Abstract
Introduction:
Undernutrition is continuing to be a major public health problem in India. Moreover, India houses more than 30% of the world's stunted children aged under 5 years. There was a paucity of a community-based cross-sectional study on the nutrition of children aged under 5 years in urban Delhi. Therefore, we conducted this study to assess the prevalence of undernutrition and their associated factors in children aged under 5 years in urban South Delhi.
Materials and Methods:
A cross-sectional community-based study was conducted in the Mehrauli area of South Delhi with a semi-structured questionnaire. Systematic random sampling without replacement was implemented. Informed written consent was sought from the parents of participants. Questions were asked regarding demography and sociocultural factors of the participants. Anthropometry measurements were obtained. Underweight and stunting were defined using WHO child growth standards 2006.
Results:
A total of 520 participants in 695 houses were contacted and interviewed. Prevalence of underweight and stunting were 34.0% and 42.6%, respectively. Sociocultural factors, associated with underweight and stunting, found in current study were fathers' education (with both, P value < 0.05), mothers' education (with both, P value < 0.05), poverty status (with both, P value <0.05), overcrowding (stunting only, P value <0.05), fathers' alcohol abuse (with both, P value < 0.05) and exclusive breastfeeding for 6 months (stunting only, P value <0.05).
Results:
A total of 520 participants in 695 houses were contacted and interviewed. Prevalence of underweight and stunting were 34.0% and 42.6%, respectively. Sociocultural factors, associated with underweight and stunting, found in current study were fathers' education (with both, P value < 0.05), mothers' education (with both, P value < 0.05), poverty status (with both, P value <0.05), overcrowding (stunting only, P value <0.05), fathers' alcohol abuse (with both, P value < 0.05) and exclusive breastfeeding for 6 months (stunting only, P value <0.05).
Conclusions:
There was a very high prevalence of underweight (34.0%) and stunting (42.6%) in children under 5 years age in Mehrauli.
Keywords: Children, Delhi, India, stunting, prevalence, undernutrition, underweight
Introduction
Undernutrition is a silent public health emergency worldwide. It is continuing to be a major public health problem in India. It is not the only indicator of poor nutrition but also a threat to the social and economic development of the population.[1] Globally, it is one of the most common causes of morbidity and mortality among children.[2] Each year, about 10 million children die due to preventable or treatable illnesses, and half of these deaths are directly or indirectly caused by undernutrition.[3]
The World Health Assembly in 2012 aimed to reduce the global burden of malnourishment in children aged under 5 years by 40% by 2025 from a pool of 171 million in 2010.[4] Sustainable Development Goals (SDG) also aimed to end all forms of malnutrition by 2030.[5] India, which has more than 30% of the global burden of stunted children aged under 5 years, succeeded to reduce the prevalence of malnutrition from 42.5% to 35.7% over the last decade.[6,7] Improved socioeconomic conditions, a reduced burden of infectious diseases, and changes in treatment modalities and their approach were the key factors that played a major role. In spite of this continuing progress, the country is still burdened with 8.1 million children suffering from severe acute malnutrition.[8,9] This undernutrition, over a period of time, results in delayed physical growth, impaired cognitive and motor development, low IQ (intellectual quotient), deteriorated cognitive performance, poor social skills, behavior problems, and susceptible to contracting diseases.[3,10]
At the community level, poor sanitation, the practice of open defecation, and repeated infections (diarrhoea, pneumonia, malaria, and worm infestations) have been implicated as the cause of such a high proportion of undernutrition in India.[11,12] Undernutrition among children is also associated with inappropriate infant and young child-feeding practices including prelacteal feeding and faulty exclusive breastfeeding, late introduction of solid food, low quality of complementary foods, food insecurity and high rates of gastrointestinal infections, and parasitic infestations.[3,11,13]
Nutritional status of preschool children is a sensitive indicator of community health and nutrition.[11,14] Therefore, it will be very useful for primary healthcare providers to have information about risk factors for undernutrition in children. Nutritional status of children aged under 5 years and its associated factors are not uniformly distributed within the country and varies from state to state. Although undernutrition in under-five children in India have been adequately studied,[15,16,17,18,19] but undernutrition and associated factors among migrant workers' children has not been studied thoroughly. Therefore, we planned this study to assess prevalence and risk factors of underweight and stunting in children under 5 years of age in an urban area of South Delhi.
