Abstract
Objective
The coronavirus disease 2019 (COVID-19) pandemic resulted in significant loss of radiologic volume as a result of shelter-at-home mandates and delay of non-time-sensitive imaging studies to preserve capacity for the pandemic. We analyze the volume-related impact of the COVID-19 pandemic on six academic medical systems (AMSs), three in high COVID-19 surge (high-surge) and three in low COVID-19 surge (low-surge) regions, and a large national private practice coalition. We sought to assess adaptations, risks of actions, and lessons learned.
Methods
Percent change of 2020 volume per week was compared with the corresponding 2019 volume calculated for each of the 14 imaging modalities and overall total, outpatient, emergency, and inpatient studies in high-surge AMSs and low-surge AMSs and the practice coalition.
Results
Steep examination volume drops occurred during week 11, with slow recovery starting week 17. The lowest total AMS volume drop was 40% compared with the same period the previous year, and the largest was 70%. The greatest decreases were seen with screening mammography and dual-energy x-ray absorptiometry scans, and the smallest decreases were seen with PET/CT, x-ray, and interventional radiology. Inpatient volume was least impacted compared with outpatient or emergency imaging.
Conclusion
Large percentage drops in volume were seen from weeks 11 through 17, were seen with screening studies, and were larger for the high-surge AMSs than for the low-surge AMSs. The lowest drops in volume were seen with modalities in which delays in imaging had greater perceived adverse consequences.
Key Words: Adaptations, COVID-19, pandemic, recovery, volume
Background
The coronavirus disease 2019 (COVID-19) pandemic led to shelter-in-place government orders issued to control contagion. In an effort to conserve resources for an anticipated surge in cases, health care systems delayed non-time-sensitive cases, admissions, and imaging. In New York City, Detroit, and Boston, the surge in admitted COVID-19 patients was dramatic. In other cities, capacity was created, yet the anticipated surge of COVID-19 patients did not materialize.
The effect of shelter-in-place orders and delaying imaging and admissions contributed to decreases of up to 87% in the number of inpatient and outpatient imaging examinations [1]. How much of this volume is recoverable and the impact on compensation are not clear [2, 3, 4]. We analyzed volume impacts, responses, and short-term solutions in three high-surge academic medical systems (AMSs), three low-surge AMSs, and a coalition of private radiology practices (Strategic Radiology; https://www.strategicradiology.org). The three low-surge AMSs at their maximum collectively included 128 hospitalized patients positive for COVID-19. Prepandemic volumes across the AMSs ranged from 7,690 studies to 32,190 studies per month. These practices represent the West, Midwest, and Northeast regions of the United States. We share adaptation measures taken, the risks related to such measures, and lessons learned at this early stage.
Materials and Methods and Data Analysis
Descriptive analyses demonstrated the radiology volume during the COVID-19 pandemic in six AMSs (three in high-surge and three in low-surge regions) and a large national private practice coalition. Weekly volume data were obtained by imaging modality and patient class (emergency, inpatient, and outpatient) for the first 21 weeks of 2019 and 2020. Year-over-year percent change (2020 versus 2019) was calculated aggregating data to compare total volume change and for each specific modality (eg, PET-CT, CT, MRI, interventional radiology [IR], breast screening) in (1) high-surge versus low-surge versus practice coalition system and (2) emergency versus inpatient versus outpatient.
Line plots displaying the data, slopes, and 95% confidence intervals for drop and recovery were estimated based on ordinary least-square regression. Decrease rates were calculated from week 11 to week 14, except for breast screening, which was calculated from week 11 to week 13 (because of nonlinearity). Recovery rates were calculated from week 15 to week 21, except for breast screening, which was calculated from week 18 to week 21. Analyses were conducted using statistical software R (version 3.6.1, 2019; http://www.r-project.org), and graphs were produced in Excel version 16.16.22, 2020 (Microsoft Corporation, Redmond, Washington).
Results
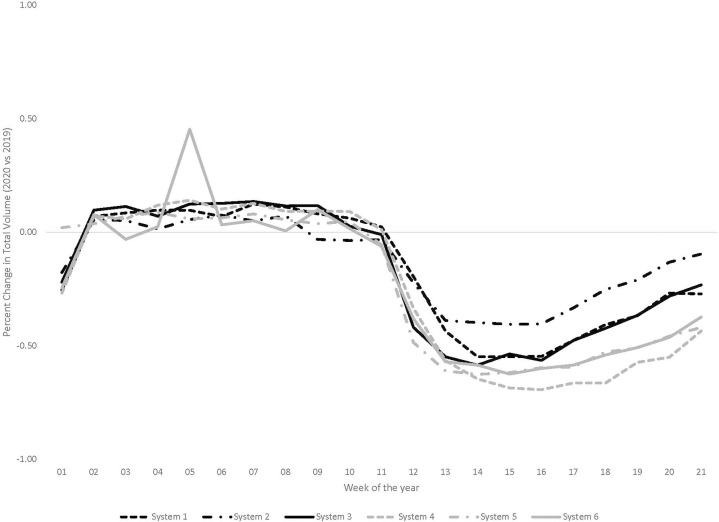
Large drops in volume started in week 11, with recovery beginning in weeks 17 and 18. Total loss in volume was 61% for all AMSs in aggregate at weeks 15 and 16 as shown in Figure 1 (39,461 and 40,156 studies, respectively, compared with 101,637 and 101,495 in weeks 15 and 16 of 2019). Table 1 demonstrates percent drops in volume (2020 versus 2019) by week, in total aggregate, in high-surge AMSs, in low-surge AMSs, and by modality. The high-surge AMSs showed a maximum decrease in volume of 65% in week 15 (26,253 in 2020 versus 75,088 in 2019). The low-surge AMSs showed a maximum decrease in volume of 52% in week 14 (13,558 studies compared with 28,087).
