Abstract
Background
Many patients with post-traumatic stress disorder (PTSD) experience dissociative symptoms. The question of whether these dissociative symptoms negatively influence the effectiveness of psychotherapy for PTSD is unresolved.
Aims
To determine the influence of dissociative symptoms on psychotherapy outcome in PTSD.
Method
We conducted a systematic search in Cochrane, Embase, PILOTS, PsycINFO, PubMed and Web of Science for relevant clinical trials. A random-effects meta-analysis examined the impact of dissociation on psychotherapy outcome in PTSD (pre-registered at Prospero CRD42018086575).
Results
Twenty-one trials (of which nine were randomised controlled trials) with 1714 patients were included. Pre-treatment dissociation was not related to treatment effectiveness in patients with PTSD (Pearson's correlation coefficient 0.04, 95% CI −0.04 to 0.13). Between-study heterogeneity was high but was not explained by moderators such as trauma focus of the psychotherapy or risk of bias score. There was no indication for publication bias.
Conclusions
We found no evidence that dissociation moderates the effectiveness of psychotherapy for PTSD. The quality of some of the included studies was relatively low, emphasising the need for high-quality clinical trials in patients with PTSD. The results suggest that pre-treatment dissociation does not determine psychotherapy outcome in PTSD.
Keywords: Dissociative disorders, post-traumatic stress disorder, individual psychotherapy, group psychotherapy
Background
In the DSM-5, a dissociative subtype was added to the classification criteria of post-traumatic stress disorder (PTSD). This subtype describes patients who meet diagnostic criteria for PTSD, and additionally have persistent or recurrent symptoms of depersonalisation (i.e. experience of unreality or detachment from one's thoughts, feelings, sensations, body or actions, for example, unreal or absent self) and derealisation (i.e. experience of unreality or detachment from one's surroundings, for example dreamlike or foggy1). The addition of a dissociative subtype to the DSM-5 was based on multiple sources of evidence, pertaining to factor analyses, brain activation patterns and response to treatment.2
Approximately 14% of the patients with PTSD meet criteria for the dissociative subtype.3 Although this subtype was only recently added to the DSM-5, research on dissociative symptoms in the context of trauma dates back to the nineteenth century.4 Several studies have shown that PTSD is associated with high levels of dissociation, both compared with non-clinical samples and patients with other psychiatric disorders.5–8 Additionally, several studies have shown that dissociation is strongly related to the other PTSD symptoms and that these clusters wax and wane together, also in response to treatments.9–13
A review of brain-imaging studies has shown that dissociative symptoms/states are related to activation of brain areas related to neurological overmodulation of affect.14 This overmodulation of affect could, among others, reduce emotional engagement with the trauma memory, which is considered to be a relevant factor in understanding the effectiveness of current psychotherapies for PTSD.15 This lack of engagement may be specifically relevant for exposure-based psychotherapy as fear activation is thought to be a crucial mechanism underlying the treatment effect.14,16–20
Aims
Currently, there is no consensus about (a) whether patients with PTSD and who dissociate benefit as much from psychotherapy as patients with PTSD who do not dissociate and (b) whether some forms of psychotherapy are particularly ineffective for patients with PTSD and dissociation. Some authors have suggested that treatment programmes need to be tailored for patients with PTSD who have dissociative symptoms, because, as a result of their limited emotion regulation capacities, trauma-focused treatments might even lead to an increase in PTSD symptoms, overall distress and functional impairment.14 Others have argued that there is no evidence for an impeding effect of dissociation on the effectiveness of psychotherapy for PTSD.21 The aim of this study is to provide more clarity to this ongoing debate by quantifying the moderating effect of dissociation on the effectiveness of psychotherapy for PTSD in a meta-analysis.
Method
This project was pre-registered at Prospero (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=86575).
Search strategies
We conducted systematic searches in the following databases up to the 28 August 2018: Cochrane trials register, Embase, PILOTS, PsycINFO, PubMed and Web of Science. Relevant results during the search of review articles, book chapters and studies were searched for further studies and additionally, key authors and research groups were contacted via email to request any data relevant to the study. Search terms were based on (MeSH) terms for PTSD [AND] dissociation [AND] psychotherapy and were adapted to every specific search engine to ensure inclusion of all relevant studies. The search includes the following terms for:
PTSD: Posttrauma* Stress Disorde*, Post-Trauma* Stress Disorde*, Post Trauma* Stress Disorde*, DESNOS, CA-PTSD, C-PTSD, PTSD;
dissociation: Dissocia* Depersonali* Derealization* Derealisation* Fugue* Psychogenic amnesia, and
psychological treatment: Psychotherap*, Therap*, Posttraumatic Growth, Interven*, Treat*, Exposure, EMDR, CBT, STAIR, Recover*.
We manually searched for studies in prior meta-analyses and reviews to ensure that no studies were missed in the systematic search. We de-duplicated data of the search following the protocol of Bramer and colleagues.22
Inclusion criteria
The criteria for individual papers for inclusion were: (a) inclusion of patients who were 18 years of age and older; (b) assessment of PTSD according to the DSM-5, DSM-IV, DSM-III-R or DSM-III criteria; (c) evaluation of psychotherapy with PTSD symptom severity as main outcome; (d) inclusion of validated self-report measures or structured clinical interviews to assess both PTSD symptom severity and dissociation severity; (e) assessment of PTSD symptom severity at pre- and post-treatment; (f) assessment of pre-treatment dissociation severity; (g) inclusion of at least ten participants per treatment condition which is analysed; (h) published in a peer-reviewed journal; and (i) written in English, Dutch, German, Italian, Spanish or French.
