Abstract
Objective
The aim was to recommend an integrated Total Worker Health (TWH) approach which embraces core human factors and ergonomic principles, supporting worker safety, health, and well-being during the COVID-19 pandemic.
Background
COVID-19 has resulted in unprecedented challenges to workplace safety and health for workers and managers in essential businesses, including healthcare workers, grocery stores, delivery services, warehouses, and distribution centers. Essential workers need protection, accurate information, and a supportive work environment with an unwavering focus on effective infection control.
Method
The investigators reviewed emerging workplace recommendations for reducing workers’ exposures to the novel coronavirus and the challenges to workers in protecting their health. Using a theoretical framework and guidelines for integrating safety and health management systems into an organization for TWH, the investigators adapted the framework’s key characteristics to meet the specific worker safety and health issues for effective infection control, providing supports for increasing psychological demands while ensuring a safe work environment.
Results
The recommended approach includes six key characteristics: focusing on working conditions for infection control and supportive environments for increased psychological demands; utilizing participatory approaches involving workers in identifying daily challenges and unique solutions; employing comprehensive and collaborative efforts to increase system efficiencies; committing as leaders to supporting workers through action and communications; adhering to ethical and legal standards; and using data to guide actions and evaluate progress.
Conclusion
Applying an integrative TWH approach for worker safety, health, and well-being provides a framework to help managers systematically organize and protect themselves, essential workers, and the public during the COVID-19 pandemic.
Application
By using the systems approach provided by the six implementation characteristics, employers of essential workers can organize their own efforts to improve system performance and worker well-being during these unprecedented times.
Keywords: human factors and ergonomics, safety management systems, coronavirus, Total Worker Health
Introduction
Workers’ safety, health, and well-being have been thrust into the national spotlight during the COVID-19 pandemic. Coronavirus and its resulting COVID-19 disease are infecting and killing essential workers every day (Rothwell, 2020). While healthcare workers are on the front lines of fighting the disease itself, other essential workers—for example, those working in grocery stores, transportation services, warehouse, construction, retail, and delivery—face workplace exposure to the virus. The virus is easily transmitted between people, increasing likelihood of infection of these essential workers and those they come in contact with (Rothan & Byrareddy, 2020).
As the risk of infection is ever present, essential workers live with fear of exposure and lack of certainty. The collective response to the COVID-19 pandemic substantially impacts the safety, health, and well-being of essential workers, who come into contact with the general public even during stay-at-home orders. The uncertainty of others’ infection statuses adds stress to each interaction. In addition, public health responses, such as physical distancing, scheduling changes, and loss of home services (e.g., cleaning, daycare, schooling), have fundamentally changed the way we live, work, and interact. These changes are stressful for everyone, but are even more stressful for those who must continue to go to a workplace while others stay at home.
Application of human factors and ergonomic knowledge provides a framework to tackle these many challenges through a systems approach that addresses the physical, organizational, and cognitive factors at play for essential workers (Dul et al., 2012). According to the International Ergonomics Association, human factors and ergonomics “uses a holistic, systems approach to apply theory, principles, and data to the design and evaluation of tasks, jobs, products, environments, and systems” (IEA, 2020).
The authors, based at the Center for Work, Health, and Well-being at the Harvard T.H. Chan School of Public Health, have used a systems approach similar to that used within the human factors and ergonomics field. This approach recognizes the multiple pathways within the workplace that impact worker safety, health, and well-being (Sorensen et al., 2016). The Center’s conceptual framework builds on many human factors and ergonomic theories including social ecological models (McLeroy et al., 1988; Stokols, 1996), hierarchy of controls (Levy et al., 2017), organizational ergonomics (McLeroy et al., 1988; Stokols, 1996), participatory frameworks (Punnett et al., 2013; Rivilis et al., 2008), job strain (Karasek & Theorell, 1990), and sociotechnical systems theory (Murphy et al., 2014; Sauter et al., 2002). This systems approach and its theoretical framework are consistent with that used by the National Institute for Occupational Safety and Health’s (NIOSH) Total Worker Health (TWH) program, other TWH Centers of Excellence, and TWH affiliates (Anger et al., 2015; Punnett et al., 2020; Tamers et al., 2019). The Center has developed several resources including an Implementation Manual to guide organizations to integrate worker safety, health, and well-being into the structure of an organization and the Workplace Integrated Safety and Health (WISH) assessment, which measures essential elements of an effective integrated approach (McLellan et al., 2017; Sorensen et al., 2018).