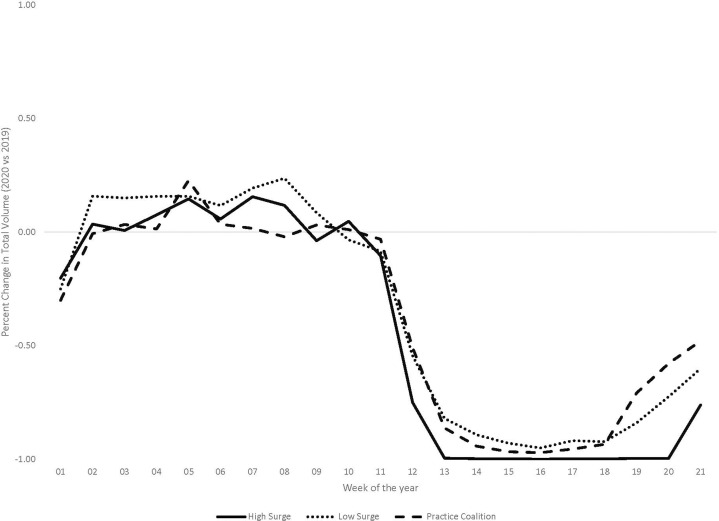
Fig 1.
Volumes of all radiology studies for 2020 calendar weeks 1 to 21 are depicted in this graph showing each of six academic medical systems (AMSs) compared against the prior year’s similar-interval volume as a result of the coronavirus disease 2019 pandemic. The AMSs include three low-surge AMSs (system 1, system 2, and system 3), and three high-surge AMSs (system 4, system 5, and system 6). The lowest-volume AMS, system 2, suffered the least drop in volume and most rapid approach to recovery, and the largest AMS, system 4, suffered the largest drop in volume.
Table 1.
Post-COVID-19 weekly volumes against the prior year’s comparable baselines over the first 21 weeks of 2020 for six AMSs in aggregate, to demonstrate the effects of the COVID-19 pandemic on radiology volumes
 |
The three high-surge AMSs and low-surge AMSs weekly volume changes are separately shown in subsequent columns, as are volumes aggregated by modality for the six combined AMSs. The greatest drops are with breast screening mammography and DEXA scans; the lowest drops were with PET/CT, XR, and IR. AMS = academic medical system; COVID-19 = coronavirus disease 2019; DEXA = dual-energy x-ray absorptiometry; Diag = diagnosis; Fluoro = fluoroscopy; IR = interventional radiology; Nuc = nuclear; Scr = screening; US = ultrasound; XR = x-ray.
The largest AMS suffered the greatest drop in total volume, measuring 70% at its nadir when compared with the prior year’s similar interval; the smallest AMS of those evaluated suffered the lowest drop in total volume, measuring 40%. Largest modality drops, when compared with similar dates of service for the prior year, were seen with all breast modalities with greatest drops in screening examinations, and with dual-energy x-ray absorptiometry (DEXA) scanning. Volume drops in the private practice coalition paralleled the changes seen with the AMSs and tracked with the trends shown by the low-surge AMSs. The modalities with greatest initial drops, such as breast screening mammography and DEXA scanning, also showed the greatest delays in trending toward volume recovery. Similarly, earliest recovery trends were seen with modalities demonstrating lower drops.
