Abstract
Objectives
This study explored the factors influencing health behaviours during the coronavirus disease 2019 (COVID-19) outbreak in China. The impact of perceived stress and positive perception of interventions on health behaviours in China were assessed using the extended information-motivation-behaviour skills (IMB) model.
Study design
Cross-sectional survey.
Methods
The Questionstar online survey tool was used to construct a structured questionnaire based on the IMB model. Between 14 and 22 February 2020, during the peak of COVID-19 epidemic in China, 2449 participants were recruited by snowball sampling on WeChat and Tencent QQ social media platforms in China. Data were collected through an online questionnaire, and structural equation modelling was performed to evaluate the extended IMB model.
Results
Health behaviours were assessed using a scoring system (total score range: 8–40); the average health behaviour score in this study was 34.62 ± 4.44. The term ‘health risk stress’ refers to the impact that perceived stress has on health, and this was experienced by 39.9% of participants. Only 35.9% of participants answered all seven questions on COVID-19 information correctly. The final model showed that information, motivation, behavioural skills, heath risk stress and positive perception of interventions had significant direct effects on health behaviours. Health behaviours were positively associated with the positive perception of interventions but negatively associated with health risk stress. Behavioural skills had the greatest impact on health behaviours.
Conclusions
In the face of public health emergencies, the extended IMB model has been used as a theoretical framework to construct more effective interventions. The government should pay attention to publicity and guidance, strengthen positive interactions with the public and disclose relevant information in a timely manner to gain trust and to maintain the positive public perception of the interventions. In terms of health education, the government should focus on behavioural skills, promptly rectify ineffective prevention information and raise awareness about the disease to relieve stress and anxiety in the population.
Keywords: Information-motivation-behaviour skills model, COVID-19, Health behaviours, Perceived stress
Highlights
-
•
Information, motivation, behavioural skills and positive perception of interventions were positive factors on health behaviours.
-
•
Health risk stress (i.e. the impact that perceived stress has on health) was negative factor on health behaviours.
-
•
Behavioural skills were the most important factor influencing health behaviour.
-
•
Of all residents, 39.9% of residents experienced health risk stress.
Introduction
On 30 January 2020, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 as the sixth public health emergency of international concern.1 As of 14 June 2020, there were 7,690,708 confirmed cases and 427,630 deaths worldwide.2 WHO risk assessment is very high. In addition to public health, COVID-19 poses a serious threat to global economic and social development.
To curb the development of the epidemic to the greatest extent, the Chinese government and other relevant departments concentrated their medical resources on the treatment of infected persons and adopted a series of comprehensive prevention and control measures based on the principles of controlling transmission sources, cutting off transmission routes and protecting vulnerable populations.3 At the same time, relevant departments and organisations released timely and accurate information about COVID-19, actively carried out health education and provided residents with authoritative, detailed and specific operational prevention and control guidelines.3 In addition, it was very important for residents to follow the instructions, adopt appropriate health behaviours and maintain good health habits, such as correctly wearing a mask and avoiding outings or gatherings. These measures help to control the epidemic and reduce the risk of infection.
The aforementioned prevention strategy is consistent with the theory of the information-motivation-behaviour skills (IMB) model, which classifies the factors affecting the occurrence and changes of preventive behaviour into three components of information, motivation and behaviour skills.4 IMB is a well-proven method that can predict and promote health behaviours.5 It has been widely used in AIDS prevention,6 , 7 health promotion,8 , 9 public health,10 , 11 chronic disease management,12 , 13 vaccination5 and other fields. The IMB model can be easily converted into intervention practice and has broad applicability.
This study adds two factors to the original IMB model—perceived stress and positive perception of interventions. Stress and anxiety in the population tends to increase during public health emergencies,14 which may have a negative impact on health behaviours. In addition, residents’ positive perception of government interventions could also have an effect on health behaviours, such as the degree of understanding and support of intervention measures.
Therefore, based on the extended IMB model, this study explores the factors influencing Chinese residents’ health behaviours during the COVID-19 outbreak, and assesses the impact of perceived stress and positive perception of interventions on health behaviours. The results of this study provide scientific basis for relevant departments and institutions to establish targeted comprehensive intervention programmes and prevention measures.
