Abstract
Introduction
Virtually all individuals with Down syndrome (DS) will develop Alzheimer's disease (AD) pathology by age 40. Cerebrospinal fluid (CSF) biomarkers have characterized AD pathology in cohorts of late‐onset AD (LOAD) and autosomal‐dominant AD (ADAD). Few studies have evaluated such biomarkers in adults with DS.
Methods
CSF concentrations of amyloid beta (Aβ)40, Aβ42, tau, phospho‐tau181 (p‐tau), neurofilament light chain (NfL), soluble triggering receptor expressed on myeloid cells 2 (sTREM2), chitinase‐3‐like protein 1 (YKL‐40), alpha synuclein (αSyn), neurogranin (Ng), synaptosomal‐associated protein 25 (SNAP‐25), and visinin‐like protein 1 (VILIP‐1) were assessed in CSF from 44 adults with DS from the Alzheimer's Biomarker Consortium–Down Syndrome study. Biomarker levels were evaluated by cognitive status, age, and apolipoprotein E gene (APOE) ε4 carrier status.
Results
Biomarker abnormalities indicative of amyloid deposition, tauopathy, neurodegeneration, synaptic dysfunction, and neuroinflammation were associated with increased cognitive impairment. Age and APOE ε4 status influenced some biomarkers.
Discussion
The profile of many established and emerging CSF biomarkers of AD in a cohort of adults with DS was similar to that reported in LOAD and ADAD, while some differences were observed.
Keywords: Alzheimer's disease, biomarkers, cerebrospinal fluid, Down syndrome, amyloid, tau
1. BACKGROUND
Due to the triplication of the amyloid precursor protein (APP) gene located on chromosome 21, virtually all individuals with Down syndrome (DS) will develop brain pathology indicative of Alzheimer's disease (AD) by the age of 40. 1 The incidence of AD dementia among older adults with DS has been observed to be as high as 77% by the seventh decade of life. 2 However, due to varying baseline or pre‐morbid levels of intellectual disability, early detection of the clinical symptoms of AD is challenging in this population. In late‐onset AD (LOAD) and autosomal dominant AD (ADAD) cohorts, longitudinal analysis of various AD biomarkers has revealed significant potential for their use in determining pathological disease stage, as well as predicting symptom onset and cognitive decline in individuals with pre‐clinical disease. 3 , 4 This pre‐symptomatic stage has been estimated to begin two to three decades before the onset of clinical symptoms. 5
In addition to the established AD cerebrospinal fluid (CSF) biomarkers amyloid beta 1‐40 (Aβ40), amyloid beta 1‐42 (Aβ42), total tau, and phospho‐tau181 (p‐tau), recent studies have identified novel biomarkers in ADAD and LOAD cohorts that significantly correlate with pathologic and clinical markers of disease progression. These emerging biomarkers include markers of neuronal and axonal injury (visinin‐like protein 1 [VILIP‐1] and neurofilament light chain [NfL]), 6 , 7 synaptic dysfunction (synaptosomal‐associated protein 25 [SNAP‐25] and neurogranin [Ng]), 8 , 9 , 10 and neuroinflammation (chitinase‐3‐like protein 1 [YKL‐40] and soluble triggering receptor expressed on myeloid cells 2 [sTREM2]). 11 , 12 , 13 In LOAD and ADAD cohorts, these emerging biomarkers are positively correlated with each other and with levels of CSF tau and p‐tau, and they have been shown to be predictive of future cognitive decline, especially in the presence of amyloid. 14 In addition to these markers, α‐synuclein (αSyn), which is typically associated with Lewy body pathology in Parkinson disease, has also been associated with AD pathology and cognitive decline. 15 , 16 Few studies have characterized these emerging biomarkers in adults with DS. 17 , 18 , 19
The Alzheimer's Biomarker Consortium–Down Syndrome (ABC‐DS) study aims to identify and track biomarkers of AD progression in adults with DS and further characterizes the contributing biological factors that will be critical for early diagnosis, disease staging, and development of effective interventions in this high‐risk population. The purpose of this study is to present the cross‐sectional analysis of CSF biomarkers of established and novel AD biomarkers in this cohort and examine biomarker relationships with age, cognitive status, and apolipoprotein E (APOE) ε4 status (the strongest genetic risk factor for LOAD). 20
2. METHODS
2.1. Participants
Adults with DS between 25 and 66 years of age were enrolled in the ABC‐DS study, a multi‐site longitudinal study of AD biomarkers in adults with DS that includes the collection of neuropsychological, neuroimaging, genetic, and fluid biomarker measures. Participants with baseline CSF collections (ages 30 to 61 years) as of January 2019 were included in this analysis. Informed consent was obtained from all participants where possible; otherwise, assent was obtained from the participant and informed consent obtained from the participant's proxy or legally authorized representative. All ABC‐DS protocols and procedures were approved by the institutional review boards at the respective local clinical performance sites.