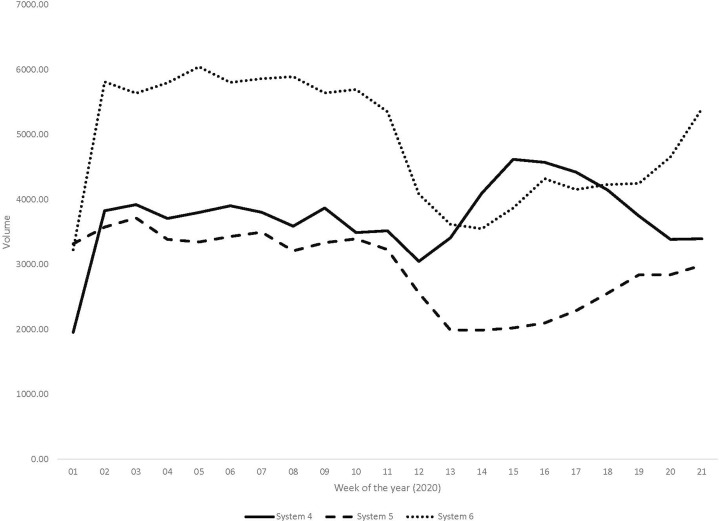
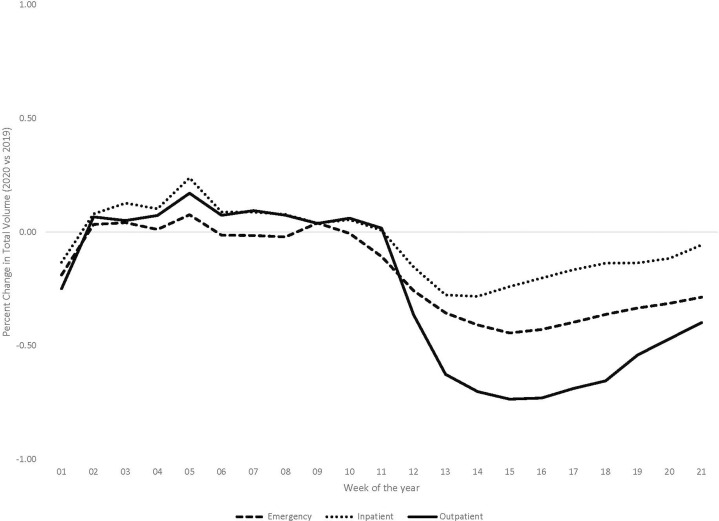
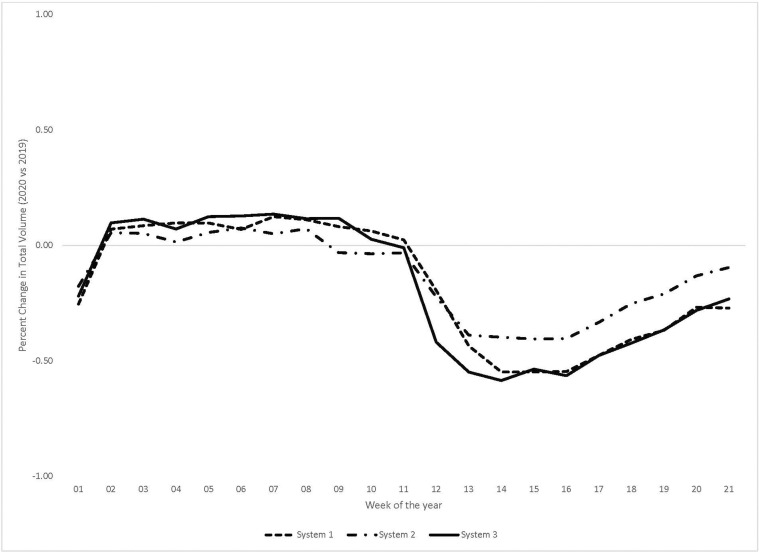
One AMS demonstrated an inpatient volume surge that was greater than baseline as shown in Figure 2 . This was the only AMS to show volume increases significantly above baseline in any modality during the pandemic, was the largest AMS by volume, and was a high-surge AMSs. From week 9 through week 12, a steady decrease in inpatient volume took place, dropping 20% from the previous year, followed by a rapid rise in inpatient volume that increased to 25% greater than the reference interval, sustained from week 14 through week 18, followed by a volume decrease to 6% below the comparison interval. When comparing inpatient, outpatient, and emergency imaging volumes in all 6 AMSs, the greatest drops in volume were seen with outpatient studies by week 15 as shown in Figure 3 . The lowest drops were with inpatient studies, with both inpatient and outpatient volumes recovering more rapidly than emergency imaging.
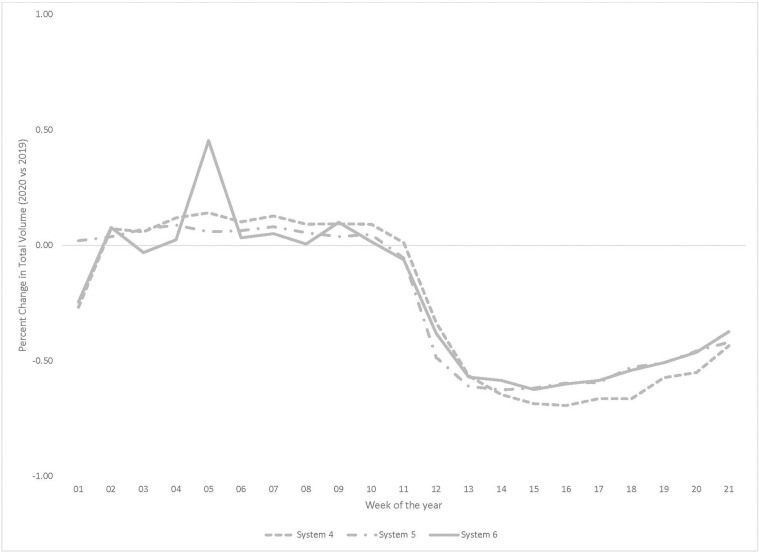
Fig 2.
Inpatient imaging volumes for each of three high-surge academic medical systems (AMSs) are shown. System 4 (solid line), the highest-surge AMS assessed in study, demonstrated a unique increase to supernormal volumes starting week 13, continuing to a new peak at 125% by week 15, with a return to normal levels by week 18. This is in contradistinction to AMS 5 (dashed line) and AMS 6 (dotted line), both of which experienced decreases. No other AMS or modality demonstrated a similar supernormal bump. This volume bump was presumably due to the high-magnitude coronavirus disease 2019 surge and the increased volume of inpatient work resulting from the large number of coronavirus disease 2019 inpatients.