Since the early days of the coronavirus outbreak, the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), and others have made various recommendations and suggestions for how employers can respond to protect workers and the public in the face of the epidemic (CDC, 2020; NIOSH, 2020; WHO, 2020). These recommendations have been numerous, frequently changing, and often lack a holistic, systems approach, which has been associated with better outcomes than single programmatic approaches (Manjourides & Dennerlein, 2019). Therefore, the objective of this paper is to recommend a workplace approach based on a TWH framework to protect the safety, health, and well-being of essential workers during the COVID-19 pandemic.
Methods
Investigators from the Harvard T.H. Chan School of Public Health Center for Work, Health, and Well-being, one of the six TWH Centers of Excellence funded by the NIOSH, developed recommendations for managers of essential workers.
The investigators first reviewed workplace requirements and recommendations that were being released by WHO, NIOSH, and other public health, worker safety, and health advocate organizations for reducing workers’ exposure to coronavirus and challenges to workers in protecting their health (Burke et al., 2020).
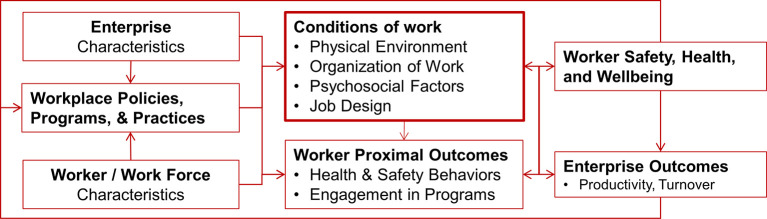
As a theoretical framework, the investigators utilized a conceptual model (Figure 1) that articulates the central role of the conditions of work and organizational policies, programs, and practices that promote adoption of system-level approaches, rather than focusing on individual worker behaviors (Sorensen et al., 2016). The model reflects that workers respond to the overall work environment while recognizing the complex interplay of factors involving individual workers (and their behaviors) and the immediate work environment, as well as characteristics of the broader contexts in which both the worker and the workplace are embedded.
Figure 1.
The Center’s conceptual model that articulates the central role of the conditions of work on worker safety, health, and well-being. Adapted from Sorensen et al. (2016).
As a framework for implementation within an organization, the investigators adapted the six key characteristics that are indicative of best practices for protecting and promoting worker safety, health, and well-being (Table 1). These six characteristics were developed by the Center as both key program characteristics for implementation (McLellan et al., 2017) and an assessment that measures the implementation of systems approaches embedded in an organization’s policies, programs, and practices (Sorensen et al., 2018).
Table 1.
Six Key Characteristics From the Workplace Integrated Safety and Health (WISH) Assessment
| Key Characteristics | Definitions From Sorensen et al. (2018) |
|---|---|
| Leadership commitment | Leadership makes worker safety, health, and well-being a clear priority for the entire organization. It drives accountability and provides the necessary resources and environment to create positive working conditions |
| Policies, programs, and practices that foster supportive working conditions | The organization enhances worker safety, health, and well-being with policies and practices that improve working conditions |
| Participation | Stakeholders at every level of an organization, including labor unions or other worker organizations if present, help plan and carry out efforts to protect and promote worker safety and health |
| Comprehensive and collaborative strategies | Employees from across the organization work together to develop comprehensive health and safety initiatives |
| Adherence | The organization adheres to federal and state regulations, as well as ethical norms, that advance worker safety, health, and well-being |
| Data-driven change | Regular evaluation guides an organization’s priority setting, decision making, and continuous improvement of worker safety, health, and well-being initiatives |
Results
Leadership Commitment
Leadership commitment is driven by clear, consistent, transparent, and empathic communication to all workers from all levels of management regarding policies, programs, and practices that protect workers from COVID-19 (Lord et al., 2017; Quelch, 2020). By doing so, leadership demonstrates that the organization places a high priority on worker health and safety, which sets the stage for ensuring accountability and support across all levels of the organization. These communications need to be supported by clear and consistent actions and implementation of new policies by leaders demonstrating these values by providing a supportive work environment while remaining calm and compassionate. Communication content should be verified for accuracy and developed based on public health recommendations and guidelines for best practices.