Data extraction and risk of bias assessment
Eligible studies were screened twice and data were extracted twice by two independent screeners. All discrepancies were resolved through discussion and consensus. Risk of bias of the studies was assessed independently by two of the authors using the Cochrane risk of bias tool, which resulted in a methodological score for each study included.23 The Cochrane scale assesses sources of bias including selection bias, detection bias and attrition bias. We added two items to this measure about: (a) the type of the PTSD measurement (clinical interview versus self-report); and (b) treatment integrity (whether the original article reported on treatment integrity, yes versus no). Consequently, the adapted Cochrane scale consisted of eight items (see supplementary Table 1 available at https://doi.org/10.1192/bjo.2020.30). Two raters scored each item, and their scores were summed into a risk of bias score (range 0–16; with higher scores indicating higher risk of bias). The risk of bias score was used as a moderator. High bias scores were not considered an exclusion criterion for further analysis.
Potential moderators
To investigate potential moderators of the effect of dissociation on psychotherapy outcome, we coded several study characteristics: (a) completely trauma-focused treatment (yes versus no); (b) randomised controlled trial (yes versus no); (c) sample size (continuous variable); and (d) risk of bias score (continuous variable). The potential moderators were independently coded by two authors and differences were resolved through discussion and consensus.
We compared treatments that were exclusively trauma focused versus those that were not. As dissociation is thought to be because of failing emotion regulation capacities, exposure to traumatic memories would result in emotional overmodulation and consequently impede fear activation and emotional learning. This may prevent the therapeutic effect of exposure, unless emotion regulation or other coping skills are also addressed.14 The treatment was coded as trauma focused if it comprised only evidence-based trauma-focused treatment strategies as described in the manuscript (i.e. prolonged exposure, cognitive processing therapy or eye movement desensitisation and reprocessing). Treatments that also comprised other treatment components (i.e. physical activity or stabilisation) or treatments that did not include trauma-focused treatment strategies were coded as not exclusively trauma focused. If a trial included both types of treatments, we extracted the effect size for the two conditions separately for this moderation analysis (see supplementary Fig. 1 for details).
Statistical analysis
The R package meta was used for all analyses.24 The effect of dissociation on PTSD treatment was determined using pooled effect sizes of the moderating effect of dissociation measured with the Pearson's correlation coefficient (r) between pre-treatment dissociation and change in PTSD symptoms from pre- to post-treatment (post-treatment minus pre-treatment PTSD symptom severity score). A positive correlation would indicate a negative relationship between dissociation and treatment effectiveness, whereas a negative correlation would indicate a positive effect of dissociation on treatment effectiveness. Where needed, we calculated the reported effect size from the data provided into r as common metric.
In cases where we were unable to calculate the effect size from the publication, we contacted the researchers for additional data. We contacted 38 researchers of whom 27 responded. Twelve of these researchers did not provide the data for various reasons (for example no access to data, no time to get data, not willing to share data). Fifteen researchers provided the requested data. Twelve of these studies met the inclusion criteria and were included in the meta-analysis.
We used a random-effects model that allows heterogeneity between studies (assessed with the Q index) and performed a rank test to detect asymmetry in the funnel plot, which is an indication of publication bias. If we had any indications of publication bias either by the rank tests or by visual inspection, we used a trim and fill procedure to correct for bias because of missing studies. In case of a statistically significant main finding of dissociation on treatment effectiveness, we performed the fail-safe tests of Rosenthal and Orwin to assess the robustness of the results. We conducted moderation analyses with a meta-regression approach by fitting mixed-effect models including potential treatment moderators to test for differences in the effect size associated with characteristics of the studies.
Results
Selection and inclusion of studies
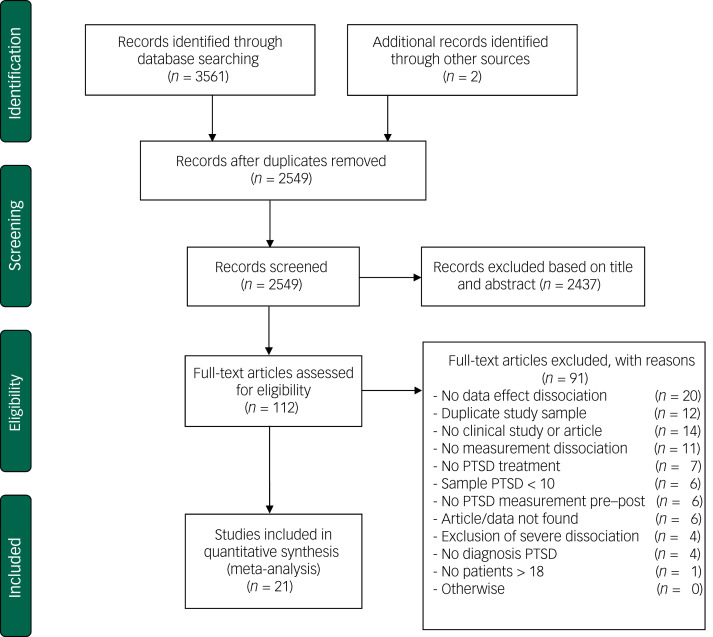
The systematic searches yielded a total of 3563 papers (2549 after removal of duplicates). Of these 2549 papers, 2437 were excluded based on title and abstract as they did not meet inclusion criteria. In total, 112 full-text papers were retrieved of which 91 were excluded because they did not meet the inclusion criteria (see Fig. 1 for details). The remaining 21 articles were included in this meta-analysis. Note that none of the included studies used severe levels of dissociation or diagnosis of dissociative (identity) disorder as exclusion criterion.
Fig. 1.
Flow chart of inclusion of studies.