Methods
Study design and participants
This study collected data via a cross-sectional survey. Questionstar, an online survey questionnaire tool, was used to prepare a structured questionnaire that was guided by the IMB model. Between 14 and 22 February 2020, corresponding with the peak of the epidemic in China, the snowball sampling method was used to recruit participants on WeChat and Tencent QQ social media platforms in China. Data were collected through an online questionnaire. Each participant could become a ‘seed’ and expand the sample size by sharing the questionnaire with their social network. Participants were required to read the informed consent and agree to participate before gaining access to the questionnaire to complete. Inclusion criteria were as follows: (1) aged ≥18 years old; (2) ability to use smart electronic devices (e.g. computers, tablets, mobile phones); and (3) agree to participate in this study (i.e. provide informed consent). Exclusion criteria were as follows: (1) suffering from a mental health illness (such as anxiety neurosis or depression) in the past year; and (2) response times of <1 min or >30 min.
Quality control
To reduce bias, the following quality control was carried out: (1) each item was set as a mandatory question to ensure the integrity of the data; (2) each internet protocol address was limited to one submission to avoid repeated filling/participation; and (3) real-time monitoring in the background recorded participants’ response time.
Measures
We developed structured questions by referring to relevant literature relating to the IMB model4 , 5 , 15 and studies on health behaviours during infectious disease outbreaks,16 , 17 the WHO and the National Health Council of the People's Republic of China on the prevention of COVID-19.18 , 19 After a pilot test of the survey, we revised and optimised the items based on the opinions of participants and finalised the contents of the questionnaire.
Demographic variables
Demographic characteristics included age, gender, education level, marital status, personal monthly income, region, province of residence, occupation and past history of mental health illness.
Knowledge/information
This section of the questionnaire included knowledge about the COVID-19 incubation period, transmission and prevention, with a total of seven items (Table 1 , I1-I7). As the survey questions included incorrect information/rumours about disease, the correct answers were revealed after submitting the questionnaires. Possible answers to items I1–I7 were ‘Yes’, ‘No’ and ‘I don't know’. Items I1–I4 were assigned one point for ‘No’, items I5–I7 were assigned one point for ‘Yes’, other answers were assigned 0 points. Cronbach's alpha = 0.607.
Table 1.
Constructs of the extended information-motivation-behavioural skills (IMB) model.
| Constructs | Items | |
|---|---|---|
| Information (Crobach's α = 0.607) |
I1 | Could antibiotics prevent COVID-19? |
| I2 | Could taking Shuanghuanglian oral liquid prevent COVID-19? | |
| I3 | Could a room fumigated with vinegar kill SARS-CoV-2? | |
| I4 | Could gauze masks or activated carbon masks prevent COVID-19? | |
| I5 | Could hot water at 56 °C kill SARS-CoV-2 for 30 min? | |
| I6 | In general, is the longest incubation period for COVID-19 14 days? | |
| I7 | Is the main transmission method of COVID-19 by droplet transmission and contact transmission? | |
| Motivation (Crobach's α = 0.558) |
M1 | I thought COVID-19 was very contagious. |
| M2 | Taking appropriate health behaviours could reduce the risk of infection. | |
| M3 | I was very afraid of COVID-19. | |
| M4 | I thought COVID-19 was serious. | |
| M5 | My family was very supportive of my health behaviours. | |
| M6 | I was aware of any confirmed or suspected cases of COVID-19 within a radius of 1 km. | |
| Behavioural skills (Crobach's α = 0.774) |
BS1 | I actively paid attention to real-time information of COVID-19. |
| BS2 | I understood the importance of home isolation during the COVID-19 pandemic. | |
| BS3 | I grasped the difference between a common cold and COVID-19. | |
| BS4 | I could put on the mask correctly. | |
| BS5 | I could take temperature correctly. | |
| BS6 | I could follow community or village committee regulations. | |
| BS7 | I took the initiative to learn preventive measures for COVID-19. | |
| BS8 | Even though the supply of masks and disinfectants was insufficient, I still actively tried to acquire them. | |
| Health behaviours (Crobach's α = 0.835) |
HB1 | Advise family members to wash their hands frequently, wear masks, etc. |
| HB2 | Wash hands frequently at home. | |
| HB3 | Reduce group activities like outings and gatherings. | |
| HB4 | Keep a safe distance from strangers when going out (at least 1 m). | |