2.2. Cognitive assessment and genetic analysis
Using a consensus‐based procedure, participants were given the following baseline diagnosis: (1) cognitively stable (CS); (2) mild cognitive impairment (DS‐MCI); (3) possible/probable dementia (DS‐AD); or (4) uncertain. A consensus conference includes at least three individuals with clinical training and expertise in evaluating dementia in adults with DS (eg, psychologist, physician), each of whom had participated in the clinical assessment of a given participant. A diagnosis of CS indicates no evidence of clinically significant cognitive decline, with performance consistent with preclinical intellectual functioning and age. A diagnosis of DS‐MCI indicates evidence of cognitive decline over time beyond what would be expected with age but of insufficient severity to suggest dementia. A diagnosis of DS‐AD indicates evidence of substantial decline of breadth and severity greater than indicative of DS‐MCI or clear evidence of substantial cognitive and functional decline with a high degree of confidence in the dementia rating. Diagnoses were made using information from core neuropsychological and informant measures (Down Syndrome Mental Status Examination, Extended & Block Design, Verbal Fluency, Berry‐Buktenica Test of Visual Motor Integration, Vineland Adaptive Behavior Scale–Third Edition, Dementia Questionnaire for People with Learning Disabilities, Reiss Screen for Maladaptive Behavior), neurological exam, medical history, and record review, generally consistent with the recommendations of the American Association on Mental Retardation‐International Association for the Scientific Study of Intellectual Disability (AAMR‐IASSID) Working Group for the Establishment of Criteria for the Diagnosis of Dementia in Individuals with Developmental Disability. 21 , 22 In most cases, the karyotype status of adults with DS was obtained from family members who had medical records with chromosomal analysis results. When the karyotype status was unavailable from medical records, blood samples were sent to a designated cytogenetics laboratory at each medical center. DNA samples were genotyped for two APOE single‐nucleotide polymorphisms (SNPs; rs429358 and rs7412) with the KASP genotyping system by LGC Genomics. Genotype data for these two SNPs were used to define APOE ε2, ε3, and ε4 alleles. For this analysis, we assigned APOE ε4 status as APOE ε4 negative (non‐carriers) or APOE ε4 positive (carriers of at least one copy of the APOE ε4 allele).
HIGHLIGHTS
Cerebrospinal fluid (CSF) biomarkers of Alzheimer's disease (AD) were assessed in a multisite cohort of adults with Down syndrome (DS)
CSF AD biomarkers are associated with mild cognitive impairment (MCI) and dementia in adults with DS
Adults with DS exhibit CSF biomarker profiles similar to those of other AD cohorts
CSF markers of amyloid and neuronal injury show apolipoprotein E gene (APOE) ε4 effects in DS
APOE ε4 influences levels of CSF amyloid beta42 (Aβ42), tau, and synaptosomal‐associated protein 25 (SNAP‐25) in adults with DS
RESEARCH IN CONTEXT
Systematic review: Few studies evaluating cerebrospinal fluid (CSF) biomarkers of Alzheimer's disease (AD) in adults with Down syndrome (DS) have been published. Therefore, all relevant articles on PubMed relating to CSF biomarkers of AD in other risk groups were also considered.
Interpretation: There are commonalities in the profile of and relationship among CSF biomarkers in adults with DS compared to those published in other AD cohorts. Therefore, these biomarkers may have potential use in determining pathological disease stage and predicting symptom onset and cognitive decline in individuals with DS, as has been reported in late‐onset and autosomal dominant forms of AD.
Future directions: Investigation of within‐person longitudinal change in biomarkers and cognition across the full disease spectrum in adults with DS are needed. A direct comparison between adults with DS and other at‐risk groups would be of great value to the field.
2.3. CSF collection and analysis
Participants underwent CSF collection via lumbar puncture (LP) between 9 am and 4 pm; typically, 10 to 20 mL of CSF was collected under gravity flow or by aspiration while the participant was sitting, lying, or prone for fluoroscopy‐assisted collection. Samples were collected into a sterile polypropylene tube, flash frozen on dry ice, and shipped to the ABC‐DS Biomarker Core at Washington University in St. Louis. Samples were thawed on wet ice, aliquoted (0.5 mL) into polypropylene tubes, flash frozen, and stored at −80°C until biomarker analysis. Frozen aliquots were thawed on wet ice the day of analysis. Concentrations of Aβ40, Aβ42, total tau, and p‐tau were measured by chemiluminescent enzyme immunoassay using a fully automated platform (LUMIPULSE G1200, Fujirebio, Malvern, PA) according to manufacturer's specifications. Ng, SNAP‐25, and VILIP‐1 were measured with microparticle‐based immunoassays using Single Molecule Counting technology employing antibodies developed in the laboratory of Dr. Jack Ladenson at Washington University in St. Louis, as described previously. 8 , 10 , 23 Concentrations of sTREM2 were measured via an in‐house enzyme‐linked immunosorbent assay (ELISA) as described previously. 12 NfL (UmanDiagnostics, Umeå, Sweden), YKL‐40 (Quidel, San Diego, CA), and αSyn (ADx Neurosciences, Ghent, Belgium) were measured via commercial ELISAs according to manufacturer recommendations. Because αSyn levels in the blood are much higher than in the CSF, hemoglobin was measured as a control for blood contamination via ELISA (Bethyl Laboratories, Montgomery, TX). 24 Hemoglobin concentrations were not correlated with αSyn concentrations in the present study, therefore all αSyn data are reported.
2.4. Statistical analysis
Group comparisons based on cognitive status (CS, DS‐MCI, or DS‐AD) were performed using Kruskal‐Wallis and Dunn tests with Holm‐Bonferroni correction for multiple comparisons. Group comparisons based on APOE ε4 carrier status (APOE ε4 positive or APOE ε4 negative) were conducted using a Mann‐Whitney U test with Holm‐Bonferroni correction for multiple comparisons and analysis of covariance (ANCOVA) with age as a covariate (for which we report adjusted P‐values). For these group comparisons, outliers ± two standard deviations (SD) from the group means were excluded from statistical analysis but were included in the figures for illustrative purposes. Biomarker correlations are presented as Spearman rho. P values <.05 were considered statistically significant.
3. RESULTS
3.1. Demographics
Demographic data are reported in Table 1. Forty‐four participants (mean age 48 ±7.5 years, range 30 to 61 years) had baseline CSF collections as of January 2019. Overall, more male than female participants underwent CSF collections. The CS and DS‐MCI groups were predominantly male. The DS‐AD group was predominantly female and significantly older than the CS group. APOE‐ε4 carriers made up roughly a third of the cohort overall, but a higher proportion of the dementia group (57%) were APOE‐ε4 carriers. Karyotyping revealed 36 individuals (82%) with trisomy 21, two with mosaicism, and two with translocation. Four individuals were missing karyotype information; however, a clinical diagnosis of DS was established. A higher number of participants were classified as CS (ie, cognitive abilities not differing from usual as defined by neuropsychological and informant measures) compared to those who showed cognitive decline from a prior evaluation. Data for diagnosis was unavailable for two individuals (both trisomy 21), so biomarker data for these participants were not included in analyses based on cognitive status, but they were included in analyses evaluating biomarker correlations and effects of APOE ε4 status.