PTSD, post-traumatic stress disorder.
Characteristics of included studies
The 21 included studies contained a total of 1714 patients from 9 RCTs and 12 uncontrolled clinical trials or treatment cohort studies.8,9,13,25–42 Table 1 shows the study characteristics and potential moderator variables (see supplementary Table 2 for more study details).
Table 1.
Selected characteristics of studies examining the effect of dissociation on post-traumatic stress disorder (PTSD) psychotherapy treatment outcome
| Study | Treatments | Effect size | Female, % | Age, mean (s.d.) | Measure PTSD; DSM | Measure dissociation | Moderators | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Completely trauma focused | Design | Sample size | Risk of bias score | |||||||
| Abramowitz & Lichtenberg (2010)25 | Hypnotherapeutic olfactory conditioning | NR | 0 | 41.2 (12.2) | IES-R; DSM-IV | DES | No | No RCT | 36 | 11.0 |
| Bae et al (2016)26 | EMDR | 1.27 completers | 59 | 34.9 (11.6) | CAPS; DSM-IV | CAPS subtype items + decreased awareness | Yes | No RCT | 60 | 8.0 |
| Cloitre et al (2012)27 | Stair/NST; Support/NST; Stair/support | 1.97 ITT | 100 | 36.4 (9.40) | CAPS; DSM-IV | TSI-DIS averaged score | No | RCT | 75 | 3.0 |
| Gantt et al (2007)28,a | Art, hypnosis, video therapy | NR | 77 | 38 (14) | IES; DSM-IV | DES | No | No RCT | 53 | 11.0 |
| Haagen et al (2018)29 | EMDR, NET, other interventions | 0.36 completers | 3.1 | 39.8 (10.1) | IES-R; DSM-IV | DES | No | No RCT | 64 | 8.0 |
| Hagenaars et al (2010)30 | Prolonged exposure | 3.07 completers | 83 | 35.75 (11.74) | CAPS; DSM-IV | DES | Yes | No RCT | 36 | 4.0 |
| Halvorsen et al (2014)31 | NET + TAU | 0.95 completers | 31 | 35.55 (11.05) | CAPS; DSM-IV | CAPS subtype items | TAU: No; NET: Yes | RCT | 81 | 5.0 |
| Harned et al (2014)32 | DBT + DBT-prolonged exposure | 1.8 ITT | 100 | 32.6 (12.0) | PSS; DSM-IV | DES | No | RCT | 12 | 3.0 |
| Kleindienst et al (2016)33 | DBT-PTSD | NR | 100 | 37.3 (10.5) | CAPS; DSM-IV | DES | No | RCT | 24 | 4.5 |
| Kratzer et al (2019)8 | EMDR + emotional regulation focused group | 1.81 completers | 88 | 47.9 (10.5) | IES-R; DSM-IV | DES | No | No RCT | 150 | 8.5 |
| Lampe et al (2014)34,a | PITT + psychodynamic group | NR. | 100 | 40.72 (10.0) | IES; DSM-IV | DES | No | No RCT | 88 | 9.0 |
| Lynch et al (2008)9,a | NR | NR | 83 | 36 (9.99) | PDS; DSM-IV | DES | No | No RCT | 127 | 8.5 |
| Murphy & Busuttil (2015)35 | Group + individual CBT | NR | 1 | NR | PSS; DSM-IV | DES | No | No RCT | 244 | 11.0 |
| Pabst et al (2014)36,a | NET; TBE | 0.95 completers | 100 | 29.91 (10.11) | PDS; DSM-IV | DES | TBE: No; NET: Yes | RCT | 36 | 3.0 |
| Resick et al (2012)37 | CPT; CPT-C; WTA | 1.68 ITT | 100 | 35.4 (12.4) | CAPS; DSM-IV | TSI-DIS | Yes | RCT | 117 | 3.0 |
| Steele et al (2018)38 | Treatment programme | 0.70 completers | 29 | 42.94 (11.63) | Mississippi scale for PTSD; DSM-III | DES | No | No RCT | 62 | 10.0 |
| Steuwe et al (2016)39 | NET + SIC | 0.70 ITT | 90.9 | 34.9 (9.71) | PDS; DSM-IV | DES | No | No RCT | 11 | 7.5 |
| van Emmerik et al (2008)40,a | CBT; SWT | 0.79 ITT | 65 | 40.87 (11.97) | IES; DSM-IV | DES | Yes | RCT | 50 | 6.5 |
| Van Minnen et al (2016)41 | Prolonged exposure; EMDR | 1.67 completers | 54 | 41.2 (10.5) | CAPS; DSM-IV | CAPS subtype items | Yes | RCT | 82 | 6.0 |
| Wolf et al (2016)42 | Prolonged exposure; PCT | NR | 100 | 44.79 (9.44) | CAPS; DSM-IV | TSI subtype items averaged score | PCT: No; prolonged exposure: Yes | RCT | 137 | 2.5 |
| Zoet et al (2018)13 | EMDR + prolonged exposure + sport | 2.03 completers | 70 | 38.16 (10.90) | CAPS; DSM-IV | CAPS subtype items | No | No RCT | 169 | 5.0 |
NR, not reported; IES, Impact of Events Scale; DES, Dissociative Experiences Scale; DES-T, DES-taxon; RCT, randomised controlled trial; EMDR, eye movement desensitisation and reprocessing; CAPS, Clinician-Administered PTSD scale; Stair: skills training in affective and interpersonal regulation; NST, narrative story telling; ITT, intention to treat; TSI-DIS: Trauma Symptom Inventory-Dissociation; NET, narrative exposure therapy; TAU, treatment as usual; DBT, dialectical behaviour therapy; DBT-PTSD, DBT for PTSD; PSS, PTSD Symptom Scale; PITT, psychodynamic imaginative trauma therapy; PDS: Post-Traumatic Stress Diagnostic Scale; CBT, cognitive– behavioural therapy; TBE, treatment by experts of borderline disorder; CPT, cognitive processing therapy; CPT-C: cognitive therapy only; WTA, written trauma accounts only; SIC, standard inpatient care; SWT: structured writing therapy; PCT, present-centred therapy.