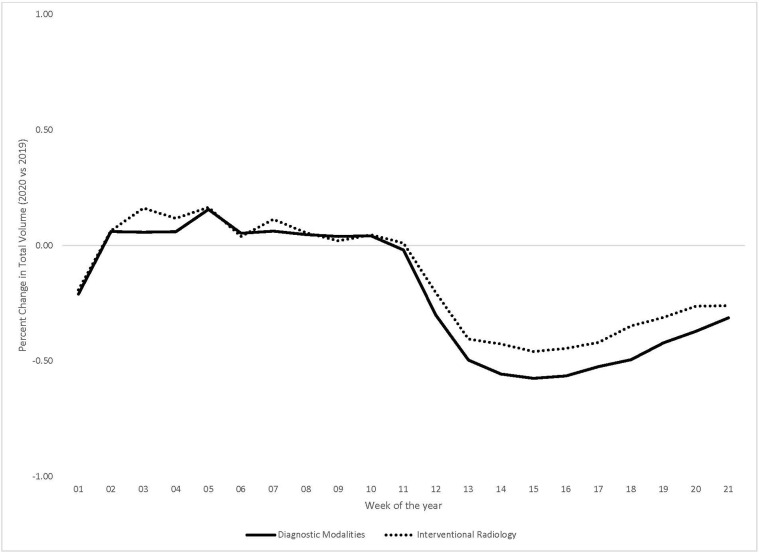
Fig 3.
Volumes for each of three sets of differentiated radiology studies, specifically emergency, outpatient, and inpatient studies, are depicted in this graph showing aggregated data from six academic medical systems (AMSs). The volume is measured against the prior year’s matched-period volume as a result of the coronavirus disease 2019 pandemic for emergency (dashed line), inpatient (dotted line), and outpatient (solid line) imaging studies. The greatest drop in volume was for outpatient studies, and the lowest drop in volume was for the inpatient studies. Both outpatient and inpatients studies demonstrated more rapid recovery slopes toward baseline than the emergency studies, which showed the slowest rate of return toward baseline.
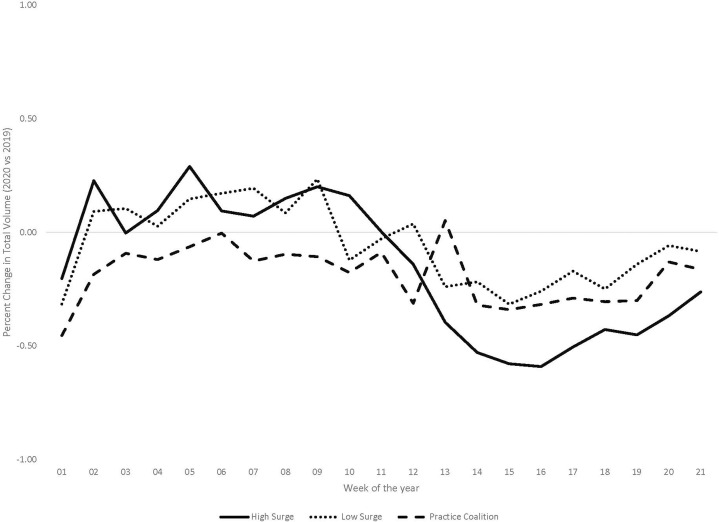
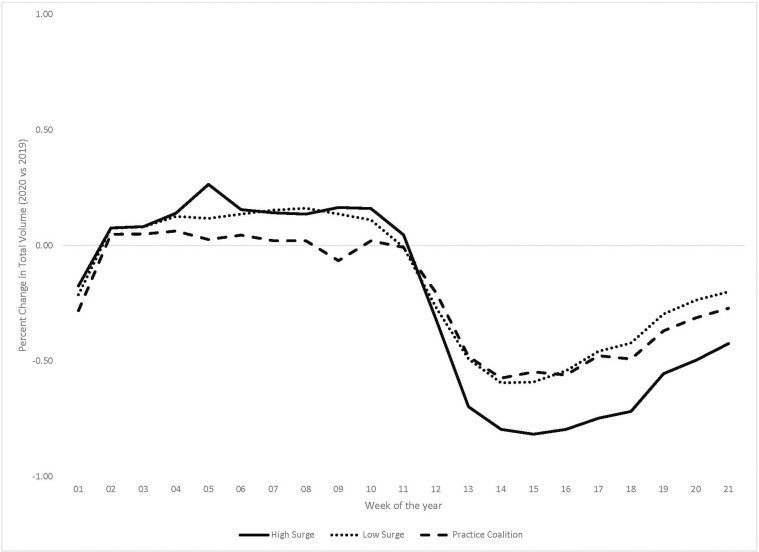
The smallest drops in volume were in the low-surge AMSs, with PET/CT demonstrating the lowest drops to 84% of baseline as shown in Figure 4 . One high-surge system demonstrated the largest drop in PET/CT volume to 33% of baseline resulting from aggressive patient rescheduling. In this same system, PET/CT volume more than doubled from the 33% nadir to 78% by week 21. The least drops in volume by modality in the high-surge AMSs were IR and plain-film x-ray.
