Abstract
Introduction:
Though the negative influence of tobacco consumption on the periodontal status of an individual is established, the magnitude of this association based on the type of tobacco used is seldom investigated.
Aim:
The aim of this study is to check the differences in the periodontal status of individuals based on their current tobacco consumption status and type of tobacco consumption.
Materials and Methods:
This study was conducted among subjects attending a teaching dental institution in Andhra Pradesh. Subjects were divided into three groups based on their current tobacco consumption status. The following parameters were recorded after examination by two calibrated investigators: number of sites with bleeding on probing; number of teeth with periodontal pockets; number of teeth with clinical attachment loss of ≥5 mm; number of teeth lost. SPSS version 20 software was used to analyze the data.
Results:
While current users demonstrated poor periodontal status than the former and nonusers, there was a significant difference in periodontal health between former users and nonusers in all the study parameters except the mean number of teeth lost. Among current users, the mean percentage of sites with bleeding and attachment loss >5 mm were found to be least among smokers compared to tobacco chewers and those who consume both smoke and smokeless forms of tobacco.
Conclusion:
The study confirms the negative influence of tobacco consumption on periodontal health and also establishes the increased destruction of clinical attachment levels among tobacco chewers compared to smokers.
Keywords: Periodontal attachment loss, smokeless tobacco, tobacco use
Introduction
Though the tobacco consumption habits among the Indian population have been reported to be decreasing, statistics relating to the prevalence of tobacco use confirm that more than one-quarter of the nation's populace still consume tobacco in one form or the other. Khaini and Beedi are among the most commonly used smokeless and smoke forms of tobacco used in India, respectively. Clear gender variations are seen in the adoption of this deleterious habit, with 42.4% of men and 14.2% of women reporting the use of tobacco. There are statewide variations in the prevalence of tobacco consumption with Andhra Pradesh (20%) demonstrating considerably lesser prevalence compared to the national average (28.6%).[1] It is an established fact that the incidence of tobacco use is higher among people belonging to lower socioeconomic strata and a cyclical relationship has been reported between tobacco consumption by poorer sections and further deterioration of their socioeconomic status owing to the negative health-related consequences of tobacco use which include coronary artery disease, emphysema, chronic bronchitis, peptic ulcer, lung, oral cavity, and gastrointestinal tract cancers.[2,3] Periodontal diseases refer to the disintegration of connective tissue that anchors the tooth and could result in tooth mortality. Poor periodontal health is one of the many adverse health consequences of tobacco use which did not receive enough emphasis, especially in light of the significant negative effect of periodontal diseases on the quality of life of the affected.[4] It is this increased incidence of periodontal diseases among tobacco users that offers an opportunity for the oral health care professionals to inquire about the tobacco consumption habits of their patients, discuss with them the deleterious effects of tobacco, and motivate them towards quitting the habit.[5]
Despite the high self-reported rate of attempting to quit the habit, the majority of people, who attempt quitting, resume using tobacco due to a variety of reasons.[6] The poor supporting environment is one of the major reasons which preclude an individual from quitting the habit of tobacco use. Previous studies highlighted the socioeconomic inequalities in the success of quit attempts, with people belonging to poorer socioeconomic strata being less successful.[7] Considering the fact that oral health care services at dental institutions are more commonly utilized by economically disadvantaged sections and the inextricable association between tobacco use and negative oral health outcomes. Ministry of Health and Family Welfare, Government of India in collaboration with various stakeholders including Dental Council of India published a book “Establishment of Tobacco Cessation Centers in Dental Institutes—An Integrated Approach in India—Operational Guidelines 2018.“[8] All the dental institutions in the country have been directed to establish tobacco cessation clinics following the aforementioned directives, and it was noted by the council that 12 dental institutions have not established tobacco cessation centers as directed, as on 27th of September, 2019.[9] In this context, it becomes important to just not to assess the association between tobacco use and periodontal disease but to establish the magnitude of influence of tobacco on periodontal status of an individual based on the type of use to better get informed and motivate the subjects with tobacco consumption habit towards quitting.