These studies provided additional data for a subsample of patients who met inclusion criteria of this meta-analysis so patient characteristics stated in this table are an estimation based on complete study sample.
Risk of bias score
The overall risk of bias of the included studies was modest (mean 6.6, s.d. = 2.94). Table 2 lists item and total scores for the risk of bias scores for each of the included studies. Agreement between two independent assessors regarding risk of bias of individual studies was high (Cohen's kappa = 0.81, s.e. = 0.04, P < 0.001).
Table 2.
Risk of bias scores of included studies with higher scores indicating a higher risk of bias.
| Item | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Total |
| Abramowitz & Lichtenberg (2010)25 | 1\1 | 1\1 | 1\1 | 1\1 | 2\2 | 2\2 | 2\2 | 1\1 | 11.0 |
| Bae et al (2016)26 | 1\1 | 1\1 | 0\0 | 1\1 | 0\0 | 2\2 | 2\2 | 1\1 | 8.0 |
| Cloitre et al (2012)27 | 0\0 | 0\1 | 2\2 | 0\0 | 0\0 | 0\0 | 0\0 | 0\1 | 3.0 |
| Gantt et al (2007)28 | 1\1 | 1\1 | 1\1 | 1\1 | 2\2 | 2\2 | 2\2 | 1\1 | 11.0 |
| Haagen et al (2018)29 | 1\1 | 1\1 | 0\0 | 1\1 | 0\0 | 2\2 | 2\2 | 1\1 | 8.0 |
| Hagenaars et al (2010)30 | 1\1 | 1\1 | 0\0 | 1\1 | 0\0 | 0\0 | 0\0 | 1\1 | 4.0 |
| Halvorsen et al (2014)31 | 1\1 | 1\1 | 2\1 | 0\0 | 0\0 | 0\0 | 2\2 | 0\1 | 5.0 |
| Harned et al (2014)32 | 1\1 | 1\1 | 1\1 | 0\0 | 0\0 | 0\0 | 0\0 | 1\1 | 3.0 |
| Kleindienst et al (2016)33 | 1\1 | 0\0 | 0\0 | 0\0 | 2\2 | 0\0 | 2\2 | 0\1 | 4.5 |
| Kratzer et al (2019)8 | 1\1 | 1\1 | 1\1 | 1\1 | 0\0 | 2\2 | 2\1 | 1\1 | 8.5 |
| Lampe et al (2014)34 | 1\1 | 1\1 | 1\1 | 1\1 | 0\0 | 2\2 | 2\2 | 1\1 | 9.0 |
| Lynch et al (2008)9 | 1\1 | 1\1 | 1\1 | 1\1 | 0\0 | 2\2 | 2\1 | 1\1 | 8.5 |
| Murphy & Busuttil (2015)35 | 1\1 | 1\1 | 2\2 | 2\2 | 2\2 | 0\0 | 2\2 | 1\1 | 11.0 |
| Pabst et al (2014)36 | 1\1 | 1\1 | 1\1 | 1\1 | 0\0 | 2\1 | 0\0 | 0\1 | 3.0 |
| Resick et al (2012)37 | 0\1 | 0\0 | 2\2 | 0\0 | 0\0 | 0\0 | 0\0 | 0\1 | 3.0 |
| Steele et al (2018)38 | 1\1 | 1\1 | 1\1 | 1\1 | 2\2 | 2\1 | 2\1 | 1\1 | 10.0 |
| Steuwe et al (2016)39 | 1\1 | 1\1 | 1\1 | 0\0 | 0\0 | 2\2 | 2\1 | 1\1 | 7.5 |
| van Emmerik et al (2008)40 | 0\0 | 1\1 | 1\1 | 0\0 | 0\0 | 2\2 | 2\2 | 0\1 | 6.5 |
| Van Minnen et al (2016)41 | 0\1 | 0\1 | 2\2 | 0\0 | 2\2 | 0\1 | 0\0 | 0\1 | 6.0 |
| Wolf et al (2016)42 | 1\1 | 1\1 | 0\0 | 0\0 | 0\0 | 0\0 | 0\0 | 0\1 | 2.5 |
| Zoet et al (2018)13 | 1\1 | 1\1 | 0\0 | 0\0 | 0\0 | 0\0 | 2\2 | 1\1 | 5.0 |
Item 1, random sequence generation; item 2, allocation concealment; item 3, selective reporting; item 4, masking of outcome assessment; item 5, incomplete outcome data; item 6, outcome measurement type; item 7, treatment integrity; item 8, other bias.