Materials and Methods
A community-based cross-sectional study was conducted in Mehrauli, New Delhi, India. This is a relatively lesser developed area of South Delhi comprising of 9 administrative wards. One ward (no. 9) was selected by simple random sampling. Majority of the residents of this ward were migrant laborers working in unorganized sectors.
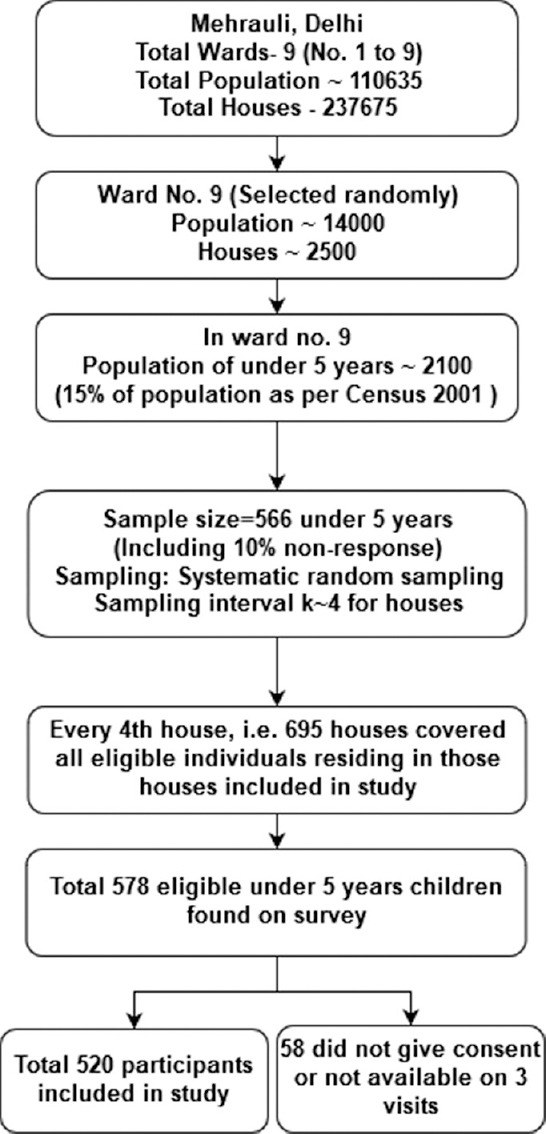
According to Census 2001,[20] population of Mehrauli was 1,10635 distributed among 23,675 houses divided into 9 wards. Of these, an estimated population of 14000 reside in nearly 2500 houses in ward 9, of which around 2100 (15%[20] of 14000) were with children aged under 5-year. An equal distribution of children aged under-five years was considered across the 2500 houses for the sampling frame. The calculated sample size was 566 considering prevalence of 42.2% of underweight under 5 years of age children (NFHS-3),[21] 10% relative precision and 10% nonresponse rate using formula (1.962*p*q)/d2 [Figure 1].
Figure 1.
Sampling methods
Systematic random sampling without replacement was employed and every fourth house was visited in ward 9 of Mehrauli. All eligible subjects (and their families) in every visited house were contacted and invited to participate in the study. Those subjects, whose family provided consent, were enrolled in the study. Children of under 5 years (less than 60 months) of age were included in this study. Age was verified with birth records if available. If birth records were not available, parents (or caretaker) were interviewed for confirmation of age using memories of indigenous calendar dates and local events that coincided with the birth of the child. Data collection was done in the year 2010.
A semi-structured questionnaire was used to collect data. It comprised of questions related to the demography of the participants, anthropometry of participants, sociocultural, and dietary characteristics. Interview of the mother, father, or any other caretaker of children was done.