| HB5 | Cover mouth and nose with a tissue or elbow when coughing or sneezing to avoid possible transmission to others. | |
| HB6 | Wear a mask when going out. | |
| HB7 | Implement a healthier diet to improve nutrition level. | |
| HB8 | Perform appropriate exercises at home. | |
| HB9 | Pay attention to opening of windows to ventilate the home (at least twice a day). | |
| Perceived stress (Crobach's α = 0.829) |
PS1 | In the past month, how often have you successfully dealt with day-to-day problems and annoyances? |
| PS2 | In the past month, how often have you felt that you were coping effectively with important changes that were occurring in your life? | |
| PS3 | In the past month, how often have you felt confident about your ability to handle your personal problems? | |
| PS4 | In the past month, how often have you felt anxious about something that happened unexpectedly? | |
| PS5 | In the past month, how often have you felt unable to control the important things in your life? | |
| PS6 | In the past month, how often have you felt nervous and ‘stressed?’ | |
| PS7 | In the past month, how often have you found that you could not cope with all the things that you had to do? | |
| PS8 | In the past month, how often have you felt that things were going your way? | |
| PS9 | In the past month, how often have you been angered because of things that happened outside of your control? | |
| PS10 | In the past month, how often have you found yourself thinking about things that you have to accomplish? | |
| PS11 | In the past month, how often have you been able to control irritations in your life? | |
| PS12 | In the past month, how often have you felt that you were on top of things? | |
| PS13 | In the past month, how often have you felt difficulties were piling up too high to overcome them? | |
| PS14 | In the past month, how often have you been able to control the way you spend your time? | |
| Positive perception of interventions Crobach's α = 0.890 |
PPI1 | Prevention and control measures increased my confidence. |
| PPI2 | I understand the prevention and control management measures. | |
| PPI3 | I supported prevention and control management measures such as closed management. | |
| PPI4 | Prevention and control measures could reduce my fear and anxiety. | |
| PPI5 | Prevention and control measures could prevent me and my family contracting COVID-19. |
COVID-19, coronavirus disease 2019.
Motivation
The motivations of participants towards their health behaviours were mainly divided into individual motivation and social motivation, which were measured by six items (Table 1, M1-M6). Participants answered using a five-point Likert scale, ranging from 1 (completely disagree) to 5 (completely agree). The higher the score, the higher the motivation. Cronbach's alpha = 0.558.
Behavioural skills
Self-efficacy and the ability to effectively execute health behaviours were used to evaluate behavioural skills, with a total of eight items (Table 1, BS1-BS8). Participants answered using a five-point Likert scale, ranging from 1 (completely disagree) to 5 (completely agree). The higher score, the more the behavioural skills related to the health behaviours. Cronbach's alpha = 0.774.
Perceived stress
Perceived stress was measured to evaluate the degree of stress caused by factors considered to be unpredictable or uncontrollable, or that were overwhelming.20 The Chinese version of the Perceived Stress Scale was used in this study,17 with a total of 14 items (Table 1, PS1-PS14), of which PS4, PS5, PS6, PS7, PS9, PS10 and PS13 were reverse items. Participants answered using a five-point Likert scale, ranging from 1 (never) to 5 (always). The higher the score, the greater the perceived stress of residents during the COVID-19 epidemic. When the total score was higher than 25, the perceived stress would impact health, which was defined as ‘health risk stress’.17 Cronbach's alpha = 0.829.
Positive perception of interventions
Positive perception of interventions refers to residents' perceptual evaluation of the government's epidemic prevention and control measures, with a total of five items (Table 1, PPI1-PPI5). The main contents were on understanding, support and evaluation of the policies. Participants answered using a five-point Likert scale, ranging from 1 (completely disagree) to 5 (completely agree). The higher the score, the higher the positive perception of interventions. Cronbach's alpha = 0.890.
Health behaviours
Health behaviours included prevention of infection of COVID-19, a healthy diet and appropriate exercise, with a total of nine items (Table 1, HB1–HB9). Participants answered using a five-point Likert scale, ranging from 1 (never) to 5 (always). The higher the score, the higher the frequency of positive health behaviours. Cronbach's alpha = 0.835.