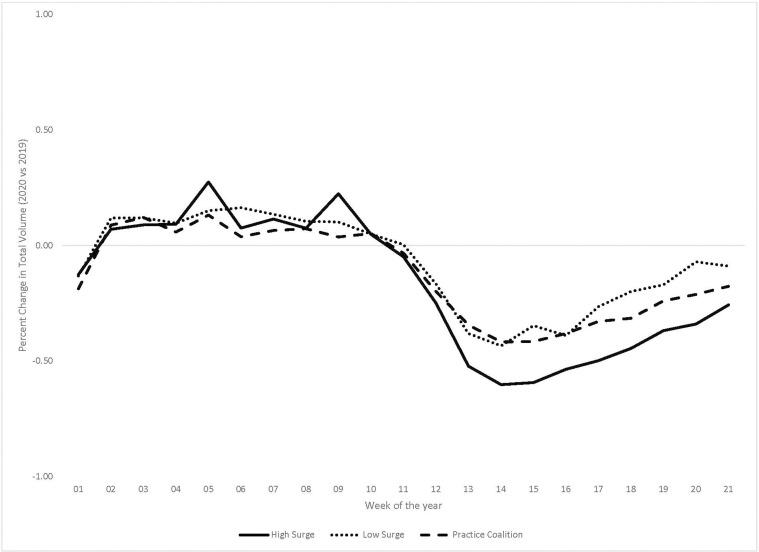
Fig 4.
PET/CT volumes are measured against the prior year’s matched-period volume as a result of the coronavirus disease 2019 pandemic for three high-surge academic medical systems (AMSs; solid line), three low-surge AMSs (dotted line), and a large national private practice coalition (dashed line). The greatest relative drop was seen by the high-surge AMSs, with the low-surge AMSs and the practice coalition showing similar relative drops in volume. PET/CT in the low-surge AMSs demonstrated the least decrease in volume of any modality. Presumably, this is in part related to the high volume of cancer patients undergoing PET/CT studies and patient intolerance for the effect that delays in care including delayed PET/CT imaging could potentially have on their survival.
The drop in total breast screening volume was 99% at its nadir in weeks 15 and 16 as shown in Figure 5 (152 studies versus 12,027 studies in 2019); similarly, DEXA scanning dropped 99% in weeks 15 and 16 (35 studies versus 3,003 studies in 2019). The maximum total volume drop in AMSs for IR was 53% in week 14 (1,077 versus 2,306 studies in 2019). The greatest volume drop for plain-film x-ray was 51% in weeks 15 and 16 (43,165 studies versus 87,689 studies in 2019). The large drops in screening breast and DEXA examinations [5] underline screening perceived as delayable and nonurgent. X-ray and IR volume decreases experienced by the low-surge AMSs were less drastic although greater drops than with PET/CT.
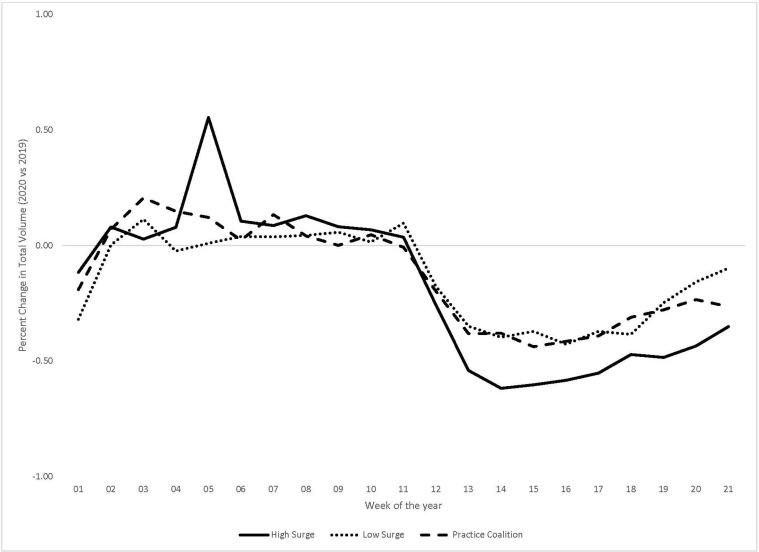
Fig 5.
Breast screening study volumes are measured against the prior year’s matched-period volume as a result of the coronavirus disease 2019 pandemic for three high-surge academic medical systems (AMSs; solid line), three low-surge AMSs (dotted line), and a large national private practice coalition (dashed line). Precipitous drops in volume were seen across the board in all three types of systems. Presumably, this is related to the screening or elective nature of such studies, in which delays in imaging, on the order of months, is likely seen to be of little medical consequence. The greatest delays in establishing a recovery slope was seen with high-surge AMSs, which showed an approximately 7-week period at nadir, before initiation of a recovery slope.
Discussion
Despite long-standing imaging volume increases [6] and our expectation to lead imaging as a robust specialty for the foreseeable future [7], the pandemic volume consequences may affect radiology incomes, cause a downturn in radiology residency applicants as followed the recession of 2008, and accelerate consolidation of practices [8]. These issues are beyond the scope of our report. Our intent was to specifically focus on (1) adaptations implemented as corrective measures; (2) risks of the actions taken; and (3) lessons learned that are applicable in the next pandemic or economic stressor.
Adaptations
Within the first wave of the COVID-19 pandemic, we cannot accurately estimate the cumulative pandemic effect; 40% to 70% drops in volume were seen from week 11 through 17 with the COVID-19 pandemic and the shelter-at-home mandates. The drops were larger for high-surge systems than for low-surge systems.
Financial adaptations considered included radiologist and staff bonus holdbacks, compensation reductions, reductions in retirement matches, layoffs of part-time and contract faculty, and furloughs as time off without pay. AMS departments may choose to utilize reserve accounts for salary. In private practices, revenue is ordinarily distributed in the form of income to avoid double taxation. In addition to having an established robust line of credit, after the pandemic, private practices may want to explore other approaches to optimize addressing future unexpected reserve case shortages. It is feasible that after the pandemic, well-resourced buyers could take full advantage of a buyer’s market [9]. Capital equipment budgets will most likely be trimmed.