Materials and Methods
This cross-sectional study was conducted among subjects attending the outpatient department of a teaching dental institution in coastal Andhra Pradesh. The teaching dental institution serves a huge demographic and people from different socioeconomic strata. The study protocol was approved by the institutional ethical committee (2_IEC-KIMS-19) and informed consent was obtained from all the study participants before the clinical examination. The sample size was determined to be 98 in each group using G*power 3.1.9.2 software and 100 subjects were included in each of the three study groups. The three study groups are as follows: current tobacco users who reported use of 100 cigarettes or other smoking forms of tobacco in their lifetime and are currently smoking every day or some days and/or chewing tobacco products at least 20 times in their life and are currently chewing tobacco products every day or some days; former tobacco users who reported use of 100 cigarettes or other smoking forms of tobacco in their lifetime and had quit smoking at the time of the study and/or chewing tobacco products at least 20 times in their life and had quit chewing tobacco products at the time of the study; and nonusers who had never smoked or chewed tobacco products in their life or who reported use of less than 100 cigarettes or other smoking forms of tobacco and less than 20 times use of chewing tobacco products.[10,11] The intention of the investigators was to recruit current users first and then identify the age and gender-matched subjects in the former user and nonuser groups. However, since none of the subjects in the current user group were females, there was no question of gender matching and subjects were only matched on their age. The study was conducted from February 2019 to July 2019. All the subjects underwent an interview seeking information about oral hygiene practices, systemic health, followed by a clinical examination to record the following parameters: number of sites with bleeding on probing; number of teeth with periodontal pockets; number of teeth with clinical attachment loss of ≥5 mm; number of teeth lost. Two investigators participated in the data collection process. The intraclass correlation coefficient values for the two examiners ranged from 0.89 to 0.94 for various parameters demonstrating a good interexaminer reliability. The data were analyzed using Statistical Package for Social Sciences (SPSS) version 20 software (IBM SPSS Statistics for Windows version 20, Armonk, NY, USA). One way analysis of variance with Tukey's post-hoc tests and Chi-square test were used to analyze the data.
Results
The mean age of the study participants was 52.13 years with a standard deviation of 10.82. Current users were observed to be older compared to former users and nonusers. There was a significant difference in the recorded clinical parameters between the three study groups [Table 1]. While current users demonstrated poor periodontal status than the former and nonusers, there was a significant difference in periodontal health between former users and nonusers in all the study parameters except the mean number of teeth lost. Gingival recession was documented to be more common among current users. Pairwise comparisons revealed significant differences among all possible pairs in the clinical parameters considered with current users having poor periodontal status than former users and nonusers [Table 2]. The only exception was the lack of difference in the mean number of teeth lost between former users and nonusers. When the current users were stratified based on the type of tobacco use, a significant difference was observed between these groups with regard to the mean percentage of sites with a bleeding, mean number of teeth with periodontal pockets, and the mean number of teeth with attachment loss greater than 5 mm. There was no significant difference in the number of teeth lost based on the type of tobacco use [Table 3]. Multiple pairwise comparisons revealed that tobacco chewers had a higher mean percentage of bleeding sites compared to smokers and those who reported using both smoking and smokeless tobacco forms. Participants who reported the use of both smoking and smokeless forms of tobacco were observed to be having more attachment loss compared to exclusive chewers and smokers [Table 4]. Graphical representation of the differences in clinical parameters between current and former tobacco users, non users was provided in Figure 1. Figure 2 shows the differences in clinical parameters among current tobacco users based on the type of tobacco use.
Table 1.
Comparison of clinical parameters between the three study groups
| Parameter | Group | n | Mean±SD | Between group sum of squares | Mean square | F | P |
|---|---|---|---|---|---|---|---|
| % of bleeding sites | Current user | 100 | 25.1±5.34 | 4337.247 | 2168.62 | 72.685 | 0.001* |
| Former user | 100 | 21.03±6.46 | |||||
| Nonuser | 100 | 15.8±4.38 | |||||
| Mean number of sites with periodontal pockets | Current user | 100 | 5.37±3.16 | 534.32 | 267.16 | 35.55 | 0.001* |
| Former user | 100 | 3.95±2.98 | |||||
| Nonuser | 100 | 2.11±1.89 | |||||
| Number of sites with attachment loss ≥5 mm | Current user | 100 | 7.32±3.43 | 1187.94 | 593.97 | 84.94 | 0.001* |
| Former user | 100 | 4.4±2.49 | |||||
| Nonuser | 100 | 2.48±1.72 | |||||
| Number of teeth lost | Current user | 100 | 4.8±2.57 | 331.74 | 165.87 | 36.53 | 0.001* |
| Former user | 100 | 2.79±2.02 | |||||
| Nonuser | 100 | 2.4±1.7 |
One way ANOVA; P≤0.05 considered statistically significant; *denotes statistical significance
Table 2.