TABLE 1.
Demographics of a cohort of adults with DS with available CSF
| Characteristic | All DS (n = 44) | CS (n = 28) | DS‐MCI (n = 7) | DS‐AD (n = 7) |
|---|---|---|---|---|
| Age, years | 48 ± 7.5 | 47 ± 7.4 | 52 ± 4.1 | 54 ± 5.0 a |
| Female/male (% female) | 17/27 (39%) | 10/18 (36%) | 1/6 (14%) c | 5/2 (71%) b |
| APOE‐ε4 carriers | 16 (36%) | 10 (36%) | 2 (29%) | 4 (57%) |
| Karyotype | ||||
| Trisomy 21 | 36 (82%) | 24 (86%) | 5 (71.4%) | 5 (71.4%) |
| Mosaicism | 2 (4.5%) | 2 (7%) | 0 (0%) | 0 (0%) |
| Translocation | 2 (4.5%) | 1 (3.5%) | 1 (14.3%) | 0 (0%) |
| Missing | 4 (9%) | 1 (3.5%) | 1 (14.3%) | 2 (28.6%) |
| CSF Biomarkers | ||||
| Aβ40 (pg/mL1) | 13610 ± 4161 | 14143 ± 4279 | 13336 ± 3067 | 10987 ± 2164 |
| Aβ42 (pg/mL2) | 909 ± 329 | 978 ± 279 | 802 ± 148 | 563 ± 104 a |
| Total Tau (pg/mL3) | 637 ± 437 | 564 ± 412 | 657 ± 385 | 994 ± 486 a |
| p‐Tau (pg/mL4) | 89.1 ± 75.8 | 69.9 ± 69.2 | 110.8 ± 75.4 | 157.9 ± 71.6 |
| Aβ42/Aβ40 ratio5 | 0.068 ± 0.019 | 0.072 ± 0.019 | 0.061 ± 0.011 | 0.052 ± 0.009 a |
| Tau/Aβ42 ratio6 | 0.856 ± 0.805 | 0.644 ± 0.527 | 0.827 ± 0.473 | 1.921 ± 1.221 a |
| p‐Tau/Aβ42 ratio7 | 0.127 ± 0.141 | 0.086 ± 0.104 | 0.141 ± 0.092 a | 0.306 ± 0.19 a |
| NfL (pg/mL8) | 2031 ± 1646 | 1747 ± 1823 | 2215 ± 712 a | 3267 ± 1167 a |
| αSyn (pg/mL9) | 1971 ± 823 | 1873 ± 807 | 2387 ± 807 | 1871 ± 546 |
| sTREM2 (pg/mL10) | 947 ± 334 | 897 ± 300 | 1035 ± 376 | 1044 ± 407 |
| YKL‐40 (ng/mL11) | 249 ± 124 | 222 ± 135 | 267 ± 92 | 327 ± 92 a |
| Ng (pg/mL12) | 4549 ± 2507 | 4144 ± 2368 | 5742 ± 3144 | 5107 ± 2004 |
| SNAP‐25 (pg/mL13) | 4.38 ± 1.86 | 4.16 ± 1.86 | 4.87 ± 2.08 | 5.45 ± 1.18 a |
| VILIP‐1 (pg/mL14) | 195 ± 93 | 180 ± 82 | 245 ± 123 | 230 ± 92 |
Age and biomarker data are reported as mean ± standard deviation (SD). Two individuals for whom data for consensus diagnosis were not available at the time of analysis were excluded from the cognitive groups. Biomarker analyses by cognitive group were conducted using Kruskal‐Wallis and Dunn tests with Holm‐Bonferroni correction for multiple comparisons. Outliers more than 2 SD from the mean were excluded from statistical analysis but are reported in the graphs and figures. P values <.05 were considered statistically significant.
Denotes significant difference from CS.
Denotes significance from DS‐MCI.
Denotes significance from DS‐AD. Superscripted numbers identify the number of outliers (values ± 2 SD from the group means) that were included in the calculations of the means but omitted from the statistical analyses: 1n = 1 in CS; 2n = 2 in CS; 3n = 2 in CS; 4n = 1 in CS; 5n = 1 in CS; 6n = 1 in CS; 7n = 2 in CS; 8n = 1 in CS; 9n = 1 in CS; 10n = 3 in CS; 11n = 1 in CS; 12n = 1 in CS; 13n = 2 in CS, n = 1 in DS‐MCI; 14n = 1 in CS.
3.2. Biomarker distributions by cognitive status
Individuals were grouped according to cognitive status (CS, DS‐MCI, or DS‐AD), and mean biomarker levels were compared (Table 1, Figure 1). Concentrations of Aβ42 and the Aβ42/Aβ40 ratio were significantly lower in individuals with dementia (P = .001 and P = .020, respectively), and total tau, YKL‐40, and SNAP‐25 levels were significantly higher in the DS‐AD group compared to the CS group (P = .009, P = .007, and P = .025, respectively). Of all the biomarkers, only NfL and the p‐tau/Aβ42 ratio were significantly higher in both DS‐MCI and DS‐AD groups (P = .0002 and P = .0001, respectively) compared to the CS group. Levels of p‐tau, αSyn, sTREM2, Ng, and VILIP‐1 were not significantly different among the groups, although the lack of significance was likely due more to the high variability than the difference in the mean concentrations.
FIGURE 1.
