (ATCUN) peptides. J. Med. Chem. 2018;61:980–988. doi: 10.1021/acs.jmedchem.7b01409. [DOI] [PubMed] [Google Scholar]
- 75.Hayden R.M., Goldberg G.K., Ferguson B.M., Schoeneck M.W., Libardo M.D.J., Mayeux S.E., Shrestha A., Bogardus K.A., Hammer J., Pryshchep S. Complementary effects of host defense peptides piscidin 1 and piscidin 3 on DNA and lipid membranes: Biophysical insights into contrasting biological activities. J. Phys. Chem. B. 2015;119:15235–15246. doi: 10.1021/acs.jpcb.5b09685. [DOI] [PubMed] [Google Scholar]
- 76.Libardo M.D.J., Bahar A.A., Ma B., Fu R., McCormick L.E., Zhao J., McCallum S.A., Nussinov R., Ren D., Angeles-Boza A.M. Nuclease activity gives an edge to host-defense peptide piscidin 3 over piscidin 1, rendering it more effective against persisters and biofilms. FEBS J. 2017;284:3662–3683. doi: 10.1111/febs.14263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Harford C., Sarkar B. Amino terminal Cu (II)-and Ni (II)-binding (ATCUN) motif of proteins and peptides: Metal binding, DNA cleavage, and other properties. Acc. Chem. Res. 1997;30:123–130. doi: 10.1021/ar9501535. [DOI] [Google Scholar]
- 78.Rai R.K., De Angelis A., Greenwood A., Opella S.J., Cotten M.L. Metal-ion Binding to Host Defense Peptide Piscidin 3 Observed in Phospholipid Bilayers by Magic Angle Spinning Solid-state NMR. ChemPhysChem. 2019;20:295–301. doi: 10.1002/cphc.201800855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Oludiran A., Courson D.S., Stuart M.D., Radwan A.R., Poutsma J.C., Cotten M.L., Purcell E.B. How Oxygen Availability Affects the Antimicrobial Efficacy of Host Defense Peptides: Lessons Learned from Studying the Copper-Binding Peptides Piscidins 1 and 3. Int. J. Mol. Sci. 2019;20:5289. doi: 10.3390/ijms20215289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dawson R.M., Liu C.Q. Cathelicidin peptide SMAP-29: Comprehensive review of its properties and potential as a novel class of antibiotics. Drug Dev. Res. 2009;70:481–498. doi: 10.1002/ddr.20329. [DOI] [Google Scholar]
- 81.Kalfa V., Jia H., Kunkle R., McCray P., Tack B., Brogden K. Congeners of SMAP29 kill ovine pathogens and induce ultrastructural damage in bacterial cells. Antimicrob. Agents Chemother. 2001;45:3256–3261. doi: 10.1128/AAC.45.11.3256-3261.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Saiman L., Tabibi S., Starner T.D., San Gabriel P., Winokur P.L., Jia H.P., McCray P.B., Tack B.F. Cathelicidin peptides inhibit multiply antibiotic-resistant pathogens from patients with cystic fibrosis. Antimicrob. Agents Chemother. 2001;45:2838–2844. doi: 10.1128/AAC.45.10.2838-2844.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alexander J.L., Yu Z., Cowan J. Amino terminal copper and nickel binding motif derivatives of ovispirin-3 display increased antimicrobial activity via lipid oxidation. J. Med. Chem. 2017;60:10047–10055. doi: 10.1021/acs.jmedchem.7b01117. [DOI] [PubMed] [Google Scholar]
- 84.Gusman H., Lendenmann U., Grogan J., Troxler R.F., Oppenheim F.G. Is salivary histatin 5 a metallopeptide? Biochim. Biophys. Acta (BBA)-Protein Struct. Mol. Enzymol. 2001;1545:86–95. doi: 10.1016/S0167-4838(00)00265-X. [DOI] [PubMed] [Google Scholar]
- 85.Conklin S.E., Bridgman E.C., Su Q., Riggs-Gelasco P., Haas K.L., Franz K.J. Specific histidine residues confer histatin peptides with copper-dependent activity against Candida albicans. Biochemistry. 2017;56:4244–4255. doi: 10.1021/acs.biochem.7b00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kulprachakarn K., Chen Y.-L., Kong X., Arno M.C., Hider R.C., Srichairatanakool S., Bansal S.S. Copper (II) binding properties of hepcidin. JBIC J. Biol. Inorg. Chem. 2016;21:329–338. doi: 10.1007/s00775-016-1342-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chen J., Barry B.A. Ultraviolet resonance Raman microprobe spectroscopy of photosystem II. Photochem. Photobiol. 2008;84:815–818. doi: 10.1111/j.1751-1097.2008.00298.x. [DOI] [PubMed] [Google Scholar]