Focus on Working Conditions
The approach starts with a focus on working conditions and policies that impact these conditions. Working conditions are central to effective infection control in the workplace. Grounded in workplace safety and health’s hierarchy of controls (Levy et al., 2017), effective infection control reduces worker exposure to the coronavirus. This includes engineering controls such as increased ventilation of fresh air and high-efficiency air filters to reduce airborne pathogens (Allen & Macomber, 2020). Separation methods such as the use of physical barriers between workers and customers at retail checkout stations provide similar controls on potential exposure. The hierarchy of controls model also includes administrative controls to allow physical distancing between workers, coworkers, clients, and customers. These can include scheduling policies that reduce workers’ contact with customers or clients; for example, scheduling retail workers to restock shelves during hours closed to customers or scheduling the same workers to the same crews/shifts. In addition, providing adequate access to handwashing facilities at work and providing personal protective equipment for workers and customers/patients (e.g., face shields, masks) provides the last layer of defense in the hierarchy. In addition, employers may provide additional resources to ensure the safety and health of their workers. As improved testing becomes available, ensuring adequate testing and contact tracing will provide an additional resource to ensure worker safety.
Implementing supportive policies and encouraging workers to use these policies can have a profound impact on workers’ physical and mental health (López et al., 2019). Sick leave with pay allows those who are sick to stay home with financial and job security and also protects the health of other workers. Implementing leave-sharing lets employees with accrued paid time-off give some of that time to others who have exhausted their own. Other policies around scheduling breaks and using personal, sick, or vacation time can relieve the stress of balancing work with greater personal obligations, especially when schools are closed, or relatives may be ill or at high risk or forced to quarantine.
Supportive working conditions can address the increased psychological demands on essential workers. These workers face many threats to their psychological well-being, including fear of exposure, the worry of taking the disease home, stress related to increased work demands and pace, and balancing work with increased personal responsibilities such as childcare. Providing flexibility with breaks, alternative scheduling, using participatory approaches, and clear and accurate communications provide a supportive social environment that addresses the extra demands on the workers (Hurtado et al., 2015). In retail settings, policies for customers to wear masks can help workers feel supported. Ensuring consistent and regular breaks provides opportunities for restoration and stress reduction.
Participation
Employee participation in decision making facilitates a broader culture of health, safety, and well-being within any organization. Participation creates a mechanism for workers to provide information to the organization. Effective and sustainable organizational functioning during COVID-19 relies upon employees feeling empowered to identify safety hazards and threats without fear of retaliation (Punnett et al., 2013; Rivilis et al., 2008). Essential workers on the front lines have extra burdens related to the fear of exposure and adapting work to meet new requirements, which adds a huge amount of stress—understanding how these burdens impact them and their ability to remain healthy and safe while continuing to perform their duties can inform workplace improvements beyond simply meeting the requirements. Employees have the best understanding of how the current work environment impacts them and how it might be improved. When managers listen to employees, it can promote the development of innovative and simple workplace improvements (Hofmann et al., 2017). Being heard may reduce workplace stress as it empowers workers and increases feelings of camaraderie and team cohesion. A simple approach may include having a short huddle with workers to ask three questions: (1) What’s going well and not so well with your health here today? (2) What about work is impacting your health positively and not so positively? (3) What can the team/unit/employer do to help your health and well-being?