Effect of dissociation on PTSD treatment
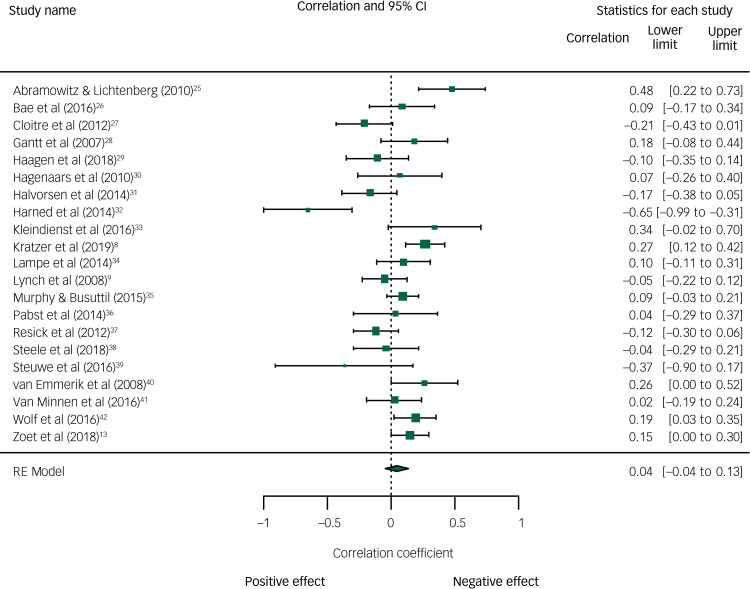
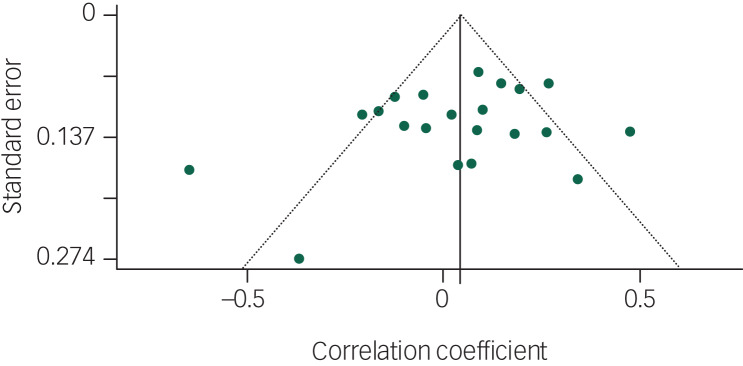
Figure 2 depicts the main results of the meta-analysis. The pooled correlation between pre-treatment dissociation and decrease in PTSD symptoms during treatment was 0.04 (95% CI −0.04 to 0.13, P = 0.32). The heterogeneity between studies was moderately high: I² = 68.90, P < 0.001. Visual inspection of the funnel plot did not indicate asymmetry in any direction (Fig. 3), which was confirmed by Kendall's tau based on the rank correlation (P = 0.46) and by Eggers’ test (P = 0.25). The funnel plot shows two potential outliers: Harned et al (2014)32 (positive effect of dissociation) and Abramowitz & Lichtenberg (2016)25 (negative effect). The study sample of Harned et al (2014)32 was very small and the drop-out was high. The study of Abramowitz & Lichtenberg (2016)25 was an open study with a relatively small sample size. Therefore, both studies may have yielded an effect size that is not so reliable.
Fig. 2.
Pearson's Correlation coefficient (r) between baseline dissociation and change in post-traumatic stress disorder symptoms from pre- to post-treatment.
Fig. 3.
Funnel plot with Pearson's correlation coefficient between dissociation and change in post-traumatic stress disorder symptoms from pre- to post-treatment.
Effect of potential moderators of the effect of dissociation on PTSD treatment outcome
Table 3 shows the results of the moderation analyses. We did not find that a higher risk of bias resulted in a larger effect of dissociation, although this effect was borderline significant (slope r = 0.03, 95% CI −0.002 to 0.06, P = 0.07). In addition, we found no difference in the effect of dissociation on the effectiveness of completely trauma-focused treatments compared with non-trauma-focused/multicomponent treatments (P = 0.76). Similarly, we did not find that the effect of dissociation was different for randomised controlled trials compared with non-randomised studies (P = 0.18), nor did we find an effect of sample size (P = 0.38).
Table 3.
Effect of dissociation on improvement in post-traumatic stress disorder (PTSD) symptoms and moderation analysesa
| n | Pearson's r | 95% CI | P | |
|---|---|---|---|---|
| Overall outcome | 21 | 0.04 | −0.04 to 0.13 | 0.32 |
| Moderation analyses | ||||
| Trauma focused | 8 | 0.06 | −0.11 to 0.22 | 0.76b |
| Not trauma focused/combination | 16 | 0.02 | −0.09 to 0.14 | |
| RCT | 9 | −0.03 | −0.17 to 0.11 | 0.18b |
| No RCT | 12 | 0.10 | −0.02 to 0.21 | |
| Sample size | 21 | 0.001 | −0.001 to 0.002 | 0.38 |
| Risk of bias score | 21 | 0.03 | −0.002 to 0.06 | 0.07 |
Positive correlation (Pearson's correlation) indicates negative effect of dissociation on PTSD improvement.
P-value indicates whether effect size of subgroups differ significantly.
To explore the effect of risk of bias on the results, we performed a post hoc analysis including only studies with a low–moderate risk of bias (i.e. risk of bias score ≤ 8 (n = 14)). The correlation between pre-treatment dissociation and decrease in PTSD symptoms during treatment for higher-quality studies was −0.01 (95% CI −0.13 to 0.10, P = 0.80) and not different from the results derived over all studies.
Discussion
Main findings
We found no evidence for a moderating effect of dissociation on psychotherapy outcome in patients with PTSD. Furthermore, differences between studies in the effect size of dissociation on treatment outcome were not explained by study characteristics. We conclude that comorbid dissociative symptoms do not reduce the effectiveness of psychotherapy in patients with PTSD. Although we did not specifically examine the dissociative subtype of PTSD, the present findings suggest that this subtype may not be associated with worse treatment outcomes as was suggested by the introduction of this subtype in the DSM-5.