- 88.Abbas I.M., Vranic M., Hoffmann H., El-Khatib A.H., Montes-Bayón M., Möller H.M., Weller M.G. Investigations of the Copper Peptide Hepcidin-25 by LC-MS/MS and NMR. Int. J. Mol. Sci. 2018;19:2271. doi: 10.3390/ijms19082271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gonzalez P., Bossak K., Stefaniak E., Hureau C., Raibaut L., Bal W., Faller P. N-Terminal Cu-Binding Motifs (Xxx-Zzz-His, Xxx-His) and Their Derivatives: Chemistry, Biology and Medicinal Applications. Chem. A Eur. J. 2018;24:8029–8041. doi: 10.1002/chem.201705398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Libardo M.D., Cervantes J.L., Salazar J.C., Angeles-Boza A.M. Improved Bioactivity of Antimicrobial Peptides by Addition of Amino-Terminal Copper and Nickel (ATCUN) Binding Motifs. ChemMedChem. 2014;9:1892–1901. doi: 10.1002/cmdc.201402033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Park C.B., Yi K.-S., Matsuzaki K., Kim M.S., Kim S.C. Structure-activity analysis of buforin II, a histone H2A-derived antimicrobial peptide: The proline hinge is responsible for the cell-penetrating ability of buforin II. Proc. Natl. Acad. Sci. USA. 2000;97:8245–8250. doi: 10.1073/pnas.150518097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hilpert K., Volkmer-Engert R., Walter T., Hancock R.E. High-throughput generation of small antibacterial peptides with improved activity. Nat. Biotechnol. 2005;23:1008–1012. doi: 10.1038/nbt1113. [DOI] [PubMed] [Google Scholar]
- 93.Alexander J.L., Thompson Z., Yu Z., Cowan J. Cu-ATCUN derivatives of Sub5 exhibit enhanced antimicrobial activity via multiple modes of action. ACS Chem. Biol. 2019;14:449–458. doi: 10.1021/acschembio.8b01087. [DOI] [PubMed] [Google Scholar]
- 94.Janicka-Kłos A., Janek T., Burger J., Czapor-Irzabek H. Human salivary MUC7 mucin fragment and its analogues. Coordination and biological studies. J. Inorg. Biochem. 2020;203:110923. doi: 10.1016/j.jinorgbio.2019.110923. [DOI] [PubMed] [Google Scholar]
- 95.Chen S., Li X., Sun G., Zhang Y., Su J., Ye J. Heavy Metal Induced Antibiotic Resistance in Bacterium LSJC7. Int. J. Mol. Sci. 2015;16:23390–23404. doi: 10.3390/ijms161023390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Economou N.J., Cocklin S., Loll P.J. High-resolution crystal structure reveals molecular details of target recognition by bacitracin. Proc. Natl. Acad. Sci. USA. 2013;110:14207–14212. doi: 10.1073/pnas.1308268110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tan K.W., Ramesh K., Chew F.T., Mok Y.K. Structural basis for the bacterial membrane insertion of dermcidin peptide, DCD-1L. Sci. Rep. UK. 2017;7:1–11. doi: 10.1038/s41598-017-13600-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Alexander J.L., Thompson Z., Cowan J.A. Antimicrobial Metallopeptides. ACS Chem. Biol. 2018;13:844–853. doi: 10.1021/acschembio.7b00989. [DOI] [PubMed] [Google Scholar]
- 99.Paulmann M., Arnold T., Linke D., Özdirekcan S., Kopp A., Gutsmann T., Kalbacher H., Wanke I., Schuenemann V.J., Habeck M. Structure-activity analysis of the dermcidin-derived peptide DCD-1L, an anionic antimicrobial peptide present in human sweat. J. Biol. Chem. 2012;287:8434–8443. doi: 10.1074/jbc.M111.332270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Juliano S.A., Pierce S., DeMayo J.A., Balunas M.J., Angeles-Boza A.M. Exploration of the innate immune system of Styela clava: Zn2+ binding enhances the antimicrobial activity of the tunicate peptide clavanin A. Biochemistry. 2017;56:1403–1414. doi: 10.1021/acs.biochem.6b01046. [DOI] [PubMed] [Google Scholar]
