Abstract
Dengue is a growing problem in Hanoi, with cyclical epidemics of increasing frequency and magnitude. In June 2019, we conducted a cross-sectional survey using mixed methods to investigate how inhabitants of Hanoi perceive and respond to the risk of mosquito-borne diseases (MBD). A total of 117 participants recruited using a stratified random sampling method were interviewed in three districts of Hanoi. Knowledge and practices (KP) regarding MBDs were assessed using a pre-tested questionnaire. Inferential statistics were used to identify factors associated with KP scores and describe the relationship between variables. Additionally, a “risk-mapping” exercise was conducted in a subsample through semi-structured interviews and analyzed qualitatively and quantitatively using the System Effects platform. Factors significantly associated with knowledge scores were education and family history of MBDs. While knowledge and practice scores were found to be positively correlated in the statistical analysis, this was not corroborated by our observations on the field. The results also revealed gaps in knowledge about MBDs and vectors and highlighted a general feeling of powerlessness which prevented the adoption of protective behaviors. Therefore, educational interventions which provide concrete tools to empower communities should have a positive impact on improving vector control.
Keywords: dengue, vector control, Vietnam, knowledge and practices (KPs), system network analysis
1. Introduction
With 3.97 billion people living in at-risk areas [1], dengue is the most widespread mosquito-borne disease. Recent decades have witnessed a dramatic re-emergence of dengue fever and dengue hemorrhagic fever worldwide—with South East Asia accounting for more than 70% of cases [2], Vietnam is among the countries bearing the highest burden [3,4]. In Hanoi city, rapid urbanization and massive population growth, along with insufficient mosquito control, have contributed to the increase in dengue vector population, leading to more frequent and cyclical epidemics [5,6]. The largest recorded outbreak occurred in 2017, when 36,354 cases and 7 deaths were reported [7].
As potential vaccines are still undergoing development, dengue prevention mainly relies on vector control [5,8]. While insecticide-based methods are facing numerous issues such as increasing resistance in Aedes sp. or environmental toxicity, researchers have been exploring alternative approaches often focusing on environmental management. Numerous studies have highlighted the critical importance of community participation in the elimination of breeding sites and emphasized the need for information and education to promote the adoption of protective practices [9,10,11,12,13,14,15,16,17,18,19,20]. However, despite increased risk communication efforts by health authorities and NGOs, control interventions are still limited by a lack of engagement by local authorities and communities in disease prevention. Achieving behavioral changes remains a key challenge that requires a deep understanding of local knowledge and practices to design and implement effective and sustainable vector control strategies.
This study aimed to investigate risk perception and prevention practices among inhabitants of Hanoi in order to identify barriers to the adoption of vector control measures. This will help inform future educational interventions.
2. Material and Methods
2.1. Study Design
This is a cross-sectional study relying on mixed methods. It was conducted in the vector season for 6 days between 10 and 27 June 2019. It included a knowledge and practices (KPs) survey and a mapping exercise to further investigate the barriers to vector control.
2.2. Study Area and Sample
Hanoi is the capital and second most populous city in Vietnam, with 7.8 million inhabitants, resulting in a density of 2239 inhabitants/km2, and has one of the highest urbanization rates in Asia [9,21]. Hanoi city is divided into 12 urban and peri-urban districts and 18 rural districts. For the aim of this study, one urban (Ba Dinh), one peri-urban (Ha Dong) and one rural district (Chuong My) were purposely chosen. In each district, four communes were identified using randomly generated GPS points and 120 households were selected for the KP study employing a stratified random sampling method. Participants in the mapping exercise were sampled from among respondents to the KP study using a convenience sampling procedure.
2.3. Ethical Approval
This study received ethics approval from the Royal Veterinary College (URN SR2019-0241) and Hanoi University of Public Health (280/2019/YTCC-HD3). Informed consent was obtained from the respondents before initiation of the survey. All participants had the opportunity to withdraw themselves from the study at any point. Data from the questionnaires was anonymized using ID numbers and encrypted on the servers of the London School of Hygiene and Tropical Medicine, London.
2.4. KP Questionnaire
A questionnaire was developed in Open Data Kit (https://getodk.org) and pre-tested to ascertain comprehensibility. Minor revisions were made afterwards. The questionnaire was divided into three sections: the first part aimed to collect the respondent’s demographic characteristics; the second included eight items assessing knowledge about MBD causes, symptoms, risk factors, and vector biology and three items assessing usual protection practices; the third asked about family history of MBDs and sources of health information. The questionnaire was administered through face-to-face interviews. Questions about knowledge were awarded one point per correct answer and questions about practices were awarded one point per protective behavior.