Comprehensive and Collaborative Strategies
Many parts of an organization can influence working conditions that in turn impact the transmission of COVID-19, as well as support workers’ well-being during the pandemic (McLellan et al., 2017; Sorensen et al., 2013). Different functional units of an organization, such as janitorial services, inventory management, sales, and shipping, will benefit from working together to understand the impacts on others’ jobs and how they can help one another. Collaborating horizontally within an organization through the use of safety and health committees or a specific COVID-19 task force can coordinate efforts that support all of an organization’s workers (Davis et al., 2014; Dennerlein et al., 2017).
Adherence
While both ethical norms and legal standards are changing quickly as communities and governments enact sweeping rules to stem the spread of COVID-19, adhering to worker safety and health standards provides a starting point to protect their workers. Organizations must follow existing and evolving standards and recommendations from governmental agencies for reducing the risk of transmission. In addition, adhering to wage and benefit requirements, especially sick leave policies and expectations, helps provide a supportive environment for workers. Many governmental and nongovernmental agencies are providing resources to help organizations create safer and more supportive environments (MassCOSH, 2020; NationalCOSH, 2020; OSHA, 2020). As standards change, for example with increased availability of testing, employers need to be poised to respond to new requirements in support of their employees’ health and safety. Respecting the values and beliefs of workers during this time is especially important so that workers will not face added psychological burdens.
Data-Driven Change
Using data to set priorities and form decisions during this time of uncertainty can guide an organization’s efforts. There is a range of data that quantifies levels of risk and can inform planning. For example, monitoring the level of carbon dioxide in indoor air provides an indication of how much fresh air is in the workplace. Using payroll and shift assignment data can identify and plan work assignments to minimize worker exposures to other workers and customers or clients (Sabbath et al., 2018). Wide availability of reliable COVID-19 tests and contact tracing can help identify those employees who need to quarantine and have access to treatment, while minimizing exposing other workers. Qualitative data from both managers and frontline workers can identify opportunities and find solutions to improve working conditions, as described above. Data can also be used to measure improvements related to the efforts implemented to reduce the health impacts of COVID-19. Quick short surveys of workers can provide confidential feedback and communicate leadership’s value of worker input. Finally, sharing findings with employees, without compromising confidentiality, is critical in developing trust. Seeing success and positive changes may boost employee morale and increase motivation to be engaged at work during this challenging time.
Discussion
Our goal for this paper is to recommend a systems approach based on a TWH framework for employers and managers at essential businesses to be strategic in implementing workplace measures to protect worker safety, health, and well-being during the COVID-19 pandemic. The amount of information, requirements, and guidelines, as well as daily public policy changes, fundamentally changes the way we live, work, and interact. These new requirements and ways we work can be overwhelming. Based on a core construct for implementing TWH strategies, the paper recommends six key characteristics of an effective approach for workplaces.
The characteristics of the approach are grounded in core fundamental human factors and ergonomics principles to improve well-being. Workplace implementation of any health and safety program requires understanding the physical, organizational, and cognitive components of the human systems interaction. These recognize the central role of the physical and organizational aspects of work and exposure through working conditions. The characteristics also recognize the key aspects of how an organization works and how to improve performance through participatory approaches, collaborative and comprehensive engagement, data-driven change, and leadership commitment. Through the conceptual model, the recommendations recognize the cognitive domain of human factors and ergonomics and how workers respond to the work environment as a whole.
