Abstract
Introduction:
World Health Organization (WHO) initiated a global movement to achieve universal health coverage (UHC). Hand hygiene (HH) is critical for achieving UHC as it is a practical and evidence-based approach with a gaugeable impact on the quality of care and patient safety in healthcare.
Material and Methods:
A cross-sectional observational study was conducted in an intensive care unit of a government hospital spanning a period of 3 years. WHO single-observer direct observation technique was used and HH compliance was noted. The results were compared over the years since the hospital was preparing to undergo a National Accreditation Board for Hospitals and Healthcare (NABH) assessment.
Results:
The overall compliance significantly increased over the years (P < 0.0001). HH compliance for hand rub (HR) and hand wash (HW) was compared among doctors, nurses, and ICU technicians, respectively. HR compliance remained more or less the same over the years (P = 0.4738) while HW compliance significantly improved (P < 0.0001).
Conclusions:
This is one of the first studies from our country evaluating HH compliance over the years in a healthcare setup undergoing accreditation. During the course of the study, we observed a significant increase in HH compliance. This can be attributed to the unflinching support of our hospital's administration and relentless efforts of our infection control team. This is our first step initiative towards improving HH and thus preventing healthcare-associated infections (HCAIs) in our setup.
Keywords: Direct observation technique, healthcare-associated infections, national accreditation board for hospitals and healthcare, universal health coverage, world health organization
Introduction
Hand hygiene (HH) is vital for infection control.[1] Ignaz Semmelweis in Vienna, Austria, and Oliver Wendell Holmes in Boston, USA, emphasized the significance of HH in a healthcare facility in mid-1800.[2]
As part of a major global initiative to improve HH in healthcare, the World Health Organization (WHO) launched a global campaign “SAVE LIVES: Clean Your Hands“ in 2009. It was a natural extension of the WHO's First Global Patient Safety Challenge: Clean Care is Safer Care.[2] As part of the campaign, WHO urges policymakers, administrators, infection control officers, healthcare workers (HCWs), and other patient care groups to contribute towards the implementation of HH as a keystone to improve healthcare quality.[1]
Over the years, HH compliance has been found to be low worldwide. Several studies from India have reported HH compliance ranging from 20–85.5%.[3,4,5,6,7] Mathur has reviewed the situation of HH around the globe and has listed a few factors responsible for low compliance in healthcare setup including physician status (rather than nurse), male sex, lack of role models, working during the week (or weekend), understaffing, patient overcrowding, insufficient time, HW agents causing dryness, and so on.[8]
National Accreditation Board for Hospitals and Healthcare providers (NABH) is an institutional member of the International Society for Quality in Health Care (ISQua), established to set a benchmark towards improving quality of healthcare institutes.[9] HH is an effective measure to prevent healthcare-associated infections (HCAIs) and thus improve the quality of patient care.[2]
There is an ever-growing burden of HCAIs in our country. The situation has worsened with the emergence of antimicrobial resistance (AMR) among pathogens of public health importance.[10] Universal health coverage (UHC) means that all people and communities can utilize the health services of sufficient quality thereby ensuring that the use of these services does not expose the user to financial hardship. HCAIs are drawing increasing attention from healthcare providers, patients as well as governments, as they provide a roadblock to UHC.[8]
This is one of the first studies from our country evaluating HH compliance over the years in a healthcare setup undergoing NABH accreditation.
Material and Methods
A cross-sectional observational study was conducted spanning a period of 3 years. A single-observer direct observation technique was used and HH data was collected. The study was conducted in an intensive care unit (ICU) of Dr. Baba Saheb Ambedkar Hospital and Medical College. Health care worker (HCW) s including doctors, nurses, technicians and nursing students were observed during routine patient care. HH compliance was noted for all five moments of HH as per WHO observation form 2009.[2] Results were calculated for overall compliance as well as under the professional category. The results were compared over the years while the hospital was preparing for undergoing NABH assessment. Data were expressed as percentages. The differences in percentages were statistically compared, tested for significance by using Fisher's exact test, and P value was determined.
Results
During this analysis, 266 HH opportunities were observed in 2015, 220 in 2016, and 290 in 2017. The overall HH compliance was 21% (56/266 opportunities) in 2015, 20% (44/220) in 2016, and 59% (171/290) in 2017. A significant increase in HH compliance was observed over the years (P < 0.0001) as seen in Figure 1.
Figure 1.