- 101.Hood M.I., Skaar E.P. Nutritional immunity: Transition metals at the pathogen-host interface. Nat. Rev. Microbiol. 2012;10:525–537. doi: 10.1038/nrmicro2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Silva F.D., Rossi D.C., Martinez L.R., Frases S., Fonseca F.L., Campos C.B.L., Rodrigues M.L., Nosanchuk J.D., Daffre S. Effects of microplusin, a copper-chelating antimicrobial peptide, against Cryptococcus neoformans. FEMS Microbiol. Lett. 2011;324:64–72. doi: 10.1111/j.1574-6968.2011.02386.x. [DOI] [PubMed] [Google Scholar]
- 103.Gagnon D.M., Brophy M.B., Bowman S.E., Stich T.A., Drennan C.L., Britt R.D., Nolan E.M. Manganese binding properties of human calprotectin under conditions of high and low calcium: X-ray crystallographic and advanced electron paramagnetic resonance spectroscopic analysis. J. Am. Chem. Soc. 2015;137:3004–3016. doi: 10.1021/ja512204s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rajput S., McLean K.J., Poddar H., Selvam I.R., Nagalingam G., Triccas J.A., Levy C.W., Munro A.W., Hutton C.A. Structure-Activity Relationships of cyclo(l-Tyrosyl-l-tyrosine) Derivatives Binding to Mycobacterium tuberculosis CYP121: Iodinated Analogues Promote Shift to High-Spin Adduct. J. Med. Chem. 2019;62:9792–9805. doi: 10.1021/acs.jmedchem.9b01199. [DOI] [PubMed] [Google Scholar]
- 105.De Aguiar I., Tavares A., Roveda A.C., Jr., Da Silva A.C., Marino L.B., Lopes É.O., Pavan F.R., Lopes L.G., Franco D.W. Antitubercular activity of Ru (II) isoniazid complexes. Eur. J. Pharm. Sci. 2015;70:45–54. doi: 10.1016/j.ejps.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 106.Yu M., Nagalingam G., Ellis S., Martinez E., Sintchenko V., Spain M., Rutledge P.J., Todd M.H., Triccas J.A. Nontoxic metal-cyclam complexes, a new class of compounds with potency against drug-resistant Mycobacterium tuberculosis. J. Med. Chem. 2016;59:5917–5921. doi: 10.1021/acs.jmedchem.6b00432. [DOI] [PubMed] [Google Scholar]
- 107.Frost S., McKenna R. Carbonic Anhydrase: Mechanism, Regulation, Links to Disease, and Industrial Applications. Springer Science & Business Media; Berlin/Heidelberg, Germany: 2014. [Google Scholar]
- 108.Chohan Z.H., Shad H.A., Youssoufi M.H., Hadda T.B. Some new biologically active metal-based sulfonamide. Eur. J. Med. Chem. 2010;45:2893–2901. doi: 10.1016/j.ejmech.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 109.Pavan F.R., Von Poelhsitz G., Do Nascimento F.B., Leite S.R., Batista A.A., Deflon V.M., Sato D.N., Franzblau S.G., Leite C.Q. Ruthenium (II) phosphine/picolinate complexes as antimycobacterial agents. Eur. J. Med. Chem. 2010;45:598–601. doi: 10.1016/j.ejmech.2009.10.049. [DOI] [PubMed] [Google Scholar]
- 110.Frei A. Metal Complexes, an untapped Source of Antibiotic Potential? Antibiotics. 2020;9:90. doi: 10.3390/antibiotics9020090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chellan P., Avery V.M., Duffy S., Triccas J.A., Nagalingam G., Tam C., Cheng L.W., Liu J., Land K.M., Clarkson G.J., et al. Organometallic Conjugates of the Drug Sulfadoxine for Combatting Antimicrobial Resistance. Chemistry. 2018;24:10078–10090. doi: 10.1002/chem.201801090. [DOI] [PubMed] [Google Scholar]
- 112.Nakahata D.H., De Paiva R.E., Lustri W.R., Ribeiro C.M., Pavan F.R., Da Silva G.G., Ruiz A.L., De Carvalho J.E., Corbi P.P. Sulfonamide-containing copper (II) metallonucleases: Correlations with in vitro antimycobacterial and antiproliferative activities. J. Inorg. Biochem. 2018;187:85–96. doi: 10.1016/j.jinorgbio.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 113.Forgacs P., Wengenack N.L., Hall L., Zimmerman S.K., Silverman M.L., Roberts G.D. Tuberculosis and trimethoprim-sulfamethoxazole. Antimicrob. Agents Chemother. 2009;53:4789–4793. doi: 10.1128/AAC.01658-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Corcoran J., Lange A., Cumming R.I., Owen S.F., Ball J.S., Tyler C.R., Winter M.J. Bioavailability of the imidazole antifungal agent clotrimazole and its effects on key biotransformation genes in the common carp (Cyprinus carpio) Aquat. Toxicol. 2014;152:57–65. doi: 10.1016/j.aquatox.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 115.Abid M., Shamsi F., Azam A. Ruthenium complexes: An emerging ground to the development of metallopharmaceuticals for cancer therapy. Mini Rev. Med. Chem. 2016;16:772–786. doi: 10.2174/1389557515666151001142012. [DOI] [PubMed] [Google Scholar]