Most included studies found non-significant effects of dissociation on the treatment outcome, which corresponds to the null finding of this meta-analysis. The results from the studies reported in this meta-analysis may differ from the conclusion from the individual papers. Some of these studies were hampered by methodological limitations, including incorrect moderation analyses. We assessed dissociation as a treatment moderator. Some individual studies, however, did not test moderation, but reported the association between dissociation and post-treatment PTSD severity.
We were able to include a relatively large number of recently published clinical trials. The addition of the dissociative subtype to the DSM-5 seems to have increased awareness and research into dissociation. We found a moderately high heterogeneity among studies, indicating that the effect of dissociation varied because of systematic differences rather than chance. Despite this variation, the pooled effect size allows a uniform conclusion since the error bars (95% CI) of the effect sizes of most studies include the pooled effect size.43 Moreover, we did not find indications for publication bias.
We examined whether the following study characteristics explained the heterogeneity between studies: type of treatment (exclusively trauma focused or not), risk of bias score, study design and sample size. We observed no effect of type of treatment, study design and sample size. Only a borderline significant effect of bias score was observed. The effect of dissociation on treatment outcome tended to be smaller in the higher-quality studies. No less than one-third of the studies (33%) had a low study quality score, however a post hoc analysis including only those studies with a low or moderate risk of bias again revealed no moderating effect of dissociation. We conclude that this meta-analysis provides no evidence for the idea that dissociation specifically reduces the effectiveness of trauma-focused treatment in those with PTSD.
Limitations
This study has some limitations. First, a meta-analysis can only be as convincing as the quality of the individual studies. In most studies, the effect size of dissociation is based on completer samples (n = 19), thereby limiting the conclusions to those patients who complete treatment. However, all included studies that reported on the effect of dissociation on treatment drop-out found that dissociation was not related to higher treatment drop-out.9,26,27,30,31,41,42 Cloitre and colleagues (2012) even found that patients with high dissociation were less likely to drop-out from treatment.27 We observed quite a few studies of less than optimal quality, however, results were independent of study quality.
As we included several non-controlled clinical trials or cohort studies, we evaluated whether the effect sizes of the included treatments were comparable with previous meta-analyses of psychotherapy for PTSD. The psychotherapies of the included studies showed large within-participant effect sizes from pre- to post-treatment (Cohen's d or Hedges’ g) for treatment completers (mean 1.42) and intention-to-treat samples (mean 1.39). These effect sizes are comparable with those found in meta-analyses investigating the effectiveness of psychotherapy for PTSD as such (and including only randomised clinical trials44).
General limitations of the current studies in patients with PTSD are a lack of long-term follow-up measurements and the use of exclusion criteria (for example suicidality, psychosis or substance misuse), which limits the generalisability of the results. We encourage future studies to use non-restrictive in- and exclusion criteria.45 Second, most (67% of) studies measured dissociation broadly with the Dissociative Experience Scale, which includes depersonalisation, derealisation, amnesia and absorption. Only a few studies measured the dissociative subtype (depersonalisation and derealisation) specifically (n = 5). Furthermore, a recent study indicated that broad and specific measures have a large overlap and high correlation.46 Future studies could focus on other instruments with a different timing of dissociation, for example within-session (state) dissociation.33
Thirdly, we exclusively focused on the effect of only one moderator, that is dissociation, on treatment effects. This specific hypothesis was based on clinical experience and theoretical considerations. Possibly, a combination of patient characteristics (i.e. dissociation, depressive symptoms and functional impairment) is more predictive of treatment responsiveness.47 Future work may consider examining combinations of moderators to detect patients who do not (fully) recover with psychotherapy and to detect differential treatment responses.48 However, the sample sizes will need to be substantial and the risk of spurious or population-specific findings increases if research is not hypothesis-driven. Finally, we did not have the power to evaluate how moderators of the effect of dissociation interact. This could provide more insight into the effect of dissociation under specific conditions.49
Interpretation
Despite these limitations, the strength of our meta-analysis is that it is the first to systematically review the effect of dissociation on psychotherapy outcome in patients with PTSD across different types of psychotherapies. Psychotherapy for PTSD is generally effective but there is room for improvement since about half of the patients still meet criteria for PTSD after treatment.50 About half of clinicians believe that any degree of dissociation is a contraindication for psychotherapeutic treatment of PTSD.45,51 Importantly, the results of our meta-analysis contrast this supposition. We found that pre-treatment dissociation did not reduce the effectiveness of psychotherapy in patients with PTSD.
Acknowledgements
We thank Djana Nesselaar for her help with the screening of the studies and we want to thank Franka Steenhuis for her help with the systematic search terms.
Author contributions
All authors contributed to formulating the research questions and design of the study. C.M.H. carried out the study, C.M.H. and M.L.M. analysed the data and C.M.H. and R.A.D.K. wrote the first draft of the article. All authors read and approved the final version.
Funding
ZonMW (W.V.d.D., M.S., grant number 843001 705) and Innovatiefonds Zorgverzekeraars (D.A.C.O, M.S., grant number 3.180)
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjo.2020.30.