Hand hygiene compliance comparison between 2015, 2016, and 2017
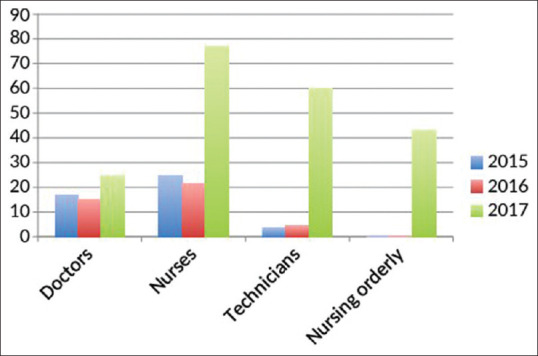
The compliance was compared among individual categories as well as for each moment of HH. Figure 2 highlights the fact that the nurses fared best among the HCW while doctors were the least compliant group.
Figure 2.
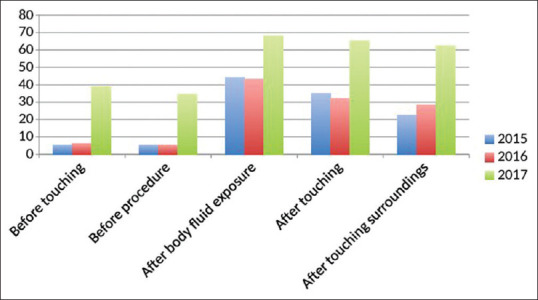
Hand hygiene compliance comparison according to the five moments of hand hygiene between 2015, 2016, and 2017
HH compliance for hand rub (HR) compared to hand wash (HW) was found to be 1.9:1,1.6:1, 2:1, and 1:1, 1:4, 1:2, among doctors, nurses, and ICU technicians in 2015 and 2017, respectively. The overall compliance for HR was found to be 15%, 12%, and 13% while it was 6%, 8%, and 46% for HW in 2015, 2016, and 2017, respectively. HR compliance remained more or less the same over the years (P = 0.4738) while HW compliance significantly improved (P < 0.0001).
Discussion
WHO initiated a global movement to achieve UHC i.e. achieving better health and well-being for all people (irrespective of their age or financial status) and access to quality essential healthcare services. Every year in support of the WHO's “Save Lives: Clean Your Hands“ campaign, we observe World Hand Hygiene Day on the 5th of May as depicted in Figure 3. As part of this, the HCWs are encouraged to participate in events such as poster competitions, role-play, etc. Reward stars are given as a token of appreciation for their efforts.
Figure 3.

Hand hygiene day celebration at our hospital
We used direct observation method for WHO's five moments of HH as it is still considered the gold standard providing qualitative and quantitative information.[11] In a study conducted by Shah et al., video surveillance was used to observe HH compliance.[6] In another study, observational method, product use method, and electronic surveillance were compared and the overall rate of HH adherence calculated.[12] In another study conducted by Nair et al. the knowledge, attitude, and practice of HH among nursing and medical students were evaluated using WHO's questionnaire for HCWs. Overall nursing students fared better than medical students.[13] Direct observation method has a few limitations. It is time-consuming, it requires a dedicated trained staff, and there is a chance of observation bias-the Hawthorne effect.[14] However, in our hospital, we do not have electronic soap dispensers/electronic surveillance technology. Therefore, a single-observer direct observation technique was used and compliance with all five moments of HH was evaluated.
Overall HH compliance in our study ranged from 21–59% over the years. A systematic review from industrialized countries reported compliance rates for ICU ranging from 30–40%.[15] Compliance as low as 8% to as high as 85% has been reported in various studies across the world and in India as shown in Table 1.[3,4,5,6,7,16]
Table 1.