2.5. Mapping Exercise
A mapping exercise was conducted through semi-structured interviews for system effects modelling [22]. Participants were provided a template with the focus question “Why do I get bitten by mosquitoes?”. They were asked to write down the factors they thought were related to the risk of getting bitten and indicate the connections between them by arrows. This resulted in directed graphs representing a network of factors centered on the focus question. The exercise was pre-tested using different framing of the focus question in order to assess comprehensibility and refine the formulation.
2.6. Statistical Analysis
Descriptive statistics were used to analyze respondents’ demographic characteristics. The nature of the data distribution was assessed using the Kolmogorov–Smirnov test. Mann–Whitney U tests, Kruskal Wallis tests and negative binomial regression were used to identify factors associated with KP scores, while Spearman’s rho was used to describe the relationship between K and P scores. Categorical variables were expressed as percentages, continuous variables as the mean ± standard deviation and discrete variables as the median ± interquartile range (IQR). A p-value < 0.05 was taken as significant for inferential statistics. Factors with a p-value > 0.1 in univariate analysis were not included in the negative binomial model. All analyses were performed using STATA 15.0.
2.7. System Network Analysis
Individual graphs constructed during the mapping exercise were replicated on the System Effects platform (https://systemeffects.com/#/admin) developed by Luke Craven, Northumbria University, and translated into adjacency matrices [22]. Language and concepts of the determinants were homogenized in order to condense individual matrices into one aggregated adjacency matrix which was used to generate a directed network graph in Gephi (https://gephi.org). This graph was visually explored to investigate the relationship between factors and identify potential barriers perceived by the community. Additionally, measures of centrality and ranking of determinants by in- and outdegree were used to identify those with the highest connectivity within the network.
3. Results
3.1. Demographics
A total of 117 questionnaires were completed. Socio-demographic characteristics of the respondents are presented in Table 1. Of the 117 respondents, 57.3% were females and 43.7% were males; the mean age was 52.13 ± 13.95, ranging from 18 to 83. In total, 86.3% had at least secondary education. The most common occupation was farming (34.2%) and 22.2% were retired.
Table 1.
Socio-demographic profile of participants.
| Characteristic | % (N = 117) |
|---|---|
| Gender | |
| Male | 42.7 (50) |
| Female | 57.3 (67) |
| Age (Mean ± SD) | 52.13 ± 13.95 |
| 18–39 | 20.5 (24) |
| 40–49 | 23.9 (28) |
| 50–59 | 24.8 (29) |
| 60+ | 30.8 (36) |
| Education | |
| Primary school | 13.7 (16) |
| Secondary school | 34.2 (40) |
| High school | 34.2 (40) |
| College/University | 17.9 (21) |
| Occupation | |
| Unemployed | 4.3 (5) |
| Farmer | 34.2 (40) |
| Worker/Seller | 17.1 (20) |
| Public or private services | 11.1 (13) |
| Self-employed | 9.4 (11) |
| Retired | 22,2 (26) |
| Student | 1.7 (2) |
| Family Member Diagnosed with Dengue | |
| Yes | 9.4 (11) |
| No | 90.6 (106) |
3.2. Assessment of Knowledge
The median score for knowledge was 7 ± 4 (med ± IQR) ranging from 0 to 18. The proportions of answers to selected questions are shown in Table 2. The majority of respondents were aware of dengue (82.1%). However, 33.3% did not know any symptoms of MBDs. Symptoms frequently mentioned included fever (61.5%), hemorrhage (45.3%) and rash (14.5%). Most respondents recognized polluted (59.8%) or stagnant water collections (62.4%) as potential mosquitoe-breeding sites but only 1.7% also mentioned clean water collections, which are preferred by Aedes sp. [6]. In total, 76.9% correctly identified either summer or rainy season as high-risk periods. The main source of health information was television (65.8%), followed by local public communication by loudspeaker (36.8%). In contrast, health workers (9.4%) and social media (3.4%) seemed to play a minor role in informing about MBDs.
Table 2.