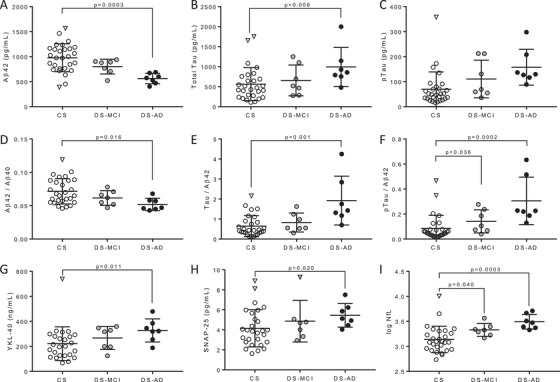
Distribution of AD biomarkers in a cohort of adults with DS by cognitive status. Levels of (A) Aβ42, (B) total tau, (C) p‐tau, (D) Aβ42/Aβ40 ratio, (E) tau/Aβ42 ratio, (F) p‐tau/Aβ42 ratio, (G) YKL‐40, (H) SNAP‐25, and (I) logNfL are plotted as a function of cognitive status. Open symbols represent cognitively stable individuals (CS), gray symbols represent individuals with MCI (DS‐MCI), and black symbols represent individuals with AD dementia (DS‐AD) defined by consensus criteria. Horizontal lines represent mean ± SD. Outliers more than 2 SD from the mean (triangles) were excluded from statistical analysis. Group comparisons were conducted using Kruskal‐Wallis and Dunn tests with Holm‐Bonferroni correction for multiple comparisons. P values <.05 were considered statistically significant
3.3. Biomarker distributions by age
In addition, the biomarker levels were also assessed with respect to age at time of LP (Table 2, Figure 2). Aβ42 (ρ = −0.47, P < .01) was negatively correlated with age, whereas levels of p‐tau (ρ = 0.55, P < .0001), NfL (ρ = 0.60, P < .0001), YKL‐40 (ρ = 0.64, P < .0001), Ng (ρ = 0.30, P < .05), SNAP‐25 (ρ = 0.32, P < .05), and VILIP‐1 (ρ = 0.55, P < .01) were all positively correlated with age. Total tau (ρ = 0.29, P = .055) and sTREM2 (ρ = 0.29, P = .060) exhibited a trend toward significance with respect to age, but these analytes were highly variable in this cohort. Aβ40 (ρ = −0.13, P = .40) and αSyn (ρ = 0.24, P = .12) were not significantly correlated with age in this cohort.
TABLE 2.
Correlation matrix of AD biomarkers in a cohort of adults with DS
| Biomarker | Aβ40 | Aβ42 | tau | p‐tau | NfL | sTREM2 | YKL‐40 | αSyn | Ng | SNAP‐25 | VILIP‐1 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | ρ | −0.13 | −0.47 | 0.29 | 0.55 | 0.60 | 0.29 | 0.64 | 0.24 | 0.30 | 0.32 | 0.43 |
| P | n.s. | <.01 | .055 | <.001 | <.0001 | .060 | <.0001 | n.s. | <.05 | <.05 | <.01 | |
| Aβ40 | ρ | 0.63 | 0.21 | 0.29 | −0.05 | 0.42 | 0.31 | 0.76 | 0.60 | 0.41 | 0.52 | |
| P | <.0001 | n.s. | .058 | n.s. | <.01 | .053 | <.0001 | <.0001 | <.01 | <.001 | ||
| Aβ42 | ρ | −0.32 | −0.44 | −0.49 | 0.08 | −0.27 | 0.14 | −0.04 | −0.16 | −0.11 | ||
| P | <.05 | <.01 | <.001 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | |||
| tau | ρ | 0.72 | 0.74 | 0.31 | 0.55 | 0.54 | 0.61 | 0.57 | 0.56 | |||
| P | <.0001 | <.0001 | <.05 | <.001 | <.001 | <.0001 | <.0001 | <.001 | ||||
| p‐tau | ρ | 0.71 | 0.47 | 0.79 | 0.73 | 0.83 | 0.70 | 0.83 | ||||
| P | <.0001 | <.01 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | |||||
| NfL | ρ | 0.44 | 0.59 | 0.38 | 0.48 | 0.45 | 0.42 | |||||
| P | <.01 | <.001 | <.05 | <.01 | <.01 | <.01 | ||||||
| sTREM2 | ρ | 0.54 | 0.56 | 0.58 | 0.32 | 0.43 | ||||||
| P | <.001 | <.001 | <.001 | <.05 | <.01 | |||||||
| YKL‐40 | ρ | 0.68 | 0.73 | 0.56 | 0.77 | |||||||
| P | <.0001 | <.0001 | <.001 | <.0001 | ||||||||
| αSyn | ρ | 0.93 | 0.61 | 0.82 | ||||||||
| P | <.0001 | <.0001 | <.0001 | |||||||||
| Ng | ρ | 0.65 | 0.84 | |||||||||
| P | <.0001 | <.0001 | ||||||||||
| SNAP‐25 | ρ | 0.75 | ||||||||||
| P | <.0001 | |||||||||||
Correlation coefficients represent Spearman rho (ρ). P values <.05 were considered statistically significant. White cells are not significant (n.s.). Lightest gray are significant with P ≤ .06; light gray are significant with P < .05; medium gray are significant with P < .01; dark gray are significant with P < .001; darkest gray are significant with P < .0001.
FIGURE 2.
