Abstract
Acute or strenuous exercise is sometimes related to upper respiratory tract infections in athletes. Practicing intense and regular exercise can lead to incorrect activation of the immune system, causing athletes to be excluded from training programs and competitions. Defensins are small antimicrobial peptides that are part of the innate immune system and dynamically involved in several biological activities. In this study, we highlight the role of human defensins in competitive basketball athletes. In particular, we consider the behavior of alpha- and beta-defensins together with white blood cells in a cohort of players. Moreover, we focus our attention on cortisol, a physiological indicator of stress, and testosterone, both of which are human hormones involved in muscle metabolism. The free-testosterone/cortisol ratio is considered to be an indicator of overtraining among athletes. This paper provides an up-to-date information of the role of human defensins as self-defense molecules during a continuous stressor such as long-term exercise, and it recognizes them as potential markers of infection.
Keywords: human defensins, physical activity, immune system, stress hormones
1. Introduction
Several studies have suggested that physical activity induces considerable physiological changes within the immune system [1,2,3,4,5,6]. Human defensins are small peptides (29–34 amino acids) that belong to the human immune system. They represent a significant family of antimicrobial peptides (AMPs) that play a crucial role in infection and inflammation and that act against infectious pathogens (bacteria, viruses, fungi, and parasites) [7]. Human defensins are organized into two classes, alpha and beta [8], based on the distance between the cysteine residues and the topology of the disulfide bridges. Human alpha-defensins are small molecules isolated from human blood, and they are mainly expressed by neutrophils [9,10]; as a result, they are called human neutrophil peptides (HPN1-4). Alpha defensin 1 (HPN1) is a constitutively expressed defensin, although its levels increase during infection. Human alpha defensins 5 and 6 (HD5 and HD6) are isolated from human Paneth cells [11,12]; these molecules are only expressed in the Paneth cells of human intestines and the female reproductive system [13]. In contrast, human beta-defensins (HBDs) are mainly found in association with epithelial surfaces (skin, gut, trachea, and oral epithelia). In humans, the most studied beta-defensins are HBD1–4 [14]. Furthermore, it is known that beta defensin 1 (HBD1) is constitutively expressed; however, its serum levels may increase in the presence of diseases such as cystic fibrosis, in which it plays a crucial role in the innate immunity of the mucous membrane in the lung [15,16]. Moreover, both alpha- and beta-defensins have broad antibacterial activity [17,18] and multiple roles in innate immunity.
Physical exercise is known to cause an increase in IgA levels in athletes’ immune systems [19]. In addition, preservation of the mucosa in professional athletes reduces the initiation of upper respiratory tract infections (URTIs). URTIs can harm athletes and negatively affect competitions and training. In fact, recent studies have showed that intense exercise was associated with self-reported symptoms of URTIs in athletes [20,21,22].
In recent years, URTIs have aroused considerable interest in the medical and scientific fields due to the development of strong resistance to the antibiotics generally used to treat these disorders, including Streptococcus pneumonia, Haemophilus influenza, Moraxella catarrhalis, Streptococcus pyogenes, and Staphylococcus aureus, which are the pathogens most frequently found in URTIs. These five pathogens exhibit strong resistance to beta-lactam and macrolide antibiotics. However, the therapy currently in use involves intramuscular administration of beta-lactams and macrolides, such as amoxicillin/clavulanate or ceftriaxone. Alternative therapies involve the administration of quinolones, but these therapeutic agents are reserved for patients who develop resistance or allergies to beta-lactams and macrolides [23,24,25].
Several studies have highlighted a strong relationship between beta-defensins and the appearance of various respiratory disorders [26]. Changes in beta-defensin expression levels can lead to the improvement or deterioration of a disease. HBDs represent a valid and effective treatment against pathologies caused by drug-resistant microorganisms; in addition, HBD administration represents a solid alternative to the pharmacological therapies currently in use [27]. Moreover, a diet rich in immune nutrients (arginine, glutamine, dietary nucleotides, and fish oil) regulates the expression of HBD1 by improving immune-system function by supporting the reduction of infectious diseases and the use of antibiotics, as well as hospitalization [28]. Gałązka-Franta and colleagues reported that URTIs in competitive athletes require considerable attention, and that diagnostic methods and therapies should be used to maintain their levels of activity while following the antidoping rules currently in place [29].
A few studies have investigated the levels of alpha- and beta-defensins following physical exercise. Some studies reported an increase in the salivary levels of beta-defensins (HBD2) following exercise and an accompanying increase in hNP1–3 levels, thereby enhancing immune function [5,9]. Generally, physical exercise elicits the initial activation of leukocytes [24,25,26,27,28,29]. Specific temporal patterns exist for specific subpopulations of leukocytes involved in the post-exercise state, including a rise in neutrophils and lymphocyte migration after exercise. Hence, the neutrophil/lymphocyte ratio (NLR), which can be measured easily from whole blood, can be used as an indication of the magnitude of the systemic inflammation and the severity of the muscle damage incurred by a given bout of exercise [30]. Another important factor involved in an athlete’s physical status is cortisol. Cortisol regulates the exercise-induced acute inflammatory response and was previously reported to be associated with a rise in neutrophil numbers and a suppression of lymphocytes [31]. Furthermore, the magnitude and function of the circulating cells in the innate immune system, such as neutrophils and natural killer cells (NK-cells), and the acquired immune system may be altered by acute and chronic exposure to exercise [3]. Blood lymphocyte numbers were shown to exponentially increase following an acute bout of exercise [32,33]. Lymphocytes are stress-responsive cells that are mobilized during physical exercise and psychological stress; therefore, analysis of the proliferation of these cells in athletes suffering symptoms consistent with this phenomenon would be of interest [32]. Cortisol represents a physiological indicator of stress [34]. Sports activity can induce physical stress, causing increased secretion of cortisol from the adrenal cortex [35]. It has been suggested that cortisol levels indicate physical stress in competitive athletes and that increasing cortisol levels through exercise can trigger immunosuppression [36,37,38]. Previous studies have shed light on how increased glucocorticoid levels decrease HBD-2 expression [38,39,40], emphasizing that this relationship could be evaluated in biological fluids such as saliva [5]. The adaptation of the endocrine system to exercise training occurs physiologically via the buffering of anabolic and catabolic processes [2,41]. For example, altered cortisol/testosterone ratios, an indicator of anabolic–catabolic balance, were utilized with limited success to determine the physiological strain of exercise training [42]. The free-testosterone/cortisol ratio (fr-T/C) was proposed as a major indicator of anabolic and catabolic effects resulting from overtraining, especially among athletes. A reduction of the testosterone/cortisol ratio by more than 30% is related to overtraining status [43]. Moreover, Urhausen et al. reported that significant increases in testosterone levels without similar big differences in cortisol levels occurred after maximum aerobic training [44]; this variation in adrenal hormones may have been related to subjects responding differently to exercise [45]. While cortisol has a catabolic effect, testosterone is responsible for the stimulation of the anabolic process of skeletal muscle growth, which increases linearly in response to exercise [46,47,48,49,50,51].