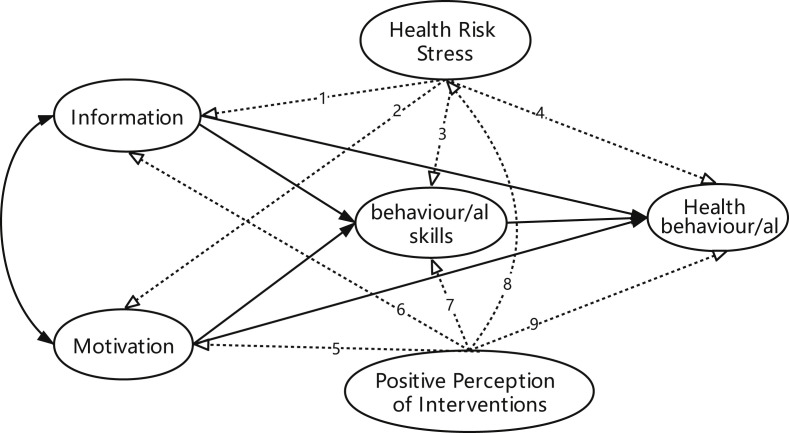
The extended IMB model
In Fig. 1 , the original IMB model is represented by solid lines, and the nine paths added in the study are represented by the dotted lines. Paths 1–4 were used to evaluate the positive impact of positive perception of interventions on health behaviours, and paths 5–8 were used to estimate the negative impact of perceived stress on health behaviours.
Fig. 1.
The extended IMB model in present study. IMB, information-motivation-behaviour skills.
Statistical analyses
Statistical analyses were completed using SAS9.4. The measurement data of normal distribution were reported by mean ± standard deviation, and the count data were reported by frequency (N) and percent (%). The Pearson correlation coefficient and point double correlation coefficient were used to estimate the correlation between variables. Confirmatory factor analysis (CFA) was used to test the relationship between latent variables and observable variables of the measurement model. In each measurement model, when the factor loading of an item was not statistically significant (P > 0.05) or the standardised factor loading estimate was less than 0.4, the item was deleted. Structural equation modelling (SEM) was used to evaluate the extended IMB model. The model was considered to have a good fit if the ratio of chi-square to degrees of freedom was <5.021, root mean square error of approximation (RMSEA) < 0.08, goodness-of-fit index (GFI) ≥0.90, Tucker–Lewis index (TLI) ≥0.90 and comparative fit index (CFI) ≥0.90.22 SEM and CFA were conducted using Amos 24.0. Bilateral P < 0.05 considered the difference to be statistically significant.
Results
Sociodemographic characteristics
In total, 2533 participants completed the questionnaires; 2449 of these were valid. Table 2 shows the sociodemographic characteristics of the study participants. The majority of the participants were under the age of 40 years (70.5%), female (66.4%), employed (74.9%), with a personal monthly income <5000 RMB (70.4%) and lived in urban areas (72.8%). Most of the respondents (75.2%) came from Chongqing Municipality and Sichuan Provinces. In total, 39.9% of participants experienced health risk stress (i.e. perceived stress had an impact of their health). The percent of errors in the information for I1 to I7 were 21.9%, 19.1%, 19.3%, 18.3%, 25.7%, 8.1% and 12.3%, respectively. Only 35.9% of participants answered all seven questions on COVID-19 information correctly.
Table 2.
Sociodemographic characteristics (n = 2449).
| Variables | N | Percent(%) | |
|---|---|---|---|
| Gender | Male | 823 | 33.6 |
| Female | 1626 | 66.4 | |
| Age (years) | 18–25 | 837 | 34.2 |
| 26–30 | 463 | 18.9 | |
| 31–40 | 427 | 17.4 | |
| 41–50 | 486 | 19.8 | |
| 51–60 | 192 | 7.8 | |
| ≥61 | 44 | 1.8 | |
| Education level | Elementary or below | 48 | 2.0 |
| Junior high school diploma | 326 | 13.3 | |
| Senior high school diploma | 310 | 12.7 | |
| Advanced diploma | 728 | 29.7 | |
| Baccalaureate degree | 881 | 36.0 | |
| Master's degree or above | 156 | 6.4 | |
| Marital status | Non-married | 1000 | 40.8 |
| Married | 1353 | 55.3 | |
| Divorced | 77 | 3.1 | |
| Widowed | 19 | 0.8 | |
| Personal monthly income (RMB) | ≤3000 | 845 | 34.5 |
| 3001–5000 | 880 | 35.9 | |
| 5001–7000 | 365 | 14.9 | |
| 7001–10000 | 215 | 8.8 | |
| ≥10,001 | 144 | 5.9 | |
| Region | Urban | 1783 | 72.8 |
| Township | 394 | 16.1 | |
| Rural | 272 | 11.1 | |
| Province of residence | Chongqing Municipality | 1408 | 57.5 |
| Sichuang Provinces | 434 | 17.7 | |
| Gansu Provinces | 151 | 6.2 | |
| Jiangxi Provinces | 114 | 4.7 | |
| Others | 342 | 14.0 | |
| Occupation | Employed | 1834 | 74.9 |
| Students | 261 | 10.7 | |
| Unemployed or ‘job-waiting’ individuals | 268 | 10.9 | |
| Retirees | 86 | 3.5 |
Measurement model
Table 3 presents the significant tests and the estimated CFA with the parameters from the extended IMB constructs. After removing item M6, the motivation latent variable retained five original items (M1-M5) that had a good fit (IFI = 0.973, CFI = 0.972 and RMSEA = 0.054). After deleting item BS8, the behavioural skill latent variable retained seven original items (BS1-BS7) that had a good fit (IFI = 0.961, CFI = 0.960 and RMSEA = 0.060). After removing item HB9, the health behaviours latent variable retained eight original items (HB1-HB8) that had a good fit (IFI = 0.983, CFI = 0.983 and RMSEA = 0.049). The five original items were reserved for the latent variable of positive perception of intervention (PPI1-PPI5), which resulted in a good fit (IFI = 0.968, CFI = 0.968 and RMSEA = 0.043).