The characteristics follow the themes from many best practice documents (Ismail et al., 2012). For example, NIOSH Essential Elements of Effective Workplace Programs and Policies for Improving Worker Health and Well-being, a precursor to the NIOSH TWH initiative, groups recommendations into four categories of organizational culture and leadership, program design, program implementation and resources, and program evaluation (NIOSH, 2008). Similarly, the Occupational Safety and Health Administration’s (OSHA) proposed injury and illness prevention program (I2P2) includes management leadership, worker participation, hazard identification and assessment, hazard prevention and control, and program evaluation and improvement (OSHA, 2012). Furthermore, other NIOSH TWH Centers of Excellence and TWH affiliates promote organizational systems approaches with similar components, especially participatory approaches and comprehensive and collaborative strategies (McLellan, 2016; Pronk, 2013; Punnett et al., 2020).
Limitations of this review are the broad nature of the approach and that the review does not provide specific solutions, for example, the different types of masks and their specific efficacy. There are a great deal of detailed examples available from government agencies, health organizations, industry and commerce, and worker safety and health advocates, identified through a search of the internet (some of which are highlighted on our website http://centerforworkhealth.sph.harvard.edu/covid19). This review provides a framework to help organizations strategically adopt and adapt these resources to their own workers and context. By design, the characteristics of the approach and the WISH (Table 1) are not mutually exclusive, which reflects a systems approach with interdependent elements.. Furthermore, there are many external factors that make implementing some guidelines more difficult. For example, the availability of personal protective equipment, disinfectant, and reliable COVID-19 testing makes it difficult for companies to comply and adds to workers feeling uncertain about their safety.
Finally, while work and the workplace are changing rapidly, these characteristics still hold true to protecting and promoting worker well-being by focusing on improving working conditions, rather than relying on individual behavior change. These characteristics are core principles that can guide any employer and help workers find support within their own organization. We expect that this framework will provide similar guidance as more nonessential businesses prepare to return to the workplace and as society as a whole responds to new phases in managing the pandemic. Organizations with such systems in place will most likely be more resilient to these new challenges.
Key Points
COVID-19 has resulted in unprecedented challenges to worker safety, health, and well-being.
A successful systems approach grounded in TWH that integrates worker safety, health, and well-being into an organization includes six key characteristics: focusing on working conditions, utilizing participatory approaches, employing comprehensive and collaborative strategies, commitment from leaders, adhering to ethical and legal standards, and data-driven change.
Applying an integrative approach for worker safety, health, and well-being provides a framework to help managers systematically organize and protect themselves, their workers, and the public during the COVID-19 pandemic.
Acknowledgments
The authors wish to thank Shana McGough and her colleagues at the Health Communication Core and Linnea Benson-Whelan at the Dana-Farber Cancer Institute for their collaboration and assistance.
This work was supported by a grant from the NIOSH for the Harvard T.H. Chan School of Public Health Center for Work, Health, and Well-being (U19 OH008861). Total Worker Health is a registered trademark of the U.S. Department of Health and Human Services (HHS). The content is solely the responsibility of the authors and does not necessarily represent the official views of HHS, the Centers for Disease Control and Prevention, or the NIOSH.
Author Biographies
Jack T. Dennerlein is a professor in the Bouvé College of Health Sciences at Northeastern University and associate director of the Harvard T.H. Chan School of Public Health Center for Work, Health, and Well-being. Dennerlein received his PhD in mechanical engineering from the University of California, Berkeley, in 1996.
Lisa Burke is the director of Research and Outreach Initiatives for the Harvard T.H. Chan School of Public Health Center for Work, Health, and Well-being at the Dana-Farber Cancer Institute. Burke earned her MSEd in psychology from the University of Pennsylvania in 1996.
Erika L. Sabbath is an associate professor at the Boston College School of Social Work and the principal investigator for The Boston Hospital Workers Health Study, a Harvard T.H. Chan School of Public Health Center for Work, Health, and Well-being research project. Sabbath received her ScD in social and behavioral sciences from the Harvard T.H. Chan School of Public Health and in epidemiology from Université Paris XI-Sud in 2012.
Jessica A. R. Williams is an assistant professor at the University of Kansas Medical Center and the principal investigator of the Enterprise Outcomes Study, a Harvard T.H. Chan School of Public Health Center for Work, Health, and Well-being research project. Williams received her PhD in health policy and management from the University of California, Los Angeles, in 2013.