The weight was measured using an infant weighing scale for less than 2 years of age and for more than 2 years of age portable electronic scale (precision 100 g) was used. Standard fiberglass infantometer (range 30–110 cm, precision 1 mm) was used to measure the length of children up to 2 years of age and portable stadiometer (precision of 1 mm) was used for height measurement of children of more than 2 years of age. Nutritional assessment was done using WHO child growth standards (2006).[22] Children with less than 2 standard deviation cutoffs of weight-for-age and height-for-age were considered as underweight and stunted, respectively.
Father was considered as having alcohol abuse if he was observed fulfilling one or more criteria of DSM-4 criteria (Diagnostics and Statistical Manual of Mental Disorders-IV)[23] for more than 1 year. The DSM-4 criteria's were as follows (i) role impairment (e.g. failed work or home obligations); (ii) hazardous use (e.g. driving, swimming or operating machinery while intoxicated); (iii) legal problems related to alcohol use; (iv) social or interpersonal problems due to alcohol.
The children who were found malnourished were referred to a nearby urban primary health center. The study was approved by the Institutional Ethics Committee of Lady Hardinge Medical College, New Delhi. A patient information sheet was provided to all participants (and their families) and was included in the study only after obtaining written informed consent of one of the parent. No funding was taken for this study.
Data entry and statistical analysis were performed using SPSS version 18.0 (SPSS Inc., Chicago). All the categorical variables were presented as frequency tables. Hypothesis testing was done using the Chi-square test for the categorical variable. A P value less than 0.05 was considered statistically significant.
Results
A community-based data collection study was conducted. On the survey, it was found that there were 2780 houses in ward 9 of Mehrauli. Total 695 houses (every fourth house) were visited and 578 children of under 5 years of age were available in those houses. Families of 40 children refused to participate in the study and 18 children were found to be not available on 3 repeated visits. Thus, 58 subjects were excluded from the final analysis and data were entered and analyzed for 520 children only.
There were 51.2% (n = 265) girls and 48.8% (n = 255) boys with most common age group involved being 12–24 month (n = 151, 29.0%) followed by 0–12 month (n = 122, 23.5%). Most participants were Hindus (n = 429, 82.5%) and belonged to nuclear families (n = 445, 85.6%). Only few (n = 27, 5.2%) participants were belong to families that had below poverty line card (BPL card).
Prevalence of underweight children was 34.0% (177 out of 520). In the gender-wise distribution of underweight children, 31.4% (80 out of 255) males were underweight as compared to 36.6% (97 out of 255) females (nonsignificant). Children belong to nuclear families were having a prevalence of 35.1% underweight as compared to 28.0% in children belong to joint families (nonsignificant). Prevalence of underweight children in houses where overcrowding was present by “person per room criteria“[10] was 39.1% as compared to 32% in those, where overcrowding was absent (nonsignificant). Those children who had exclusive breastfeeding for 6 months showed 57.9% prevalence of underweight as compared to 30.0% in those who were exclusively breastfed for less than 6 months or not exclusively breastfed for any duration (nonsignificant) [Table 1].
Table 1.
Association of underweight and sociocultural factors
| Sociocultural factors | Weight for age <2 SD (underweight) numbers n=177 | Weight for age >2SD numbers n=343 | Chi-square test, P |
|---|---|---|---|
| Gender | 1.584, 0.21 | ||
| Male | 80 (31.4) | 175 (68.6) | |
| Female | 97 (36.6) | 168 (63.4) | |
| Religion | 0.56, 0.812 | ||
| Hindu | 147 (34.3) | 282 (65.7) | |
| Muslim/Christian/Sikh | 30 (33.0) | 61 (67.0) | |
| Family Type | 1.423, 0.233 | ||
| Nuclear | 156 (35.1) | 289 (64.9) | |
| Joint | 21 (28.0) | 54 (72.0) | |
| Father’s education | 25.24, <0.001 | ||
| Schooling up to 10th | 154 (40.3) | 228 (59.7) | |
| Schooling 11th or more | 23 (16.7) | 115 (83.3) | |
| Mother’s education | 31.97, <0.001 | ||
| Schooling up to 10th | 169 (39.5) | 259 (60.5) | |
| Schooling 11th or more | 8 (8.7) | 84 (91.3) | |
| Poverty (BPL card) | 16.74, <0.001 | ||
| Below poverty line | 19 (70.4) | 8 (29.6) | |
| Above poverty line | 158 (32.0) | 335 (68.0) | |
| Overcrowding (person per room criteria) | 2.4, 0.121 | ||
| Present | 59 (39.1) | 92 (60.9) | |
| Absent | 118 (32.0) | 251 (68.0) | |
| Father alcohol abuse | 22.56, <0.001 | ||
| Yes | 44 (57.9) | 32 (42.1) | |
| No | 133 (30.0) | 311 (70.0) | |
| Exclusive breastfeeding for 6 months | 2.98, 0.085 | ||
| Present | 19 (25.3) | 56 (74.7) | |
| Absent | 158 (35.5) | 287 (64.5) |
Figures in parentheses represent row-wise percentages
In the present study, important factors associated with the underweight occurrence were fathers' education, mothers' education, poverty status, and fathers' alcohol abuse status. Fathers' education beyond 10th class had a significantly lower prevalence of 16.7% of underweight as compared to fathers' education up to or below 10th class where underweight prevalence was 40.3% (P < 0.001). Similarly, mothers' education beyond 10th class witnessed only 8.7% underweight as compared to 39.5% when mother's education was up to or below 10th class (P < 0.001). Below poverty line families showed a 70% prevalence of underweight as compared to only 32.0% in families above the poverty line (P < 0.001). Fathers' alcohol abuse status also affected the prevalence of underweight among under 5 years children. Children with fathers' having alcohol abuse, showed 57.9% prevalence of underweight whereas it was only 30.0% in children without this factor (significant, <0.001) [Table 1].
Prevalence of stunting was 42.6% (222 out of 520 children) among all children aged under 5 years. Significantly (P < 0.05) associated factors with stunting were fathers' education (50.5% in education up to 10th, 21.0% in education 11th or more, P value <0.001), mothers' education (47.7% in education up to 10th, 19.6% in education 11th or more, P value <0.001), poverty status (92.6% in BPL, 40.0% in APL, P value <0.001), overcrowding (51.7% in children with overcrowding present, 39.0% in children with overcrowding absent, P value 0.008), fathers' alcohol abuse (77.6% in children with fathers' alcohol abuse, 36.7% in children having father without alcohol abuse, P value <0.001), and exclusive breastfeeding for 6 months (21.3% in children exclusively breastfed for 6 months, 46.3% in children less than months or not exclusively breastfed, P value <0.001) [Table 2]. Other factors such as gender, religion, and family type were not found to be associated with stunting [Table 2].
Table 2.
Association of stunting and sociocultural factors
| Sociocultural factors | Height/length for age <2 SD (stunting) numbers n=222 | Height/length for age >2 SD numbers n=298 | Chi-square test, P |
|---|---|---|---|
| Gender | 2.47, 0.116 | ||
| Male | 100 (39.2) | 155 (60.8) | |
| Female | 122 (46.0) | 143 (54.0) | |
| Religion | 0.938, 0.333 | ||
| Hindu | 179 (41.7) | 250 (58.3) | |
| Muslim/Christian/Sikh | 43 (47.3) | 48 (52.7) | |
| Family Type | 3.138, 0.077 | ||
| Nuclear | 197 (44.3) | 248 (55.7) | |
| Joint | 25 (33.3) | 50 (66.7) | |
| Father’s education | 36.082, <0.001 | ||
| Schooling up to 10th | 193 (50.5) | 189 (49.5) | |
| Schooling 11th or more | 29 (21.0) | 109 (79.0) | |
| Mother’s education | 24.436, <0.001 | ||
| Schooling up to 10th | 204 (47.7) | 224 (52.3) | |
| Schooling 11th or more | 18 (19.6) | 74 (80.4) | |
| Poverty (BPL card) | 28.984, <0.001 | ||
| Below poverty line | 25 (92.6) | 2 (7.4) | |
| Above poverty line | 197 (40.0) | 296 (60.0) | |
| Overcrowding (person per room criteria) | 6.98, 0.008 | ||
| Present | 78 (51.7) | 73 (48.3) | |
| Absent | 144 (39.0) | 225 (61.0) | |
| Father alcohol abuse | 44.412, <0.001 | ||
| Yes | 59 (77.6) | 17 (22.4) | |
| No | 163 (36.7) | 281 (63.3) | |
| Exclusive breastfeeding for 6 months | 16.342, <0.001 | ||
| Present | 16 (21.3) | 59 (78.7) | |
| Absent | 206 (46.3) | 239 (53.7) |
Figures in parentheses represent row-wise percentages
Discussion
In our study, the prevalence of underweight and stunting were 34.0% and 42.6%, respectively. This shows a very high prevalence of malnutrition. Similar results were also concluded by other studies. As per the National Family Health Survey 4 (NFHS-4)[7] 2015–2016, 35.7% children (<5 years) were underweight, 38.4% were stunted, and 21.0% were wasted in the country. In the same survey (NFHS-4) in Delhi, 32.3%, 17.1%, and 27.0% children of under 5 years were stunted, wasted, and underweight, respectively. Meshram et al. (2012)[24] conducted a community-based cross-sectional survey on malnutrition in 1751 preschool children of 1 to 5 years of age with WHO growth standards. In their survey, they found that the prevalence of underweight, stunting, and wasting was 64.0%, 61.0%, and 29.0%, respectively. Jeyakumar et al. (2019)[25] conducted a cross-sectional study among under 2 years of age children in an urban slum in Pune, Maharashtra. They found that the prevalence of stunting, wasting, and underweight were 34%, 15.3%, and 21.8%, respectively. Swami et al. (2001)[17] reported a high prevalence (51.6%) of protein-energy malnutrition in 1286 preschool children in Chandigarh. Sahu et al. (2019)[26] also documented a very high prevalence (as per the WHO growth chart) of underweight (60.3%) and stunting (46.5%). Similar high prevalence of underweight (25.1%) and stunting (31.2%) was found by Huey et al. (2019, Western Mumbai).[27]
In the current study, the prevalence of underweight in male participants was 31.4% as compared to 36.6% in female participants (nonsignificant difference). Jeyakumar et al. (2019)[25] also found no significant association with gender and undernutrition. Results of Meshram et al. (2012)[24] were different from our study. They found a significant association of gender (more in males as compared to females) with undernutrition (underweight, stunting, and wasting).
In our study, the prevalence of underweight and stunting in Hindu (underweight 34.3%, stunting 41.7%) and other religions (underweight 33.0%, stunting 47.3%) were found to be not significantly different from one another. In this study, we found that family types (nuclear or joint) have no significant differences in the prevalence of underweight or stunting.
In our study, we found that fathers' education, as well as mothers' education (up to 10th class or 11th or more classes), have significant impact on underweight (P-value <0.001 for both mother's and fathers' education) and stunting (P-value <0.001 for both mother's and fathers' education) prevalence in participants. Meshram et al. (2012)[24] also found similar results. They found that underweight prevalence is significantly associated with literacy status (more in illiterates) of the parents. Ray et al. (2001)[18] also reported that malnutrition in under 5 years children is associated with parents' educational status whereas, Jeyakumar et al. (2019)[25] found no significant association between mothers education and undernutrition.
In this study, we found that poverty is an important associated factor with underweight and stunting. Participants having below poverty line card have significantly higher prevalence of underweight (BPL 70.4%, APL 32.0%, P value < 0.001) and stunting (BPL 92.6%, APL 40.0%, P value < 0.001). These results are in accordance with Meshram et al. (2012),[24] where they found that lower wealth index participants had a higher prevalence of undernutrition as compared to higher wealth index participants. Our results are different from the results obtained by Jeyakumar et al. (2019),[25] where they have not found any significant association between socioeconomic class and undernutrition.