Proportion of responses to various questions about knowledge.
| Question | % (N = 117) |
|---|---|
| Which Disease(s) Transmitted by Mosquitoes Have you Heard About? | |
| Don’t know any | 12.8 (15) |
| Dengue | 82.1 (96) |
| Japanese encephalitis | 0.9 (1) |
| Zika | 1.7 (2) |
| Malaria | 15.4 (18) |
| What Symptoms of MBDs do You Know? * | |
| Don’t know any | 33.3 (39) |
| High fever | 61.5 (72) |
| Muscle pain | 4.3 (5) |
| Nausea/vomiting | 2.6 (3) |
| Severe headache | 4.3 (5) |
| Rash | 14.5 (17) |
| Hemorrhage | 45.3 (53) |
| What do You Think Can Increase the Risk of Getting Infected with MBDs? * | |
| Don’t know | 46.2 (54) |
| Warm and wet season | 36.8 (43) |
| High population density | 1.7 (2) |
| Stagnant water | 28.2 (33) |
| Livestock keeping | 16.2 (19) |
| Can You List Mosquito Breeding Sites? * | |
| Don’t know any | 6.0 (7) |
| Clean water collection | 1.7 (2) |
| Drain/polluted water | 59.8 (70) |
| Stagnant water containers | 62.4 (73) |
| Tires | 5.1 (6) |
| Water tanks, jars or buckets | 25.6 (30) |
| Vase | 6.0 (7) |
| Bonsai rockery | 6.0 (7) |
| Garbage/rubbish | 2.6 (3) |
| Which Season do You Think is Most at Risk for MBDs? | |
| Spring | 18.8 (22) |
| Summer | 51.3 (60) |
| Autumn | 2.6 (3) |
| Winter | 0.9 (1) |
| No difference | 0.9 (1) |
| Rainy season | 25.6 (30) |
* more than one answer can be reported.
3.3. Assessment of Practices
The median score for practices was 3 ± 1 (med ± IQR), ranging from 0 to 7. The proportions of various preventive methods reported by the participants are shown in Table 3. The most commonly used were bed nets (83.8%) and insecticides (65.8%). When asked about the frequency of elimination of both natural and domestic breeding sites such as water containers, discarded tires and various wastes, 76.1% reported eliminating breeding sites at least weekly and 49.6% daily. Personal protective measures such as coils, repellents and covering clothing were rarely mentioned.
Table 3.
Proportion of responses to various questions about practices.
| Question | % (N = 117) |
|---|---|
| Which Methods do You Use to Prevent Yourself and Your Family from Getting Infected with MBDs? * | |
| Don’t use any | 0.9 (1) |
| Screening of doors/windows | 0.9 (1) |
| Mosquito repellent creams/liquid | 16.2 (19) |
| Mosquito nets | 83.8 (98) |
| Electric rackets | 35.9 (42) |
| Mosquito coils/Incense sticks | 2.6 (3) |
| Covering clothes | 3.4 (4) |
| Keeping lids on water tanks | 3.4 (4) |
| Use of chemicals in water containers | 4.3 (5) |
| Anti-mosquito products (e.g., insecticides) | 65.8 (77) |
| Elimination of breeding sites | 44.4 (52) |
| Fish in water containers | 6.8 (8) |
| Mosquito traps inside home | 12.8 (15) |
| How Often do You Remove Mosquito Breeding Sites? | |
| Never | 0.9 (1) |
| Once in several months | 11.1 (13) |
| Once per month | 1.7 (2) |
| 2–3 times per month | 6.8 (8) |
| Once a week | 6.8 (8) |
| 2–3 times per week | 19.7 (23) |
| Daily | 49.6 (58) |
| Only after raining | 3.4 (4) |
* more than one answer can be reported.
3.4. Association Between KP Scores and Demographic Variables
Results of the statistical analyses are presented in Table 4. Factors with a p-value < 0.1 in univariate analysis were further assessed using binomial regression to control for confounding. Education (p-value = 0.001) and family history of MBDs (p-value = 0.04) were the two factors found to be significantly associated with knowledge scores. No factor was found to be associated with practices.
Table 4.