Susan E. Peters is a research associate in the Department of Social and Behavioral Sciences at the Harvard T.H. Chan School of Public Health and a coinvestigator at its Center for Work, Health, and Well-being. Peters received her PhD in health and rehabilitation sciences from the University of Queensland, Australia, in 2016.
Lorraine Wallace is the associate director of the Dana-Farber Cancer Institute Center for Community Based Research and the assistant director for the Harvard T.H. Chan School of Public Health Center for Work, Health, and Well-being. Wallace received her MPH from the University of Massachusetts, Amherst, in 1995.
Melissa Karapanos is a research project director at the Dana-Farber Cancer Institute and outreach project director for the Harvard T.H. Chan School of Public Health Center for Work, Health, and Well-being. Karapanos received her MPH from the University of North Carolina at Chapel Hill in 2014.
Glorian Sorensen is a professor in the Department of Social and Behavioral Sciences, director of the Center for Work, Health, and Well-being at the Harvard T.H. Chan School of Public Health, and director for the Center for Community Based Research at the Dana-Farber Cancer Institute. Sorensen received her PhD in occupational sociology from the University of Minnesota in 1983.
ORCID iD
Jack T. Dennerlein https://orcid.org/0000-0001-7703-643X
References
- Allen J. G., Macomber J. D. (2020). Healthy buildings: How indoor spaces drive performance and productivity. Harvard University Press. [Google Scholar]
- Anger W. K., Elliot D. L., Bodner T., Olson R., Rohlman D. S., Truxillo D. M., Kuehl K. S., Hammer L. B., Montgomery D. (2015). Effectiveness of total worker health interventions. Journal of Occupational Health Psychology, 20, 226–247. 10.1037/a0038340 [DOI] [PubMed] [Google Scholar]
- Burke L., Wallace L., Karapanos M., Dennerlein J. T. (2020). Harvard T.H. Chan School of Public Health Center for work health and well-being coronavirus (COVID-19) resource website. http://centerforworkhealth.sph.harvard.edu/covid19
- CDC (2020). Centers for disease control interim guidance for businesses and employers to plan and respond to coronavirus disease 2019 (COVID-19): Plan, prepare and respond to coronavirus disease 2019. https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-business-response.html
- Davis L., Miner C., Laramie A., Sparer E. H., Wegman D. (2014). Moving into the Future: Promoting safe patient handling for worker and patient safety in Massachusetts hospitals. Commonwealth of Massachusetts. http://www.mass.gov/eohhs/docs/dph/occupational-health/ergo-sph-hospitals-2014.pdf
- Dennerlein J. T., O’Day E. T., Mulloy D. F., Somerville J., Stoddard A. M., Kenwood C., Teeple E., Boden L. I., Sorensen G., Hashimoto D. (2017). Lifting and exertion injuries decrease after implementation of an integrated hospital-wide safe patient handling and mobilisation programme. Occupational and Environmental Medicine, 74, 336–343. 10.1136/oemed-2015-103507 [DOI] [PubMed] [Google Scholar]
- Dul J., Bruder R., Buckle P., Carayon P., Falzon P., Marras W. S., Wilson J. R., van der Doelen B. (2012). A strategy for human factors/ergonomics: Developing the discipline and profession. Ergonomics, 55, 377–395. 10.1080/00140139.2012.661087 [DOI] [PubMed] [Google Scholar]
- Hofmann D. A., Burke M. J., Zohar D. (2017). 100 years of occupational safety research: From basic protections and work analysis to a multilevel view of workplace safety and risk. Journal of Applied Psychology, 102, 375–388. 10.1037/apl0000114 [DOI] [PubMed] [Google Scholar]
- Hurtado D. A., Nelson C. C., Hashimoto D., Sorensen G. (2015). Supervisors’ support for nurses’ meal breaks and mental health. Workplace Health & Safety, 63, 107–115. 10.1177/2165079915571354 [DOI] [PubMed] [Google Scholar]