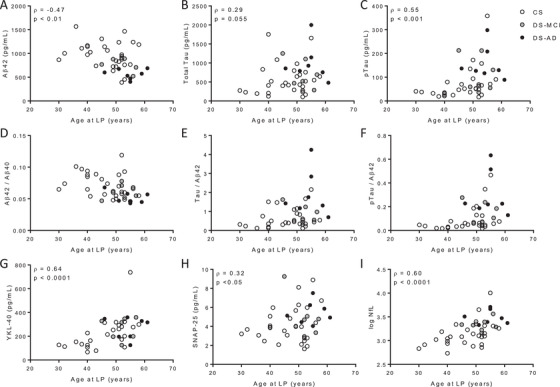
Distribution of AD biomarkers in a cohort of adults with DS by age and cognitive status. Levels of (A) Aβ42, (B) total tau, (C) p‐tau, (D) Aβ42/Aβ40 ratio, (E) tau/Aβ42 ratio, (F) p‐tau/Aβ42 ratio, (G) YKL‐40, (H) SNAP‐25, and (I) logNfL are plotted as a function of age at LP. Open symbols represent cognitively stable individuals (CS), gray symbols represent individuals with MCI (DS‐MCI), and black symbols represent individuals with AD dementia (DS‐AD) defined by consensus criteria. Correlations coefficients represent Spearman rho (ρ). P values <.05 were considered statistically significant and are shown.
3.4. APOE effects
We examined CSF biomarkers by APOE ε4 carrier status by designating individuals as APOE ε4‐positive or ‐negative (Figure 3). Levels of sTREM2, SNAP‐25, and the tau/Aβ42 ratio were significantly higher in those who were APOE ε4‐positive versus ε4‐negative (P = .024, P = .035, and P = .049, respectively). After controlling for age, Aβ42, total tau, SNAP‐25 and the tau/Aβ42 ratio were significantly different between carriers and non‐carriers (adjusted P = .008, P = 0.027, P = .028, and 0.015, respectively). Significant APOE ε4–associated differences in other biomarkers were not observed (all P > .05).
FIGURE 3.
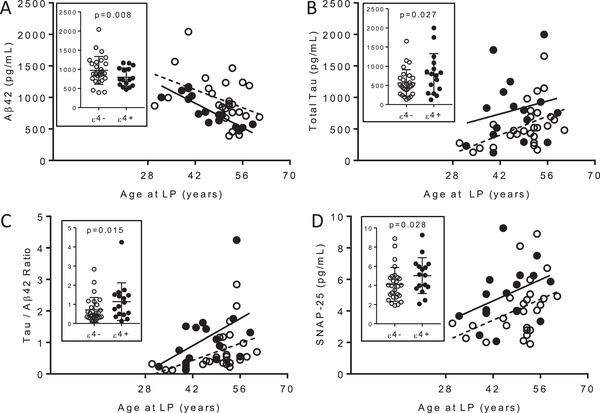
Distribution of CSF biomarkers by age and APOE ε4 carrier status. Levels of (A) Aβ42, (B) total tau, (C) the tau/Aβ42 ratio, and (D) SNAP‐25 are plotted as a function of age at LP. Open circles and dotted lines represent APOE ε4 non‐carriers (ε4‐). Black circles and solid lines represent APOE ε4 carriers (ε4+). Lines are linear regressions of biomarker data by age at LP. One individual did not have APOE genotype data and was excluded from this analysis. Group comparisons were performed by ANCOVA with age as a covariate. Adjusted P values <.05 were considered statistically significant
3.5. Biomarker correlations
The correlation among CSF biomarkers in the cohort as a whole was also assessed (Table 2). Aβ40 was significantly positively correlated with Aβ42 (ρ = 0.63, P < .0001), sTREM2 (ρ = 0.42, P < .01), αSyn (ρ = 0.64, P < .0001), Ng (ρ = 0.30, P < .05), SNAP‐25 (ρ = 0.32, P < .05), and VILIP‐1 (ρ = 0.43, P < .01). Aβ42 was negatively correlated with tau (ρ = −0.32, P < .05), p‐tau (ρ = −0.44, P < .01), and NfL (ρ = −0.49, P < .001). Total tau, p‐tau, NfL, sTREM2, YKL‐40, αSyn, Ng, SNAP‐25, and VILIP‐1 were all positively correlated with each other (P < .05, P < .01, P < .001, or P < .0001 for all). For illustrative purposes, select correlations are shown in Figure 4.
FIGURE 4.
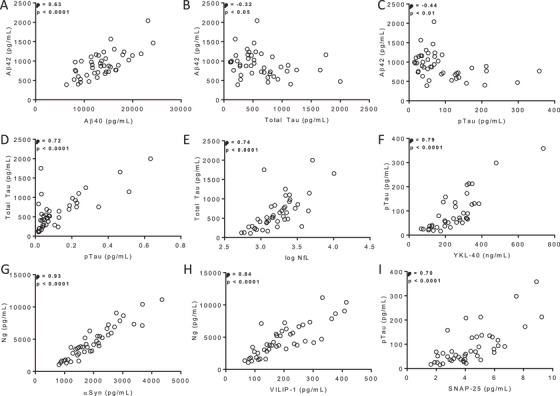
Scatter plots of select biomarker correlations. Plotted are the relationships between levels of (A) Aβ42 and Aβ40, (B) Aβ42 and total tau, (C) Aβ42 and p‐tau, (D) total tau and p‐tau, (E) total tau and log NfL, (F) p‐tau and YKL‐40, (G) Ng and αSyn, (H) Ng and VILIP‐1, and (I) p‐tau and SNAP‐25. Correlation coefficients represent Spearman rho (ρ). P values <.05 were considered statistically significant.