Additional frugality measures include stopping open searches and reducing unfunded research and administrative time. Furloughs may affect staff radiologists and delay start dates for new hires. As we gain a better understanding of at-risk volume for future instances, modality-specific staffing may be considered. As an example, if IR volume is expected to decrease 15% for a 7-week stretch and breast imaging volume is expected to decrease 70% for a 7-week stretch, furloughs may be applied by modality and demand.
For ongoing expense control, the pandemic has demonstrated the possibility for remotely placing nonclinical support staff. During the shelter mandates, scheduling, billing, and management employees telecommuted from home, showing that we may not need the prepandemic footprint. Much of the nonclinical staff could move to less expensive space, telecommuting a percentage of the time. Efforts are directed at maximizing capacity through efficiency to recover lost volume and revenue, while working through large backlogs. One of our AMSs has shortened routine MRI examinations to 7 min of scanning time, allowing slots of 20 to 25 min in length. As we maximize capacity, gains are offset by waiting room distancing and increased slot times for cleaning reducing efficiency. We recognize the need to develop a more robust digital platform for patients, also helping minimize waiting room utilization.
Risks of Actions
In areas in which high rates of COVID-19 contagion were suspected, telecommuting allowed preservation of radiologists by minimizing infection risks within the work setting [10]. In some instances, departments chose to half-staff with A and B teams, preserving half of the team as a reserve group as the other half served on site. Simultaneously, in AMSs also physically separating attending physicians from resident physicians, most practices created distancing by depopulating reading rooms [11]. This displacement outside of the formerly congregational reading rooms resulted in security and safety for the radiologists, while also having the unfavorable consequence of greater isolation.
Telecommuting results in increased distance from colleagues and coworkers and decreased visibility as far as clinicians and patients are concerned [12]. An unfavorable by-product of radiologist distancing at work and by telecommuting may be the impression of radiologists utilizing technologists, nurses, and residents as human shields while maximizing radiologists’ physical perimeter. The optics are potentially damaging in the long term for the larger radiology team beyond radiologists and may counteract loyalty and high-performance interdependence. Conversely, remote reading can be a valuable tool to improve radiologist morale and wellness with no loss of integration with trainees in the academic practice setting and technical staff so long as careful attention is paid to ensuring that a critical mass of radiologists is always on site.
Risks of action include implementation of fair financial adjustments. One example is the just application of financial restraint measures; another is the need to assume only an equitable share of health system pain. In applying just restraint measures, it may be necessary to consider disproportionate measures. Frontline caregivers such as interventional radiologists and technologists who are exposed to contagion in carrying out their mission should perhaps receive consideration from facing identical decreases in compensation tolerated by individuals who relocated to home by choice or inadequate work volume. It is the responsibility of radiology leadership to ensure that the share of health system pain is not disproportionately shouldered by radiology. Just because radiologists are able to telecommute, it should not be the case that we have to endure unfair wage adjustments.
Lessons Learned
In the United States, radiology volumes began a slow recovery starting approximately in week 15. Although straight-line extrapolation suggests an intersection of current total imaging growth with 100% pre-COVID-19 numbers at or near week 33, there is inadequate confidence in extrapolating such a recovery to 100% of the pre-COVID-19 expected volumes. Because of possible future second waves or regional outbreaks, the recovery trend may slow down or potentially flatten over time. External factors such as downturns in the economy and broader usage of competitive telehealth may also affect volume recovery. In addition, until a vaccine is available, some populations may be reluctant to return to their usual way of life. Therefore, it is premature to extrapolate a full 100% recovery in practice volumes based on the observed linear trend from weeks 15 to 21.
Lower pandemic-related volume drops were seen with PET/CT imaging in the low-surge AMSs and x-ray and IR in our high-surge AMSs. When relative preservation of PET/CT volume was demonstrated, it may in part be related to both the significant warranted anxiety experienced by cancer patients, in concert with their need for treatment continuation, despite the greater dangers these same patients faced if they contracted COVID-19 in public spaces and health care facilities. A similar sense of treatment urgency may well apply to patients scheduled for IR studies, explaining the relatively lesser drops in IR volume. The perceived disadvantages of delaying such examinations may affect ongoing financial performance if we are facing multiple future short- and long-term COVID-19 resurgences. With plain-film x-ray, the relative volume preservation may well have been related to the increased plain-film volume experienced in areas in which COVID-19 also hit the hardest, as was the case with the high-surge AMSs, an example including anticipated larger than average numbers of chest x-rays in high-surge areas.
Another set of lessons learned may relate to temporary physical distancing from each other and clinicians, reminding us to direct increased attention toward the radiologist-to-clinician relationship. Receiving a report with an electronic signature from a radiologist a referring clinician has not met is not effective in building trust necessary for a branding strategy. This realization follows that of industry sectors that have ended or reduced remote-work arrangements [13,14].
Radiology practices across the country are financially vulnerable to this pandemic as a direct result of the dominant fee schedule payment and practice structures in place today. Such structural challenges are fundamental and are not simple to address. As one example, in the COVID-19 pandemic we are seeing in part the unique vulnerability of our fee-for-service model, in which our dependency on per-transaction revenue when combined with shelter-at-home created a perfect storm. Alternatively, vertically integrated systems may weather the storm with less losses as they continue collecting unchanged member subscription fees on a continuing basis, while simultaneously incurring diminished imaging expenses. Correcting this vulnerability is not simple.