Therefore, this study aimed to examine the responses of basketball players during training, competition, and recovery, considering (i) the immune system, i.e., (a) mucosal immunity (human defensins: HNP1 and HBD-1) and (b) differences in exercise-induced leucocyte subset numbers and total leucocytes, and (ii) stress hormones, such as cortisol and testosterone.
We hypothesized that physical activity would increase serum alpha- and beta-defensins, thereby enhancing immune function. This might be useful for the maintenance of older adults’ and athletes’ health.
2. Results
2.1. Evaluation of α- and β-Defensins in Professional Athletes
To determine how intense physical activity influences antimicrobial peptide (AMP) trends, alpha- and beta-defensins (HNP1 and HBD-1, respectively) were evaluated with ELISA (Enzyme-Linked ImmunoSorbent Assay) using the athletes’ sera. The ELISA test showed that levels of beta-defensins were higher between 3 and 12 months compared to 0 months (Figure 1A). We also compared 3 months against 6 and 12 months, which showed a significant increase (Figure 1A), and 6 months against 12 months (Figure 1A). The levels between 6 and 12 months were constant (Figure 1A). The alpha-defensins exhibited a similar trend (Figure 1B). In fact, their levels were higher between 3 and 12 months as compared to 0 months (Figure 1B). However, when we compared 3 months against 6 and 12 months, the levels showed a decrease that remained constant throughout the 6 and 12 months comparison (Figure 1B).
Figure 1.
ELISA assay. (A) Beta-defensin and (B) alpha-defensin levels of 15 professional basketball athletes at 0, 3, 6, and 12 months since the start of a championship competition. The data are expressed as the means ± SDs. Significance was determined by the Student’s t-test: (p < 0.05), ** (p < 0.01), and *** (p < 0.001) represent significance compared to 0 months; # (p < 0.05), (p < 0.01), and ### (p < 0.001) represent significance compared to 3 months.
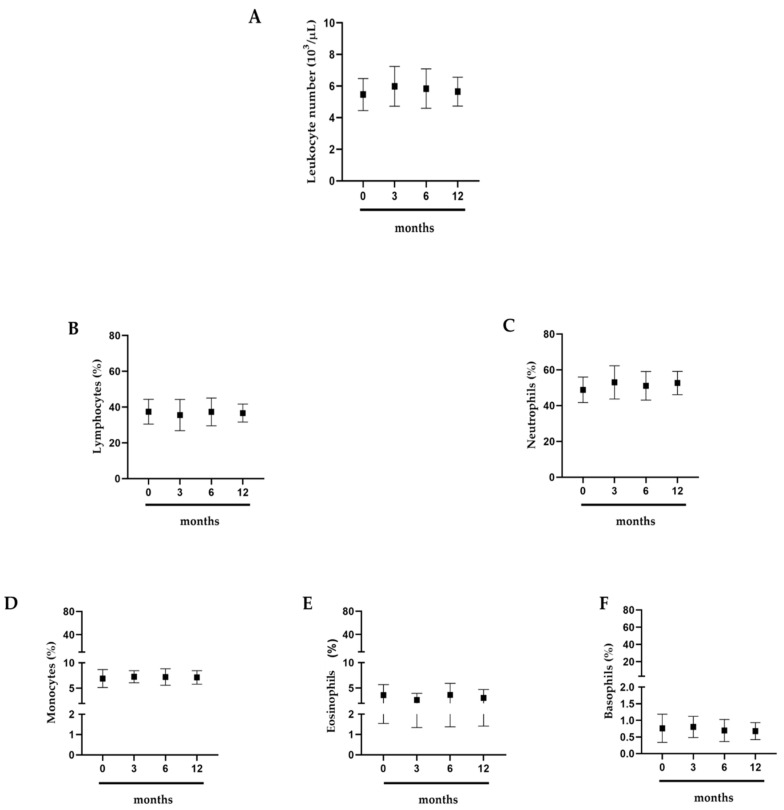
2.2. Effects of Intense Exercise on White Blood Cells
To highlight how prolonged exercise affects athletes’ health, we evaluated the white blood cells of professional basketball athletes. It was interesting to note that leukocytes, lymphocytes, neutrophils, eosinophils, and basophils did not show significant variations (Figure 2A–F).
Figure 2.
White blood cells. (A) Leukocytes; (B) lymphocytes; (C) neutrophils; (D) monocytes; (E) eosinophils; (F) basophils. Assessment of 15 professional basketball athletes at 0, 3, 6, and 12 months. The data are expressed as the means ± SDs. Significance was determined by the Student’s t-test.