Table 3.
Constructs for information, motivation, behavioural skills, health behaviours, perceived stress and positive perception of interventions (n = 2449).
| Constructs items (total scores range) | β | P | Mean | SD | IFI/CFI | RMSEA | Crobach's α |
|---|---|---|---|---|---|---|---|
| Perceived stress (0–56) | |||||||
| Score | 22.25 | 7.20 | 0.829 | ||||
| Information (0–7) | |||||||
| Knowledge score | 4.34 | 1.27 | 0.607 | ||||
| Motivation (5–25) | |||||||
| M1 | 0.470 | <0.001 | 23.15 | 2.67 | 0.973/0.972 | 0.054 | 0.639 |
| M2 | 0.413 | <0.001 | |||||
| M3 | 0.510 | <0.001 | |||||
| M4 | 0.669 | <0.001 | |||||
| M5 | 0.476 | <0.001 | |||||
| Behavioural skills (7–35) | |||||||
| BS1 | 0.415 | <0.001 | 23.15 | 2.67 | 0.961/0.960 | 0.060 | 0.768 |
| BS2 | 0.451 | <0.001 | |||||
| BS3 | 0.444 | <0.001 | |||||
| BS4 | 0.671 | <0.001 | |||||
| BS5 | 0.675 | <0.001 | |||||
| BS6 | 0.630 | <0.001 | |||||
| BS7 | 0.609 | <0.001 | |||||
| Positive perception of interventions (5–25) | |||||||
| PPI1 | 0.784 | <0.001 | 22.25 | 2.97 | 0.968/0.968 | 0.043 | 0.890 |
| PPI2 | 0.800 | <0.001 | |||||
| PPI3 | 0.785 | <0.001 | |||||
| PPI4 | 0.750 | <0.001 | |||||
| PPI5 | 0.758 | <0.001 | |||||
| Health behaviours (8–40) | |||||||
| HB1 | 0.606 | <0.001 | 23.15 | 2.67 | 0.983/0.983 | 0.049 | 0.844 |
| HB2 | 0.760 | <0.001 | |||||
| HB3 | 0.711 | <0.001 | |||||
| HB4 | 0.718 | <0.001 | |||||
| HB5 | 0.707 | <0.001 | |||||
| HB6 | 0.561 | <0.001 | |||||
| HB7 | 0.584 | <0.001 | |||||
| HB8 | 0.430 | <0.001 | |||||
SD = standard deviation; IFI = incremental fit index; CFI = comparative fit index; RMSEA = root mean square error of approximation.
The reliabilities of the scales in information, motivation, behavioural skills, perceived stress, positive perception of interventions and health behaviours were 0.607, 0.639, 0.768, 0.829, 0.890 and 0.844, respectively. In addition, all standardised factor loading estimates were >0.4 and significant (P < 0.05) in each measurement model.
Correlation analysis
The correlation coefficients among all constructs are presented in Table 4 . The correlation coefficient between all constructs were statistically significant, except for between information and motivation (r = −0.006, P = 0.716), between positive perception of interventions and information (r = 0.032, P = 0.109) and between health risk stress and motivation (r = −0.031, P = 0.123). Therefore, these three paths were deleted in the extended IMB model, namely, ‘Health Risk Stress → Motivation’, ‘Positive perception of intervention measures → Information’ and ‘Information → Motivation’, respectively.
Table 4.