- IEA I. E. A. (2020). What is ergonomics. https://iea.cc/what-is-ergonomics/
- Ismail Z., Doostdar S., Harun Z. (2012). Factors influencing the implementation of a safety management system for construction sites. Safety Science, 50, 418–423. 10.1016/j.ssci.2011.10.001 [DOI] [Google Scholar]
- Karasek R., Theorell T. (1990). Healthy work: Stress, productivity, and the reconstruction of working life. Basic Books. [Google Scholar]
- Levy B. S., Wegman D. H., Baron S. L., Sokas R. K. (2017). Occupational and environmental health: Recognizing and preventing disease and injury (7th ed.). Oxford University Press. [Google Scholar]
- López Gómez M. A., Sabbath E., Boden L., Williams J. A. R., Hopcia K., Hashimoto D., Sorensen G. (2019). Organizational and psychosocial working conditions and their relationship with mental health outcomes in patient-care workers. Journal of Occupational and Environmental Medicine, 61, e480–e485. 10.1097/JOM.0000000000001736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord R. G., Day D., Zaccaro S. J., Avolio B. J., Eagly A. H. (2017). Leadership in applied psychology: Three waves of theory and research. Journal of Applied Psychology, 102, 434–451. 10.1037/apl0000089 [DOI] [PubMed] [Google Scholar]
- Manjourides J., Dennerlein J. T. (2019). Testing the associations between leading and lagging indicators in a contractor safety pre-qualification database. American Journal of Industrial Medicine, 62, 317–324. 10.1002/ajim.22951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MassCOSH (2020). Massachusetts coalition for occupational safety and health, comprehensive information on Covid-19. http://www.masscosh.org/publications/featured-articles/comprehensive-information-covid-19
- McLellan D., Moore W., Nagler E., Sorensen G. (2017). Implementing an integrated approach: Weaving worker health, safety, and well-being into the fabric of your organization. http://centerforworkhealth.sph.harvard.edu/resources/guidelines-implementing-integrated-approach
- McLellan R. K. (2016). Total worker health: A promising approach to a safer and healthier workforce. Annals of Internal Medicine, 165, 294–295. 10.7326/M16-0965 [DOI] [PubMed] [Google Scholar]
- McLeroy K. R., Bibeau D., Steckler A., Glanz K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15, 351–377. 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- Murphy L. A., Robertson M. M., Carayon P. (2014). The next generation of macroergonomics: Integrating safety climate. Accident Analysis & Prevention, 68, 16–24. 10.1016/j.aap.2013.11.011 [DOI] [PubMed] [Google Scholar]
- NationalCOSH (2020). National council for occupational safety and health, coronavirus: Resources for workers. https://nationalcosh.org/coronavirus
- NIOSH (2008). Essential Elements of Effective Workplace Programs and Policies for Improving Worker Health and Wellbeing DHHS (NIOSH) Publication No. 2010-140 . https://www.cdc.gov/niosh/twh/essentials.html
- NIOSH (2020). The National Institute for Occupational Safety and Health (NIOSH) Coronavirus Disease-2019. https://www.cdc.gov/niosh/emres/2019_ncov.html
- OSHA (2012). Injury and illness prevention program: White paper. https://www.osha.gov/dsg/topics/safetyhealth/OSHAwhite-paper-january2012sm.pdf
- OSHA (2020). US Occupational Safety and Health Administration: Guidance on preparing workplaces for COVID-19. https://www.osha.gov/Publications/OSHA3990.pdf
- Pronk N. P. (2013). Integrated worker health protection and promotion programs: Overview and perspectives on health and economic outcomes. Journal of Occupational and Environmental Medicine, 55, S30–37. 10.1097/JOM.0000000000000031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punnett L., Cavallari J. M., Henning R. A., Nobrega S., Dugan A. G., Cherniack M. G. (2020). Defining ‘Integration’ for Total Worker Health®: A new proposal. Annals of Work Exposures and Health, 64, 223–235. 10.1093/annweh/wxaa003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punnett L, Warren N, Henning R, Nobrega S, Cherniack M, Team C.-N, CPH-NEW Research Team (2013). Participatory Ergonomics as a model for integrated programs to prevent chronic disease. Journal of Occupational and Environmental Medicine, 55, S19–S24. 10.1097/JOM.0000000000000040 [DOI] [PubMed] [Google Scholar]