2.3. Measurements of Cortisol and Testosterone
To understand how physical activity influences anabolic and catabolic hormone trends, cortisol and testosterone titers were measured. In this analysis, both hormones were observed to increase when compared to 0 months (Figure 3A,B). Essentially, both hormones increased significantly between 0 and 6 months (Figure 3A,B); however, at 12 months, the values returned to baseline levels (Figure 3A,B).
Figure 3.
Hormonal dosages. (A) Cortisol; (B) testosterone. Evaluation of hormones in 15 professional basketball athletes at 0, 3, 6, and 12 months. The data are expressed as the means ± SDs. The significance was determined by the Student’s t-test: * (p < 0.05), (p < 0.01), and *** (p < 0.001) represent significance compared to 0 months; # (p < 0.05), ## (p < 0.01), and ### (p < 0.001) represent significance compared to 3 months; (p < 0.05), (p < 0.01), and $$$ (p < 0.001) represent significance compared to 6 months.
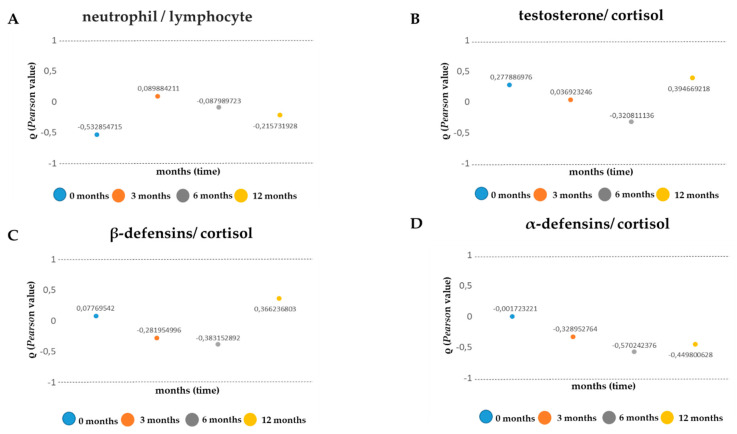
2.4. Comparison of Inflammatory Indices
To shed light on how professional physical activity influences cell/muscle “stress”, we evaluated four inflammatory indices [29,49] by analyzing and comparing neutrophil/lymphocyte ratios, testosterone/cortisol ratios, beta-defensin/cortisol ratios, and alpha-defensin/cortisol ratios. To emphasize the trends of these ratios over time, we used Pearson’s linear correlation coefficient (Table 1). In the analysis conducted, the neutrophil/lymphocyte ratio presented a moderate negative linear correlation in months 0 and 12, while at 3 and 6 months no correlation was observed (Table 1, Figure 4A). Other fascinating data were observed from the testosterone/cortisol ratios, where the two hormones demonstrated a negative linear correlation (Table 1, Figure 4B) at 6 months and a positive correlation at 12 months (Table 1, Figure 4B). For the beta-defensin/cortisol ratios, a negative linearity index was noted (Table 1, Figure 4C) between 3 and 6 months; in addition, at 12 months we noted a moderate positive correlation (Table 1, Figure 4C). Finally, the alpha-defensin/cortisol ratio exhibited a negative correlation between 0 and 12 months (Table 1, Figure 4D).
Table 1.
Pearson’s correlation (ρ) between neutrophils (N), lymphocytes (L), testosterone (T), cortisol (C), beta-defensins (B), and alpha-defensins (A) at different analyzed times. The Pearson index was considered significant for values between +1 and −1.
| Variables | P | |||
|---|---|---|---|---|
| 0 Months | 3 Months | 6 Months | 12 Months | |
| N vs. L | −0.53 | 0.08 | −0.08 | −0.21 |
| T vs. C | 0.28 | 0.04 | −0.32 | 0.39 |
| B vs. C | 0.07 | −0.28 | −0.38 | 0.36 |
| A vs. C | −0.001 | −0.32 | −0.57 | −0.44 |
Figure 4.
Inflammatory indices. (A) testosterone/cortisol ratios; (B) neutrophil/lymphocyte ratios; (C) beta-defensin/cortisol ratios; (D) alpha-defensin/cortisol ratios. Values obtained from the Pearson’s analysis are reported on the y-axis; time is reported on the x-axis.
3. Discussion
Laboratory diagnostics in sports medicine are becoming increasingly important for the assessment and monitoring of athletes’ health [52,53]. Intense and continuous physical exercise, training, and competitions are known to induce metabolic adaptations, particularly in the serum concentrations of numerous biochemical parameters. These modifications reflect the changes that occur in the body in response to the intensity and duration of training exercises, as well as the specific stress of certain muscle groups and motor units during the execution of these exercises. These adaptations translate into alterations of specific parameters in terms of concentration and activity. Therefore, their identification could represent a new method of clinical evaluation.
We aimed to shed light on the biochemical, serological, and hematological parameter changes following exercise. We assessed several parameters, since the response to exercise-induced stress implies a complex involvement of organs and tissues and no studies currently exist in the literature regarding the integration of these different aspects. To make our observations, we collected peripheral blood samples from a group of professional athletes who had given informed consent.
Following our observation of the results obtained, we highlighted that the levels of alpha- and beta-defensins (HNP1 and HBD-1, respectively) increased progressively with training intensification. These antimicrobial peptides have a fundamental role in the human innate immune system; indeed, they are involved in different inflammatory processes that respond to different human pathogens [54,55,56,57,58,59]. Their increase could coincide with athletes’ self-defense adaptations that protect against possible respiratory diseases that could affect them during competition seasons [20,21,22,23,24,25].
This study has shown that in the athletes examined, exercise does not cause alteration in the number of white blood cells. Increases in lymphocytes, neutrophils, monocytes, and basophils that are constant over time are known to act as sentinels for the improper functioning of the immune system or for the presence of an infectious disease that is prolonged and not properly eradicated [3,19,20,21,22,23,24,25].