Correlation coefficients among model constructs (n = 2449).
| Constructs | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1.Information | 1 | ||||
| 2.Motivation | −0.006 | 1 | |||
| 3.Behavioural skills | 0.187∗ | 0.184∗ | 1 | ||
| 4.Health behaviours | 0.161∗ | 0.245∗ | 0.494∗ | 1 | |
| 5.Health risk stress | −0.084a, ∗ | −0.031a | −0.203a, ∗ | −0.283a, ∗ | 1 |
| 6.Positive perception of interventions | 0.032 | 0.137∗ | 0.535∗ | 0.416∗ | −0.190a, ∗ |
∗P < 0.001.
Point biserial correlation coefficient with heath risk stress (perceived stress has an impact on health).
Path analysis
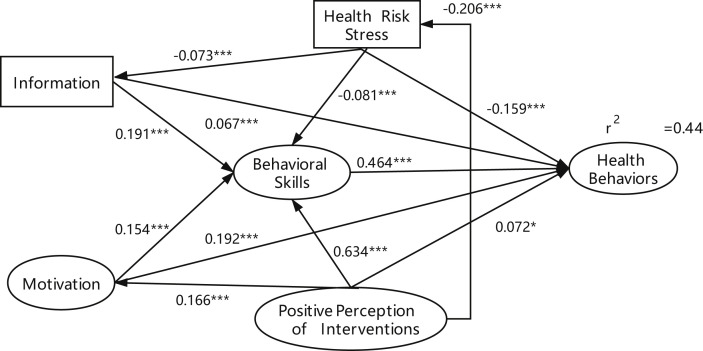
The final extended IMB model (Fig. 2 ) had a good fit; that is, χ2/df ratio = 1511.733/309 = 4.892, GFI = 0.949, CFI = 0.939, TLI = 0.930, RMSEA = 0.041. Five factors had significant direct effects on health behaviours; namely, information (β = 0.067, t = 3.408, P < 0.001), motivation (β = 0.192, t = 7.357, P < 0.001), behavioural skills (β = 0.464, t = 10.487, P < 0.001), health risk stress (β = −0.159, t = −8.110, P < 0.001) and positive perception of interventions (β = 0.072, t = 2.212, P = 0.027). Health risk stress exerted indirect impacts on health behaviours through behavioural skills and information. Positive perception of interventions also exerted indirect impacts on health behaviours through behavioural skills, health risk stress and motivation.
Fig. 2.
The final extended IMB model. Coefficients are standardized path coefficients. Variables in eclipses represent latent variables, in squares observed variables. ∗P < 0.05. ∗∗∗P < 0.001. IMB, information-motivation-behaviour skills.
In conclusion, the total effect coefficients of information, motivation, behavioural skills, health risk stress and positive perception of intervention on health behaviours were 0.156, 0.263, 0.464, −0.208 and 0.452, respectively. All variables accounted for 44.0% of health behaviours.
Discussion
This study successfully constructed an extended IMB model, wherein information, motivation, behavioural skills and positive perceptions of interventions are positive factors, and health risk stress is a negative factor for health behaviours. Previous studies have found that IMB has certain intervention effects.9 , 10 , 11 News media act as agents of information and persuasion during the COVID-19 pandemic;23 therefore, the extended IMB model was used as a theoretical framework to implement health behaviour interventions for the public via various electronic devices. For example, the government or relevant organisations released prevention measures, health education and other important information about the epidemic via text messages in China.
Information and motivation have a direct effect on health behaviours, which means that acquisition of prevention knowledge, correctly understanding the severity, contagion, and lethality of COVID-19 and maintaining a strong prevention motivation may promote health behaviours directly, without the need for complex or novel behavioural skills.4 However, the results indicated that residents are not confident about their knowledge. Approximately one-fifth of the respondents thought that taking antibiotics, consuming Shuanghuanglian oral solution or vinegar, or using gauze masks or activated carbon masks could prevent COVID-19. Such erroneous knowledge could lead to ineffective preventive measures by the population and increase the risk of infection. Therefore, it is necessary to target and proactively conduct health education for groups of different cultural levels and regions to improve residents' prevention knowledge.
Behavioural skills are indispensable for improving health behaviours15 and long-term prevention behaviours depends on behavioural skills.24 The results of this study validate the importance of behavioural skills, which are the mediating factor of information, motivation, perceived stress and positive perception of interventions. Behavioural skills are also the most important direct factors affecting health behaviours, in line with findings from other studies.6 , 12 , 13 Therefore, the government advise the public on correct health behaviours, such as wearing masks, washing hands and the use of disinfectants, so that residents can obtain these skills to reduce the risk of infection. It is also necessary to guarantee the supply of protective materials.