Hand hygiene compliance studies in healthcare setup conducted in India over the last 10 years
| Study | Study period | Place | HH compliance measurement method | HH Opportunities observed | HH compliance (%) | HH compliance following intervention |
|---|---|---|---|---|---|---|
| Chavali (2014) | 10 days | Pune | DOT | 1500 | 78 | - |
| Sharma (2011) | 60 days | Punjab | DOT | 911 | 43.2 | - |
| Tyagi (2018) | 120 days | Telangana | DOT | 3661 | 23(NICU) | - |
| 235 | 34(labour room) | |||||
| Shah (2015) | 7 days | Gujarat | video-surveillance | 1081 | 85.5 | - |
| Sastry (2017) | 1 year | Pondicherry | DOT | 1080 | 45.5 | - |
| Present study | 3 years | Delhi | DOT | 646 | 21 | 59 |
During the course of the study, we observed a significant increase in HH compliance (P < 0.0001) from a modest 21% to 59% in 2017. This can be attributed to the consorted effort of our hospital's administration and infection control team. The increased awareness and dedication towards HH can also be attributed to the fact that our hospital was preparing for accreditation. In another Indian study conducted by Chavali et al. in an accredited hospital, a substantially high HH compliance was noted. The study was conducted after 1 year of dedicated training which could be the reason for such high compliance rates observed, thus reflecting the importance of continuous training of HCW.[3] In another study conducted in a referral hospital in Mali, Africa, HH compliance increased from a meager 8% to 21.8% (P < 0.0001) by promoting WHO's multimodal HH improvement strategy.[16] In a similar study conducted in an ICU in Brazil, 119 HH opportunities were observed wherein overall compliance was found to be 21% and 24.8% before and after the intervention, respectively.[17] In another study by Pittet et al., HH compliance increased from 48% to 66% over a 3-year period.[18]
In our study, HH compliance was found to be more among the nurses as compared to doctors, this was similar to the observation of Randle et al.[19] On the other hand, in a study conducted by Sharma et al. compliance was found to be higher amongst doctors.[4]
In our study, the HCW fared best for WHO moment 3 and 4 (68.2% and 65.5%), this might point towards the desire to safeguard oneself from HCAI. This finding is similar to another study conducted by Borges et al.[17] Furthermore, a study conducted in a surgical ICU, very high HH compliance of 93% and 91% were noted for moments 3 and 4 while the overall HH compliance was found to be 69%.[3]
Primary healthcare is the grass-root level of healthcare services in any community and the first level of contact between patient and healthcare providers.[20] In a commentary published by Tartari et al., the authors have emphasized the significance of healthcare institutes in implementation of WHO recommendations for improvement of primary healthcare especially in developing countries like India.[21] Healthcare-associated infections (HCAIs) are preventable, yet no country or healthcare facility has been able to achieve zero HCAI rate.[19] HCAIs are drawing increasing attention from patients and governments alike and unless effective measures are taken, we are heading towards a global crisis situation.[7] In a study conducted by Cummings in a tertiary medical center in Durham, North Carolina, HH noncompliance was found to be associated with significant attributable hospital costs. They found that the hospital spends $1,779,283 on annual methicillin-resistant Staphylococcus aureus infection-related expenses due to low HH compliance.[22]
India is a diverse nation where the quality of healthcare is governed majorly by whether the healthcare setup is government or privately funded. This is primarily due to lack of infrastructure and manpower compared to heavy patient load in a government setup. In addition, limitations like availability of clean running water, soap, HR, and a general attitude of noncompliance amongst healthcare providers towards even basic procedures of infection control present as a roadblock to HH. This finding has been reciprocated in a study conducted in south India by Tyagi et al. in newborn units and labor rooms of private and public healthcare setups. The authors observed that the compliance to HH is influenced by facility ownership with better results in private facilities.[4]
The present study was conducted while our hospital was preparing to undergo a NABH assessment. As a part of the preparation, HCWs underwent intensive training with the help of posters, performance feedback, and verbal reminders. The number of ICN doubled. Regular rounds to monitor the progress followed this. All these factors provided the thrust that improved the HH compliance noted in our setup.
This is our first step initiative towards improving HH and thus preventing HCAIs in our setup. Our study highlights the importance of targeted, multifaceted approach starting from administrative support, policy formulation, dedicated staff, and availability of consumables such as alcoholbased HRs in improving HH in a healthcare setup. However, we have not correlated the effect of improved HH on HCAIs. A further study correlating HCAI with HH compliance should be next in line. In addition, observation bias might have influenced the HCWs behavior in our setup. A covert HH observational study can be deliberated to identify the Hawthorne effect on HH compliance.
It is pertinent to point here that expert opinion from tertiary care centers limited data on the impact of HH is required to set up guidelines for its use in the ever-expanding scope of primary care practice. Moreover, as per WHO for the patient safety, the first level of contact of individuals, the family, and community with the national health system will help in integrating effective HH as the first element for a continuing healthcare process.
Conclusion
Unflinching support of hospital's administration, relentless efforts of infection control team and creative initiatives towards improving HH go a long way together in preventing healthcare-associated infections (HCAIs).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The research was conducted at the intensive care unit of Dr. Baba Saheb Ambedkar Hospital and Medical College. Our hospital administration, healthcare staff especially infection control nurses gave full support and contributed immensely to our study.