The adaptations produced by the action of some hormones, such as cortisol and testosterone, have been particularly impressive. These two hormones titers allow the assessment of the athlete’s correct muscle condition. Our data showed that both hormones increase between months 0 and 6. However, the Pearson correlation shed light on the fact that their ratios have a negative linear correlation at 6 months. That is, at 6 months, the increase in cortisol is not directly proportional to the increase in testosterone. Since their increase is not directly proportional, it is possible to speak of a negative linear correlation, which is to say that an increase in testosterone does not correlate to a linear increase in cortisol. These data show a perfect balance between anabolic and catabolic metabolism [41,42,43,44,45,46,47,48,49]. In fact, it is known that increased testosterone levels may induce a reduction in the transforming growth factor beta (TGF-β) signal, which in turn reduces osteoprogenitor cells and increases lean muscle mass [59,60,61,62], thereby increasing anabolic effects. In fact, testosterone is an anabolic hormone (i.e., it binds proteins), thanks to which muscle growth occurs. At the same time, it provides energy to the muscles and accelerates the reconstruction of glycogen after the effort. The synergy of these mechanisms increases the athlete’s lean muscle mass and reduces the fat mass of the muscle.
Our study indicated that during intense and prolonged physical activity, the human body puts in place a series of defense and adaptation mechanisms to combat a prolonged stress state that could be harmful to both the respiratory and muscular systems. It is well known that competitive athletes follow a diet suited to sustaining their intense training schedules [63]. Often, this diet is enriched with food supplements and multivitamins in accordance with the antidoping rules in place. In this scenario, it would be useful to use supplements containing cycled and engineered analogues of alpha- and beta-defensins [63,64,65,66,67,68,69,70,71]. The use of these analogues could support the decreased inflammatory state to which the athlete is subjected, protecting them from any pathologies. In addition, as frequently reported in the literature, nutrition and, therefore, the intestinal microbiota are essential for the correct functionality of the whole body [57,72].
4. Materials and Methods
4.1. Experimental Approach
We evaluated leukocytes, antimicrobial peptides (i.e., alpha- and beta-defensins), cortisol (a catabolic hormone), and testosterone (an anabolic hormone) to evaluate the stresses undergone by professional basketball players and caused by physical exercise during competition season. The study was designed following the recommendations for clinical research contained in the Helsinki Declaration of the World Medical Association, and the protocol was approved by the Ethics Committee of the School of Medicine, University of Naples Federico II, protocol number 200/17.
4.2. Participants
This study examined professional basketball players (n = 15). The participants were all male and were informed about the research and the protocols used. The players had the following physical characteristics, reported as means ± SDs: age of 25 ± 6 years, weight of 92 ± 10 kg, and height of 195 ± 9 cm. None of the subjects smoked, drank alcohol, or consumed drugs known to alter the chemical parameters of the leukocyte or hormonal formula. All subjects followed a similar diet throughout the season and, above all, the same diet during the study. This was monitored continuously by the team doctors. The players followed the same training program, i.e., they trained every day for two sessions, with a morning session consisting of a gym workout for 2 h and an afternoon session consisting of basketball practice for 3 h. This training program was followed daily, except on the days of official games played during the season (two games per week).
4.3. Blood Sampling
Blood samples from competitive athletes were taken at 0 months in the preseason phase, 3 months after the start of the championship, 6 months after the start of the championship, and 12 months after the start of the championship. Leukocyte or hormone concentrations were evaluated using blood samples from the athletes. The parameters analyzed were leukocytes (4.8 × 103 to 10.8 × 103/µL), neutrophils (40–70%), lymphocytes (20–45%), monocytes (3–10%), eosinophils (0–6%), basophils (0–1.5%), cortisol (50–200 ng/mL), and testosterone (300–900 ng/dL). Blood and serum samples were taken in the morning, before training, for all athletes.
4.4. Biochemical Determinations
White blood cell counts were performed using the Siemens Advia 2120i hematology analyzer according to the manufacturer’s recommendations. Sera were analyzed for cortisol and testosterone concentrations by means of immunoassay procedures using the Immulite 2000 analyzer (Cortisol and Testosterone Immunoassay Kit; Siemens Healthineers, Malvern, PA, USA) according to the manufacturer’s recommendations.
4.5. Determination of α- and β-Defensins
Alpha- and beta-defensins were assessed in the participants’ sera using ELISA (Human DEFα1 and Human DEFB1 ELISA Kit; Elabscience, Buckingham, UK) according to the manufacturer’s recommendations. The sera were stored at −80 °C until use. The parameters analyzed were beta defensins (0.03125–2 µg/mL) and alpha defensins (0.03125–2 µg/mL).
4.6. Data Analysis and Statistics
All statistical analyses were performed using GraphPad Prism 8.4.0 (GraphPad Software Inc., La Jolla, CA, USA). Data were expressed as the means ± standard deviations. The Student’s t-test was used to compare the groups, with values of p < 0.05 considered significant. To evaluate the relationships between testosterone and cortisol, alpha-defensin and cortisol, beta-defensin and cortisol, and neutrophils and lymphocytes (to determine whether they could be used as indices of inflammation), Pearson’s linear correlation coefficient was used. Here, a value of +1 corresponded to a perfect positive linear correlation, 0 corresponded to an absence of a linear correlation, and −1 corresponded to a perfect negative linear correlation. In fact, the correlation index is +1 in the presence of a perfect positive linear correlation (i.e., Y = a + bX, b > 0), while it is -1 in the presence of a perfect negative linear correlation (i.e., Y = a + bX, b < 0).
5. Conclusions
The biochemical parameters analyzed in this study were used as indices to evaluate and monitor the physical conditions of athletes at different stages of a sports season in order to protect athletes’ health and also to prevent either the deterioration of athletes’ form or the occurrence of respiratory disease. This study lays the foundations for outlining a panel of specific markers in as much detail as possible, which then can be applied to individual athletes. Obtained results could be reported in a personalized file for each individual athlete, allowing athletic trainers and sports doctors to plan personalized training and recovery programs and, fundamentally, to monitor the health status of athletes in order to monitor the numerous effects induced by intense physical activity.
Acknowledgments
We thank Andrea Piccolo for helpful discussions on statistical analysis and the Pearson correlation. We thank Molly Li (Assistant Editor, MDPI) for helpful discussions on paper organization.
Author Contributions
Data curation, R.P., M.B., C.M. (Cristina Mennitti), L.G., A.F., S.L., M.G.D.B., C.P., R.C., P.S., G.D., D.T., M.C., E.L.C., A.L., C.M. (Cristina Mazzaccara), G.F., B.L., and O.S.; formal analysis, R.P., M.B., C.M. (Critina Mennitti), and O.S.; validation, R.P., M.B., C.M. (Cristina Mennitti), and O.S.; investigation, R.P., M.B., C.M. (Cristina Mennitti), and O.S.; methodology, R.P., M.B., C.M. (Cristina Mennitti), and O.S.; writing—review and editing, R.P., M.B., C.M. (Cristina Mennitti), and O.S.: conceptualization, R.P. and O.S.; supervision, R.P. and O.S.; writing—original draft, R.P., M.B., C.M. (Cristina Mennitti), and O.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.West N.P., Pyne D.B., Renshaw G., Cripps A.W. Antimicrobial peptides and proteins, exercise and innate mucosal immunity. FEMS Immunol. Med. Microbiol. 2006;48:293–304. doi: 10.1111/j.1574-695X.2006.00132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gleeson M. Immune function in sport and exercise. J. Appl. Physiol. 2007;103:693–699. doi: 10.1152/japplphysiol.00008.2007. [DOI] [PubMed] [Google Scholar]
- 3.Walsh N.P., Gleeson M., Shephard R.J., Gleeson M., Woods J.A., Bishop N.C., Fleshner M., Green C., Pedersen B.K., Hoffman-Goetz L., et al. Position statement. Part one: Immune func-tion and exercise. Exerc. Immunol. Rev. 2011;17:6–63. [PubMed] [Google Scholar]
- 4.Moreira A., Delgado L., Moreira P., Haahtela T. Does exercise increase the risk of upper respiratory tract infections? Br. Med. Bull. 2009;90:111–131. doi: 10.1093/bmb/ldp010. [DOI] [PubMed] [Google Scholar]
- 5.Usui T., Yoshikawa T., Orita K., Ueda S.Y., Katsura Y., Fujimoto S., Yoshimura M. Changes in salivary antimicrobial peptides, immunoglobulin A and cortisol after prolonged strenuous exercise. Eur. J. Appl. Physiol. 2011;111:2005–2014. doi: 10.1007/s00421-011-1830-6. [DOI] [PubMed] [Google Scholar]
- 6.Davison G., Allgrove J., Gleeson M. Salivary antimicrobial peptides (LL-37 and alpha-defensins HNP1-3), antimicrobial and IgA responses to prolonged exercise. Eur. J. Appl. Physiol. 2009;106:277–284. doi: 10.1007/s00421-009-1020-y. [DOI] [PubMed] [Google Scholar]
- 7.Lai Y., Gallo R.L. AMPed up immunity: How antimicrobial peptides have multiple roles in immune defense. Trends Immunol. 2009;30:131–141. doi: 10.1016/j.it.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hazlett L., Wu M. Defensins in innate immunity. Cell Tissue Res. 2011;343:175–188. doi: 10.1007/s00441-010-1022-4. [DOI] [PubMed] [Google Scholar]
- 9.Selsted M.E., Ouellette A.J. Mammalian defensins in the antimicrobial immune response. Nat. Immunol. 2005;6:551–557. doi: 10.1038/ni1206. [DOI] [PubMed] [Google Scholar]
- 10.Ganz T., Selsted M.E., Szklarek D., Harwig S.S., Daher K., Bainton D.F., Lehrer R.I. Defensins. Natural peptide antibiotics of human neutrophils. J. Clin. Investig. 1985;76:1427–1435. doi: 10.1172/JCI112120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones D.E., Bevins C.L. Paneth cells of the human small intestine express an antimicrobial peptide gene. J. Biol. Chem. 1992;267:23216–23225. [PubMed] [Google Scholar]
- 12.Jones D.E., Bevins C.L. Defensin-6 mRNA in human Paneth cells: Implications for antimicrobial peptides in host defense of the human bowel. FEBS Lett. 1993;315:187–192. doi: 10.1016/0014-5793(93)81160-2. [DOI] [PubMed] [Google Scholar]
- 13.Wang G. Human antimicrobial peptides and proteins. Pharmaceuticals (Basel) 2014;7:545–594. doi: 10.3390/ph7050545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suarez-Carmona M., Hubert P., Delvenne P., Herfs M. Defensins: “Simple” antimicrobial peptides or broad-spectrum molecules? Cytokine Growth Factor Rev. 2015;26:361–370. doi: 10.1016/j.cytogfr.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Goldman M.J., Anderson G.M., Stolzenberg E.D., Kari U.P., Zasloff M., Wilson J.M. Human beta-defensin-1 Is a Salt-Sensitive Antibiotic in Lung That Is Inactivated in Cystic Fibrosis. Cell. 1997;88:553–560. doi: 10.1016/S0092-8674(00)81895-4. [DOI] [PubMed] [Google Scholar]
- 16.Tesse R., Cardinale F., Santostasi T., Polizzi A., Manca A., Mappa L., Iacoviello G., De Robertis F., Logrillo V.P., Armenio L. Association of β-defensin-1 gene polymorphisms with Pseudomonas aeruginosa airway colonization in cystic fibrosis. Genes Immun. 2008;9:57–60. doi: 10.1038/sj.gene.6364440. [DOI] [PubMed] [Google Scholar]
- 17.Schröder J.M., Harder J. Human beta-defensin-2. Int. J. Biochem. Cell. Biol. 1999;31:645–651. doi: 10.1016/S1357-2725(99)00013-8. [DOI] [PubMed] [Google Scholar]
- 18.Harder J., Bartels J., Christophers E., Schroder J.M. Isolation and characterization of human beta -defensin-3, a novel human inducible peptide antibiotic. J. Biol. Chem. 2001;276:5707–5713. doi: 10.1074/jbc.M008557200. [DOI] [PubMed] [Google Scholar]
- 19.Trochimiak T., Hübner-Woźniak E. Effect of exercise on the level of immunoglobulin a in saliva. Biol. Sport. 2012;29:255–261. doi: 10.5604/20831862.1019662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gleeson M. Mucosal immune responses and risk of respiratory illness in elite athletes. Exerc. Immunol. 2000;6:5–42. [PubMed] [Google Scholar]
- 21.Gleeson M., McDonald W.A., Pyne D.B., Cripps A.W., Francis J.L., Fricker P.A., Clancy R.L. Salivary IgA levels and infection risk in elite swimmers. Med. Sci. Sports Exerc. 1999;31:67–73. doi: 10.1097/00005768-199901000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Gleeson M., Pyne D.B. Special feature for the Olympics: Effects of exercise on the immune system: Exercise effects on mucosal immunity. Immunol. Cell Biol. 2000;78:536–544. doi: 10.1111/j.1440-1711.2000.t01-8-.x. [DOI] [PubMed] [Google Scholar]
- 23.Nieman D.C. Exercise immunology: Future directions for research related to athletes, nutrition, and the elderly. Int. J. Sports Med. 2000;1:S61–S68. doi: 10.1055/s-2000-1453. [DOI] [PubMed] [Google Scholar]
- 24.Jacobs M.R. Emergence of antibiotic resistance in upper and lower respiratory tract infections. Am. J. Manag. Care. 1999;11:651–661. [PubMed] [Google Scholar]
- 25.Wang L.M., Qiao X.L., Ai L., Zhai J.J., Wang X.X. Isolation of antimicrobial resistant bacteria in upper respiratory tract infections of patients. 3 Biotech. 2016;6:166. doi: 10.1007/s13205-016-0473-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scudiero O., Brancaccio M., Mennitti C., Laneri S., Lombardo B., De Biasi M.G., De Gregorio E., Pagliuca C., Colicchio R., Salvatore P., et al. Human Defensins: A Novel Approach in the Fight against Skin Colonizing Staphylococcus aureus. Antibiotics. 2020;9:198. doi: 10.3390/antibiotics9040198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olvera D.P.R., Cabello Gutiérrez C. Multifunctional Activity of the β-Defensin-2 during Respiratory Infections. Immune Response Act. 2018 doi: 10.5772/intechopen.80611. [DOI] [Google Scholar]
- 28.Supp D.M., Gardner J., Klingenberg J.M., Neely A.N. Antibiotic resistance in clinical isolates of Acinetobacter baumannii, Pseudomonas aeruginosa, and Staphylococcus aureus does not impact sensitivity to human beta defensin 4. Burns. 2009;35:949–955. doi: 10.1016/j.burns.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 29.Sherman H., Chapnik N., Froy O. Albumin and amino acids upregulate the expression of human beta-defensin 1. Mol. Immunol. 2006;43:1617–1623. doi: 10.1016/j.molimm.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 30.Gałązka-Franta A., Jura-Szołtys E., Smółka W., Gawlikcorresponding R. Upper Respiratory Tract Diseases in Athletes in Different Sports Disciplines. J. Hum. Kinet. 2016;53:99–106. doi: 10.1515/hukin-2016-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pyne D.B. Regulation of neutrophil function during exercise. Sports Med. 1994;17:245–258. doi: 10.2165/00007256-199417040-00005. [DOI] [PubMed] [Google Scholar]
- 32.Peake J., Suzuki K. Neutrophil activation, antioxidant supplements and exercise-induced oxidative stress. Exerc. Immunol. Rev. 2004;10:129–141. [PubMed] [Google Scholar]
- 33.Khanfer R., Phillips A.C., Carroll D., Lord J.M. Altered human neutrophil function in response to acute psychological stress. Psychosom. Med. 2010;72:636–640. doi: 10.1097/PSY.0b013e3181e7fae8. [DOI] [PubMed] [Google Scholar]
- 34.Zahorec R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl. Lek. Listy. 2001;102:5–14. [PubMed] [Google Scholar]
- 35.Greenham G., Buckley J.D., Garrett J., Eston R., Norton K. Biomarkers of Physiological Responses to Periods of Intensified, Non-Resistance-Based Exercise Training in Well-Trained Male Athletes: A Systematic Review and Meta-Analysis. Sports Med. 2018;48:2517–2548. doi: 10.1007/s40279-018-0969-2. [DOI] [PubMed] [Google Scholar]
- 36.Anane L.H., Edwards K.M., Burns V.E., Drayson M.T., Riddell N.E., van Zanten J.J., Wallace G.R., Mills P.J., Bosch J.A. Mobilization of gammadelta T lymphocytes in response to psychological stress, exercise, and beta-agonist infusion. Brain Behav. Immun. 2009;23:823–829. doi: 10.1016/j.bbi.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 37.Mohr M., Draganidis D., Chatzinikolaou A., Barbero-Álvarez J.C., Castagna C., Douroudos I., Avloniti A., Margeli A., Papassotiriou I., Flouris A.D., et al. Muscle damage, inflammatory, immune and performance responses to three football games in 1 week in competitive male players. Eur. J. Appl. Physiol. 2016;116:179–193. doi: 10.1007/s00421-015-3245-2. [DOI] [PubMed] [Google Scholar]
- 38.de Kloet E.R., Joëls M., Holsboer F. Stress and the brain: From adaptation to disease. Nat. Rev. Neurosci. 2005;6:463–475. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- 39.Duclos M., Gouarne C., Bonnemaison D. Acute and chronic effects of exercise on tissue sensitivity to glucocorticoids. J. Appl. Physiol. (1985) 2003;94:869–875. doi: 10.1152/japplphysiol.00108.2002. [DOI] [PubMed] [Google Scholar]
- 40.Elenkov I.J., Chrousos G.P. Stress Hormones, Th1/Th2 patterns, Pro/Anti-inflammatory Cytokines and Susceptibility to Disease. Trends Endocrinol. Metab. 1999;10:359–368. doi: 10.1016/S1043-2760(99)00188-5. [DOI] [PubMed] [Google Scholar]
- 41.Ronsen O., Haug E., Pedersen B.K., Bahr R. Increased neuroendocrine response to a repeated bout of endurance exercise. Med. Sci. Sports Exerc. 2001;33:568–575. doi: 10.1097/00005768-200104000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Tomita T., Nagase T., Ohga E., Yamaguchi Y., Yoshizumi M., Ouchi Y. Molecular mechanisms underlying human beta-defensin-2 gene expression in a human airway cell line (LC2/ad) Respirology. 2002;7:305–310. doi: 10.1046/j.1440-1843.2002.00415.x. [DOI] [PubMed] [Google Scholar]
- 43.McDermott A.M., Redfern R.L., Zhang B., Pei Y., Huang L., Proske R.J. Defensin expression by the cornea: Multiple signalling pathways mediate IL-1beta stimulation of hBD-2 expression by human corneal epithelial cells. Investig. Ophthalmol. Vis. Sci. 2003;44:1859–1865. doi: 10.1167/iovs.02-0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Starner T.D., Agerberth B., Gudmundsson G.H., McCray P.B., Jr. Expression and activity of beta-defensins and LL-37 in the developing human lung. J. Immunol. 2005;174:1608–1615. doi: 10.4049/jimmunol.174.3.1608. [DOI] [PubMed] [Google Scholar]
- 45.Kuoppasalmi K., Adlercreutz H. Interaction between catabolic and anabolic steroid hormones in muscular exercise. In: Fotherby K., Pal S.B., editors. Exercise Endocrinology. De Gruyter; Berlin, Germany: 1984. pp. 65–98. [Google Scholar]
- 46.Urhausen A., Kindermann W. The endocrine system in overtraining. In: Warren M.P., Constantini N.W., editors. Sports Endocrinology. Humana Press; Totowa, NJ, USA: 2000. pp. 347–370. [Google Scholar]
- 47.Budgett R. Fatigue and underperformance in athletes: The overtraining syndrome. Br. J. Sports Med. 1998;32:107–110. doi: 10.1136/bjsm.32.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hazar S., Hazar M., Korkmaz S., Bayil S., Gürkan A.C. The effect of graded maximal aerobic exercise on some metabolic hormones, muscle damage and some metabolic end products in sportsmen. Sci. Res. Essays. 2011;6:1337–1343. [Google Scholar]
- 49.Karacabey K., Peker I., Saygın O., Cıloglu F., Ozmerdivenli R., Bulut V. University Effect of acute aerobic and anaerobic exercise on humoral immune factors in elite athletes. Biotechnol. Biotechnol. Equip. 2014;19:175–180. doi: 10.1080/13102818.2005.10817177. [DOI] [Google Scholar]
- 50.Thomas N.E., Leyshon A., Hughes M.G., Davies B., Graham M., Baker J.S. The effect of anaerobic exercise on salivary cortisol, testosterone and immunoglobulin (A) in boys aged 15–16 years. Eur. J. Appl. Physiol. 2009;107:455–461. doi: 10.1007/s00421-009-1146-y. [DOI] [PubMed] [Google Scholar]
- 51.Martínez A.C., Seco Calvo J., Tur Marí J.A., Abecia Inchaurregui L.C., Orella E.E., Biescas A.P. Testosterone and cortisol changes in professional basketball players through a season competition. J. Strength Cond. Res. 2010;4:1102–1108. doi: 10.1519/JSC.0b013e3181ce2423. [DOI] [PubMed] [Google Scholar]
- 52.Lombardo B., Izzo V., Terracciano D., Ranieri A., Mazzaccara C., Fimiani F., Cesaro A., Gentile L., Leggiero E., Pero R., et al. Laboratory medicine: Health evaluation in elite athletes. Clin. Chem. Lab. Med. 2019;57:1450–1473. doi: 10.1515/cclm-2018-1107. [DOI] [PubMed] [Google Scholar]
- 53.Zebisch A., Schulz E., Grosso M., Lombardo B., Acierno G., Sill H., Iolascon A. Identification of a novel variant of epsilon-gamma-delta-beta thalassemia highlights limitations of next generation sequencing. Am. J. Hematol. 2015;90:E52–E54. doi: 10.1002/ajh.23913. [DOI] [PubMed] [Google Scholar]
- 54.Pero R., Angrisano T., Brancaccio M., Falanga A., Lombardi L., Natale F., Laneri S., Lombardo B., Galdiero S., Scudiero O. Beta-defensins and analogs in Helicobacter pylori infections: mRNA expression levels, DNA methylation, and antibacterialactivity. PLoS ONE. 2019;14:e0222295. doi: 10.1371/journal.pone.0222295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pero R., Brancaccio M., Laneri S., De Biasi M.G., Lombardo B., Scudiero O. A Novel View ofHuman Helicobacter pylori Infections: Interplay between Microbiota and Beta-Defensins. Biomolecules. 2019;9:237. doi: 10.3390/biom9060237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pero R., Coretti L., Nigro E., Lembo F., Laneri S., Lombardo B., Daniele A., Scudiero O. β-Defensins in the Fight against Helicobacter pylori. Molecules. 2017;22:424. doi: 10.3390/molecules22030424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Colavita I., Nigro E., Sarnataro D., Scudiero O., Granata V., Daniele A., Zagari A., Pessi A., Salvatore F. Membrane protein 4F2/CD98 is a cell surface receptor involved in the internalization and trafficking of human β-Defensin 3 in epithelial cells. Chem. Biol. 2015;22:217–228. doi: 10.1016/j.chembiol.2014.11.020. [DOI] [PubMed] [Google Scholar]