In the face of public health emergencies, the level of anxiety will be related to the severity of the disease.25 The results found that 39.9% of residents suffered from health risk stress. Health risk stress is negatively related to health behaviours, information and behavioural skills, which showed that excessive stress is not conducive to positive health behaviours, and that nervousness and being out of control can lead to negative coping styles. Individuals who maintain a high level of awareness of the danger and maintain a moderate level of stress are the most likely to adopt appropriate health behaviours.14 Therefore, it is necessary for relevant departments to guide residents to treat the epidemic objectively, calmly and rationally, and to take effective intervention measures to reduce stress and anxiety in the population.
The total effects of positive perception of interventions on health behaviours are similar to the effects seen with behavioural skills. The positive perception of interventions is negatively related to health risk stress. It is not only a direct influencing factor of health behaviours but also indirectly affects health behaviours through motivation and behavioural skills. It was revealed that suitable prevention and control measures adopted by the government and relevant organisations could reduce the fear and anxiety of residents and improve health behaviours. Therefore, the government should provide accurate, open and transparent information on the situation of the epidemic, strengthen interactions with the public and win the trust of residents. When residents have a high level of trust in the government, stress significantly decreased.26
This study has some limitations, including: (1) the randomisation of the sample was poor; however, a large sample size was used to ensure a certain number of individuals in all categories, to minimise bias; (2) extrapolation of the results is limited to some extent; data mainly represented the regions of Chongqing and Sichuan or regions with similar pandemic severity. Chongqing Municipality borders Hubei Province (the epicentre of the epidemic) and is adjacent to Sichuan Province. Between 20 January and 22 February, the total number of confirmed cases in Chongqing Municipality and Sichuan Province was 573 (six deaths) and 526 (three deaths), respectively.27 In view of the international nature of COVID-19 and its implications, future studies should include a broader sample.
This study has used the extended IMB model as a theoretical framework to construct more effective interventions during the COVID-19 epidemic in China. The government should pay attention to publicity and guidance, strengthen positive interaction with the public and disclose relevant information in a timely manner to gain trust and to maintain the positive public perception of the interventions. In terms of health education, the government should focus on behavioural skills, promptly rectify ineffective prevention information and raise awareness about the disease to relieve stress and anxiety in the population.
Author statements
Ethical approval
The study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University Ethics (No.2020250).
Funding
This work was supported by the National Key Project for Infectious Diseases of the Ministry of Science and Technology of China (grant numbers: 2018ZX10721102-005) and Chongqing Medical University New Coronavirus Emergency Research Special Project (grant numbers: CQMUNCP0305).
Competing interests
None declared.
Acknowledgements
The authors thank all individuals who volunteered to participate in this study and are grateful to ELSEVIER services in manuscript language polishing.
References
- 1.WHO Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [cited 2020 February 15]; Available from:
- 2.WHO Coronavirus disease 2019 (COVID-19)Situation report – 146. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [cited 2020 June 1]; Available from:
- 3.Shao S., Zhou Z., Li Y., Liu S., Lu L., Hou S. Experiences and practices in the current prevention and control of the novel coronavirus pneumonia in China. Disaster Med Public Health Prep. 2020:1–19. doi: 10.1017/dmp.2020.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fisher J.D., Fisher W.A. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 5.Fisher W.A. Understanding human papillomavirus vaccine uptake. Vaccine. 2012;30(Suppl 5):149–156. doi: 10.1016/j.vaccine.2012.04.107. [DOI] [PubMed] [Google Scholar]