click here to view supplementary material
Declaration of interest
D.A.C.O., C.M.H., W.V.d.D. and M.S. report grants from ZonMW, grants from Innovatie fonds Zorgverzekeraars, during the conduct of the study; others authors have nothing to disclose.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjo.2020.30.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th edn) (DSM-5). American Psychiatric Association, 2013. [Google Scholar]
- 2.Friedman MJ. Finalizing PTSD in DSM-5: getting here from there and where to go next. J Trauma Stress 2013; 26: 548–56. [DOI] [PubMed] [Google Scholar]
- 3.Stein DJ, Koenen KC, Friedman MJ, Hill E, McLaughlin KA, Petukhova M, et al. Dissociation in posttraumatic stress disorder: evidence from the World Mental Health Surveys. Biol Psychiat 2013; 73: 302–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Janet P. L’état Mentale des Hystériques: Les Accidents Mentaux. [The Mental State of Hystericals: Mental Accidents.] Rueff, 1894. [Google Scholar]
- 5.Lyssenko L, Schmahl C, Bockhacker L, Vonderlin R, Bohus M, Kleindienst N. Dissociation in psychiatric disorders: a meta-analysis of studies using the Dissociative Experiences Scale. Am J Psychiatry 2018; 175: 37–46. [DOI] [PubMed] [Google Scholar]
- 6.Putnam FW, Carlson EB, Ross CA, Anderson G, Clark P, Torem M, et al. Patterns of dissociation in clinical and nonclinical samples. J Nerv Ment Dis 1996; 184: 673–9. [DOI] [PubMed] [Google Scholar]
- 7.Özdemir B, Celik C, Oznur T. Assessment of dissociation among combat-exposed soldiers with and without posttraumatic stress disorder. Eur J Psychotraumatol 2015; 6:26657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kratzer L, Heinz P, Schennach R, Schiepek GK, Padberg F, Jobst A. Inpatient treatment of complex PTSD following childhood abuse: effectiveness and predictors of treatment outcome. Psychother Psychosom Med Psychol 2019; 69: 114–22. [DOI] [PubMed] [Google Scholar]
- 9.Lynch SM, Forman E, Mendelsohn M, Herman J. Attending to dissociation: assessing change in dissociation and predicting treatment outcome. J Trauma Dissociation 2008; 9: 301–19. [DOI] [PubMed] [Google Scholar]
- 10.Harned MS, Korslund KE, Foa EB, Linehan MM. Treating PTSD in suicidal and self-injuring women with borderline personality disorder: development and preliminary evaluation of a dialectical behavior therapy prolonged exposure protocol. Behav Res Ther 2012; 50: 381–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rothbaum BO, Astin MC, Marsteller F. Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. J Trauma Stress 2005; 18: 607–16. [DOI] [PubMed] [Google Scholar]
- 12.Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, Ogrodniczuk J. Comparative efficacy, speed, and adverse effects of three PTSD treatments: exposure therapy, EMDR, and relaxation training. J Consult Clin Psychol 2003; 71: 330–8. [DOI] [PubMed] [Google Scholar]
- 13.Zoet HA, Wagenmans A, van Minnen A, de Jongh A. Presence of the dissociative subtype of PTSD does not moderate the outcome of intensive trauma-focused treatment for PTSD. Eur J Psychotraumatol 2018; 9: 1468707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Christian S, Bremner JD, et al. Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype. Am J Psychiatry 2010; 167: 640–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schnyder U, Ehlers A, Elbert T, Foa EB, Gersons BPR, Resick PA, et al. Psychotherapies for PTSD: what do they have in common? Eur J Psychotraumatol 2015; 6; 10.3402/ejpt.v6.28186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ebner-Priemer UW, Mauchnik J, Kleindienst N, Schmahl C, Peper M, Rosenthal Z, et al. Emotional learning during dissociative states in borderline personality disorder. J Psychiatry Neurosci 2009; 34: 214–22. [PMC free article] [PubMed] [Google Scholar]
- 17.Jaycox LH, Foa EB, Morral AR. Influence of emotional engagement and habituation on exposure therapy for PTSD. J Consult Clin Psychol 1998; 66: 185–92. [DOI] [PubMed] [Google Scholar]
- 18.Foa EB, McLean CP. The Efficacy of Exposure Therapy for Anxiety-Related Disorders and Its Underlying Mechanisms: The Case of OCD and PTSD. Annu Rev Clin Psychol 2016; 12: 1–28. [DOI] [PubMed] [Google Scholar]
- 19.Pittig A, Treanor M, LeBeau RT, Craske MG. The role of associative fear and avoidance learning in anxiety disorders: Gaps and directions for future research. Neurosci Biobehav R 2018; 88: 117–40. [DOI] [PubMed] [Google Scholar]
- 20.Cooper AA, Clifton EG, Feeny NC. An empirical review of potential mediators and mechanisms of prolonged exposure therapy. Clin Psychol Rev 2017; 56: 106–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Minnen A, Harned MS, Zoellner L, Mills K. Examining potential contraindications for prolonged exposure therapy for PTSD. Eur J Psychotraumatol 2012; 3:10.3402/ejpt.v3i0.18805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 2016; 104: 240–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JPT, Green S, Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell, 2008. [Google Scholar]
- 24.Schwarzer G. “meta: Meta-Analysis with R.” R package version 1.6-0. R Project, 2010. (http://CRAN.R-project.org/package=meta)
- 25.Abramowitz EG, Lichtenberg P. A new hypnotic technique for treating combat-related posttraumatic stress disorder: a prospective open study. Int J Clin Exp Hyp 2010; 58: 316–28. [DOI] [PubMed] [Google Scholar]
- 26.Bae H, Kim D, Park YC. Dissociation predicts treatment response in eye-movement desensitization and reprocessing for posttraumatic stress disorder. J Trauma Dissociation 2016; 17: 112–30. [DOI] [PubMed] [Google Scholar]