- 116.Colina-Vegas L., Dutra J.L., Villarreal W., Neto J.H.d.A., Cominetti M.R., Pavan F., Navarro M., Batista A.A. Ru (II)/clotrimazole/diphenylphosphine/bipyridine complexes: Interaction with DNA, BSA and biological potential against tumor cell lines and Mycobacterium tuberculosis. J. Inorg. Biochem. 2016;162:135–145. doi: 10.1016/j.jinorgbio.2016.06.023. [DOI] [PubMed] [Google Scholar]
- 117.Da Silva J.P., Silva I.C., Pavan F.R., Back D.F., De Araujo M.P. Bis (diphenylphosphino) amines-containing ruthenium cymene complexes as potential anti-Mycobacterium tuberculosis agents. J. Inorg. Biochem. 2017;173:134–140. doi: 10.1016/j.jinorgbio.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 118.Paixão D.A., Marzano I.M., Jaimes E.H., Pivatto M., Campos D.L., Pavan F.R., Deflon V.M., Maia P.I.d.S., Ferreira A.M.D.C., Uehara I.A. Novel copper (II) complexes with hydrazides and heterocyclic bases: Synthesis, structure and biological studies. J. Inorg. Biochem. 2017;172:138–146. doi: 10.1016/j.jinorgbio.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 119.Hoffman A.E., DeStefano M., Shoen C., Gopinath K., Warner D.F., Cynamon M., Doyle R.P. Co (II) and Cu (II) pyrophosphate complexes have selectivity and potency against Mycobacteria including Mycobacterium tuberculosis. Eur. J. Med. Chem. 2013;70:589–593. doi: 10.1016/j.ejmech.2013.10.044. [DOI] [PubMed] [Google Scholar]
- 120.Do Couto Almeida J., Marzano I.M., Pivatto M., Lopes N.P., Ferreira A.M.D.C., Pavan F., Silva I., Pereira-Maia E.C., Von Poelhsitz G., Guerra W. Synthesis, cytotoxic and antitubercular activities of copper (II) complexes with heterocyclic bases and 3-hydroxypicolinic acid. Inorg. Chim. Acta. 2016;446:87–92. doi: 10.1016/j.ica.2016.03.005. [DOI] [Google Scholar]
- 121.Shah S., Dalecki A.G., Malalasekera A.P., Crawford C.L., Michalek S.M., Kutsch O., Sun J., Bossmann S.H., Wolschendorf F. 8-Hydroxyquinolines are boosting agents of copper-related toxicity in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2016;60:5765–5776. doi: 10.1128/AAC.00325-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jeżowska-Bojczuk M., Stokowa-Sołtys K. Peptides having antimicrobial activity and their complexes with transition metal ions. Eur. J. Med. Chem. 2018;143:997–1009. doi: 10.1016/j.ejmech.2017.11.086. [DOI] [PubMed] [Google Scholar]
- 123.Stokowa-Sołtys K., Barbosa N.A., Kasprowicz A., Wieczorek R., Gaggelli N., Gaggelli E., Valensin G., Wrzesiński J., Ciesiołka J., Kuliński T. Studies of viomycin, an anti-tuberculosis antibiotic: Copper (ii) coordination, DNA degradation and the impact on delta ribozyme cleavage activity. Dalton Trans. 2016;45:8645–8658. doi: 10.1039/C6DT00245E. [DOI] [PubMed] [Google Scholar]
- 124.Smieja M., Marchetti C., Cook D., Smaill F.M. Isoniazid for preventing tuberculosis in non-HIV infected persons. Cochrane Database Syst. Rev. 1999;2:CD001363. doi: 10.1002/14651858.CD001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Firmino G.S., De Souza M.V., Pessoa C., Lourenco M.C., Resende J.A., Lessa J.A. Synthesis and evaluation of copper (II) complexes with isoniazid-derived hydrazones as anticancer and antitubercular agents. BioMetals. 2016;29:953–963. doi: 10.1007/s10534-016-9968-7. [DOI] [PubMed] [Google Scholar]
- 126.Ahmed M., Rooney D., McCann M., Devereux M., Twamley B., Galdino A.C.M., Sangenito L.S., Souza L.O.P., Lourenço M.C., Gomes K. Synthesis and antimicrobial activity of a phenanthroline-isoniazid hybrid ligand and its Ag+ and Mn2+ complexes. BioMetals. 2019;32:671–682. doi: 10.1007/s10534-019-00204-5. [DOI] [PubMed] [Google Scholar]