Knowledge (K) and practice (P) scores with respect to demographics.
| Variable | K Score 7 ± 4 | p-Value (Univariable) |
p-Value (Multivariable) |
P Score 3 ± 1 | p-Value (Univariable) |
p-Value (Multivariable) |
|---|---|---|---|---|---|---|
| Gender * | ||||||
| Male | 8 ± 3 | 0.138 | - | 4 ± 3 | 0.610 | - |
| Female | 7 ± 5 | 3 ± 2 | ||||
| Age ** | ||||||
| 18–39 | 7 ± 5.5 | 0.429 | - | 3 ± 2 | 0.697 | - |
| 40–49 | 7 ± 3.5 | 3 ± 2 | ||||
| 50–59 | 8 ± 6 | 3 ± 2 | ||||
| 60+ | 7.5 ± 5 | 3.5 ± 2 | ||||
| District ** | ||||||
| Chuong My | 7 ± 4 | 0.065 | 0.092 | 3 ± 2 | 0.019 | 0.142 |
| Ha Dong | 8 ± 5 | 4 ± 2 | ||||
| Ba Dinh | 8 ± 3 | 4 ± 2 | ||||
| Education ** | ||||||
| Primary school | 6 ± 5 | 0.003 | 0.001 | 3 ± 2 | 0.041 | 0.233 |
| Secondary school | 7 ± 3.5 | 3 ± 2.5 | ||||
| High school | 8.5 ± 4 | 4 ± 2 | ||||
| College/University | 8 ± 4 | 3 ± 2 | ||||
| Occupation** | ||||||
| Unemployed | 6 ± 1 | 0.022 | 0.396 | 3 ± 2 | 0.003 | 0.319 |
| Farmer | 7 ± 4.5 | 3 ± 2 | ||||
| Worker/Seller | 7 ± 2.5 | 3 ± 0.5 | ||||
| Public or private services | 9 ± 5 | 5 ± 2 | ||||
| Self-employed | 8 ± 6 | 5 ± 3 | ||||
| Retired | 9 ± 5 | 4 ± 2 | ||||
| Student | 3.5 ± 1 | 2 ± 4 | ||||
| Family member diagnosed with dengue * | ||||||
| Yes | 12 ± 6 | 0.047 | 0.050 | 4 ± 1 | 0.032 | 0.188 |
| No | 7 ± 0.4 | 3 ± 1 |
* Mann–Whitney U test; ** Kruskal–Wallis test; Note: Data are presented as the median ± interquartile range.
3.5. Correlation Between Knowledge and Practices
Spearman’s rank correlation indicated a strong positive correlation between knowledge and practices (Spearman’s rho = 0.6161, p < 0.001).
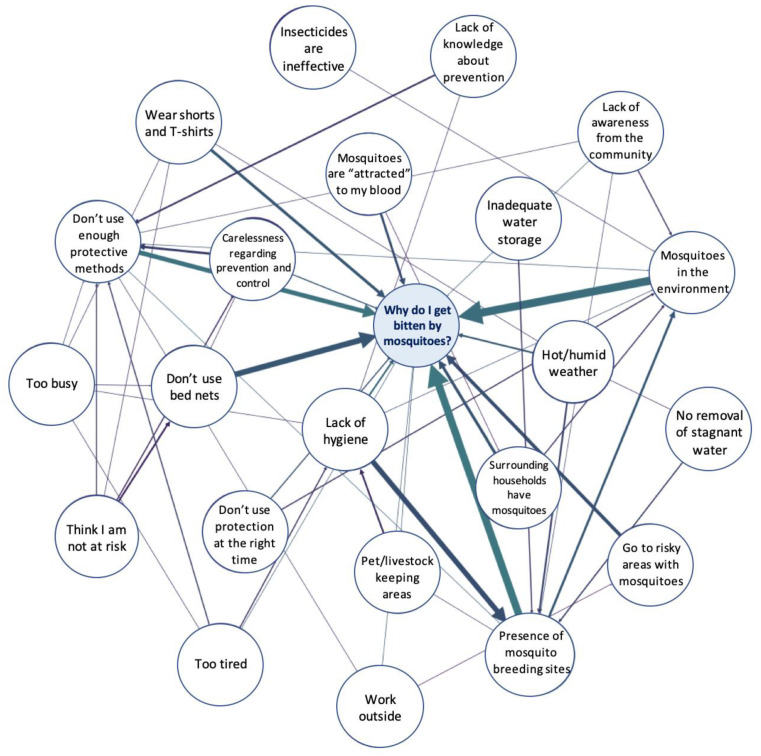
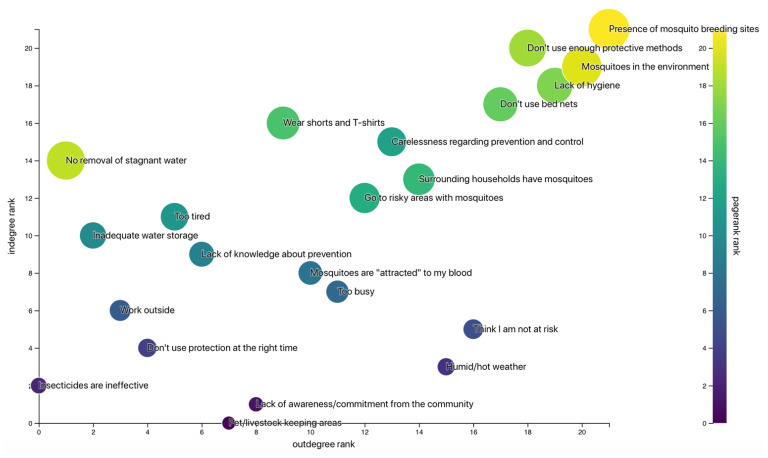
3.6. System Network Analysis
In total, 31 individual graphs were constructed during semi-structured interviews and aggregated into one graph representing the participants’ perception of risk factors for getting bitten by mosquitoes (Figure 1). In addition to its visual exploration, degree and centrality measures presented in Table 5 and Figure 2 showed that the most influential factors identified by the participants were the presence of breeding sites in the environment, the lack of protective measures and the lack of hygiene. Factors related to the lack of protection included misuse of bed nets, poor knowledge about prevention, low risk perception and an attitude of negligence. Overall, our discussions with the participants highlighted a fatalistic attitude regarding disease control: while a majority believed they were at risk of getting infected, they perceived the presence of mosquitoes in the environment as something natural and did not think they could have control over it. Most of them did not feel responsible for eliminating breeding sites and blamed the neighboring households for not performing doing so properly. Additionally, some participants believed mosquitoes could not bite during the day and therefore neglected to use bed nets when sleeping at noontime.
Figure 1.