- 6.Hu L., Luo Y.T., Zhong X.N., Lu R.R., Wang Y., Sharma M. Condom use and related factors among rural and urban men who have sex with men in Western China: based on information-motivation-behavioral skills model. Am J Men's Health. 2020;14:1–10. doi: 10.1177/1557988319899799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qu D., Zhong X.N., Xiao G.Y., Dai J.H., Liang H., Huang A.L. Adherence to pre-exposure prophylaxis among men who have sex with men: a prospective cohort study. Int J Infect Dis. 2018;75:52–59. doi: 10.1016/j.ijid.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Fleary S.A., Joseph P., Chang H. Applying the information-motivation-behavioral skills model to explain adolescents' fruits and vegetables consumption. Appetite. 2020;147:104546. doi: 10.1016/j.appet.2019.104546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.John S.A., Walsh J.L., Weinhardt L.S. The information-motivation-behavioral skills model revisited: a network-perspective structural equation model within a public sexually transmitted infection clinic sample of hazardous alcohol users. AIDS Behav. 2017;21:1208–1218. doi: 10.1007/s10461-016-1446-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cooperman N.A., Lu S.E., Richter K.P., Bernstein S.L., Williams J.M. Pilot study of a tailored smoking cessation intervention for individuals in treatment for opioid dependence. Nicotine Tob Res. 2018;20:1152–1156. doi: 10.1093/ntr/ntx189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ownby R.L., Waldrop-Valverde D., Caballero J., Jacobs R.J. Baseline medication adherence and response to an electronically delivered health literacy intervention targeting adherence. Neurobehav HIV Med. 2012;4:113–121. doi: 10.2147/NBHIV.S36549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen Q., Wang H.W., Wang Y.C., Wang Z.Z., Zhao D.J., Cai Y. Exploring effects of self-management on glycemic control using a modified information–motivation–behavioral skills model in type 2 diabetes mellitus patients in Shanghai, China:A cross-sectional study. J Diabetes. 2018;10:734–743. doi: 10.1111/1753-0407.12655. [DOI] [PubMed] [Google Scholar]
- 13.Nelson L.A., Wallston K.A., Kripalani S., LeStourgeon L.M., Williamson S.E., Mayberry L.S. Assessing barriers to diabetes medication adherence using the Information-Motivation-Behavioral skills model. Diabetes Res Clin Pract. 2018;142:374–384. doi: 10.1016/j.diabres.2018.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leung G.M., Lam T.-H., Ho L.-M., Ho S.-Y., Chan B.-H.-Y., Wong I.-O.-L. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. 2003;57:857–863. doi: 10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fisher J.D., Fisher W.A., Williams S.S., Malloy T.E. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13:238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- 16.Dayna L.-B., Anita D.L., Paul V., Esther G. Coping with the threat of severe acute respiratory syndrome: role of threat appraisals and coping responses in health behaviors. Asian J Soc Psychol. 2004;7:9–23. doi: 10.1111/j.1467-839X.2004.00131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lv S.L., Tian B.C., Yang T.Z., Chen D.W., Chi Y.H. Perceived stress in general public during prevalence of severe acute respiratory syndrome and it impact on health behavior. Chin J Prev Med. 2010;44:128–133. [PubMed] [Google Scholar]
- 18.National Health Commission of the People's Republic of China Coronavirus disease (COVID-19) knowledge of prevention. 2020. http://www.nhc.gov.cn/xcs/kpzs/list_gzbd.shtml [cited 2020 February 5]; Available from: [DOI] [PMC free article] [PubMed]
- 19.WHO Coronavirus disease (COVID-19) advice for the public. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [cited 2020 February 5]; Available from:
- 20.Alexia K., Demosthenes P., Aggeliki Z., Marios V., Ioannis S., Filippos T. Validation of a Greek version of PSS-14:a global measure of perceived stress. Cent Euro J Publ Health. 2012;20:104–109. doi: 10.21101/cejph.a3698. [DOI] [PubMed] [Google Scholar]
- 21.Blair W., Bengt M., Duane F.A., Gene F.S. Assessing reliability and stability in panel models. Socio Methodol. 1977;8:84–139. [Google Scholar]
- 22.Daire H., Joseph C., Michael R.M. Structural equation modelling guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60. [Google Scholar]
- 23.De Coninck D., d'Haenens L., Matthijs K. Forgotten key players in public health: news media as agents of information and persuasion during the COVID-19 pandemic. Publ Health. 2020;183:65–66. doi: 10.1016/j.puhe.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walsh J.L., Senn T.E., Scott-Sheldon L.A., Vanable P.A., Carey M.P. Predicting condom use using the Information-Motivation-Behavioral Skills (IMB) model: a multivariate latent growth curve analysis. Ann Behav Med. 2011;42:235–244. doi: 10.1007/s12160-011-9284-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gabriel M.L., Lai-Ming H., Steve K.K.C., Sai-Yin H., John B.-S., Y L C R. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin Infect Dis. 2005;40:1713–1720. doi: 10.1086/429923. [DOI] [PubMed] [Google Scholar]
- 26.Sha L.X., Liu Y., Wang W.D., Chen Y. Analysis and simulation an mass psychology by CAS theory -research on policies to respond to critical events. Henan Soc Sci. 2005;13:1–6. [Google Scholar]
- 27.WHO Coronavirus disease 2019 (COVID-19)Situation report – 33. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [cited 2020 May 26 ]; Available from: