Abstract
Objective
We compared the effects of high-intensity interval training (HIIT) and moderate-intensity continuous training (MICT) on insulin sensitivity and other important metabolic adaptations in adults with obesity.
Methods
Thirty-one inactive adults with obesity (age: 31 ± 6 years; body mass index: 33 ± 3 kg/m2) completed 12 weeks (4 sessions/week) of either HIIT (10 × 1-minute at 90%HRmax, 1-minute active recovery; n = 16) or MICT (45 minutes at 70%HRmax; n = 15). To assess the direct effects of exercise independent of weight/fat loss, participants were required to maintain body mass.
Results
Training increased peak oxygen uptake by ~10% in both HIIT and MICT (P < 0.0001), and body weight/fat mass were unchanged. Peripheral insulin sensitivity (hyperinsulinemic-euglycemic clamp) was ~20% greater the day after the final exercise session compared to pretraining (P < 0.01), with no difference between HIIT and MICT. When trained participants abstained from exercise for 4 days, insulin sensitivity returned to pretraining levels in both groups. HIIT and MICT also induced similar increases in abundance of many skeletal muscle proteins involved in mitochondrial respiration and lipid and carbohydrate metabolism. Training-induced alterations in muscle lipid profile were also similar between groups.
Conclusion
Despite large differences in training intensity and exercise time, 12 weeks of HIIT and MICT induce similar acute improvements in peripheral insulin sensitivity the day after exercise, and similar longer term metabolic adaptations in skeletal muscle in adults with obesity. These findings support the notion that the insulin-sensitizing effects of both HIIT and MICT are mediated by factors stemming from the most recent exercise session(s) rather than adaptations that accrue with training.
Keywords: Insulin resistance, exercise training, high-intensity interval training, skeletal muscle
Exercise is regularly prescribed for the prevention and treatment of several obesity-related metabolic disorders, including insulin resistance, which precedes and contributes to the development of many chronic diseases (e.g., type 2 diabetes, cardiovascular disease). Although the health benefits of moderate-intensity continuous training (MICT) in adults with obesity are well-recognized (1-4), to optimize the development of exercise programs targeting enhanced metabolic health in obesity, it is important to expand our understanding about how exercise leads to these improvements, with particular emphasis on the effects of exercise on insulin sensitivity. Importantly, the direct effects of exercise training on insulin sensitivity are confounded when an exercise training program is accompanied by weight loss, because even modest amounts of weight loss can have profound beneficial effects on insulin sensitivity (5). Moreover, each session of exercise is known to improve insulin sensitivity into the next day (6-8), but the insulin-sensitizing effects of several weeks, months, or even years of “conventional” MICT are often lost even after just a few days without exercise (6, 9, 10). These data support the notion that the effect of MICT on insulin action appears to be primarily from the acute effects of the most recent exercise session, rather than to the longer lasting exercise-induced adaptations (e.g., increased mitochondrial density and metabolic enzymes in skeletal muscle).
There is a growing interest and appreciation for the potential of high-intensity interval training (HIIT) to improve metabolic health in adults with obesity (11, 12). Little and colleagues (13) reported that a low-volume HIIT protocol involving 10 × 1-minute intervals at ~90% maximal heart rate (HRmax), with 1-minute active recovery in between intervals (total exercise time of ~25 minutes) attenuated hyperglycemia in patients with obesity and type 2 diabetes after performing only 6 sessions over 2 weeks. HIIT has also been found to induce relatively rapid improvements in whole-body aerobic capacity (14, 15), muscle mitochondrial markers (14, 15), and GLUT4 protein abundance (14) in adults with overweight/obesity. An important added benefit of HIIT is that low-volume HIIT protocols can require a shorter time commitment compared with MICT (16), and time constraints have been identified as a commonly reported barrier to regular exercise participation (17). However, findings regarding the effects of HIIT on indices of insulin resistance are equivocal (14, 18, 19). Discrepancies among studies may be related to the timing of measurement relative to the last training session, differences in the duration of training, and the method of measuring insulin sensitivity. To our knowledge, no studies have conducted a comprehensive comparison of the effects of HIIT versus MICT on insulin sensitivity using the hyperinsulinemic-euglycemic clamp technique, together with other important clinical and sub-clinical markers of metabolic health (e.g., hepatic lipid accumulation, visceral adiposity, lipolytic rate, muscle lipid profile) in adults with obesity.
The primary aim of this study was to compare the effects of 12 weeks of low-volume HIIT versus MICT on insulin sensitivity in adults with obesity. We also sought to examine the effects of training on several physiological outcomes that may influence insulin sensitivity including whole-body lipolytic rate, hepatic and visceral fat content, skeletal muscle lipidomic alterations, and muscle metabolic adaptations. We hypothesized that despite the lower training volume with HIIT versus MICT, the exposure to high-intensity exercise stimulus with HIIT would impart more robust adaptive responses in skeletal muscle and liver, leading to a more persistent improvement in insulin sensitivity than observed with MICT. Importantly, participants were required to maintain weight throughout training, enabling us to determine the effects of exercise independent from weight loss.
Methods
Subjects
Thirty-one adults with obesity (body mass index [BMI]: 30-40 kg/m2) adults completed the study. All participants were sedentary (not participating in any regular aerobic or resistance exercise), nonsmokers, weight-stable (within ± 2 kg for at least 6 months), not taking any medications or supplements known to influence their metabolism, and did not have any history of cardiovascular or metabolic disease. Women were premenopausal and not pregnant or lactating; some women were taking contraceptive medication. Participants first completed a detailed medical history survey and resting electrocardiogram, which were reviewed by a physician prior to any testing. The study was approved by the University of Michigan institutional review board and registered at clinicaltrials.gov (NCT02706093). All participants provided informed, written consent before participation.
Study design
The overall study design included 3 phases: (1) pretesting, including 1 “metabolic study” (i.e., hyperinsulinemic-euglycemic clamp, [d5]glycerol tracer to measure whole-body lipolysis, muscle biopsies), (2) a 12-week exercise training intervention (HIIT vs. MICT), and (3) posttesting, which included 2 metabolic studies, 1 conducted the day after the last exercise session (“trained 1d postEx”) and the other conducted after participants abstained from exercise for 4 days (“trained 4d postEx”) to remove the confounding influence of the acute effects of exercise. An overview of the study design is shown in Fig. 1.
Figure 1.
Overview of study design. All participants completed their final exercise session at 1800 hours the night preceding the 1d postEx metabolic study.
Body composition and hepatic and visceral adiposity measurements
Body composition was assessed using dual-energy x-ray absorptiometry (Lunar DPX DEXA scanner, GE, WI). Hepatic and visceral lipid accumulation were assessed using magnetic resonance imaging (Ingenia 3T MR System, Phillips, the Netherlands). These measurements were conducted before and after subjects completed the 12-week exercise training intervention.
Aerobic fitness testing
Graded exercise testing was performed on a stationary cycle ergometer (Corvival, Lode, the Netherlands) using an incremental exercise protocol starting at 40W and increasing 20W per minute until volitional exhaustion. The rate of oxygen consumption was measured throughout this test using a metabolic cart (Max-II, Physiodyne Inc, NY) and peak oxygen uptake (VO2peak) was determined as the highest 30-second average before volitional fatigue. Measurements of respiratory exchange ratio ≥ 1.1 and HRmax ≥ 90% of age predicted values (220 – age) were used as secondary indices to help confirm maximal effort during these tests. VO2peak was measured before and after 12 weeks of training.
Training interventions
Group assignment to either MICT (n = 15) or HIIT (n = 16) was conducted in a counterbalanced manner in attempt to optimize matching of sex and baseline body weight, BMI, and VO2peak among participants in each group. The training interventions were both 12 weeks long, and exercise was performed using stationary cycling, treadmill, elliptical, or rowing ergometers. The number of participants choosing cycling (MICT, n = 6; HIIT, n = 5), treadmill/elliptical (MICT, n = 9; HIIT, n = 10), and rowing (MICT, n = 0; HIIT, n = 1) as the primary exercise modality was similar between groups. The time subjects exercised each day was not controlled. Participants assigned to MICT completed 4 sessions per week of 45 minutes of continuous aerobic exercise at 70% of their HRmax. Participants assigned to HIIT completed 4 sessions per week involving a 3-minute warm-up at ~65% HRmax, 10 × 1-minute intervals at 90% HRmax with 1-minute low-intensity active recovery between intervals, and a 3-minute cool-down at ~65% HRmax after completing all intervals. This low-volume HIIT protocol has been used previously (13-14, (20-21). Because the objective of this study was to compare the metabolic effects of a low-volume HIIT protocol to a more “conventional” and commonly prescribed steady-state exercise training program (1, 12), exercise time and energy expenditure were intentionally not matched between groups. Each session of HIIT was considerably shorter than MICT (25 vs. 45 minutes) and estimated energy expenditure was also much lower during each session of HIIT vs. MICT (~150 vs. ~250 kcals).
Training familiarization/ramp-up.
During the first 2 weeks of training, participants in both groups followed a regimented ramp-up training protocol to progressively increase their exercise intensity and duration. During the first week, subjects in both groups completed 4 sessions of exercise involving 25 minutes at 65% HRmax. During the second week, MICT performed 4 × 35-minute sessions of exercise at 70% HRmax, whereas HIIT performed 2 × 1 minute high-intensity intervals the first session, 4 × 1-minute high-intensity intervals the second session, 6 × 1-minute high-intensity intervals the third session, and 8 × 1-minute high-intensity intervals the fourth session. All participants began their final training prescription at the beginning of week 3.
Monitoring of training adherence and weight maintenance.
Study staff supervised all exercise training sessions during the first 3 weeks of training. For the remainder of the 12-week training program, subjects were required to complete 2 supervised and 2 unsupervised training sessions each week. Downloadable telemetry heart rate devices (Polar, Finland) were provided to all participants and were required to be worn during all exercise training sessions. Heart rate data during all sessions were reviewed by study staff to ensure completion of all sessions at the assigned intensity and duration. To assess the direct effects of exercise training (independently of changes in body weight), subjects were required to maintain stable body weight throughout training. This was successfully achieved by requiring participants to be weighed several times each week. If body mass began to deviate by 1% to 2% from baseline, participants consulted with our research study dietitian for nutritional guidance for weight maintenance.
Standardized diets before the overnight metabolic studies
During the evening before each metabolic study (1 before training and 2 after training; Fig. 1 and “Study design” section), participants were provided and ate a standardized dinner (30% of estimated total daily energy expenditure) at 1900 hours and a standardized snack (10% of estimated total daily energy expenditure) at 2200 hours. The macronutrient composition of the meal and snacks was 55% carbohydrate, 30% fat, and 15% protein. Participants ate the exact same meals for all 3 of their metabolic studies. None of the participants were following a habitual diet with a macronutrient composition that deviated greatly from the meals and snacks provided (e.g., ketogenic diet). For the trained 1d postEx visit, participants completed their usual exercise session at 1800 hours (before dinner). During this visit, participants also ingested a nutritional supplement drink with their dinner (Boost Plus, Nestle, Switzerland; 50% carbohydrate, 35% fat, and 15% protein). The caloric content of this supplement was individually determined to replace the calories expended during their exercise session. This enabled us to determine the metabolic effects of exercise without the influence of an exercise-induced energy deficit.
Metabolic studies
For each metabolic study visit, participants arrived at the Michigan Clinical Research Unit at 1730 hours the evening before metabolic testing. They were provided a standardized meal and snack at 1900 hours and 2200 hours, respectively, after which they fasted until completion of all measurements the next morning. Participants slept in their hospital room overnight.
At 0630 hours the next morning, we measured resting energy expenditure and fat oxidation using indirect calorimetry (Vmax Encore, SensorMedics, CA). At ~0700 hours, IV catheters were inserted into a hand/forearm vein on each arm. A baseline blood sample was collected and then at ~0800 hours, we began primed continuous infusions of [6-6 d2]glucose (35 μmol/kg priming dose; 0.41 μmol/kg/min continuous infusion) and [d5]glycerol (1.5 μmol/kg priming dose; 0.1 μmol/kg/min continuous infusion). At ~0815 hours, a skeletal muscle biopsy (~120 mg) was obtained from the vastus lateralis and quickly dissected free of any adipose or connective tissue, rinsed with saline, blotted dry, and flash frozen in liquid nitrogen. Beginning at ~0950 hours, we collected 3 arterialized (heated hand technique) blood samples separated by 5 minutes each; these plasma samples were used for the determination of overnight fasted glucose and glycerol kinetics. At ~1000 hours, we began a 2-hour hyperinsulinemic-euglycemic clamp to determine insulin sensitivity (22). Briefly, a primed, continuous infusion of insulin (40 mU/m2/min) was administered; blood glucose was assessed every 5 minutes and 20% dextrose (enriched with [6-6 d2]glucose) was infused at a variable rate to accommodate changes in blood glucose to maintain blood glucose at the participants’ overnight fasted levels. After blood glucose concentration stabilized without further changes in the rate of 20% dextrose infusion for ≥ ~20 minutes, arterialized blood samples were collected every 5 minutes during the final 20 minutes of the clamp for the determination of steady-state plasma glucose and glycerol kinetics and serum insulin concentration.
Analytical procedures
Circulating concentrations of substrates and inflammatory biomarkers.
Plasma concentrations of glucose (TR-15221, ThermoFisher, MO), cholesterol (#999-02601, Wako Chemicals, VA), triglycerides (T2449, Sigma, MO), CRP (CR120C, Cal Biotech, CA), and IL-6 (HS600C, R&D Systems, MN) were assessed using commercially available kits. Serum insulin concentration was assessed using a chemiluminescent immunoassay (Siemens 1000). HbA1C was assessed by the University of Michigan Pathology Laboratory using HPLC.
Plasma glucose and glycerol kinetics.
Gas chromatography-mass spectroscopy (MS; Agilent 5973 Networks, Mass Selective Detector, Agilent, DE) was used to determine the tracer-to-tracee ratio for plasma glucose and glycerol, as we have reported previously (8).
Protein abundance of some key factors regulating muscle metabolism.
A portion of each muscle biopsy sample (25 ± 4 mg wet weight) was homogenized in ice-cold 1X RIPA buffer (#9806, Cell Signaling Technology, MA) with freshly added protease and phosphatase inhibitors (P8340, P5726, and P0044; Sigma) using 2 5-mm steel beads (TissueLyser II, Qiagen, CA). Homogenates were solubilized by rotating at 50 rpm for 60 minutes at 4°C and then centrifuged at 4°C for 15 minutes at 15 000g. The supernatant was collected and protein concentration was assessed using the bicinchoninic acid method (#23225, ThermoFisher). Samples for Western blotting were prepared in 4X Laemmli buffer, heated for 5 minutes at 95°C, and equal amounts of protein (15 μg) were loaded onto handcast gels ranging from 8% to 15%. After separation by SDS-PAGE, proteins were transferred onto nitrocellulose membranes. Membranes were blocked for 2 hours at room temperature, incubated with primary antibodies overnight at 4°C, washed, and then incubated with appropriate secondary antibody (#7074 or #7076, Cell Signaling Technology). All blots were developed using enhanced chemiluminescence (#1705061, BioRad or #34095, Fisher) and imaged (FluorChem E Imager, ProteinSimple, CA). Primary antibodies were Total OXPHOS cocktail (ab110411, Abcam, MA), Cytochrome c oxidase subunit IV (COX-IV, #4844, Cell Signaling Technology), carnitine O-palmitoyltransferase 1 (CPT1B, ab134988, Abcam), adipose triglyceride lipase (ATGL, #2138, Cell Signaling Technology), p-ATGLser404 (kind gift of Dr. Matthew Watt, University of Melbourne), hormone-sensitive lipase (HSL, #18381, Cell Signaling Technology), p-HSLser660 (#4126, Cell Signaling Technology), comparative gene identification-58 (CGI-58, ab183739, Abcam), G0/G1 Switch 2 (G0S2, 12091-1-AP, ProteinTech, IL), glycerol-3-phosphate acyltransferase 1 (PA5-20524, ThermoFisher), and hexokinase II (#2867, Cell Signaling Technology). As a loading control, membranes were stained with Memcode total protein stain (#24580, ThermoFisher)—the Memcode image was quantified and used to normalize protein abundance (23). To reduce gel-to-gel variability, an internal standard sample (composite skeletal muscle lysate from 8 obese individuals) was loaded on each gel and protein abundance was also normalized to this lane.
Muscle glycogen.
A small portion of each muscle sample was freeze dried for 48 hours (7 ± 3 mg dry weight) and homogenized in ice-cold water using 2 5-mm steel beads (TissueLyser II, Qiagen). Homogenates were then boiled for 5 minutes at 100°C and spun for 5 minutes at 13 000g (room temperature)—glycogen was determined in the supernatant using a glycogen assay kit (MAK016, Sigma; reference 24-26).
Hepatic and visceral fat.
A multiecho Dixon product sequence was performed with a breath-hold of at least 16 seconds. Scans were converted to 3-dimensional meta-image format using Matlab. Analysis was performed using 3D Slicer software and in-house Matlab routines. Briefly, visceral fat area was determined from 3, 5-mm axial slices in the L2-L3 vertebral region and hepatic fat percentage from 3, 5-mm axial slices of the liver. All analyses were performed by a trained investigator who was blinded to subject, group assignment, and training status.
Skeletal muscle lipidomics.
Untargeted liquid chromatography-MS-based shotgun lipidomics (tandem MS) was performed by the Michigan Regional Comprehensive Metabolomics Resource Core on samples from a subset of participants from HIIT (n = 8) and MICT (n = 9). A small portion of each muscle biopsy samples was weighed and homogenized. Lipids were extracted by a modified Bligh-Dyer method using a 2:2:2 ratio volume of methanol:H2O:dichloromethane at room temperature after spiking internal standards (27). The organic layer was collected and dried under nitrogen and the dried lipid extract was reconstituted in 100 μL of Buffer B (10:85:5 acetonitrile/isopropanol/H2O) containing 10 mM ammonium acetate and subjected to liquid chromatography MS by electrospray ionization (LABSIEX 5600 TOF MS: SCIEX, MA). Lipids were identified using LIPIDBLAST computer-generated tandem-MS library (28) and normalized to tissue weight.
Calculations
Resting metabolic rate.
Resting metabolic rate was calculated from the rates of oxygen consumption and carbon dioxide production using the modified Weir equation (29).
Glucose and glycerol rate of appearance (Ra).
Glucose Ra (glucose rate of appearance in plasma; i.e., hepatic glucose production) and glycerol Ra (glycerol rate of appearance in plasma, an index of whole-body lipolytic rate) were calculated from trace-to-tracee ratio using the steady-state Steele equation (30).
Peripheral insulin sensitivity.
Our primary measure of peripheral insulin sensitivity was the glucose rate of disappearance from plasma during steady-state clamp conditions, calculated as the sum of the exogenous glucose infusion rate and hepatic glucose production and normalized to steady-state insulin concentration and fat-free mass. We also report glucose infusion rate normalized to steady-state insulin concentration and fat-free mass (i.e., M-value). The M-value is commonly used as an indicator of whole-body insulin sensitivity but does not account for hepatic glucose production.
Statistical analysis
Data were checked for normality and nonnormally distributed data were log-transformed before statistical analysis. In the few cases where missing data for some measurements for some subjects was unavoidable (e.g., inadequate tissue yield, challenges with blood sampling), data for these measurements were excluded for all trials for these subjects. In these few instances, specific sample size is reported for each outcome. Linear mixed models were used to examine the main effects of group (MICT vs. HIIT) and visit (pre, trained 1d postEx, and trained 4d postEx) and group × visit interactions. When significant effects were observed, post hoc comparisons were made using Fisher’s least significant difference method. For lipidomic comparisons, linear mixed-effects models were used to determine significant effects between exercise and training groups using RStudio: lme4 package (31), and corrected for multiple comparisons for individual lipid species (32). P values ≤ 0.05 were considered statistically significant. Data are presented as mean ± SD unless noted otherwise.
Results
Pretraining subject characteristics
Pretraining subject characteristics are presented in Table 1. All participants were inactive young adults (31 ± 6 years) with obesity (BMI 33 ± 3 kg/m2). Pretraining anthropometric characteristics and the distribution of men/women were similar between MICT and HIIT (Table 1).
Table 1.
Whole-Body Phenotyping Measures Before and After Training
| MICT | HIIT | ||||
|---|---|---|---|---|---|
| Age (years) | 30 ± 6 | 32 ± 7 | |||
| Sex | 5 men, 10 women | 7 men, 9 women | |||
| Pretraining | Trained | Pretraining | Trained | ||
| Anthropometric characteristics | |||||
| Body mass (kg) | 100.0 ± 10.7 | 99.6 ± 10.6 | 96.6 ± 14.6 | 96.5 ± 14.4 | |
| Fat mass (kg) | 42.9 ± 8.1 | 42.3 ± 8.1 | 39.4 ± 6.5 | 38.8 ± 6.3 | |
| Fat-free mass (kg) | 57.1 ± 8.6 | 57.3 ± 8.8 | 57.3 ± 10.9 | 57.7 ± 10.9 | |
| BMI (kg/m2) | 34.1 ± 3.3 | 34.0 ± 3.0 | 32.4 ± 2.5 | 32.3 ± 2.4 | |
| Whole-body aerobic capacity | |||||
| VO2peak (L/min) | 2.4 ± 0.5 | 2.6 ± 0.5a | 2.5 ± 0.6 | 2.8 ± 0.6a | |
| Resting whole-body metabolic rate b | |||||
| RMR (kcal/d) | 1477 ± 230 | 1462 ± 202 | 1469 ± 172 | 1462 ± 201 | |
| Respiratory exchange ratio | 0.81 ± 0.04 | 0.80 ± 0.04 | 0.79 ± 0.04 | 0.79 ± 0.04 | |
Data are presented as mean ± SD.
aSignificant increase compared with pretraining (main effect; P < 0.001).
bMICT n = 14, HIIT n = 16 for RMR measurements. There were no significant differences between groups at baseline, and no significant group × visit interactions.
Anthropometric characteristics and RMR assessed in the trained state were obtained 4 days after the last exercise session.
Abbreviations: BMI, body mass index; HIIT, high-intensity interval training; MICT, moderate-intensity continuous training; RMR, resting metabolic rate; VO2peak, peak oxygen uptake.
Training effects on aerobic capacity, body composition, and resting energy expenditure
Adherence to the scheduled exercise training was very high and identical between groups, with participants completing an average of 95% of scheduled exercise sessions (MICT 95 ± 7%, HIIT: 95 ± 8%; all participants completed at least 75% of scheduled training sessions). Training increased aerobic capacity, as demonstrated by a ~10% increase in VO2peak in both MICT and HIIT (P < 0.0001) with no difference between groups (Table 1). By design, BMI, fat mass, and fat-free mass all remained stable throughout the training period (Table 1). There were no significant effects of training on resting metabolic rate or resting respiratory exchange ratio (Table 1), indicating unaltered resting energy expenditure and fuel selection under overnight fasting conditions.
Training effects on clinical biomarkers and lipid accumulation in liver and viscera
Three months of exercise training without weight loss did not affect resting blood pressure (systolic or diastolic), HbA1C, or overnight fasted circulating concentrations of total cholesterol, triglycerides, glucose, insulin, C-reactive protein, or IL-6 and there were no significant differences between MICT and HIIT for any of these parameters (Table 2). In addition, in the absence of weight loss, hepatic lipid accumulation, and visceral adipose tissue content were not significantly altered by MICT or HIIT (Table 2).
Table 2.
Clinical and Subclinical Biomarkers Before and After Training
| MICT | HIIT | ||||
|---|---|---|---|---|---|
| Pretraining | Trained | Pretraining | Trained | ||
| Clinical biomarkers | |||||
| Systolic blood pressure (mm Hg) | 128 ± 11 | 125 ± 13 | 127 ± 12 | 127 ± 14 | |
| Diastolic blood pressure (mm Hg) | 76 ± 9 | 74 ± 9 | 74 ± 9 | 74 ± 8 | |
| HbA1C (%) | 5.2 ± 0.3 | 5.2 ± 0.3 | 5.3 ± 0.3 | 5.4 ± 0.3 | |
| Plasma glucose (mM) | 5.0 ± 0.4 | 5.0 ± 0.5 | 4.8 ± 0.4 | 4.8 ± 0.4 | |
| Serum Insulin (μU/mL) | 18 ± 9 | 18 ± 8 | 16 ± 11 | 16 ± 8 | |
| Plasma cholesterol (mg/dL) | 153 ± 31 | 151 ± 31 | 156 ± 32 | 163 ± 34 | |
| Plasma triglycerides (mM) | 1.2 ± 0.7 | 1.1 ± 0.6 | 0.9 ± 0.7 | 1.0 ± 0.7 | |
| Plasma IL-6 (pg/mL) | 2.7 ± 1.3 | 3.4 ± 1.6 | 4.6 ± 7.6 | 3.8 ± 4.4 | |
| Plasma C-reactive protein (mg/L) | 9 ± 10 | 15 ± 16 | 5 ± 5 | 5 ± 6 | |
| Hepatic and visceral fat a | |||||
| Hepatic fat (%) | 10.4 ± 10.0 | 9.0 ± 7.3 | 8.7 ± 7.5 | 7.5 ± 5.4 | |
| Visceral fat area (cm2) | 157 ± 74 | 155 ± 70 | 169 ± 90 | 161 ± 77 | |
Data are presented as mean ± SD.
aMICT n = 12, HIIT n = 15 for hepatic and visceral fat analyses. There were no significant effects of group or visit, and no significant group × visit interactions. Clinical biomarkers in the trained state were obtained 4 days after the last exercise session.
Abbreviations: HIIT, high-intensity interval training; MICT, moderate-intensity continuous training.
Training effects on insulin sensitivity
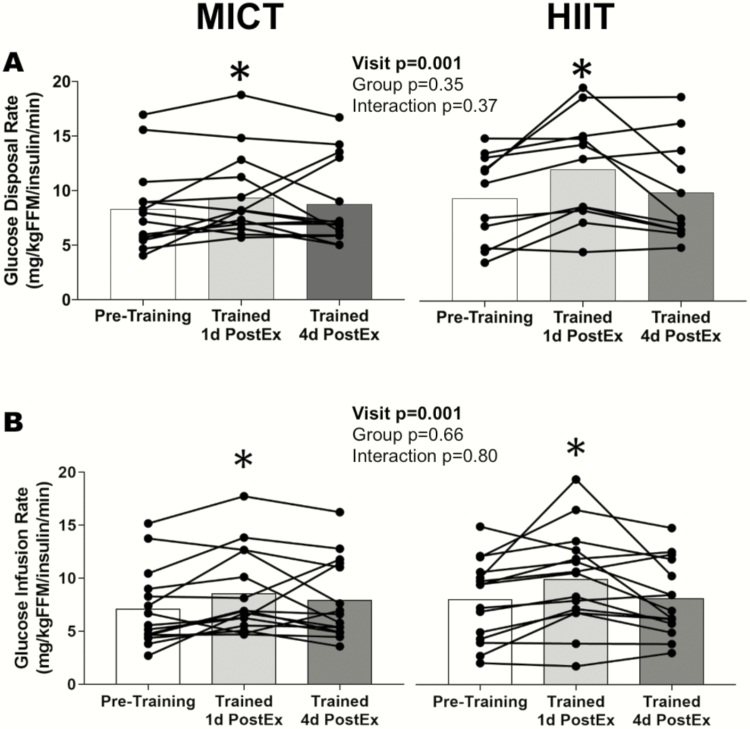
Peripheral insulin sensitivity.
Three months of training significantly increased the rate of glucose disposal during the hyperinsulinemic-euglycemic clamp when measured 1 day after exercise (P < 0.01), with no significant difference observed between HIIT and MICT (Fig. 2A). However, when trained participants abstained from exercise for 4 days, insulin sensitivity returned to pretraining levels in both groups. The glucose infusion rate during the clamp procedure (i.e., M-value) followed the same pattern, being significantly elevated at trained 1d postEx (P < 0.001) and then returning to pretraining levels at trained 4d postEx, with no significant differences between HIIT and MICT (Fig. 2B).
Figure 2.
Peripheral insulin sensitivity in response to training. (A) Rate of glucose disposal normalized to fat-free mass and insulin concentration during the hyperinsulinemic-euglycemic clamp (MICT n = 14, HIIT n = 11). (B) M-value: rate of exogenous glucose infusion normalized to fat-free mass and insulin concentration during the hyperinsulinemic-euglycemic clamp (MICT n = 15, HIIT n = 15). *Significant main effect for visit. Post hoc analysis identified trained 1d postEx was significantly greater than pretraining and trained 4d postEx (P < 0.05). The group means are indicated by bars and individual subjects’ data are connected by lines. HIIT, high-intensity interval training; MICT, moderate-intensity continuous training.
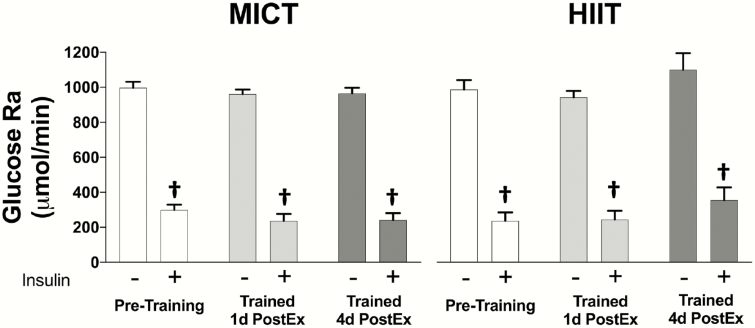
Hepatic insulin sensitivity.
Fasting hepatic glucose production (glucose Ra) was unaffected by training in both MICT and HIIT (Fig. 3). As expected, hepatic glucose production was profoundly suppressed (~75%) during the hyperinsulinemic-euglycemic clamp (P < 0.0001), but neither MICT nor HIIT affected this insulin-mediated suppression in glucose Ra. Importantly, this was the case for both trained 1d postEx and trained 4d postEx (Fig. 3).
Figure 3.
Hepatic glucose production in response to training. Glucose rate of appearance in the systemic circulation under fasting and insulin-stimulated conditions (MICT n = 14, HIIT n = 10). †Significant main effect of insulin (P < 0.05). There were no significant main effects of group or visit, and no significant interactions. Data are presented as mean ± SEM. HIIT, high-intensity interval training; MICT, moderate-intensity continuous training.
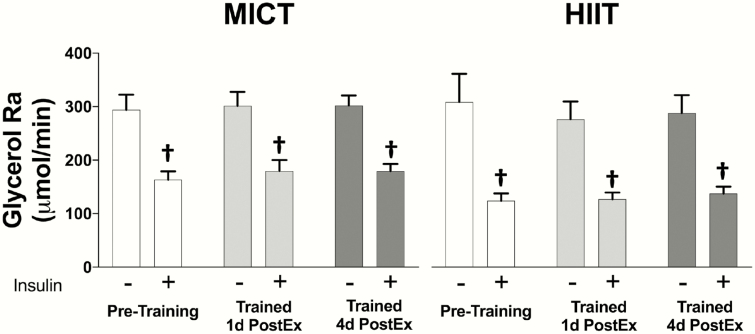
Antilipolytic sensitivity to insulin.
Whole-body lipolytic rate (glycerol Ra) after an overnight fast was not altered after 3 months of MICT or HIIT (Fig. 4). The potent antilipolytic effects of insulin reduced glycerol Ra during the clamp to levels ~50% lower than fasting (P < 0.0001), but again there was no effect of exercise training, whether or not subjects exercised the day before the measurement (Fig. 4).
Figure 4.
Whole-body lipolytic rate in response to training. Glycerol rate of appearance in the systemic circulation under fasting and insulin-stimulated conditions (MICT n = 14, HIIT n = 12). †Significant main effect of insulin (P < 0.05). There were no significant main effects of group or visit, and no significant interactions. Data are presented as mean ± SEM. HIIT, high-intensity interval training; MICT, moderate-intensity continuous training.
Skeletal muscle adaptations in response to training
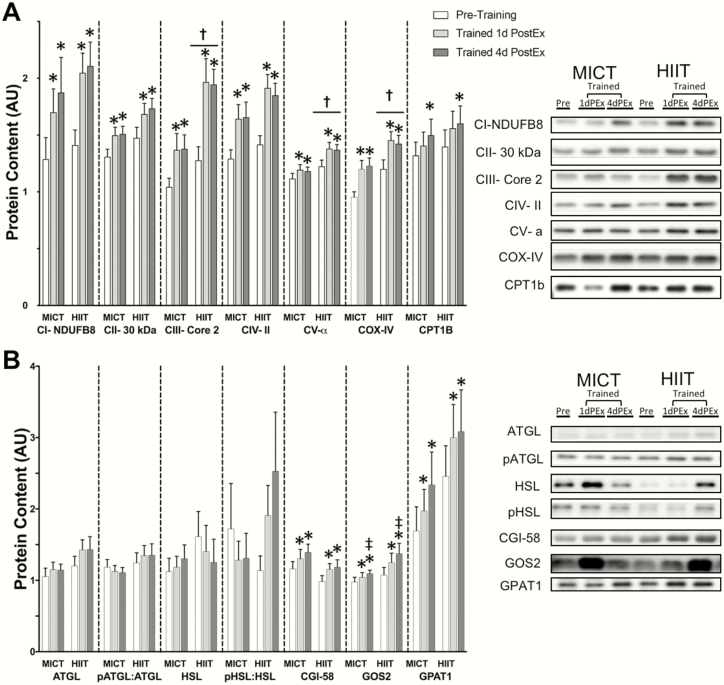
Muscle mitochondrial proteins.
Training significantly increased the protein abundance of subunits from all 5 mitochondrial respiratory complexes, as well as total COX-IV protein content (Fig. 5A, all P < 0.01), and MICT and HIIT induced similar increases in these proteins (no significant group × visit interactions). Training also significantly increased the abundance of CPT1B (P < 0.05), the protein in the mitochondrial outer membrane responsible for acyl-CoA transport, with no significant difference between MICT and HIIT (Fig. 5A).
Figure 5.
Skeletal muscle protein adaptations in response to training. (A) Protein abundance of mitochondrial proteins. (B) Protein abundance of proteins related to lipolysis and esterification. Sample sizes were MICT n = 14 and HIIT n = 16. *Significant main effect of visit, with post hoc tests identifying a significant difference compared with pretraining (P < 0.05). ‡Significant main effect of visit, with post hoc tests identifying significant difference compared with trained 1d postEx (P < 0.05). †Significant main effect of group (P < 0.05). There were no significant group × visit interactions. Data are presented as mean ± SEM. In the representative blots, “PEx” refers to postexercise. HIIT, high-intensity interval training; MICT, moderate-intensity continuous training.
Muscle proteins that regulate lipolysis and esterification.
Neither MICT nor HIIT significantly altered the total abundance of the key lipase proteins ATGL or HSL (Fig. 5B). There was also no significant change in the phosphorylation of ATGL at ser404 or HSL at ser660 in either group, suggesting unchanged muscle lipolytic activation under resting, non-insulin-stimulated conditions (muscle biopsies were not collected during the hyperinsulinemic clamp). Interestingly, training significantly increased the abundance of the key positive and negative regulators of ATGL lipase activity (CGI-58 and G0S2, respectively), with no significant differences between MICT and HIIT (Fig. 5B). Training also significantly increased the abundance of the esterification protein glycerol-3-phosphate acyltransferase 1, with no significant differences between MICT and HIIT (Fig. 5B).
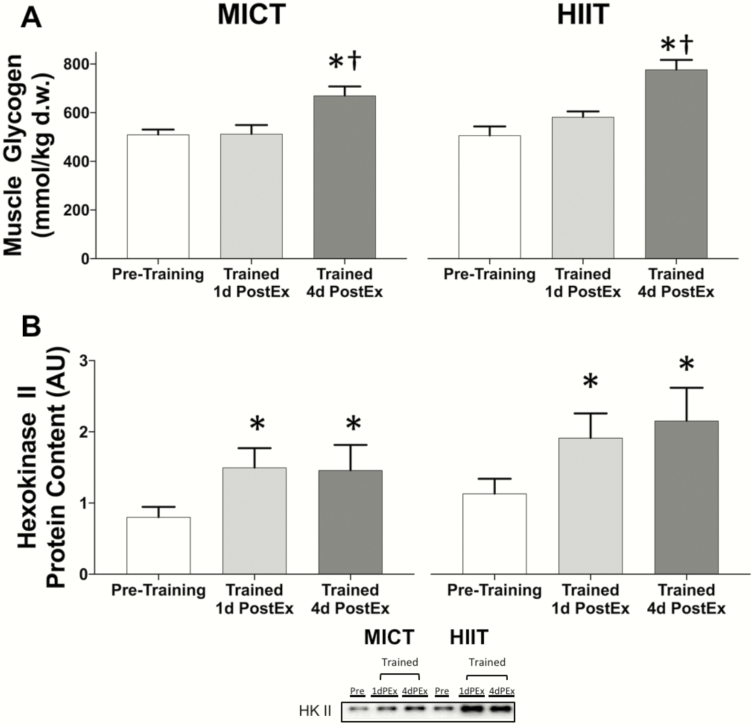
Muscle glycogen concentration and hexokinase II protein abundance.
When subjects had ~4 days to recover after their most recent session of exercise, training was found to significantly increase muscle glycogen concentration by ~40% (trained 4d postEx vs. pretraining: P < 0.0001) with no difference between MICT and HIIT (Fig. 6A). As expected, because of the reliance on muscle glycogen during exercise, when trained subjects exercised the evening before the measurements, muscle glycogen concentration was lower in trained 1d postEx versus trained 4d postEx (P < 0.0001), and muscle glycogen concentration during trained 1d postEx was not different from pretraining levels (Fig. 6A). Muscle glycogen concentrations during all visits were similar in MICT and HIIT (Fig. 6A). Training also significantly increased hexokinase II protein abundance by ~70%, with no difference between MICT and HIIT (Fig. 6B).
Figure 6.
Skeletal muscle glycogen content and hexokinase II protein abundance in response to training. (A) Muscle glycogen content (mmol per kilogram dry tissue weight). (B) Relative protein abundance of hexokinase II. Sample sizes were MICT n = 14 and HIIT n = 16. *Significant main effect of visit, with post hoc tests identifying a significant difference compared with pretraining (P < 0.05). †Significant main effect of visit, with post hoc tests identifying a significant difference compared with trained 1d postEx (P < 0.05). There were no significant main effects of group and no significant group × visit interactions. Data are presented as mean ± SEM. In the representative blots, “PEx” refers to postexercise. HIIT, high-intensity interval training; MICT, moderate-intensity continuous training.
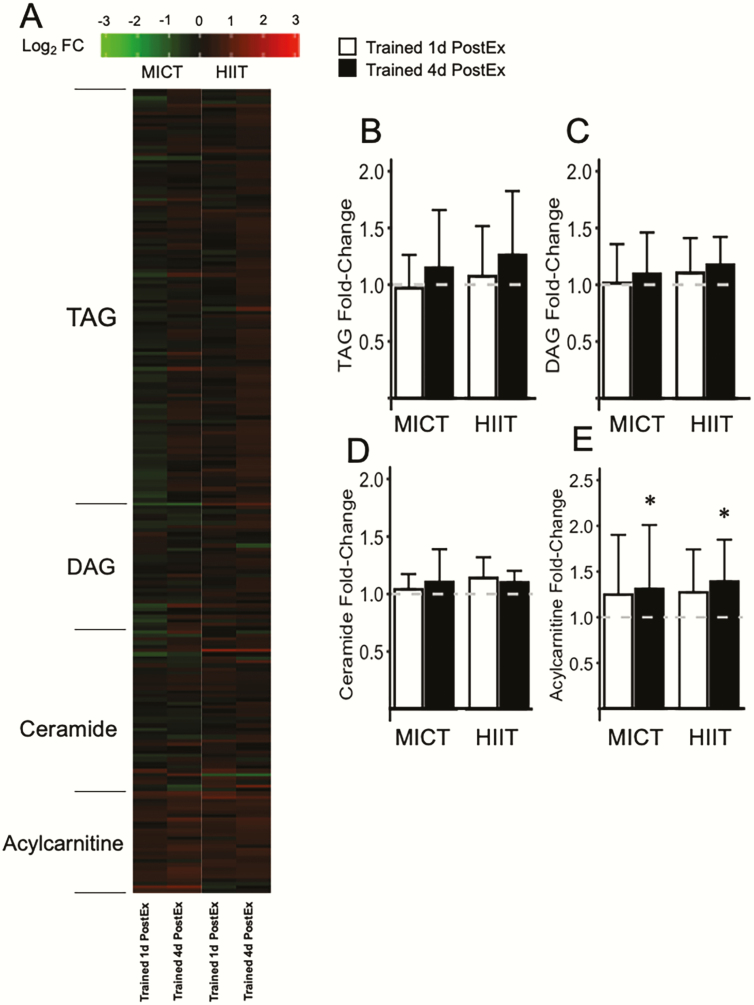
Skeletal muscle lipid responses to MICT and HIIT
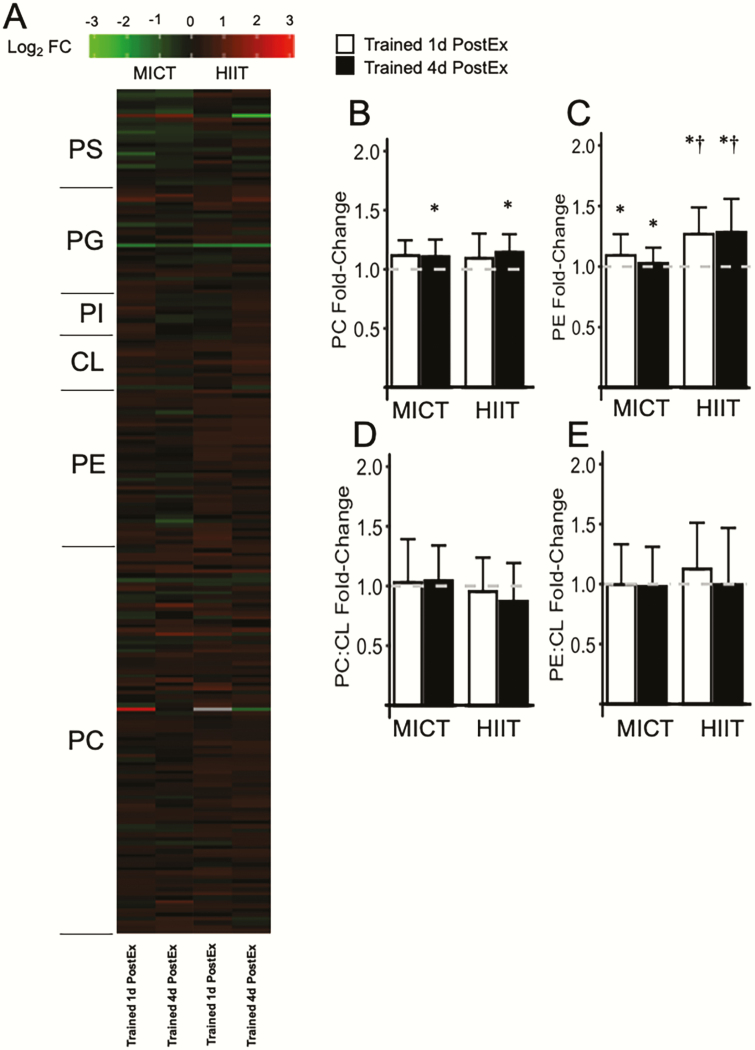
Using unbiased shotgun lipidomics, 734 lipid species were detected from 26 different lipid classes within 5 lipid categories (fatty acids, glycerolipids, glycerophospholipids, sphingolipids, sterols). The total abundance of primary muscle acylglycerols (triacylglycerol [TAG] and diacylglycerol [DAG]) did not change after exercise training in either HIIT or MICT (Fig. 7B-C; all supplementary materials are located in a digital research materials repository) (33). The saturation state of these lipids was also not affected by either exercise training program (33). Similarly, total skeletal muscle ceramide abundance (Fig. 7) and ceramide saturation state (33) were also not different after training. In contrast, total acylcarnitine (AC) abundance increased in muscle after exercise training (P = 0.03; Fig. 7E), with a significant increase specifically in polyunsaturated AC (P = 0.02), and long-chain AC (i.e., >16C; P = 0.02). We also found a significant increase (P < 0.05) in the most abundant phospholipids—phosphatidylcholine (PC) and phosphatidylethanolamine (PE) after exercise training in both groups (Fig. 8B-C). The increase in PE abundance from pretraining to trained 1d postEx and trained 4d postEx was slightly, yet significantly greater after HIIT compared with MICT (P = 0.04). When normalized to total cardiolipin (which is found almost exclusively in the inner mitochondrial membrane), the increased abundances of PC and PE after exercise training were no longer apparent (P > 0.05; Fig. 8D-E). Although PC and PE both increased in response to training, there was a greater increase in PE compared with PC, resulting in a small but significant reduction in the PC:PE ratio after exercise training (main effect P = 0.04). The PC:PE ratio was also lower after HIIT compared with MICT (P = 0.03).
Figure 7.
Skeletal muscle triacylglycerol, diacylglycerol, ceramide, and acylcarnitine abundance in response to training. (A) Heatmap displaying log2 fold-change (log2 FC) relative to pretraining for individual triacylglycerol (TAG), diacylglycerol (DAG), ceramide, and acylcarnitine species. (B-E) Relative abundance of total TAG, DAG, ceramide, and acylcarnitine normalized to pretraining. The pretraining level is indicated by the dashed line at 1.0. *Significant main effect of visit compared with pretraining (P < 0.05). There were no significant main effects of group and no significant group × visit interactions. Data are presented as mean ± SD (MICT n = 9, HIIT n = 8). HIIT, high-intensity interval training; MICT, moderate-intensity continuous training.
Figure 8.
Skeletal muscle phospholipid abundance in response to training. (A) Heatmap displaying log2 fold-change (log2 FC) relative to pretraining, for individual phospholipid species; phosphatidylserine (PS), phosphatidylglycerol (PG), phosphatidylinositol (PI), cardiolipin (CL), phosphatidylethanolamine (PE), and phosphatidylcholine (PC). (B-C) Relative abundance of total PC and PE normalized to pretraining. The pretraining level is indicated by the dashed line at 1.0. (D-E) Total PC and PE abundance expressed relative to total CL and normalized to pretraining. The pretraining ratio is indicated by the dashed line at 1.0. *Significant main effect of visit compared with pretraining (P < 0.05). †Significant group × visit interaction, with a larger increase compared with pretraining in HIIT versus MICT (P < 0.05). Data are presented as mean ± SD (MICT n = 9, HIIT n = 8). HIIT, high-intensity interval training; MICT, moderate-intensity continuous training.
Discussion
Our novel study design allowed for us to compare the metabolic responses to 12 weeks of MICT and HIIT, assessed the day after a session of exercise and after our trained participants abstained from exercise for 4 days. Despite robust differences in the exercise stimulus, 12 weeks of low-volume HIIT improved peripheral insulin sensitivity similarly to more conventional steady-state endurance exercise training (i.e., MICT) when measured the day after exercise. However, this improvement in insulin sensitivity with either training protocol did not persist after abstaining from exercise for only 4 days. These findings, therefore, support the notion that the insulin sensitizing effects of both HIIT and MICT are primarily mediated by factors stemming from the most recent exercise session(s) rather than a result of adaptations that accrue with chronic training. Interestingly, the observed longer term adaptive responses to training were very similar between HIIT and MICT, which induced comparable increases in oxidative capacity, corresponding elevations in the abundance of many skeletal muscle proteins involved in mitochondrial respiration, lipid and carbohydrate metabolism, as well as similar alterations in muscle lipid profile. Overall, our findings indicate that despite large differences in training intensity and volume, HIIT and MICT induce similar acute improvements in peripheral insulin sensitivity the day after exercise, as well as similar longer-term metabolic adaptations in skeletal muscle in adults with obesity.
Consistent with the well-described training-induced increase in muscle glycogen concentration (34, 35), when our subjects abstained from exercise for 4 days after training, muscle glycogen concentration was elevated by ~40% above pretraining levels. The training-induced increase in muscle glycogen concentration was not apparent when measured the day after exercise in our study, likely from inadequate time for full recovery of the muscle glycogen used during the exercise session performed the evening before. Because an exercise-induced reduction in muscle glycogen is a main contributor to this postexercise improvement in insulin sensitivity (36, 37), we contend the reduction in muscle glycogen may be the primary driver for the short-lived improvement in insulin sensitivity we measured trained 1d postEx. Along these lines, our finding that muscle glycogen concentration measured the day after exercise was similar between MICT and HIIT was likely a major factor underlying this similar increase in peripheral insulin action between groups. Interestingly, exposure to the 10 minutes of high intensity exercise during a session of HIIT (along with low-intensity active recovery between intervals and warm up/cool down) was enough to match the glycogen depletion following 45 minutes of MICT, despite markedly lower exercise time and energy expenditure in HIIT versus MICT. Changes in intramyocellular lipids and lipid intermediates (e.g., diacylglycerol, ceramide) after acute exercise have also been linked to improved insulin sensitivity after acute exercise (38), but our finding that muscle DAG and ceramide abundance were not different the day after exercise in either HIIT or MICT suggests that changes in the accumulation of these bioactive lipids did not contribute to the observed increase in insulin sensitivity. However, the localization and/or species changes of DAG and ceramide can affect insulin sensitivity (39-41), so our measures cannot rule out the possibility that acute changes in these muscle lipid parameters after exercise may have contributed to the increased insulin sensitivity the day after exercise. From a clinical perspective, similar improvements in acute insulin sensitivity between HIIT and MICT, despite meaningful differences in exercise time (25 vs. 45 minutes), has important practical implications because exercise time has been identified as a major factor contributing to low exercise adherence (17).
Our unique study design enabled us to determine if improvements in insulin sensitivity persisted when removing the effects of the most recent session(s) of exercise, and our finding that posttraining insulin sensitivity returned to pretraining levels after our subjects did not exercise for 4 days is in line with several previous studies reporting that exercise training does not increase insulin sensitivity when controlling for changes in body weight and the last session of exercise (10, 42, 43). However, these previous studies only examined the effects of conventional steady-state endurance exercise training (e.g., MICT), and here we confirm that this is the case for HIIT as well. The effect size for the differences in our peripheral insulin sensitivity measures between pretraining and trained 4d postEx was < 0.30, suggesting that the lack of a persistent improvement in insulin sensitivity measured 4 days after 12 weeks of training was not due to being statistically underpowered for this comparison. It is important to acknowledge the considerable controversy regarding the role of exercise training on insulin sensitivity, with many studies reporting improved insulin sensitivity after chronic endurance training (44-47). However, most of these studies did not fully control for changes in body weight/fat mass, and even very small changes in body weight can have potent, multiorgan insulin sensitizing effects (5). Therefore, to assess the direct effects of exercise training on insulin action, it is critical to have participants strictly maintain body mass throughout training, as we have done here. Importantly, in addition to weight maintenance in our study, 12 weeks of HIIT and MICT also did not change body composition (i.e., fat mass and fat-free mass). Some of the discrepancy regarding the effects of exercise training on insulin sensitivity may also be due to the timing of measurements after the most recent session and the content and composition of meals consumed after exercise. Acute effects of exercise could persist for at least a few days after exercise, especially if the meals consumed after exercise do not replenish muscle glycogen (37, 48, 49). By strictly controlling for weight loss, body composition changes, and timing of exercise relative to the metabolic measurements, our findings provide strong evidence that the impacts of both HIIT and MICT on insulin sensitivity are due to the acute effects of the most recent exercise training session(s) that persist into the next day.
The lack of persistent improvement in peripheral insulin sensitivity after training in our study occurred despite significant increases in whole-body oxidative capacity and mitochondrial respiratory protein abundance. Although increases in oxidative capacity are clearly beneficial for improving exercise tolerance, how, or even if, increased muscle mitochondrial density/oxidative capacity directly affects insulin sensitivity is controversial (50-52). Mitochondrial density is often reported to be lower in insulin-resistant compared with insulin-sensitive populations, and it has been suggested that training-induced increases in muscle mitochondrial density and oxidative capacity may directly contribute to improvements in insulin sensitivity (53). Proponents of this hypothesis have suggested that increased mitochondrial density is associated with an increased proportion of fat oxidation at rest (54, 55), and, in turn, this increased fat oxidation may lead to decreased accumulation of bioactive lipid species in skeletal muscle that may directly impair insulin signaling (53). However, although increased mitochondrial density is a consistent adaptation to exercise training in obese adults, resting fat oxidation is often found to remain unaltered after training (56, 57), which is supported by our data. Importantly, as noted by others (50-52), even in sedentary, obese individuals, skeletal muscle mitochondrial oxidative capacity greatly exceeds requirements for resting fat oxidation, so it is not clear how an increased capacity for fat oxidation (e.g., increased mitochondrial density) after training would alter intramyocellular lipid abundance under resting conditions.
A key mechanism contributing to insulin resistance in obesity is an elevated whole-body lipolytic rate and consequent excessive delivery of fatty acids to tissues such as skeletal muscle and liver (58-60). Glycerol Ra (µmol/min) under fasting conditions is commonly found to be ~2-fold higher in obese compared with lean adults and the glycerol Ra values in our participants were very similar to previous reports in obese adults, demonstrating very high whole-body lipolytic rates (61, 62). An important finding in our study was that, in the absence of weight loss, neither HIIT nor MICT altered whole-body lipolytic rate after an overnight fast. The lack of effect of MICT on resting lipolytic rate supports previous literature involving low- or moderate-intensity exercise training (57, 61, 63, 64) and our data provide the first evidence that HIIT also does not significantly alter resting lipolytic rate in obese humans. We previously demonstrated that reductions in lipolytic rate are a key mechanism contributing to improvements in insulin sensitivity after weight loss with or without exercise training (62). We speculate that the strict maintenance of body weight in the present study contributed to the finding of unchanged lipolytic rate with exercise training, and that decreases in lipolytic rate may be important to enable persistent improvements in insulin sensitivity in adults with obesity. Delineating the direct effect of exercise from the indirect effect that exercise may have on weight loss has high clinical impact because several long-term exercise training studies (i.e., > 6 months) indicate that exercise training often does not result in meaningful weight loss if diet is not controlled or at least monitored (65-68).