- 127.Coelho T.S., Halicki P.C.B., Silva L., Jr., De Menezes Vicenti J.R., Goncalves B.L., Almeida da Silva P.E., Ramos D.F. Metal-based antimicrobial strategies against intramacrophage Mycobacterium tuberculosis. Lett. Appl. Microbiol. 2020 doi: 10.1111/lam.13298. in press. [DOI] [PubMed] [Google Scholar]
- 128.Giovagnoli S., Marenzoni M.L., Nocchetti M., Santi C., Blasi P., Schoubben A., Ricci M. Synthesis, characterization and in vitro extracellular and intracellular activity against M ycobacterium tuberculosis infection of new second-line antitubercular drug-palladium complexes. J. Pharm. Pharmacol. 2014;66:106–121. doi: 10.1111/jphp.12162. [DOI] [PubMed] [Google Scholar]
- 129.Singh A., Lumb I., Mehra V., Kumar V. Ferrocene-appended pharmacophores: An exciting approach for modulating the biological potential of organic scaffolds. Dalton Trans. 2019;48:2840–2860. doi: 10.1039/C8DT03440K. [DOI] [PubMed] [Google Scholar]
- 130.Zhang J., Bond A.M. Conditions required to achieve the apparent equivalence of adhered solid-and solution-phase voltammetry for ferrocene and other redox-active solids in ionic liquids. Anal. Chem. 2003;75:2694–2702. doi: 10.1021/ac026329f. [DOI] [PubMed] [Google Scholar]
- 131.Stringer T., Seldon R., Liu N., Warner D.F., Tam C., Cheng L.W., Land K.M., Smith P.J., Chibale K., Smith G.S. Antimicrobial activity of organometallic isonicotinyl and pyrazinyl ferrocenyl-derived complexes. Dalton Trans. 2017;46:9875–9885. doi: 10.1039/C7DT01952A. [DOI] [PubMed] [Google Scholar]
- 132.Teixeira M.C., Carbone C., Sousa M.C., Espina M., Garcia M.L., Sanchez-Lopez E., Souto E.B. Nanomedicines for the Delivery of Antimicrobial Peptides (AMPs) Nanomaterials. 2020;10:560. doi: 10.3390/nano10030560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Makvandi P., Wang C.Y., Zare E.N., Borzacchiello A., Niu L.N., Tay F.R. Metal–Based Nanomaterials in Biomedical Applications: Antimicrobial Activity and Cytotoxicity Aspects. Adv. Funct. Mater. 2020;30:1910021. doi: 10.1002/adfm.201910021. [DOI] [Google Scholar]
- 134.Manning T., Mikula R., Lee H., Calvin A., Darrah J., Wylie G., Phillips D., Bythell B.J. The copper (II) ion as a carrier for the antibiotic capreomycin against Mycobacterium tuberculosis. Bioorg. Med. Chem. Lett. 2014;24:976–982. doi: 10.1016/j.bmcl.2013.12.053. [DOI] [PubMed] [Google Scholar]
- 135.Muñoz-Bonilla A., Fernández-García M. Polymeric materials with antimicrobial activity. Prog. Polym. Sci. 2012;37:281–339. doi: 10.1016/j.progpolymsci.2011.08.005. [DOI] [Google Scholar]
- 136.Wang C.-Y., Makvandi P., Zare E.N., Tay F.R., Niu L.-N. Advances in Antimicrobial Organic and Inorganic Nanocompounds in Biomedicine. Adv. Ther. 2020 doi: 10.1002/adtp.202000024. in press. [DOI] [Google Scholar]
- 137.Makvandi P., Gu J.T., Zare E.N., Ashtari B., Moeini A., Tay F.R., Niu L.-n. Polymeric and inorganic nanoscopical antimicrobial fillers in dentistry. Acta Biomater. 2020;101:69–101. doi: 10.1016/j.actbio.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 138.Martin-Serrano Á., Gómez R., Ortega P., De la Mata F.J. Nanosystems as vehicles for the delivery of antimicrobial peptides (AMPs) Pharmaceutics. 2019;11:448. doi: 10.3390/pharmaceutics11090448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Jamaledin R., Di Natale C., Onesto V., Taraghdari Z.B., Zare E.N., Makvandi P., Vecchione R., Netti P.A. Progress in Microneedle-Mediated Protein Delivery. J. Clin. Med. 2020;9:542. doi: 10.3390/jcm9020542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.De Almeida Pachioni-Vasconcelos J., Lopes A.M., Apolinário A.C., Valenzuela-Oses J.K., Costa J.S.R., De Oliveira Nascimento L., Pessoa A., Barbosa L.R.S., De Oliveira Rangel-Yagui C. Nanostructures for protein drug delivery. Biomater. Sci. 2016;4:205–218. doi: 10.1039/C5BM00360A. [DOI] [PubMed] [Google Scholar]
- 141.Garcia-Orue I., Gainza G., Girbau C., Alonso R., Aguirre J.J., Pedraz J.L., Igartua M., Hernandez R.M. LL37 loaded nanostructured lipid carriers (NLC): A new strategy for the topical treatment of chronic wounds. Eur. J. Pharm. Biopharm. 2016;108:310–316. doi: 10.1016/j.ejpb.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 142.Chen G., Zhou M., Chen S., Lv G., Yao J. Nanolayer biofilm coated on magnetic nanoparticles by using a dielectric barrier discharge glow plasma fluidized bed for immobilizing an antimicrobial peptide. Nanotechnology. 2009;20:465706. doi: 10.1088/0957-4484/20/46/465706. [DOI] [PubMed] [Google Scholar]
- 143.Dror Y., Ophir C., Freeman A. Innovations and Emerging Technologies in Wound Care. Elsevier; Amsterdam, The Netherlands: 2020. Silver–enzyme hybrids as wide-spectrum antimicrobial agents; pp. 293–307. [Google Scholar]
- 144.Chen W.Y., Chang H.Y., Lu J.K., Huang Y.C., Harroun S.G., Tseng Y.T., Li Y.J., Huang C.C., Chang H.T. Self-assembly of antimicrobial peptides on gold nanodots: Against multidrug-resistant bacteria and wound-healing application. Adv. Funct. Mater. 2015;25:7189–7199. doi: 10.1002/adfm.201503248. [DOI] [Google Scholar]
- 145.Zheng K., Setyawati M.I., Lim T.-P., Leong D.T., Xie J. Antimicrobial cluster bombs: Silver nanoclusters packed with daptomycin. ACS Nano. 2016;10:7934–7942. doi: 10.1021/acsnano.6b03862. [DOI] [PubMed] [Google Scholar]
- 146.Wang L., Hu C., Shao L. The antimicrobial activity of nanoparticles: Present situation and prospects for the future. Int. J. Nanomed. 2017;12:1227–1249. doi: 10.2147/IJN.S121956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Camila Micheletti A., Kika Honda N., R Pavan F., QF Leite C., De Fatima Cepa Matos M., Trentin Perdomo R., Bogo D., Braz Alcantara G., Beatriz A. Increment of antimycobaterial activity on lichexanthone derivatives. Med. Chem. 2013;9:904–910. doi: 10.2174/1573406411309070003. [DOI] [PubMed] [Google Scholar]
- 148.Dos Santos E.R., Mondelli M.A., Pozzi L.V., Corrêa R.S., Salistre-de-Araújo H.S., Pavan F.R., Leite C.Q., Ellena J., Malta V.R., Machado S.P. New ruthenium (II)/phosphines/diimines complexes: Promising antitumor (human breast cancer) and Mycobacterium tuberculosis fighting agents. Polyhedron. 2013;51:292–297. doi: 10.1016/j.poly.2013.01.004. [DOI] [Google Scholar]
- 149.Santos J.A.d., Corrales R.C.N.R., Pavan F.R., Leite C.Q.F., Dias R.M.d.P., Silva A.D.d. Synthesis and antitubercular evaluation of new 1, 2, 3-triazole derivatives of carbohydrates. Mediterr. J. Chem. 2012;1:281–288. doi: 10.13171/mjc.1.6.2012.02.05.15. [DOI] [Google Scholar]
- 150.Pereira G.A., Massabni A.C., Castellano E.E., Costa L.A.S., Leite C.Q.F., Pavan F.R., Cuin A. A broad study of two new promising antimycobacterial drugs: Ag (I) and Au (I) complexes with 2-(2-thienyl) benzothiazole. Polyhedron. 2012;38:291–296. doi: 10.1016/j.poly.2012.03.016. [DOI] [Google Scholar]
- 151.Mondelli M., Pavan F., De Souza P.C., Leite C.Q., Ellena J., Nascimento O.R., Facchin G., Torre M.H. Study of a series of cobalt (II) sulfonamide complexes: Synthesis, spectroscopic characterization, and microbiological evaluation against M. tuberculosis. Crystal structure of [Co (sulfamethoxazole) 2 (H2O) 2]·H2O. J. Mol. Struct. 2013;1036:180–187. doi: 10.1016/j.molstruc.2012.09.064. [DOI] [Google Scholar]
- 152.Pavan F.R., Poelhsitz G.V., Da Cunha L.V., Barbosa M.I., Leite S.R., Batista A.A., Cho S.H., Franzblau S.G., De Camargo M.S., Resende F.A. In vitro and in vivo activities of ruthenium (II) phosphine/diimine/picolinate complexes (SCAR) against Mycobacterium tuberculosis. PLoS ONE. 2013;8:642428. doi: 10.1371/journal.pone.0064242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pavan F.R., Poelhsitz G.V., Barbosa M.I., Leite S.R., Batista A.A., Ellena J., Sato L.S., Franzblau S.G., Moreno V., Gambino D. Ruthenium (II) phosphine/diimine/picolinate complexes: Inorganic compounds as agents against tuberculosis. Eur. J. Med. Chem. 2011;46:5099–5107. doi: 10.1016/j.ejmech.2011.08.023. [DOI] [PubMed] [Google Scholar]
- 154.Mehta S., Kaur G., Bhasin K. Tween-embedded microemulsions–Physicochemical and spectroscopic analysis for antitubercular drugs. AAPS PharmSciTech. 2010;11:143–153. doi: 10.1208/s12249-009-9356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Jeetah R., Bhaw-Luximon A., Jhurry D. Dual encapsulation and controlled delivery of anti-TB drugs from PEG-block-poly (ester-ether) nanomicelles. J. Nanopharm. Drug Deliv. 2013;1:240–257. doi: 10.1166/jnd.2013.1025. [DOI] [Google Scholar]
- 156.Choi S.-R., Britigan B.E., Moran D.M., Narayanasamy P. Gallium nanoparticles facilitate phagosome maturation and inhibit growth of virulent Mycobacterium tuberculosis in macrophages. PLoS ONE. 2017;12:e0177987. doi: 10.1371/journal.pone.0177987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Praphakar R.A., Jeyaraj M., Ahmed M., Kumar S.S., Rajan M. Silver nanoparticle functionalized CS-g-(CA-MA-PZA) carrier for sustainable anti-tuberculosis drug delivery. Int. J. Biol. Macromol. 2018;118:1627–1638. doi: 10.1016/j.ijbiomac.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 158.Zare E.N., Jamaledin R., Naserzadeh P., Afjeh-Dana E., Ashtari B., Hosseinzadeh M., Vecchione R., Wu A., Tay F.R., Borzacchiello A. Metal-Based Nanostructures/PLGA Nanocomposites: Antimicrobial Activity, Cytotoxicity, and Their Biomedical Applications. ACS Appl. Mater. Interfaces. 2020;12:3279–3300. doi: 10.1021/acsami.9b19435. [DOI] [PubMed] [Google Scholar]
- 159.Pereira E.D., Souza F.G., Jr., Pinto J.C.C., Cerruti R., Santana C. Synthesis, Characterization and Drug Delivery Profile of Magnetic PLGA-PEG-PLGA/Maghemite Nanocomposite. Wiley Online Library; Hoboken, NJ, USA: 2014. pp. 18–25. Macromolecular Symposia. [Google Scholar]
- 160.Gajendiran M., Yousuf S.M.J., Elangovan V., Balasubramanian S. Gold nanoparticle conjugated PLGA-PEG-SA-PEG-PLGA multiblock copolymer nanoparticles: Synthesis, characterization, in vivo release of rifampicin. J. Mater. Chem. B. 2014;2:418–427. doi: 10.1039/C3TB21113D. [DOI] [PubMed] [Google Scholar]
- 161.Manning T., Mikula R., Wylie G., Phillips D., Jarvis J., Zhang F. Structural measurements and cell line studies of the copper-PEG-Rifampicin complex against Mycobacterium tuberculosis. Bioorg. Med. Chem. Lett. 2015;25:451–458. doi: 10.1016/j.bmcl.2014.12.053. [DOI] [PubMed] [Google Scholar]
- 162.Ellis T., Chiappi M., García-Trenco A., Al-Ejji M., Sarkar S., Georgiou T.K., Shaffer M.S., Tetley T.D., Schwander S., Ryan M.P. Multimetallic microparticles increase the potency of rifampicin against intracellular Mycobacterium tuberculosis. ACS Nano. 2018;12:5228–5240. doi: 10.1021/acsnano.7b08264. [DOI] [PubMed] [Google Scholar]
- 163.Jahagirdar P.S., Gupta P.K., Kulkarni S.P., Devarajan P.V. Intramacrophage delivery of dual drug loaded nanoparticles for effective clearance of Mycobacterium tuberculosis. J. Pharm. Sci. 2020;20:30177-5. doi: 10.1016/j.xphs.2020.03.018. [DOI] [PubMed] [Google Scholar]
- 164.Zhao C., Liu X., Zhang X., Yan H., Qian Z., Li X., Ma Z., Han Q., Pei C. A facile one-step method for preparation of Fe3O4/CS/INH nanoparticles as a targeted drug delivery for tuberculosis. Mater. Sci. Eng. C. 2017;77:1182–1188. doi: 10.1016/j.msec.2017.03.137. [DOI] [PubMed] [Google Scholar]