Multiple pairwise comparisons of the clinical parameters between the study groups
| Parameter | Reference Group | Comparison Group | Mean difference | P |
|---|---|---|---|---|
| % of bleeding sites | Current user | Former user | 4.07 | 0.001* |
| Nonuser | 9.29 | 0.001* | ||
| Former user | Nonuser | 5.22 | 0.001* | |
| Mean number of sites with periodontal pockets | Current user | Former user | 1.42 | 0.001* |
| Nonuser | 3.26 | 0.001* | ||
| Former user | Nonuser | 1.84 | 0.001* | |
| Number of sites with attachment loss ≥5 mm | Current user | Former user | 2.92 | 0.001* |
| Nonuser | 4.84 | 0.001* | ||
| Former user | Nonuser | 1.92 | 0.001* | |
| Number of teeth lost | Current user | Former user | 2.01 | 0.001* |
| Nonuser | 2.4 | 0.001* | ||
| Former user | Nonuser | 0.39 | 0.4 |
Tukey’s post hoc tests; P≤0.01 considered statistically significant; *denotes statistical significance
Table 3.
Comparison of clinical parameters among current users based on the type of use
| Parameter | Group | n | Mean±SD | Between group sum of squares | Mean square | F | P |
|---|---|---|---|---|---|---|---|
| % of bleeding sites | Chewer | 51 | 28.1±4.006 | 1227.18 | 613.59 | 37.96 | 0.001* |
| Smoker | 18 | 18.78±2.88 | |||||
| Both | 31 | 23.83±4.56 | |||||
| Mean number of sites with periodontal pockets | Chewer | 51 | 6.33±3.36 | 99.13 | 49.56 | 5.37 | 0.06* |
| Smoker | 18 | 4.19±2.84 | |||||
| Both | 31 | 4.67±2.52 | |||||
| Number of sites with attachment loss ≥5 mm | Chewer | 51 | 7.29±3.6 | 29.04 | 14.52 | 1.23 | 0.04* |
| Smoker | 18 | 6.27±3.49 | |||||
| Both | 31 | 7.74±3.29 | |||||
| Number of teeth lost | Chewer | 51 | 4.88±2.71 | 11.05 | 5.52 | 0.82 | 0.4 |
| Smoker | 18 | 4.11±1.99 | |||||
| Both | 31 | 5.06±2.64 |
One way ANOVA; P≤0.05 considered statistically significant; *denotes statistical significance
Table 4.
Multiple pairwise comparisons of the clinical parameters among current users based on the type of use
| Parameter | Reference group | Comparison group | Mean difference | P |
|---|---|---|---|---|
| % of bleeding sites | Chewer | Smoker | 9.32 | 0.001* |
| Both | 4.25 | 0.001* | ||
| Smoker | Both | −5.06 | 0.001* | |
| Mean number of sites with periodontal pockets | Chewer | Smoker | 1.67 | 0.038* |
| Both | 2.14 | 0.071 | ||
| Smoker | Both | 0.47 | 0.85 | |
| Number of sites with attachment loss ≥5 mm | Chewer | Smoker | 1.02 | 0.046* |
| Both | −0.45 | 0.83 | ||
| smoker | Both | −1.47 | 0.04* |
Tukey’s post-hoc tests; P≤0.01 considered statistically significant; *denotes statistical significance
Figure 1.