In this study prevalence of underweight in participants whose families have overcrowding is 39.1% as compared to 32.0% in those where overcrowding was absent (difference nonsignificant). Effect of overcrowding on stunting (overcrowding present 51.7%, overcrowding absent 39.0%) prevalence was significant (P-value 0.008) in our study. In our study, fathers' alcohol abuse is significantly (P-value < 0.001 for both underweight and stunting) associated factor with underweight (fathers' alcohol abuse present 57.0%, fathers' alcohol abuse absent 30.0%) and stunting (fathers' alcohol abuse present, fathers' alcohol abuse absent) in participants.
In this research, we found that exclusive breastfeeding for 6 months is significantly (P-value <0.001) associated with poor stunting indicators but not with poor underweight indicators. These results are in accordance with Jeyakumar et al. (2019),[25] where they found that the introduction of complementary feeding before 6 months is associated with a higher occurrence of wasting.
Conclusions
In our study, the prevalence of underweight and stunting in children under 5 years of age were 34.0% and 42.6%, respectively in Mehrauli area of South Delhi. Significantly (P-value <0.05) associated factors with the underweight occurrence, found in the current study, were fathers' education, mothers' education, poverty status, and fathers' alcohol abuse status. Furthermore, important factors that were significantly (P-value <0.05) associated with stunting were fathers' education, mothers' education, poverty status, overcrowding, fathers' alcohol abuse, and exclusive breastfeeding for the months.
Declaration of patient consent
The written and informed consent obtained from the parents/guardian. In the form, the parents/guardian has given their consent for anthropometric measurements and related history. The parents/guardian understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
None.
References
- 1.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet (London, England) 2003;361:2226–34. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 2.UNICEF. The State of the World's Children 2005- Childhood under threat UNICEF. 2005. Available from: https://wwwuniceforg/publications/index_24432html . cited 2019 Nov 01.
- 3.Mengistu K, Alemu K, Destaw B. Prevalence of malnutrition and associated factors among children aged 6-59 Months at Hidabu Abote district, North Shewa, Oromia regional state. J Nutr Disord Ther. 2013;T1:1–15. [Google Scholar]
- 4.World Health Organization. Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition. Geneva: WHO; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United Nations. Sustainable DevelopmentGoals. New York, USA: United Nations; 2015. Available from: https://sustainabledevelopmentunorg/topics/sustainabledevelopmentgoals . Cited 2019 Nov 01. [Google Scholar]
- 6.UNICEF India. Nutrition stories from India. New Delhi: UNICEF India; 2019. Available from: https://unicefin/Story/1124/Nutrition . Cited 2019 Nov 01. [Google Scholar]
- 7.International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey-4 (NFHS-4) 2015-16. Mumbai: IIPS; 2017. Available from: http://rchiipsorg/nfhs/factsheet_nfhs-4shtml . Cited 2019 Nov 01. [Google Scholar]
- 8.UNICEF. Strategy for improved nutrition of children and women in developing countries. United Nations Children's Fund. Indian J Pediatr. 1991;58:13–24. doi: 10.1007/BF02810402. [DOI] [PubMed] [Google Scholar]
- 9.Sachdev HP. Assessing child malnutrition: Some basic issues. Bull Nutr Foundations India. 1995;16:1–5. [Google Scholar]
- 10.Park K. Park's Textbook of Preventive and Social Medicine. 24th ed. Jabalpur: Banarsidas Bhanot; 2017. [Google Scholar]