- 165.Battisti M., Vecchione R., Casale C., Pennacchio F.A., Lettera V., Jamaledin R., Profeta M., Di Natale C., Imparato G., Urciuolo F. Non-invasive production of multi-compartmental biodegradable polymer microneedles for controlled intradermal drug release of labile molecules. Front. Bioeng. Biotechnol. 2019;7:296. doi: 10.3389/fbioe.2019.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Yan Q., Cheng Z., Liu H., Shan W., Cheng Z., Dai X., Xue Y., Chen F. Enhancement of Ag85B DNA vaccine immunogenicity against tuberculosis by dissolving microneedles in mice. Vaccine. 2018;36:4471–4476. doi: 10.1016/j.vaccine.2018.06.025. [DOI] [PubMed] [Google Scholar]
- 167.Di Natale C., La Manna S., Malfitano A.M., Di Somma S., Florio D., Scognamiglio P.L., Novellino E., Netti P.A., Marasco D. Structural insights into amyloid structures of the C-terminal region of nucleophosmin 1 in type A mutation of acute myeloid leukemia. Biochim. Biophys. Acta (BBA)-Proteins Proteom. 2019;1867:637–644. doi: 10.1016/j.bbapap.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 168.La Manna S., Scognamiglio P.L., Roviello V., Borbone F., Florio D., Di Natale C., Bigi A., Cecchi C., Cascella R., Giannini C. The acute myeloid leukemia-associated Nucleophosmin 1 gene mutations dictate amyloidogenicity of the C-terminal domain. FEBS J. 2019;286:2311–2328. doi: 10.1111/febs.14815. [DOI] [PubMed] [Google Scholar]
- 169.Di Natale C., Scognamiglio P.L., Cascella R., Cecchi C., Russo A., Leone M., Penco A., Relini A., Federici L., Di Matteo A. Nucleophosmin contains amyloidogenic regions that are able to form toxic aggregates under physiological conditions. FASEB J. 2015;29:3689–3701. doi: 10.1096/fj.14-269522. [DOI] [PubMed] [Google Scholar]
- 170.La Manna S., Roviello V., Scognamiglio P.L., Diaferia C., Giannini C., Sibillano T., Morelli G., Novellino E., Marasco D. Amyloid fibers deriving from the aromatic core of C-terminal domain of nucleophosmin 1. Int. J. Biol. Macromol. 2019;122:517–525. doi: 10.1016/j.ijbiomac.2018.10.210. [DOI] [PubMed] [Google Scholar]
- 171.Russo A., Diaferia C., La Manna S., Giannini C., Sibillano T., Accardo A., Morelli G., Novellino E., Marasco D. Insights into amyloid-like aggregation of H2 region of the C-terminal domain of nucleophosmin. Biochim. Biophys. Acta (BBA)-Proteins Proteom. 2017;1865:176–185. doi: 10.1016/j.bbapap.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 172.Scognamiglio P.L., Di Natale C., Leone M., Cascella R., Cecchi C., Lirussi L., Antoniali G., Riccardi D., Morelli G., Tell G. Destabilisation, aggregation, toxicity and cytosolic mislocalisation of nucleophosmin regions associated with acute myeloid leukemia. Oncotarget. 2016;7:59129. doi: 10.18632/oncotarget.10991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wang Q., Zhang X., Zheng J., Liu D. Self-assembled peptide nanotubes as potential nanocarriers for drug delivery. RSC Adv. 2014;4:25461–25469. doi: 10.1039/c4ra03304c. [DOI] [Google Scholar]
- 174.Brandelli A. Nanostructures as promising tools for delivery of antimicrobial peptides. Mini Rev. Med. Chem. 2012;12:731–741. doi: 10.2174/138955712801264774. [DOI] [PubMed] [Google Scholar]
- 175.Hissam R., Farmer B.L., Pandey R.B. Scaffolding of an antimicrobial peptide (KSL) by a scale-down coarse-grained approach. Phys. Chem. Chem. Phys. 2011;13:21262–21272. doi: 10.1039/c1cp22361e. [DOI] [PubMed] [Google Scholar]
- 176.Carmona-Ribeiro A.M., De Melo Carrasco L.D. Novel formulations for antimicrobial peptides. Int. J. Mol. Sci. 2014;15:18040–18083. doi: 10.3390/ijms151018040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Selim A., Elhaig M., Taha S., Nasr E. Antibacterial activity of silver nanoparticles against field and reference strains of Mycobacterium tuberculosis, Mycobacterium bovis and multiple-drugresistant tuberculosis strains. Rev-Off Int. Epizoot. 2018;37:823–830. doi: 10.20506/rst.37.3.2888. [DOI] [PubMed] [Google Scholar]
- 178.Harrison C. Drug researchers pursue new lines of attack against COVID-19. Nat. Biotechnol. 2020;38:659–662. doi: 10.1038/d41587-020-00013-z. [DOI] [PubMed] [Google Scholar]