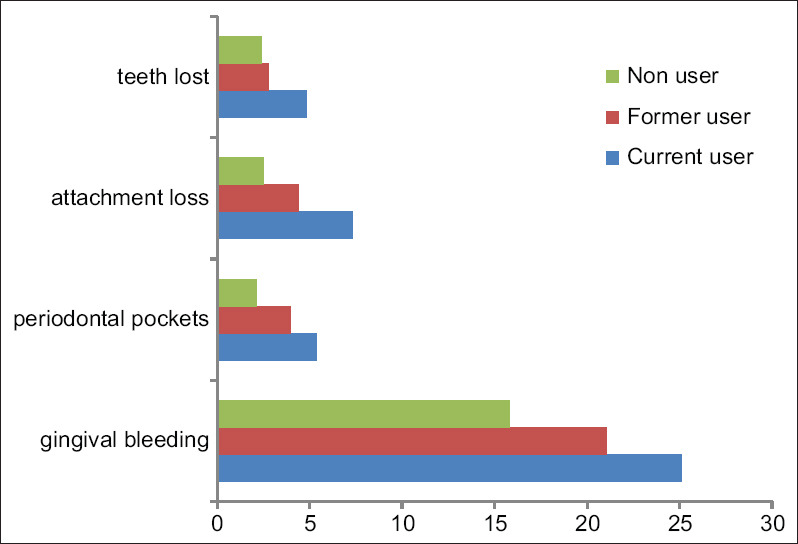
Bar chart showing the differences in clinical parameters between the study groups
Figure 2.
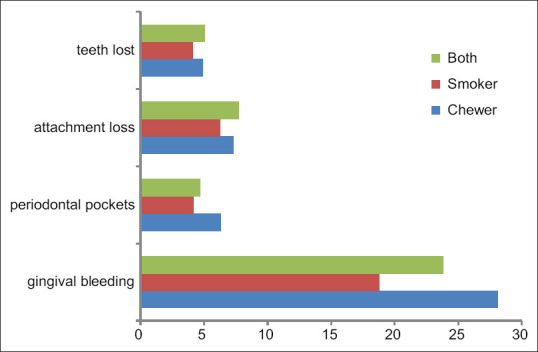
Bar chart showing differences in clinical parameters based on the nature of tobacco use
Discussion
In light of the established association between periodontal status and the systemic health of an individual, it is understood that tobacco consumption deteriorates systemic health both directly and in an indirect manner, with poor periodontal status assuming a mediating role. Primary care physicians and oral health care professionals play a key role in advising and supporting the subjects in the process of quitting tobacco. Also, oral health is increasingly being emphasized as an essential component of primary care.[12] Often oral health care facilities serve as the primary contact points for people in the diagnosis of chronic conditions and in engaging the subjects to seek requisite medical care.[13] Literature suggests that dentists administering an efficient tobacco cessation program could achieve a 10–15% quit rate in a year.[14] In this context, oral health care professionals are expected to play a key role in improving the health status of the communities they are serving in, by proactively involving in tobacco cessation counseling.[15]
It is unfortunate that the habit of tobacco consumption is on the rise in developing nations.[16] The acquisition of tobacco chewing habits in different forms is more alarming. In the present study, it was found that 82% of the current tobacco users have tobacco chewing habits, while 49% reported using smoking forms of tobacco. These numbers are in accordance with the Global Adult Tobacco Survey 2016–17 data.[1] The reasons for increasing the use of smokeless forms of tobacco are the relatively cheaper cost of these products and less revealing the nature of their use compared to smoking.[16] The study results reinforce the negative influence of tobacco use on periodontal status. Though there are numerous studies evaluating the impact of tobacco use on the periodontal health of an individual, this is one of the first studies which attempted to comprehensively document periodontal status by considering different clinical parameters. It was identified in the present study that current users have a significantly higher percentage of sites with bleeding compared to former users and nonusers. Among current users, exclusive smokers had the least incidence of gingival bleeding. These results are in compliance with those reported by Gautam et al.[17] and Feldman et al.[18] The possible reason for this finding is the inhibitory effect of nicotine, one of the many harmful by-products of tobacco smoke, on the manifestation of the early signs of periodontal disease, because of its local vasoconstrictive action.