4. DISCUSSION
This report describes results of the initial cross‐sectional analysis of CSF biomarker data in the multi‐site ABC‐DS study. Due to the limited number of studies of CSF biomarkers related to risk for AD in adults with DS, sample sizes were not formally constructed, and all participants with available CSF collections were included in the analysis. Despite the small number of participants with available CSF (n = 44), the AD biomarker profiles in this cohort of adults with DS are remarkably similar to those observed in LOAD and ADAD cohorts. 5 , 14 In general, low CSF Aβ42 and the Aβ42/Aβ40 ratio (indicative of amyloid deposition) were observed in individuals with AD dementia (compared to the MCI and CS groups), while biomarkers of tauopathy (p‐tau) and neurodegeneration (total tau, NfL) were higher. This is consistent with findings in other cohorts of adults with DS, 17 , 18 , 25 as well as ADAD and LOAD. 14 CSF NfL and the p‐tau/Aβ42 ratio were the only markers that significantly differentiated both the DS‐AD and DS‐MCI groups from the CS group, despite the relatively high variability in absolute values of both markers (Figure 1). Fortea et al. reported high diagnostic performance of CSF Aβ42, p‐tau, and NfL in a larger cohort of adults with DS. 17 Further analysis is required to determine the diagnostic utility of these biomarkers at the individual subject level in the present cohort. Results in the two cohorts may differ given that the CS group in the present study is expected to be diminished due to rapid biomarker changes observed in the fifth decade of life in CS adults with DS. As expected, several biomarkers were significantly correlated with age in adults with DS, consistent with data from other AD cohorts. 14 With respect to age, it seems that most, if not all, of the biomarkers are already changing at the ages examined in this cohort, suggesting the need to include even younger participants in the study, who would be expected to be earlier in the evolution of the disease process. The high variability in levels of tau and SNAP‐25 as a function of age suggests that there may be additional processes taking place in individuals with DS. Longitudinal analysis will be necessary to elucidate individual changes over time, but in this cross‐sectional analysis, it appears that CSF Aβ42 concentrations are still declining (indicative of continuing amyloid deposition), and measures of tauopathy and neurodegeneration are exhibiting robust increases, by age ≈40 (Figure 2).
The presence of the APOE ε4 allele is a strong risk factor for the development of LOAD, as well as for an earlier onset of clinical symptoms of dementia. 20 , 26 The APOE genotype has also similarly been reported to influence age of symptom onset in ADAD mutation carriers. 27 , 28 , 29 Whether APOE genotype also influences CSF biomarker profiles in ADAD remains to be determined.
In this small study of adults with DS, we found that presence of an APOE ε4 allele was associated with significantly lower CSF Aβ42 and higher SNAP‐25, tau and the tau/Aβ42 ratio, even after controlling for age. A previous study of LOAD in cognitively normal older adults in the preclinical stage also reported similar APOE ε4 effects on CSF Aβ42; however, CSF tau was not affected by APOE ε4 status, likely due to the very early disease stage in that solely preclinical cohort. 30 Higher CSF levels of SNAP‐25 were recently associated with APOE ε4 carrier status in LOAD. 31 To our knowledge, this is the first study to evaluate the APOE genotype effects on these biomarkers in DS. The mechanisms underlying these associations remain to be determined. Future studies should include APOE genotype as an important variable to consider when evaluating the role of apoE across the cognitive aging spectrum in DS.
The correlation profile of the various CSF biomarkers in this cohort of adults with DS was consistent with other reports in LOAD and ADAD, 5 , 32 with strong positive correlations among the various markers of neuronal injury but less with Aβ markers, thus potentially supporting commonality in the underlying pathologic processes among different forms of genetic and sporadic AD. However, there are some differences. The relatively large positive correlation (ρ = 0.63) observed between Aβ40 and Aβ42 in DS likely reflects the overexpression and overproduction of APP and its resultant Aβ peptides due to triplication of chromosome 21. Reductions in Aβ42, but not Aβ40, with advancing age likely reflect the AD‐associated aggregation and deposition of Aβ42 as amyloid plaques. Analyses of the association between CSF biomarkers and amyloid imaging in the ABC‐DS cohort are ongoing and will provide a direct test of this hypothesis. Although markers of neuroinflammation (sTREM2 and YKL‐40) were more strongly correlated with markers of neuronal injury than markers of amyloid (Aβ42), the causality remains to be determined. Of particular note is the very high positive correlation (ρ = 0.93) observed between CSF αSyn and Ng. This finding is supported by a report that these proteins may be binding partners at the synapse. 33 It is likely that a similarly high correlation will also be observed in LOAD and/or ADAD, but this has yet to be reported. If consistently observed in other cohorts, this would support the use of CSF levels of αSyn as a potential biomarker of synaptic dysfunction.
This study has several limitations. Although large for cohorts of individuals with DS, the small sample size limits the statistical power required to identify differences of small magnitude and to allow proper control for potentially important covariates. The small number also reduces our ability to draw conclusions that may be generalizable to the DS population as a whole. Lack of an age‐matched comparator control group without DS limits our ability to define general trisomy 21–related effects. Heterogeneity in CSF sample collection procedures (eg, method and timing of LP) in ABC‐DS may also influence analyte recovery, notably Aβ peptides known to exhibit diurnal variability. 34 However, the use of the ratio of CSF Aβ42/Aβ40 as a marker of amyloid helps reduce this potential effect.
Our understanding of the timing of pathologic processes that develop over the entire natural course of AD (from CS through stages of cognitive and functional decline) has been made possible by biomarker evaluation. Recent data from the largest international ADAD cohort (Dominantly Inherited Alzheimer Network, DIAN) demonstrated abnormalities in CSF markers of all pathologic processes (including amyloid, tau, neuronal injury, synaptic dysfunction, and neuroinflammation) in AD mutation carriers during the 20 to 30 year asymptomatic/preclinical period, with CSF concentrations of biomarkers increasing in abnormality as individuals approached their estimated age of symptom onset. 5 Despite challenges unique to the DS population (eg, heterogeneity in premorbid cognitive abilities, heterogeneity in the prevalence and age‐of‐onset of dementia, and existence of comorbidities due to the triplication of chromosome 21), longitudinal clinical and biomarker studies such as ABC‐DS are critical to better define AD‐related processes that will enable early diagnosis, disease staging, elucidation of clinically relevant targets for clinical trials, and eventually, the discovery of effective interventions in this high‐risk population.
CONFLICTS OF INTEREST
Ms. Henson, Mr. Doran, and Drs. Christian, Handen, Klunk, Lai, Lee, Rosas, Schupf, Zaman, and Lott report no conflicts. Dr. Fagan has received research support from Biogen, Fujirebio, and Roche Diagnostics. She is a member of the scientific advisory boards for Roche Diagnostics, Genentech, and AbbVie, and she also consults for Araclon/Griffols, DiademRes, and Otsuka Pharmaceuticals.
ACKNOWLEDGMENTS
The Alzheimer's Biomarkers Consortium–Down Syndrome (ABC‐DS) is funded by the National Institute on Aging and the Eunice Kennedy Shriver National Institute for Child Health and Human Development (U01 AG051406 and U01 AG051412). The work contained in this publication was also supported through the following National Institutes of Health Programs: The Alzheimer's Disease Research Centers Program (P50 AG008702, P30 AG062421, P50 AG16537, P50 AG005133, P50 AG005681, and P30 AG062715), the Eunice Kennedy Shriver Intellectual and Developmental Disabilities Research Centers Program (U54 HD090256 and U54 HD087011), the National Centers for Advancing Translational Sciences (UL1TR001873, UL1 TR002373, UL1 TR001414, UL1 TR001857, and UL1 TR002345), the National Centralized Repository for Alzheimer Disease and Related Dementias (U24 AG021886), and DS‐Connect (The Down Syndrome Registry) supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
The authors thank the ABC‐DS study participants (adults with Down syndrome), their families and care providers, and the ABC‐DS research and support staff for their invaluable contributions to this study. Dr. Beau Ances provided insightful comments. The content is the sole responsibility of the authors and does not necessarily represent the official views of the NIH.
Henson RL, Doran E, Christian BT, et al. Cerebrospinal fluid biomarkers of Alzheimer's disease in a cohort of adults with Down syndrome. Alzheimer's Dement. 2020;12:e12057 10.1002/dad2.12057
Alzheimer's Biomarkers Consortium‐Down Syndrome(ABC‐DS) Investigators: Howard J. Aizenstein, MD, PhD; Beau M. Ances, MD, PhD; Howard F. Andrews, PhD; Karen Bell, MD; Rasmus M. Birn, PhD; Adam M. Brickman, PhD; Peter Bulova, MD; Amrita Cheema, PhD; Kewei Chen, PhD; Bradley T. Christian, PhD; Isabel Clare, PhD; Lorraine Clark, PhD; Ann D. Cohen, PhD; John N. Constantino, MD; Eric W. Doran, MS; Anne M. Fagan, PhD; Eleanor Feingold, PhD; Tatiana M. Foroud, PhD; Benjamin L. Handen, PhD; Sigan L. Hartley, PhD; Elizabeth Head, PhD; Rachel L. Henson, MS; Christy Hom, PhD; Lawrence Honig, MD; Milos D. Ikonomovic, MD; Sterling C. Johnson, PhD; Courtney Jordan, RN; M. Ilyas Kamboh, PhD; David Keator, PhD; William E. Klunk MD, PhD; Julia K. Kofler, MD; William Charles Kreisl, MD; Sharon J. Krinsky‐ McHale, PhD; Florence Lai, MD; Patrick Lao, PhD; Charles Laymon, PhD; Joseph Hyungwoo Lee, DrPH; Ira T. Lott, MD; Victoria Lupson, PhD; Mark Mapstone, PhD; Chester A. Mathis, PhD; Davneet Singh Minhas, PhD; Neelesh Nadkarni, MD; Sid O'Bryant, PhD; Deborah Pang, MPH; Melissa Petersen, PhD; Julie C. Price, PhD; Margaret Pulsifer, PhD; Michael S. Rafii, MD, PhD; Eric Reiman, MD; Batool Rizvi, MS; Herminia Diana Rosas, MD; Marwan N. Sabbagh, MD; Nicole Schupf, PhD; Wayne P. Silverman, PhD; Dana L. Tudorascu, PhD; Rameshwari Tumuluru, MD; Benjamin Tycko, MD, PhD; Badri Varadarajan, PhD; Desiree A. White, PhD; Michael A. Yassa, PhD; Shahid Zaman, MD, PhD; Fan Zhang, PhD.
REFERENCES
- 1. Lott IT, Head E. Dementia in Down syndrome: unique insights for Alzheimer disease research. Nat Rev Neurol. 2019;15:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zigman WB, Schupf N, Sersen E, Silverman W. Prevalence of dementia in adults with and without Down syndrome. Am J Ment Retard. 1996;100:403‐412. [PubMed] [Google Scholar]
- 3. McDade E, Wang G, Gordon BA, et al. Longitudinal cognitive and biomarker changes in dominantly inherited Alzheimer disease. Neurology. 2018;91:e1295–e1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sutphen CL, Jasielec MS, Shah AR, et al. Longitudinal cerebrospinal fluid biomarker changes in preclinical Alzheimer disease during middle age. JAMA Neurol. 2015;72:1029‐1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schindler SE, Li Y, Todd KW, etal. Emerging cerebrospinal fluid biomarkers in autosomal dominant Alzheimer's disease. Alzheimer's Dement. 2019;15(5):655‐665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tarawneh R, D'Angelo G, Macy E, et al. Visinin‐like protein‐1: diagnostic and prognostic biomarker in Alzheimer disease. Ann Neurol. 2011;70:274‐285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mattsson N, Insel PS, Palmqvist S, et al. Cerebrospinal fluid tau, neurogranin, and neurofilament light in Alzheimer's disease. EMBO Mol Med. 2016;8:1184‐1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kester MI, Teunissen CE, Crimmins DL, et al. Neurogranin as a cerebrospinal fluid biomarker for synaptic loss in symptomatic Alzheimer disease. JAMA Neurol. 2015;72:1275‐1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tarawneh R, D'Angelo G, Crimmins D, et al. Diagnostic and prognostic utility of the synaptic marker neurogranin in Alzheimer disease. JAMA Neurol. 2016;73:561‐571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sutphen CL, McCue L, Herries EM, etal. Longitudinal decreases in multiple cerebrospinal fluid biomarkers of neuronal injury in symptomatic late onset Alzheimer's disease. Alzheimer's Dement. 