- Quelch J. A. (2020). 7 leadership principles for managing in the time of coronavirus. Working Knowledge. https://hbswk.hbs.edu/item/7-leadership-principles-for-managing-in-the-time-of-coronavirus
- Rivilis I., Van Eerd D., Cullen K., Cole D. C., Irvin E., Tyson J., Mahood Q. (2008). Effectiveness of participatory ergonomic interventions on health outcomes: A systematic review. Applied Ergonomics, 39, 342–358. 10.1016/j.apergo.2007.08.006 [DOI] [PubMed] [Google Scholar]
- Rothan H. A., Byrareddy S. N. (2020). The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity, 109, 102433. 10.1016/j.jaut.2020.102433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothwell J. (2020). A survey of essential workers shows a political divide: Most of them worry about contagion, but there’s a partisan difference in concern levels and workplace safety actions.New York Times. https://www.nytimes.com/2020/04/27/upshot/red-blue-workplace-differences-coronavirus.html.
- Sabbath E. L., Hashimoto D., Boden L., Dennerlein J. T., Williams J. A. R., Hopcia K., Orechia T., Tripodis Y., Stoddard A., Sorensen G. (2018). Cohort profile: The Boston Hospital Workers Health Study (BHWHS). International Journal of Epidemiology, 47, 1739–1740. 10.1093/ije/dyy164 [DOI] [PubMed] [Google Scholar]
- Sauter S., Brightwell S. W., Colligan M. J., Hurrell J. J., Katz T. M., LeGrande D. E., Tetrick L. E. (2002). The changing organization of work and safety and health of working people. Department of Health and Human Services, National Institute for Occupational Health and Safety. [Google Scholar]
- Sorensen G., McLellan D., Dennerlein J. T., Pronk N. P., Allen J. D., Boden L., Okechukwu C. A., Hashimoto D., Stoddard A., Wagner G. R. (2013). Integration of health protection and health promotion: Rationale, indicators, and metrics. Journal of occupational and environmental medicine, 55, S12–18. 10.1097/JOM.0000000000000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G., McLellan D. L., Sabbath E. L., Dennerlein J. T., Nagler E. M., Hurtado D. A., Pronk N. P., Wagner G. R. (2016). Integrating worksite health protection and health promotion: A conceptual model for intervention and research. Preventive Medicine, 91, 188–196. 10.1016/j.ypmed.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G., Sparer E., Williams J. A. R., Gundersen D., Boden L., Dennerlein J. T., Hashimoto D., Katz J. N., McLellan D. L., Okechukwu C. A., Pronk N. P., Revette A., Wagner G. R. (2018). Measuring best practices for workplace safety, health, and well-being: The workplace integrated safety and health assessment. Journal of Occupational and Environmental Medicine, 60, 430–439. 10.1097/JOM.0000000000001286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokols D. (1996). Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion, 10, 282–298. 10.4278/0890-1171-10.4.282 [DOI] [PubMed] [Google Scholar]
- Tamers S., Chosewood L., Childress A., Hudson H., Nigam J., Chang C.-C. (2019). Total worker Health ® 2014–2018: The novel approach to worker safety, health, and well-being evolves. International Journal of Environmental Research and Public Health, 16, 321. 10.3390/ijerph16030321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2020). World Health Organization Coronavirus disease (COVID-19) technical guidance: Guidance for schools, workplaces & institutions. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/guidance-for-schools-workplaces-institutions