The observation made in the present study that current users have a significantly higher number of teeth with periodontal pockets is inconsistent with the studies done by Gautam et al.[17] Akaji et al., and[19] Katuri et al.[20] Among current users, chewers demonstrated a significantly higher number of teeth with periodontal pockets which are in accordance with the studies conducted by Robertson et al.[21] and Chu et al.[22] It was observed in this study that the number of teeth with attachment loss greater than 5 mm was more in those participants who reported the use of both forms of tobacco compared to exclusive smokers and chewers. This is in accordance with the studies reported by Katuri et al.,[20] Monten et al.,[23] Amarasena et al.,[24] and Mittal et al.[25] Verma et al.[26] reported greater attachment loss among tobacco chewers in a study conducted among gutkha chewers in the Delhi NCR region. The rational explanations for the more severe destruction of periodontal attachment apparatus among subjects consuming smokeless tobacco forms are manifold. Few justifications in this direction could be comparatively high blood nicotine levels among chewers than smokers, mechanical injury and irritation caused by holding smokeless forms of tobacco in close proximity to the gingival tissue, and higher incidence of gingival hyperemia among chewers caused by the aggravation of inflammatory reactions by smokeless tobacco.[26] The results from this study inform the oral health care professionals about the form-dependent association between tobacco and periodontal health and help them better play their roles in the arena of primary health care. There is a necessity for these care providers to undergo training on tobacco cessation counseling, since the majority of tobacco users already know the negative influence of tobacco on oral and general health, and it is not only the knowledge that needs to be shared but also the attitude that needs to be changed.[27,28]
Conclusion
The study confirms the negative influence of tobacco consumption on periodontal health and also establishes the increased destruction of clinical attachment levels among tobacco chewers compared to smokers. In light of the proven negative association between periodontal disease and systemic health of an individual, these findings give a heads up for the dental fraternity to get more actively involved in tobacco cessation counseling and directly participate in health promotion, in general, and oral health promotion in particular.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.GATS. Global Adult Tobacco Survey: Fact sheet, India 2016-17. 2017. [Last accessed on 2019 Nov 08]. Available from: http://wwwwhoint/tobacco/surveillance/survey/gats/GATS_India_2016-17_FactSheetpdf .
- 2.US NCI and WHO. The economics of tobacco and tobacco control National Cancer Institute (Tobacco Control Monograph 21, NIH Publication No 16-CA-8029) Bethesda, MD: 2016. [Last accessed on 2019 Aug 22]. Available from: http://cancercontrolcancergov/brp/tcrb/monographs/21/indexhtml . [Google Scholar]
- 3.Committee on the Public Health Implications of Raising the Minimum Age for Purchasing Tobacco Products; Board on Population Health and Public Health Practice; Institute of MedicineBonnie RJ, Stratton K, Kwan LY, editors. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products. Washington (DC): National Academies Press (US); 2015. Jul 23, p. 4. The Effects of Tobacco Use on Health. [PubMed] [Google Scholar]
- 4.Leite FR, Nascimento GG, Scheutz F, López R. Effect of smoking on periodontitis: A systematic review and meta-regression. Am J Prev Med. 2018;54:831–41. doi: 10.1016/j.amepre.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 5.Johnson NW. The role of the dental team in tobacco cessation. Eur J Dent Educ. 2004;8:18–24. doi: 10.1111/j.1399-5863.2004.00318.x. [DOI] [PubMed] [Google Scholar]
- 6.Chaiton M, Diemert L, Cohen JE, Bondy SJ, Selby P, Philipneri A, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open. 2016;6:e011045. doi: 10.1136/bmjopen-2016-011045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Atlanta (GA): The health consequences of smoking - 50 years of progress: A report of the surgeon general; 2014. [PubMed] [Google Scholar]
- 8.Gadpyale AK, Usta MS, Kharbanda OP, Jhanjhee S, Murthy P, Munish VG, et al. operational guidelines. Ministry of Health and Family Welfare, Government of India; 2018. [Last accessed on 2019 Nov 08]. (2018) Establishment of tobacco cessation centers in dental institutes an integrated approach in India. Available from: http://wwwdciindiagovin/Rule_Regulation/FinaloperationalguidelinesTCCindentalcollegespdf . [Google Scholar]
- 9.Dental Council of India. List of dental colleges those have not established tobacco cessation centres (as on 2792019) [Last accessed on 2019 Nov 11]. Available from: http://wwwdciindiagovin/Rule_Regulation/List%20of%20TCC%20in%20Dental%20Colleges11pdf .