References
- 1.Peters A, Borzykowski T, Tartari E, Kilpatrick C, Mai SH, Allegranzi B, et al. Clean care for all-it's in your hands“: The May 5th, 2019 world health organization SAVE LIVES: Clean your hands campaign. Antimicrob Resist Infect Control. 2019;8:64. doi: 10.1186/s13756-019-0513-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO guidelines on hand hygiene in health care. Geneva: WHO; 2009. [Last accessed on 2019 Feb 19]. Available from: https://appswhoint/iris/bitstream/handle/10665/44102/9789241597906_engpdf; jsessionid=BAA3C200C392F76B2FFE0B93A3A4A077?sequence=1 . [Google Scholar]
- 3.Chavali S, Menon V, Shukla U. Hand hygiene compliance among healthcare workers in an accredited tertiary care hospital. Indian J Crit Care Med. 2014;18:689–93. doi: 10.4103/0972-5229.142179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma S, Sharma S, Puri S, Whig J. Hand hygiene compliance in the intensive care units of a tertiary care hospital. Indian J Community Med. 2011;36:217–21. doi: 10.4103/0970-0218.86524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tyagi M, Hanson C, Schellenberg J, Chamarty S, Singh S. Hand hygiene in hospitals: An observational study in hospitals from two southern states of India. BMC Public Health. 2018;18:1299. doi: 10.1186/s12889-018-6219-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah R, Patel DV, Shah K, Phatak A, Nimbalkar S. Video surveillance audit of hand-washing practices in a neonatal intensive care unit. Indian Pediatr. 2015;52:409–11. doi: 10.1007/s13312-015-0646-6. [DOI] [PubMed] [Google Scholar]
- 7.Sastri AS. Impact of a hand hygiene audit on hand hygiene compliance in a tertiary care public sector teaching hospital in South India. Am J Infect Control. 2017;45:498–501. doi: 10.1016/j.ajic.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Mathur P. Hand hygiene: Back to the basics of infection control. Indian J Med Res. 2011;134:611–20. doi: 10.4103/0971-5916.90985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National accreditation board for hospitals and healthcare providers. 2018. [Last accessed on 2019 Feb 19]. Available: from: https://wwwnabhco/introductionaspx .
- 10.Cummings KL, Anderson DJ, Kaye KS. Hand hygiene noncompliance and the cost of hospital-acquired methicillin-resistant staphylococcus aureus infection. Infect Control Hosp Epidemiol. 2010;31:357–64. doi: 10.1086/651096. [DOI] [PubMed] [Google Scholar]
- 11.Indian Council of Medical Research Department of Health Research Treatment Guidelines for Antimicrobial Use in Common Syndromes. 2017. [Last accessed on 2019 Feb 19]. Available from: https://wwwicmrnicin/sites/default/files/guidelines/treatment_guidelines_for_antimicrobialpdf .
- 12.Marra AR, Moura DF, Paes AT, Santos OF, Edmond MB. Measuring rates of hand hygiene adherence in the intensive care setting: A comparative study of direct observation, product usage, and electronic counting devices. Infect Control Hosp Epidemiol. 2010;31:796–801. doi: 10.1086/653999. [DOI] [PubMed] [Google Scholar]
- 13.Nair SS, Hanumantappa R, Hiremath SG, Siraj MA, Raghunath P. Knowledge, attitude, and practice of hand hygiene among medical and nursing students at a tertiary health care centre in Raichur, India. ISRN Prev Med. 2014;2014:608927. doi: 10.1155/2014/608927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu KS, Lee SSJ, Chen JK, Chen YS, Tsai HC, Chen YJ, et al. Identifying heterogeneity in the Hawthorne effect on hand hygiene observation: A cohort study of overtly and covertly observed results. BMC Infect Dis. 2018;18:369. doi: 10.1186/s12879-018-3292-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erasmus V. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;3:283–94. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 16.Allegranzi B. Successful implementation of the world health organization hand hygiene improvement strategy in a referral hospital in Mali, Africa. Infect Control Hosp Epidemiol. 2010;31:133–41. doi: 10.1086/649796. [DOI] [PubMed] [Google Scholar]
- 17.Borges LF, Rocha LA, Nunes MJ, Filho PP. Low compliance to handwashing program and high nosocomial infection in a Brazilian hospital. Interdiscip Perspect Infect Dis. 2012;2012:579681. doi: 10.1155/2012/579681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pittet D, Hugonnet S, Harbarth S. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet. 2000;356:1307–12. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 19.Randle J, Arthur A, Vaughan N. Twenty-four-hour observational study of hospital hand hygiene compliance. J Hosp Infect. 2010;76:252–5. doi: 10.1016/j.jhin.2010.06.027. [DOI] [PubMed] [Google Scholar]
- 20.Tartari E, Muthukumaran P, Peters A, Allegranzi B, Pittet D. Monitoring your institution: The WHO hand hygiene self-assessment frameworkdis it worth it? Clin Microbiol Infect. 2019;25:925–8. doi: 10.1016/j.cmi.2019.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Donaldson MS, Yordy KD, Lohr KN, editors. Primary Care: America's Health in a New Era. Washington (DC): National Academies Press (US); 1996. pp. 1–12. [PubMed] [Google Scholar]
- 22.Saito H, Allegranzi B, Pittet D. WHO hand hygiene campaign: Preventing sepsis in health care and the path to universal health coverage. Lancet Infect Dis. 2018;18:490–2. doi: 10.1016/S1473-3099(18)30228-7. [DOI] [PubMed] [Google Scholar]