- 58.Girolami F., Frisso G., Benelli M., Crotti L., Iascone M., Mango R., Mazzaccara C., Pilichou K., Arbustini E., Tomberli B., et al. Contemporary genetic testing in inherited cardiac disease: Tools, ethical issues, and clinical applications. J. Cardiovasc. Med. (Hagerstown) 2018;19:1–11. doi: 10.2459/JCM.0000000000000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Detta N., Frisso G., Limongelli G., Marzullo M., Calabrò R., Salvatore F. Genetic analysis in a family affected by sick sinus syndrome may reduce the sudden death risk in a young aspiring competitive athlete. Int. J. Cardiol. 2014;170:e63–e65. doi: 10.1016/j.ijcard.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 60.Kraemer W.J., Ratamess N.A., Hymer W.C., Nindl B.C., Fragala M.S. Growth Hormone(s), Testosterone, Insulin-Like Growth Factors, and Cortisol: Roles and Integration for Cellular Development and Growth with Exercise. Front. Endocrinol. (Lausanne) 2020;11:33. doi: 10.3389/fendo.2020.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Querques F., Cantilena B., Cozzolino C., Esposito M.T., Passaro F., Parisi S., Lombardo B., Russo T., Pastore L. Angiotensin receptor I stimulates osteoprogenitor proliferation through TGFβ-mediated signaling. J. Cell. Physiol. 2015;230:1466–1474. doi: 10.1002/jcp.24887. [DOI] [PubMed] [Google Scholar]
- 62.Ragozzino E., Brancaccio M., Di Costanzo A., Scalabrì F., Andolfi G., Wanderlingh L.G., Patriarca E.J., Minchiotti G., Altamura S., Varrone F., et al. 6-Bromoindirubin-3’-oxime intercepts GSK3 signaling to promote and enhance skeletal muscle differentiation affecting miR-206 expression in mice. Sci. Rep. 2019;9:18091. doi: 10.1038/s41598-019-54574-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thomas D.T., Erdman K.A., Burke L.M. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and Athletic Performance. J. Acad. Nutr. Diet. 2016;116:501–528. doi: 10.1016/j.jand.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 64.Peschel A., Jack R.W., Otto M., Collins L.V., Staubitz P., Nicholson G., Kalbacher H., Nieuwenhuizen W.F., Jung G., Tarkowski A., et al. Staphylococcus aureus resistance to human defensins and evasion of neutrophil killing via the novel virulence factor MprF is based on modification of membrane lipids with L-lysine. J. Exp. Med. 2001;193:1067–1076. doi: 10.1084/jem.193.9.1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kristian S.A., Durr M., van Strijp J.A., Neumeister B., Peschel A. MprF-mediated lysinylation of phospholipids in Staphylococcus aureus leads to protection against oxygen-independent neutrophil killing. Infect. Immun. 2003;71:546–549. doi: 10.1128/IAI.71.1.546-549.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Friedman L., Alder J.D., Silverman J.A. Genetic changes that correlate with reduced susceptibility to daptomycin in Staphylococcus aureus. Antimicrob. Agents Chemother. 2006;50:2137–2145. doi: 10.1128/AAC.00039-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jones T., Yeaman M.R., Sakoulas G., Yang S.J., Proctor R.A., Sahl H.G., Schrenzel J., Xiong Y.Q., Bayer A.S. Failures in clinical treatment of Staphylococcus aureus Infection with daptomycin are associated with alterations in surface charge, membrane phospholipid asymmetry, and drug binding. Antimicrob. Agents Chemother. 2008;52:269–278. doi: 10.1128/AAC.00719-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Falanga A., Nigro E., De Biasi M.G., Daniele A., Morelli G., Galdiero S., Scudiero O. Cyclic Peptides as Novel Therapeutic Microbicides: Engineering of Human Defensin Mimetics. Molecules. 2017;20:1217. doi: 10.3390/molecules22071217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Scudiero O., Nigro E., Cantisani M., Colavita I., Leone M., Mercurio F.A., Galdiero M., Pessi A., Daniele A., Salvatore F., et al. Design and activity of a cyclic mini-β-defensin analog: A novel antimicrobial tool. Int. J. Nanomed. 2015;10:6523–6539. doi: 10.2147/IJN.S89610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nigro E., Colavita I., Sarnataro D., Scudiero O., Zambrano G., Granata V., Daniele A., Carotenuto A., Galdiero S., Folliero V., et al. An ancestral host defence peptide within human β-defensin 3 recapitulates the antibacterial and antiviral activity of the full-length molecule. Sci. Rep. 2015;5:18450. doi: 10.1038/srep18450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Falanga A., Valiante S., Galdiero E., Franci G., Scudiero O., Morelli G., Galdiero S. Dimerization in tailoring uptake efficacy of the HSV-1 derived membranotropic peptide gH625. Sci. Rep. 2017;7:9434. doi: 10.1038/s41598-017-09001-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sommese L., Pagliuca C., Avallone B., Ippolito R., Casamassimi A., Costa V., Colicchio R., Cerciello R., D’Armiento M., Scarpato M., et al. Evidence of Bacteroides fragilis protection from Bartonella henselae-induced damage. PLoS ONE. 2012;7:e49653. doi: 10.1371/journal.pone.0049653. [DOI] [PMC free article] [PubMed] [Google Scholar]