- 10.Ryan H, Trosclair A, Gfroerer J. Adult current smoking: Differences in definitions and prevalence estimates—NHIS and NSDUH, 2008. J Environ Public Health. 2012;2012:918368. doi: 10.1155/2012/918368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agaku IT, Awopegba AJ, Filippidis FT. The impact of inter-survey differences in the definition of current smokeless tobacco use on comparability of US national and state-specific prevalence estimates, 2009-2011. Prev Med. 2015;74:86–92. doi: 10.1016/j.ypmed.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 12.Hummel J, Phillips KE, Holt B, Hayes C. Oral health: An essential component of primary care. Seattle, WA: Qualis Health; 2015. Jun, [Google Scholar]
- 13.Gambhir RS. Primary care in dentistry - An untapped potential. J Family Med Prim Care. 2015;4:13–8. doi: 10.4103/2249-4863.152239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warnakulasuriya S. Effectiveness of tobacco counseling in the dental office. J Dent Educ. 2002;66:1079–87. [PubMed] [Google Scholar]
- 15.Zhang Y, He J, He B, Huang R, Li M. Effect of tobacco on periodontal disease and oral cancer. Tob Induc Dis. 2019;17:40. doi: 10.18332/tid/106187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mukherjee K, Hadaye RS. Gutkha its determinants among secondary school male students. Indian J Community Med. 2006;31:177. [Google Scholar]
- 17.Gautam DK, Jindal V, Gupta SC, Tuli A, Kotwal B, Thakur R. Effect of cigarette smoking on the periodontal health status: A comparative, cross sectional study. J Indian Soc Periodontol. 2011;15:383–7. doi: 10.4103/0972-124X.92575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feldman RS, Bravacos JS, Rose CL. Association between smoking different tobacco products and periodontal disease indexes. J Periodontol. 1983;54:481–7. doi: 10.1902/jop.1983.54.8.481. [DOI] [PubMed] [Google Scholar]
- 19.Akaji EA, Folaranmi N. Tobacco use and oral health of inmates in a Nigerian prison. Niger J Clin Pract. 2013;16:473–7. doi: 10.4103/1119-3077.116892. [DOI] [PubMed] [Google Scholar]
- 20.Katuri KK, Alluri JK, Chintagunta C, Tadiboina N, Borugadda R, Loya M, et al. Assessment of periodontal health status in smokers and smokeless tobacco users: A cross-sectional study. J Clin Diagn Res. 2016;10:ZC143–6. doi: 10.7860/JCDR/2016/22160.8700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robertson PB, Walsh M, Greene J, Ernster V, Grady D, Hauck W. Periodontal effects associated with the use of smokeless tobacco. J Periodontol. 1990;61:438–3. doi: 10.1902/jop.1990.61.7.438. [DOI] [PubMed] [Google Scholar]
- 22.Chu YH, Tatakis DN, Wee AG. Smokeless tobacco use and periodontal health in a rural male population. J Periodontol. 2010;81:848–54. doi: 10.1902/jop.2010.090310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montén U, Wennström JL, Ramberg P. Periodontal conditions in male adolescents using smokeless tobacco (moist snuff) J Clin Periodontol. 2006;33:863–8. doi: 10.1111/j.1600-051X.2006.01005.x. [DOI] [PubMed] [Google Scholar]
- 24.Amarasena N, Ekanayaka AN, Herath L, Miyazaki H. Tobacco use and oral hygiene as risk indicators for periodontitis. Community Dent Oral Epidemiol. 2002;30:115–23. doi: 10.1034/j.1600-0528.2002.300205.x. [DOI] [PubMed] [Google Scholar]
- 25.Mittal S, Dani N, Abullais S, Al-Qahtani N, Shah K. Effect of smoking and tobacco chewing on periodontal disease and non-surgical treatment outcome: A clinical and biochemical study. J Int Acad Periodontol. 2018;20:12–8. [PubMed] [Google Scholar]
- 26.Verma SK, Kumar BD, Singh S, Kumari P, Agarwal A, Singh TK, et al. Effect of gutkha chewing on periodontal health and oral hygiene of peoples in Delhi NCR region of North India: A cross-sectional multicentered study. J Family Med Prim Care. 2019;8:564–7. doi: 10.4103/jfmpc.jfmpc_439_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muniandy S. Knowledge on smoking and periodontal disease: A cross-sectional survey among targeted respondents. J Indian Soc Periodontol. 2019;23:275–80. doi: 10.4103/jisp.jisp_479_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu DC, Ho TC, Duangthip D, Gao SS, Lo EC, Chu CH. Dental students' awareness, preparedness and barriers towards managing tobacco-using patients-A cross-sectional study. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16101862. pii: E1862 doi: 103390/ijerph 16101862. [DOI] [PMC free article] [PubMed] [Google Scholar]