Aggregated map of determinants of mosquito control in households in Hanoi, Vietnam. The thickness of each edge is proportional to its weight, i.e., the number of participants who identified this link.
Table 5.
Network statistics of key determinants.
| Factor | Weighted Indegree | Weighted Outdegree | Eigencentrality | PageRank |
|---|---|---|---|---|
| Presence of mosquito breeding sites | 20 | 17 | 0.525666 | 0.098047 |
| Do not use enough protective methods | 14 | 10 | 0.065081 | 0.064626 |
| Lack of hygiene | 7 | 13 | 0.035786 | 0.043412 |
| Do not use bed nets | 5 | 10 | 0.039116 | 0.032595 |
Figure 2.
Ranking of determinants by in- and outdegree. Circles are sized according to the PageRank value of each factor.
4. Discussion
Our study highlighted gaps in knowledge of inhabitants of Hanoi about dengue disease and vectors. Although most of the surveyed population were aware of dengue, one-third of the respondents were unable to give details of any symptoms and most of the remaining respondents only mentioned fever. This is likely to contribute to underestimating the occurrence of dengue fever and result in people not seeking adequate care. Mistaken beliefs also resulted in improper protective behaviors and limited use of personal protection, with a minority of respondents being aware that mosquitoes could bite during the day and reproduce in clean water collections, which could possibly reflect a confusion with the malaria vector Anopheles sp. A previous study conducted in Laos in 2009 revealed that one-third of respondents believed dengue and malaria were transmitted by the same vector and could not differentiate between the two diseases [23]. This misconception could contribute to the implementation of inappropriate Aedes control measures. Our results also suggested limited engagement in spreading health information by health workers.
In agreement with previous studies, we found the level of education and history of MBDs to be associated with knowledge [21,24,25]. Unlike most of those studies, we also found a positive correlation between knowledge and practices. However, this was contradicted by our observations in the field: although almost half of the participants reported eliminating breeding sites daily, we were able to collect mosquito larvae on most household premises (results not shown), particularly in rural and peri-urban areas, where the presence of rubbish and tires provided multiple breeding sites. This result is therefore likely to be affected by declaration bias. The influence of knowledge on the adoption of preventive behaviors has been inconsistently described in the scientific literature, with the majority of studies failing to demonstrate any link between a community’s knowledge and better practices [25,26,27,28]. Knowledge does not always translate into more adequate behaviors, and risk perception has been shown to be a key component of the adoption of protective practices. A study in Malawi has shown for example that showing freshly captured mosquitoes to participants was more effective than educational leaflets in improving their understanding of the risk and increasing the use of bed nets [29].