- 27.Cloitre M, Petkova E, Wang J, Lu FH. An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depress Anxiety 2012; 29: 709–17. [DOI] [PubMed] [Google Scholar]
- 28.Gantt L, Tinnin LW. Intensive trauma therapy of PTSD and dissociation: an outcome study. Arts Psychother 2007; 34: 69–80. [Google Scholar]
- 29.Haagen JFG, van Rijn A, Knipscheer JW, van der Aa N, Kleber RJ. The dissociative post-traumatic stress disorder (PTSD) subtype: a treatment outcome cohort study in veterans with PTSD. Br J Clin Psychol 2018; 7: 203–22. [DOI] [PubMed] [Google Scholar]
- 30.Hagenaars MA, van Minnen A, Hoogduin KAL. The impact of dissociation and depression on the efficacy of prolonged exposure treatment for PTSD. Behav Res Ther 2010; 48: 19–27. [DOI] [PubMed] [Google Scholar]
- 31.Halvorsen JO, Stenmark H, Neuner F, Nordahl HM. Does dissociation moderate treatment outcomes of narrative exposure therapy for PTSD? A secondary analysis from a randomized controlled clinical trial. Behav Res Ther 2014; 57: 21–8. [DOI] [PubMed] [Google Scholar]
- 32.Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of dialectical behavior therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behav Res Ther 2014; 55: 7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kleindienst N, Priebe K, Gorg N, Dyer A, Steil R, Lyssenko L, et al. State dissociation moderates response to dialectical behavior therapy for posttraumatic stress disorder in women with and without borderline personality disorder. Eur J Psychotraumatol 2016; 7: 10.3402/ejpt.v7.30375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lampe A, Hofmann P, Gast U, Reddemann L, Schusler G. Long-term course in female survivors of childhood abuse after psychodynamically oriented, trauma-specific inpatient treatment: a naturalistic two-year follow-up. Z Psychosom Med Psychother 2014; 60: 267–82. [DOI] [PubMed] [Google Scholar]
- 35.Murphy D, Busuttil W. Exploring outcome predictors in UK veterans treated for PTSD. Psychology Research 2015; 5(8): 441–51. [Google Scholar]
- 36.Pabst A, Schauer M, Bernhardt K, Ruf-Leuschner M, Goder R, Elbert T, et al. Evaluation of narrative exposure therapy (NET) for borderline personality disorder with comorbid posttraumatic stress disorder. Clin Neuropsychiatry 2014; 11: 108–17. [Google Scholar]
- 37.Resick PA, Suvak MK, Johnides BD, Mitchell KS, Iverson KM. The impact of dissociation on PTSD treatment with cognitive processing therapy. Depress Anxiety 2012; 29: 718–30. [DOI] [PubMed] [Google Scholar]
- 38.Steele E, Wood DS, Usadi EJ, Applegarth DM. TRR's warrior camp: an intensive treatment program for combat trauma in active military and veterans of all eras. Mil Med 2018; 183: 403–7. [DOI] [PubMed] [Google Scholar]
- 39.Steuwe C, Rullkotter N, Ertl V, Berg M, Neuner F, Beblo T, et al. Effectiveness and feasibility of narrative exposure therapy (NET) in patients with borderline personality disorder and posttraumatic stress disorder–a pilot study. BMC Psychiatry 2016; 16: 254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Emmerik AAP, Kamphuis JH, Emmelkamp PMG. Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioral therapy or structured writing therapy: a randomized controlled trial. Psychother Psychosom 2008; 77: 93–100. [DOI] [PubMed] [Google Scholar]
- 41.van Minnen A, van der Vleugel BM, van den Berg DP, de Bont PA, de Roos C, van der Gaag M, et al. Effectiveness of trauma-focused treatment for patients with psychosis with and without the dissociative subtype of post-traumatic stress disorder. Br J Psychiatry 2016; 209: 347–8. [DOI] [PubMed] [Google Scholar]
- 42.Wolf EJ, Lunney CA, Schnurr PP. The influence of the dissociative subtype of posttraumatic stress disorder on treatment efficacy in female veterans and active duty service members. J Consult Clin Psychol 2016; 84: 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fletcher J. What is heterogeneity and is it important? BMJ 2007; 334: 94–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee DJ, Schnitzlein CW, Wolf JP, Vythilingam M, Rasmusson AM, Hoge CW. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systemic review and meta-analyses to determine first-line treatments. Depress Anxiety 2016; 33: 792–806. [DOI] [PubMed] [Google Scholar]
- 45.Ronconi JM, Shiner B, Watts BV. Inclusion and exclusion criteria in randomized controlled trials of psychotherapy for PTSD. J Psychiatr Pract 2014; 20: 25–37. [DOI] [PubMed] [Google Scholar]
- 46.Swart S, Wildschut M, Draijer N, Langeland W, Smit JH. Dissociative subtype of posttraumatic stress disorder or PTSD with comorbid dissociative disorders: comparative evaluation of clinical profiles. Psychol Trauma 2019; 12: 38–45. [DOI] [PubMed] [Google Scholar]
- 47.Deisenhofer AK, Delgadillo J, Rubel JA, Bohnke JR, Zimmermann D, Schwartz B, et al. Individual treatment selection for patients with posttraumatic stress disorder. Depress Anxiety 2018; 35: 541–50. [DOI] [PubMed] [Google Scholar]
- 48.DeRubeis RJ, Cohen ZD, Forand NR, Fournier JC, Gelfand LA, Lorenzo-Luaces L. The Personalized Advantage Index: translating research on prediction into individualized treatment recommendations. A demonstration. PLoS One 2014; 9: e83875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li XR, Dusseldorp E, Meulman JJ. Meta-CART: a tool to identify interactions between moderators in meta-analysis. Brit J Math Stat Psy 2017; 70: 118–36. [DOI] [PubMed] [Google Scholar]
- 50.Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry 2005; 162: 214–27. [DOI] [PubMed] [Google Scholar]
- 51.Becker CB, Zayfert C, Anderson E. A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behav Res Ther 2004; 42: 277–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjo.2020.30.
click here to view supplementary material