- 11.Sachdev HP, Kapil U, Vir S. Consensus Statement National Consensus Workshop on Management of SAM Children through Medical Nutrition Therapy. Indian Pediatr. 2010;47:661–5. doi: 10.1007/s13312-010-0097-z. [DOI] [PubMed] [Google Scholar]
- 12.Bloss E, Wainaina F, Bailey RC. Prevalence and predictors of underweight, stunting, and wasting among children aged 5 and under in western Kenya. J Trop Pediatr. 2004;50:260–70. doi: 10.1093/tropej/50.5.260. [DOI] [PubMed] [Google Scholar]
- 13.Meshram II, Laxmaiah A, Reddy GC, Ravindranath M, Venkaiah K, Brahmam GN. Prevalence of under-nutrition and its correlates among under 3 year-old children in rural areas of Andhra Pradesh, India. Ann Hum Biol. 2011;38:93–101. doi: 10.3109/03014460.2010.498387. [DOI] [PubMed] [Google Scholar]
- 14.WHO, UNICEF, USAID, AED, UCDAVIS, IFPRI. Indicators for assessing infant and young child feeding practices. Geneva: WHO; 2008. Available from: https://www.who.int/nutrition/publications/infantfeeding/9789241596664/en/ Cited 2019 Nov 01. [Google Scholar]
- 15.Kumar HN, Mohanan P, Kotian S, Sajjan BS, Kumar SG. Prevalence of overweight and obesity among preschool children in semi urban South India. Indian Pediatr. 2008;45:497–49. [PubMed] [Google Scholar]
- 16.Rao S, Joshi SB, Kelkar RS. Changes in nutritional status and morbidity over time among pre-school children from slums in Pune, India. Indian Pediatr. 2000;37:1060–71. [PubMed] [Google Scholar]
- 17.Swami HM, Thakur JS, Bhatia SP, Bhatia V. Nutritional status of pre-school children in an integrated child development service (ICDS) block of Chandigarh. J Indian Med Assoc. 2001;99:554–6. [PubMed] [Google Scholar]
- 18.Ray SK, Haldar A, Biswas B, Misra R, Kumar S. Epidemiology of undernutrition. Indian J Pediatr. 2001;68:1025–30. doi: 10.1007/BF02722348. [DOI] [PubMed] [Google Scholar]
- 19.Laxmaiah A, Rao KM, Brahmam GN, Kumar S, Ravindranath M, Kashinath K, et al. Diet and nutritional status of rural preschool children in Punjab. Indian Pediatr. 2002;39:331–8. [PubMed] [Google Scholar]
- 20.Office of the Registrar General and Census Commissioner India. Census Data 2001. New Delhi: Government of India; 2001. [Google Scholar]
- 21.International Institute for Population Sciences (IIPS) National Family Health Survey -3 (NHFS-3) Mumbai: International Institute for Population Sciences (IIPS); 2007. Available from: http://rchiipsorg/NFHS/nfhs3_national_reportshtml . Cited 2019 Nov 01. [Google Scholar]
- 22.World Health Organization. The WHO Child Growth Standards. Geneva: WHO; 2006. Available from: https://wwwwhoint/childgrowth/standards/en/ Cited 2019 Nov 01. [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 24.Meshram II, Arlappa N, Balakrishna N, Laxmaiah A, Mallikarjun Rao K, Gal Reddy C, et al. Prevalence and determinants of undernutrition and its trends among pre-school tribal children of Maharashtra State, India. J Trop Pediatr. 2012;58:125–32. doi: 10.1093/tropej/fmr035. [DOI] [PubMed] [Google Scholar]
- 25.Jeyakumar A, Nikam S, Nayak S. Prevalence and risk factors of undernutrition among children less than 2 years in urban slums of Pune, Maharashtra, India. Ecology Food Nutr. 2019;58:456–69. doi: 10.1080/03670244.2019.1613985. [DOI] [PubMed] [Google Scholar]
- 26.Sahu SK, Rajaa S, Vijayageetha M, Selvaraj K, Sambath PM, Roy G. Strengthening growth monitoring among under-5-year children to fight childhood undernutrition in India. J Family Med Prim Care. 2019;8:231–8. doi: 10.4103/jfmpc.jfmpc_225_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huey SL, Finkelstein JL, Venkatramanan S, Udipi SA, Ghugre P, Thakker V, et al. Prevalence and correlates of undernutrition in young children living in urban slums of Mumbai, India: A cross sectional study. Front Public Health. 2019;7:191. doi: 10.3389/fpubh.2019.00191. [DOI] [PMC free article] [PubMed] [Google Scholar]