2018;14(7):869‐879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Craig‐Schapiro R, Perrin RJ, Roe CM, et al. YKL‐40: a novel prognostic fluid biomarker for preclinical Alzheimer's disease. Biol Psychiatry. 2010;68:903‐912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Piccio L, Deming Y, Del‐Águila JL, et al. Cerebrospinal fluid soluble TREM2 is higher in Alzheimer disease and associated with mutation status. Acta Neuropathol. (Berl.) 2016;131:925‐933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Suárez‐Calvet M, Araque Caballero MA, Kleinberger G, et al. Early changes in CSF sTREM2 in dominantly inherited Alzheimers disease occur after amyloid deposition and neuronal injury. Sci Transl Med. 2016;8:369ra178‐369ra178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Molinuevo JL, Ayton S, Batrla R, et al. Current state of Alzheimer's fluid biomarkers. Acta Neuropathol. (Berl.) 2018;136:821‐853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Twohig D, Rodriguez‐Vieitez E, Sando SB, et al. The relevance of cerebrospinal fluid α‐synuclein levels to sporadic and familial Alzheimer's disease. Acta Neuropathol. Commun. 2018;6:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Korff A, Liu C, Ginghina C, Shi M, Zhang J α‐Synuclein in cerebrospinal fluid of Alzheimer's disease and mild cognitive impairment. J Alzheimers Dis. 2013;36:679‐688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fortea J, Carmona‐Iragui M, Benejam B, et al. Plasma and CSF biomarkers for the diagnosis of Alzheimer's disease in adults with Down syndrome: a cross‐sectional study. Lancet Neurol. 2018;17:860‐869. [DOI] [PubMed] [Google Scholar]
- 18. Portelius E, Soininen H, Andreasson U, et al. Exploring Alzheimer molecular pathology in Down's Syndrome cerebrospinal fluid. Neurodegener Dis. 2014;14:98‐106. [DOI] [PubMed] [Google Scholar]
- 19. Lee N‐C, Chien Y‐H, Hwu W‐L. A review of biomarkers for Alzheimer's disease in Down syndrome. Neurol Ther. 2017;6:69‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Corder EH, Saunders A, Strittmatter W, etal. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science. 1993;261:921‐923. [DOI] [PubMed] [Google Scholar]
- 21. Aylward EH, Burt DB, Thorpe LU, Lai F, Dalton A. Diagnosis of dementia in individuals with intellectual disability. J Intellect Disabil Res. 1997;41:152‐164. [DOI] [PubMed] [Google Scholar]
- 22. Burt DB, Aylward EH Test battery for the diagnosis of dementia in individuals with intellectual disability. Working Group for the Establishment of Criteria for the Diagnosis of Dementia in Individuals with Intellectual Disability. J Intellect Disabil Res. 2000;44(Pt 2):175‐180. [DOI] [PubMed] [Google Scholar]
- 23. Crimmins DL, Herries EM, Ohlendorf MF, et al. Double monoclonal immunoassay for quantifying human visinin‐like protein‐1 in CSF. Clin Chem. 2017;63:603‐604. [DOI] [PubMed] [Google Scholar]
- 24. Goldman JG, Andrews H, Amara A, et al. Cerebrospinal fluid, plasma, and saliva in the BioFIND study: Relationships among biomarkers and Parkinson's disease Features. Mov Disord. 2018;33:282‐288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dekker AD, Fortea J, Blesa R, De Deyn PP Cerebrospinal fluid biomarkers for Alzheimer's disease in Down syndrome. Alzheimers Dement Diagn Assess Dis Monit. 2017;8:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mattsson N, Eriksson O, Lindberg O, et al. Effects of APOE ε4 on neuroimaging, cerebrospinal fluid biomarkers, and cognition in prodromal Alzheimer's disease. Neurobiol Aging. 2018;71:81‐90. [DOI] [PubMed] [Google Scholar]
- 27. Pastor P, Roe CM, Villegas A, et al. Apolipoprotein Eepsilon4 modifies Alzheimer's disease onset in an E280A PS1 kindred. Ann Neurol. 2003;54:163‐169. [DOI] [PubMed] [Google Scholar]
- 28. Ryman DC, Acosta‐Baena N, Aisen PS, etal. Symptom onset in autosomal dominant Alzheimer disease. Neurology. 2014;83:253‐260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vélez JI, Lopera F, Sepulveda‐Falla D, etal. APOE*E2 allele delays age of onset in PSEN1 E280A Alzheimer's disease. Mol Psychiatry. 2016;21:916‐924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Morris JC, Roe CM, Xiong C, etal. APOE predicts Aβ but not tau Alzheimer's pathology in cognitively normal aging. Ann Neurol. 2010;67:122‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang S, Zhang J, Pan T. APOE ε4 is associated with higher levels of CSF SNAP‐25 in prodromal Alzheimer's disease. Neurosci Lett. 2018;685:109‐113. [DOI] [PubMed] [Google Scholar]
- 32. Palmqvist S, Insel PS, Stomrud E, etal. Cerebrospinal fluid and plasma biomarker trajectories with increasing amyloid deposition in Alzheimer's disease. EMBO Mol Med. 2019;11(12):e11170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Koob AO, Shaked GM, Bender A, et al. Neurogranin binds α‐synuclein in the human superior temporal cortex and interaction is decreased in Parkinson's disease. Brain Res. 2014;1591:102‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dobrowolska JA, Kasten T, Huang Y, et al. Diurnal patterns of soluble amyloid precursor protein metabolites in the human central nervous system. PLoS One. 2014;9:e89998. [DOI] [PMC free article] [PubMed] [Google Scholar]