The “risk-mapping” exercise allowed us to better understand the perception of risk and barriers preventing the implementation of protective measures. To our knowledge, this is the first time that system effects modelling was employed to explore the factors related to the perceived risk and prevention of mosquito bites. Overall, it highlighted a fatalistic attitude towards disease control combined with a lack of personal responsibility. The majority of participants did not believe that they have control over the risk and perceived the presence of mosquitoes in the environment as inevitable. This corroborates health-belief models, which have shown that perception of self-efficacy is a crucial component of the translation of risk perception to a concrete preventive behavior [28,30]. This can also be related to the findings of a previous study in Martinique, which interpreted the participants’ reluctance to apply dengue prevention despite a good risk perception as the result of a “normalization” process and questioned the effectiveness of risk communication for community mobilization in endemic areas [28]. In addition, most participants blamed their neighbors or health authorities for improper management of breeding sites rather than taking responsibility for it. Similar attitudes were described in a study conducted in Hanoi in 2017, where most people would rely exclusively on health authorities for implementing vector control [31].
Our study had several limitations. Firstly, all interviews were conducted during the day when most workers were absent, which can explain the high proportion of retired individuals and limit the representativity of the sample. Prevention practices were self-reported and therefore declaration bias cannot be ruled out, as demonstrated by our contradictory observations on site. Selection of participants for the “mapping exercise” relied mostly on convenience sampling. The exercise would also have benefited from a preparatory training session to give participants more autonomy and limit the influence of the interviewer when constructing the graphs.
5. Conclusion and Recommendations
Our study demonstrates the existence of barriers to implementing vector control measures in Hanoi, which included improper knowledge of vector biology and disease features, low self-responsibility and low perceived self-efficacy. In order for risk awareness to translate into actual protective behaviors, we recommend the adoption of participatory approaches to engage communities and encourage compliance by demonstrating the feasibility and effectiveness of vector control measures, in coordination with local authorities.
Acknowledgments
The authors would like to thank Luke Craven for his assistance in this study and all respondents for participating in the survey.
Author Contributions
Conceptualization, J.F.L. and L.C.; methodology, L.C. and J.F.L.; software, L.C.; formal analysis, L.C.; investigation, L.C., L.P.-T., and T.N.-T.; resources, J.F.L.; data curation, L.C.; writing—original draft preparation, L.C.; writing—review and editing, all; visualization, L.C.; supervision, J.F.L. and H.N.-V.; project administration, J.F.L.; funding acquisition, J.F.L. All authors have read and agreed to the published version of the manuscript.
Funding
This cross-sectional study is part of the “Metropolitan Mosquitoes Project” funded by the Swedish Research Council for Environment, Agricultural Sciences and Spatial Planning (Formas, grant number 2016-00364). The project was also supported by CGIAR Research Program on Agriculture for Nutrition and Health (A4NH).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Brady O.J., Gething P.W., Bhatt S., Messina J.P., Brownstein J.S., Hoen A.G., Moyes C.L., Farlow A.W., Scott T.W., Hay S.I. Refining the Global Spatial Limits of Dengue Virus Transmission by Evidence-Based Consensus. PLOS Neglected Trop. Dis. 2012;6:e1760. doi: 10.1371/journal.pntd.0001760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatt S., Gething P.W., Brady O.J., Messina J.P., Farlow A.W., Moyes C.L., Drake J.M., Brownstein J.S., Hoen A.G., Sankoh O., et al. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee H.S., Nguyen-Viet H., Nam V.S., Lee M., Won S., Duc P.P., Grace D. Seasonal patterns of dengue fever and associated climate factors in 4 provinces in Vietnam from 1994 to 2013. BMC Infect. Dis. 2017;17:218. doi: 10.1186/s12879-017-2326-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pham Thi K.L., Briant L., Gavotte L., Labbe P., Perriat-Sanguinet M., Cornillot E., Vu T.D., Nguyen T.Y., Tran V.P., Nguyen V.S., et al. Incidence of dengue and chikungunya viruses in mosquitoes and human patients in border provinces of Vietnam. Parasites Vectors. 2017;10:556. doi: 10.1186/s13071-017-2422-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cuong H.Q., Hien N.T., Duong T.N., Phong T.V., Cam N.N., Farrar J., Nam V.S., Thai K.T.D., Horby P. Quantifying the Emergence of Dengue in Hanoi, Vietnam: 1998–2009. PLOS Neglected Trop. Dis. 2011;5:e1322. doi: 10.1371/journal.pntd.0001322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen-Tien T., Lundkvist Å., Lindahl J. Urban transmission of mosquito-borne flaviviruses—A review of the risk for humans in Vietnam. Infect. Ecol. Epidemiol. 2019;9:1660129. doi: 10.1080/20008686.2019.1660129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . Update on the Dengue Situation in the Western Pacific Region. WHO; Geneva, Switzerland: 2017. Dengue Situation Update. [Google Scholar]
- 8.Gubler D.J. The Global Emergence/Resurgence of Arboviral Diseases As Public Health Problems. Arch. Med. Res. 2002;33:330–342. doi: 10.1016/S0188-4409(02)00378-8. [DOI] [PubMed] [Google Scholar]
- 9.Minh An D.T., Rocklöv J. Epidemiology of dengue fever in Hanoi from 2002 to 2010 and its meteorological determinants. Glob. Health Action. 2014;7:23074. doi: 10.3402/gha.v7.23074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swaddiwudhipong W., Lerdlukanavonge P., Khumklam P., Koonchote S., Nguntra P., Chaovakiratipong C. A survey of Knowledge, Attitude and Practice of the prevention of Dengue hemorrhagic fever in an urban community of Thailand. Southeast Asian J. Trop. Med. Public Health. 1992;5:1–2. [PubMed] [Google Scholar]
- 11.Arunachalam N., Tyagi B.K., Samuel M., Krishnamoorthi R., Manavalan R., Tewari S.C., Ashokkumar V., Kroeger A., Sommerfeld J., Petzold M. Community-based control of Aedes aegypti by adoption of eco-health methods in Chennai City, India. Pathog. Glob. Health. 2012;106:488–496. doi: 10.1179/2047773212Y.0000000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pengvanich V. Family Leader Empowerment Program Using Participatory Learning Process for Dengue Vector Control. J. Med. Assoc. Thail. 2011;94:235. [PubMed] [Google Scholar]
- 13.Abeyewickreme W., Wickremasinghe A.R., Karunatilake K., Sommerfeld J., Axel K. Community mobilization and household level waste management for dengue vector control in Gampaha district of Sri Lanka; an intervention study. Pathog. Glob. Health. 2012;106:479–487. doi: 10.1179/2047773212Y.0000000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Espinoza-Gomez F. Educational campaign versus malathion spraying for the control of Aedes aegypti in Colima, Mexico. J. Epidemiol. Community Health. 2002;56:148–152. doi: 10.1136/jech.56.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andersson N., Nava-Aguilera E., Arosteguí J., Morales-Perez A., Suazo-Laguna H., Legorreta-Soberanis J., Hernandez-Alvarez C., Fernandez-Salas I., Paredes-Solís S., Balmaseda A., et al. Evidence based community mobilization for dengue prevention in Nicaragua and Mexico (Camino Verde, the Green Way): Cluster randomized controlled trial. BMJ. 2015:h3267. doi: 10.1136/bmj.h3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paixão M.M., Ballouz T., Lindahl J.F. Effect of Education on Improving Knowledge and Behavior for Arboviral Diseases: A Systematic Review and Meta-Analysis. Am. J. Trop. Med. Hyg. 2019 doi: 10.4269/ajtmh.19-0170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kusuma Y.S., Burman D., Kumari R., Lamkang A.S., Babu B.V. Impact of health education based intervention on community’s awareness of dengue and its prevention in Delhi, India. Glob Health Promot. 2019;26:50–59. doi: 10.1177/1757975916686912. [DOI] [PubMed] [Google Scholar]