We sought to identify potential durable changes after the pandemic, from necessary or accidental measures we implemented in the pandemic that we recognize should in large part revert to a prepandemic state once possible [15,16]. The potentially durable adaptations that have been implemented with the pandemic may include a host of operational, architectural, and strategic changes. Operational changes will likely include expanded hours, staggered radiologist shifts, and shorter MRI protocols. Architectural changes will include remote placement of nonclinical staff and redesigned reading rooms. Strategic changes will include novel partnerships.
Another lesson learned relates to the vulnerability we have as individual and to some degree clinically isolated systems. Perhaps robust and interconnected imaging delivery systems could allow us to flex up and down to share radiologists across systems for capacity needs. If an AMS in Seattle is hit first in a pandemic with a flood of chest-imaging COVID-19 cases, simultaneously with San Diego emptying non-time-sensitive cases in anticipation of a pandemic wave, perhaps San Diego could be of assistance and with the right infrastructure could lend a hand with distance interpretations as it experiences low imaging volumes while awaiting its own pandemic wave. In reverse, when such a wave hits San Diego, if Seattle is over the apex of its pandemic wave, it could return the favor. Such network efficiencies could partially blunt downside challenges if networks are sufficiently broad to include adequate geographic distances, because pandemics may occur in asynchronous waves in distant locations.
There is potentially much to be learned from comparing distributed practice models with a broader footprint with centralized practice models. In the case of AMSs that we evaluated, the largest AMS examined was a high-surge AMS including multiple hospitals and a very large number of outpatient imaging centers that happened to be hit particularly hard by COVID-19 and shelter-at-home orders. When looking at a typical highly decentralized system with multiple point-of-care sites of service, there is an extraordinary drop in volume as a result of shelter-at-home orders with accompanying stalling of revenue flow. A narrow-footprint practice with a pure inpatient focus may demonstrate a different type of pandemic vulnerability with shelter-at-home orders leading to declining and restrictive non-time-sensitive admissions, resulting in inpatient census drops, rather than suffering principally from declining ambulatory visits in a principally outpatient model. Even if a major COVID-19 surge is experienced, there is still a relative loss of revenue as high-margin elective surgical charges are replaced by lower margin medicine and ICU admissions.
In locales where the COVID-19 surge is controlled or low and flat, when there is a shelter-at-home mandate, there is even less bed occupancy because of a lack of COVID-19 volume. The highly decentralized system may in the longer term more quickly recover volume with extended hours and shifts, capitalizing more fully on its greater capacity and adaptation to environmentally driven referral pattern changes. This same flexibility allows the typical highly decentralized system to possess greater profitability with the right payer mix, allowing it to generate greater overage in the first place, with the resultant ability to effectively generate a disaster or rainy-day reserve safety cushion.
Limitations
Our study is limited by the short 21-week interval utilized for data gathering, with only a short period of recovery permitting extrapolation to baseline. We recognize this is a preliminary report and intend longer-term follow-up to confirm the trends over a longer interval and ideally to include a recovery cycle.
Our study is also limited by the relatively small number of seven systems contributing data; we hope to secure data from a larger number of AMSs and practices as part of a longer-term study, to secure greater statistical significance for our conclusions.
An additional limitation of our study is measuring 2020 weekly intervals solely against 2019; any single-year irregularities in 2019 would reflect on the assessment. Our future studies will seek a more comprehensive aggregation of several past reference years to accommodate for this variable; we were unable to assemble multiple years of data given our intent to expediently generate this preliminary report.
Take-Home Points
-
▪
Adaptations to both the volume drops and preserving safety included frugality measures, moving clinical and nonclinical staff off site, and maximizing operational efficiency to the extent possible.
-
▪
Risks of actions taken included fragmenting teams by separating members and moving them off site, in addition to ensuring that fairness was utilized when frugality and financial adjustments were necessitated.
-
▪
Lessons learned included the vulnerability and disproportionately large drops for screening studies such as screening breast mammography and DEXA scanning when compared with critical studies such as PET/CT and plain-film x-ray.
-
▪
Large percentage drops in volume were seen from week 11 through 17 and 18 with the COVID-19 pandemic and the shelter-at-home mandates. The drops in volume were larger for high-surge AMSs than for the low-surge AMSs, and parallel changes were seen in the larger economy.
-
▪
The largest uniform drops in volume were seen with screening modalities such as breast screening examinations and DEXA scanning, which demonstrated greatest sustained decreases in volume of up to 99%.
-
▪
There were lesser drops in volume for PET/CT in the low-surge AMSs, and IR and plain-film x-ray in the high-surge AMSs; these lesser drops suggest greater study value or necessity during or despite the COVID-19 pandemic.
Acknowledgments
The authors thank and acknowledge the Society of Chairs of Academic Radiology Departments (SCARD) COVID writing taskforce for their guidance in the planning and development of this manuscript: Dr Jennifer Harvey, MD, Dr Max Rosen, MD. The authors also thank and acknowledge the many member practices of Strategic Radiology who contributed the data utilized in the generation of this manuscript, in addition to Mr David Polmanteer, Director of Analytics and Business Intelligence for Strategic Radiology, Mr Devin Dixon of University of California San Francisco, Mr Dan Alexa of New York University, Mr Josie Palazzollo of the Henry Ford Hospital, and Mr Kevin Pian of the Massachusetts General Hospital for centralizing, compiling, and sharing the contributed data.