- 18.Healy K., Hamilton G., Crepeau T., Healy S., Unlu I., Farajollahi A., Fonseca D.M. Integrating the Public in Mosquito Management: Active Education by Community Peers Can Lead to Significant Reduction in Peridomestic Container Mosquito Habitats. PLoS ONE. 2014;9:e108504. doi: 10.1371/journal.pone.0108504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sreedevi A., Burru R., Rao G., Yalamanchili P., Subhaprada C., Kumari V., Kala S., Ms A. Study on awareness about vector borne diseases and education about preventive measures in rural field practice areas of Kurnool medical college, Kurnool. Int. J. Med. Sci. Public Health. 2016;5:1803. doi: 10.5455/ijmsph.2016.25122015325. [DOI] [Google Scholar]
- 20.Saurabh S., Veerakumar A.M., Kalaiselvi S., Palanivel C. Effectiveness of individual health education on the practice of dengue fever prevention in an urban area of Puducherry, India. Indian J. Community Health. 2014;26:434–437. [Google Scholar]
- 21.Hung P.T. Master’s Thesis. KIT (Royal Tropical Institute); Amsterdam, The Netherlands: 2016. Factors determining Dengue in Viet Nam and vector control strategy: A literature review. [Google Scholar]
- 22.Craven L. System Effects: A Hybrid Methodology for Exploring the Determinants of Food In/Security. Ann. Am. Assoc. Geogr. 2017;109:1011–1027. doi: 10.1080/24694452.2017.1309965. [DOI] [Google Scholar]
- 23.Mayxay M., Cui W., Thammavong S., Khensakhou K., Vongxay V., Inthasoum L., Sychareun V., Armstrong G. Dengue in peri-urban Pak-Ngum district, Vientiane capital of Laos: A community survey on knowledge, attitudes and practices. BMC Public Health. 2013;13:434. doi: 10.1186/1471-2458-13-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yasuoka J., Mangione T.W., Spielman A., Levins R. Impact of education on knowledge, agricultural practices, and community actions for mosquito control and mosquito-borne disease prevention in rice ecosystems in Sri Lanka. Am. J. Trop. Med. Hyg. 2006;74:1034–1042. doi: 10.4269/ajtmh.2006.74.1034. [DOI] [PubMed] [Google Scholar]
- 25.Kumaran E., Doum D., Keo V., Sokha L., Sam B., Chan V., Alexander N., Bradley J., Liverani M., Prasetyo D.B., et al. Dengue knowledge, attitudes and practices and their impact on community-based vector control in rural Cambodia. PLoS Negl. Trop. Dis. 2018;12:e0006268. doi: 10.1371/journal.pntd.0006268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rigau-Pérez J.G., Clark G.G., Ruiz-Pérez M., Winch P.J., Leontsini E., Gubler D.J. Community-based dengue prevention programs in Puerto Rico: Impact on knowledge, behavior, and residential mosquito infestation. Am. J. Trop. Med. Hyg. 2002;67:363–370. doi: 10.4269/ajtmh.2002.67.363. [DOI] [PubMed] [Google Scholar]
- 27.Huynh T., Tsuzuki A., Luu L., Tsunoda T., Takagi M., Kawada H. Effect of Existing Practices on Reducing Aedes aegypti Pre-adults in Key Breeding Containers in Ho Chi Minh City, Vietnam. Am. J. Trop. Med. Hyg. 2009;80:752–757. [PubMed] [Google Scholar]
- 28.Setbon M., Raude J. Population response to the risk of vector-borne diseases: Lessons learned from socio-behavioural research during large-scale outbreaks. EHTJ. 2009;2 doi: 10.3402/ehtj.v2i0.7083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoshi T., Martin Banda P., Foster Pemba D., Sunahara T., Minakawa N. Beyond buzzing: Mosquito watching stimulates malaria bednets use—A household-based cluster-randomized controlled assessor blind educational trial. Emerg. Microbes Infect. 2019;2:1–6. doi: 10.1038/emi.2013.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Godin G. L’éducation pour la santé : Les fondements psycho-sociaux de la définition des messages éducatifs. Sci. Soc. Santé. 1991;9:67–94. doi: 10.3406/sosan.1991.1185. [DOI] [Google Scholar]
- 31.Nguyen-Tien T., Probandari A., Ahmad R.A. Barriers to Engaging Communities in a Dengue Vector Control Program: An Implementation Research in an Urban Area in Hanoi City, Vietnam. Am. J. Trop. Med. Hyg. 2019;100:964–973. doi: 10.4269/ajtmh.18-0411. [DOI] [PMC free article] [PubMed] [Google Scholar]