Footnotes
Dr Norbash reports personal fees from GE, Siemens, Penumbra, Stryker, IBM, and stock with Boston Imaging Core Laboratories, outside the submitted work. Dr Brink reports personal fees from Accumen, Inc, outside the submitted work. Dr Hess reports personal fees from General Electric, Siemens Healthineers, Focused Ultrasound Foundation, and the RSNA, outside the submitted work. The other authors state that they have no conflict of interest related to the material discussed in this article. Dr Norbash, Dr Moore, Dr Recht, Dr Brink, Dr Hess, Mr Won, Dr Jain, Dr Sun, Dr Brown, and Dr Enzmann are nonpartner, non–partnership track employees.
Additional Resources
Additional resources can be found online at: https://doi.org/10.1016/j.jacr.2020.07.001.
Additional Resources
Supplementary Figure 1a.
Supplementary Figure 1b.
Supplementary Figure 2.
Supplementary Figure 3.
Supplementary Figure 4.
Supplementary Figure 5.
References
- 1.Naidich J.J., Boltyenkov A., Wang J.J., Chusid J., Hughes D., Sanelli P.C. Impact of the COVID-19 pandemic on imaging case volumes. J Am Coll Radiol. 2020;17:865–872. doi: 10.1016/j.jacr.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stempniak M. 4 steps radiology providers can take to return from “COVID-19 induced imaging austerity.” Radiology Business. https://www.radiologybusiness.com/topics/healthcare-economics/jacr-radiology-covid-19-pandemic-imaging-austerity?utm_source=newsletter&utm_medium=rb_news Available at: Published May 5, 20202. Accessed July 28, 2020.
- 3.Page L. COVID-19: what will happen to physician income this year? Medscape. https://www.medscape.com/viewarticle/930434 Published May 13, 2020.Available at: Accessed July 28, 2020.
- 4.Lee C.I., Raoof S., Patel S.B. Coronavirus disease 2019 (COVID-19) and your radiology practice: Case triage, staffing strategies, and addressing revenue concerns. J Am Coll Radiol. 2020;17:752–754. doi: 10.1016/j.jacr.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stempniak M. Cancer screenings drop upward of 94% during pandemic, with concerns of lingering sluggishness. https://www.radiologybusiness.com/topics/healthcare-economics/cancer-screenings-epic-ehr-covid-19-coronavirus?utm_source=newsletter&utm_medium=rb_news Available at: Published May 4, 2020. Accessed July 28, 2020.
- 6.Smith-Bindman R., Migloretti D.L., Larson E.B. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood) 2008;27:1491–1502. doi: 10.1377/hlthaff.27.6.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wikipedia The infinite game. https://en.wikipedia.org/wiki/The_Infinite_Game Available at: Accessed July 28, 2020.
- 8.Fleishon H.B., Vijayasarathi A., Pyatt R., Schoppe K., Rosenthal S.A., Silva E., 3rd White paper: corporatization in radiology. J Am Coll Radiol. 2019 doi: 10.1016/j.jacr.2019.07.003. 16):1364-1374. [DOI] [PubMed] [Google Scholar]
- 9.Ross J.R. COVID or not, big money is buying radiology practices. should yours be selling? Radiology Practice. https://www.radiologybusiness.com/topics/radiology-practice/covid-or-not-big-money-buying-radiology-practices-should-yours-be-selling?utm_source=newsletter&utm_medium=rb_news Available at: Published April 29, 2020. Accessed July 28, 2020.
- 10.Davarpanah A.H., Mahdavi A., Sabri A. Novel screening and triage strategy in iran during deadly coronavirus disease 2019 (COVID-19) epidemic: value of humanitarian teleconsultation service. J Am Coll Radiol. 2020;17:734–738. doi: 10.1016/j.jacr.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen R.C., Cheng L.T.E., Lim J.L.L. Touch me not: safe distancing in radiology during coronavirus disease 2019 (COVID-19) J Am Coll Radiol. 2020;17:739–742. doi: 10.1016/j.jacr.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Slanetz P.J., Parikh U., Chapman T., Motuzas C.L. Coronavirus disease 2019 (COVID-19) and radiology education—strategies for survival. J Am Coll Radiol. 2020;17:743–745. doi: 10.1016/j.jacr.2020.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simon J. Employers pull plug on remote work. Wall Street Journal, July 26, 23017, B1.
- 14.Simons J. IBM, a pioneer of remote work, calls workers back to the office: Big Blue says move will improve collaboration and accelerate the pace of work. Wall Street Journal. https://www.wsj.com/articles/ibm-a-pioneer-of-remote-work-calls-workers-back-to-the-office-1495108802 Available at: Published May 18, 2017. Accessed July 28, 2020.
- 15.Davenport M.S., Bruno M.S., Iyer R.S. ACR statement on safe resumption of routine radiology care during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Radiol. 2020;17:839–844. doi: 10.1016/j.jacr.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baur A., Georgiev P., Munshi I.R., Stepniak M. Healthcare providers: preparing for the next normal after COVID-19. McKinsey & Company. https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/healthcare-providers-preparing-for-the-next-normal-after-covid-19 Available at: Accessed July 28, 2020. Published May 8, 2020.