In parallel with our findings of unchanged total fat mass, we found no significant alteration in hepatic or visceral fat content in either HIIT or MICT. Although some studies that have reported small but significant changes in hepatic and visceral fat after exercise training without weight loss (43, 69-72), our findings align with other studies that found unchanged lipid accumulation in these tissues after moderate-intensity exercise training (73, 74). We expand on the latter by demonstrating that hepatic and visceral lipid deposition were also unchanged after 12 weeks of HIIT. Some of the discrepancies regarding the effects of exercise training on lipid accumulation in the liver and viscera may be related to methodological differences (e.g., magnetic resonance imaging, magnetic resonance spectroscopy, computed tomography techniques) and/or the influence of subtle differences in changes in body weight within and across studies. In studies reporting significant reductions in liver/visceral fat after exercise without weight loss, the magnitude of these changes is small compared with those observed with weight loss via either diet alone or diet plus exercise (43, 70). Moreover, the reduction in visceral fat after weight loss has been found to be the same whether or not subjects exercised while losing weight (43).
Exercise training is known to modify muscle lipid metabolism (75), and our observation that both HIIT and MICT modified the abundance of factors regulating muscle lipase activity is generally consistent with this notion. Although neither HIIT nor MICT altered the protein content of the primary lipase enzymes, ATGL or HSL, our finding that training simultaneously increased abundance of both positive (CGI-58) and negative (G0S2) regulators of ATGL activity is intriguing. The functional relevance of the concurrent increase in these proteins is unclear, but it is attractive to consider that the training-induced increase of both of these proteins may allow for enhanced lipolytic regulation in skeletal muscle—to more rapidly and accurately match intracellular fatty acid availability to meet changing muscle energy requirements in transitions from rest to exercise and vice versa.
Although endurance exercise training is often found to increase muscle TAG abundance, especially in nonobese subjects (76, 77), our finding that neither MICT nor HIIT altered muscle TAG is consistent with several other studies in adults with obesity (78-80). Muscle TAG are already elevated in obese subjects even without exercise (81), likely because of the excessive lipolytic rates commonly found in obese patients (61, 82), which in turn delivers abundant fatty acids to skeletal muscle to provide substrate for muscle TAG synthesis. Because exercise training did not modify the high lipolytic rate in our obese subjects, it was not surprising that exercise training did not increase muscle TAG any further. The maintenance of high lipolytic rates after training (and thereby maintaining the delivery of ample substrate for DAG and ceramide synthesis) may also help explain why we did not detect a measurable reduction in muscle DAG or ceramide abundance. Although muscle DAG and ceramide concentrations have been linked with insulin resistance (83, 84), changes in the localization of these bioactive lipids within the myocyte (e.g., proximity to the sarcolemma) may be even more important for modulating insulin sensitivity (39, 40). Unfortunately, we were not able to measure the localization of these muscle lipids in our study.
Muscle acylcarnitine accumulation has also been linked with insulin resistance (85). As such, the increased abundance of long-chain acylcarnitines in skeletal muscle after both MICT and HIIT was unexpected. Although this very modest increase in muscle acyl-carnitine abundance may have contributed to the lack of a training-induced increase in insulin sensitivity, we contend this possibility is remote (86). Factors responsible for this training-induced increase in acylcarnitine are not completely clear, but it is possible that the persistently high lipolytic rate in our obese subjects may once again underlie this observation. Acylcarnitines accumulate when CPT-1-mediated mitochondrial transport of fatty acyl-CoA and subsequent rates of β-oxidation exceed the rates of downstream reactions (i.e., TCA cycle, electron transport, oxidative phosphorylation). Although training increased the abundance of muscle CPT-1B abundance, as well as other markers for increase mitochondrial density and fatty acid oxidative capacity, our measurements were conducted at rest, when energy expenditure is very low (similarly low before vs. after training). Therefore, a persistently elevated lipolytic rate and the resultant excessive delivery of fatty acids to an expanded mitochondrial network may increase β-oxidation. Without a compensatory increase in energy expenditure/ATP production, this could result in an accumulation of fatty acyl-CoAs, which are readily converted to acylcarnitine. Given the suggested links between acylcarnitine accumulation and insulin resistance (85) this response may seem detrimental, but the magnitude of increase in acylcarnitine we observed after training did not correspond with impaired insulin action in our subjects.
Changes in the ratio of the most abundant phospholipids, PC and PE, have also been implicated in regulating insulin sensitivity, with a lower PC:PE ratio associated with enhanced insulin action (87, 88). In our study, however, the reduction in muscle PC:PE ratio found after training was not accompanied by an improvement in insulin action. PC and PE are primarily found on mitochondrial membranes, and because the increase in both muscle PC and PE were no longer evident when we normalized to the mitochondrial marker, cardiolipin, we interpret this to indicate that the increase in these phospholipids were largely a reflection of mitochondrial biogenesis in response to exercise training. However, factors that may be responsible for the slight, but significantly greater proportional increase in PE versus PC after training (especially in HIIT) are not clear.
Our findings that 3 months of HIIT and MICT induced similar increases in VO2peak and skeletal muscle mitochondrial proteins are in line with previous studies comparing sprint interval training with MICT (89-92). Indeed, the general similarity of adaptations to HIIT and MICT raises the important question as to how similar adaptations can be derived from a substantially smaller volume of exercise with HIIT. Compared with moderate-intensity exercise, higher-intensity exercise recruits more type II muscle fibers and elicits a higher rate of overall glycogenolysis (93, 94). In our study, despite the lower volume of exercise in HIIT, muscle glycogen was similarly reduced the day after exercise when compared to MICT; and as noted previously, we suggest that this is a key factor contributing to the similar acute improvement in insulin sensitivity the day after exercise. In addition, because muscle glycogen availability is known to influence intracellular signaling cascades (e.g., AMP kinase) that augment mitochondrial biogenesis and proteins involved in carbohydrate/lipid handling (95-98), we contend the comparable glycogen depletion with each session HIIT and MICT may also drive the broadly similar skeletal muscle training adaptations. Our finding that 12 weeks of HIIT and MICT have similar effects on VO2peak and skeletal muscle mitochondrial proteins suggests that obese individuals can achieve similar benefits from selecting either of these approaches, thereby expanding exercise options.
Experimental considerations and limitations
Although this was a well-controlled study, there are some limitations that should be considered. The distribution of men and women was similar in our HIIT and MICT groups, but our study was not adequately powered to determine sex differences in training responses between groups. We did examine potential group × visit × sex interactions for our primary outcomes—none were statistically significant. Because of the requirement for scheduled posttesting relative to the completion of the 12-week training intervention, we were not able to control the timing of testing relative to menstrual phase, which may increase variability in some outcomes. For our posttraining DEXA measurements, we did not standardize for some factors that have been reported (99) to have small influences on body composition assessment (e.g., fasting status, time of day, number of hours post exercise), and therefore cannot completely discount the possibility that very small improvements in body composition occurred with training. We would note that if small improvements in body composition did occur, they did not translate to improved insulin sensitivity assessed 4 days after the last exercise session. As discussed in detail previously, we deliberately chose not to match total work, energy expenditure, or total exercise time between HIIT and MICT to enable a more translational comparison of 2 distinct but commonly implemented exercise prescriptions. Therefore, our findings do not distinguish the influence of exercise intensity, duration, or energy expenditure per se on our primary outcomes. However, based on our findings we can conclude that the low-volume HIIT protocol we employed resulted in similar adaptations compared with MICT despite a lower exercise time requirement and energy expenditure. Our participants had obesity (BMI 30-40 kg/m2) but otherwise did not present with detectable cardiometabolic disease, which enabled us to study a population that is at elevated risk of developing type 2 diabetes but avoid the potential confounding influence of medications on insulin sensitivity and training adaptations (100-103). Therefore, although our findings translate to the very large population of adults with obesity and/or prediabetes who have yet to develop overt cardiometabolic health complications, the responses to HIIT and MICT in adults with obesity-related metabolic complications may not be identical (104, 105).
Conclusion
In summary, our findings demonstrate that despite considerably lower exercise duration and energy expenditure, low-volume HIIT induced remarkably similar adaptations compared with the more “conventional” endurance exercise training (i.e., MICT) in adults with obesity. The similarities in the adaptive responses to HIIT and MICT were observed at both the clinical level (e.g., insulin sensitivity, aerobic capacity, hepatic and visceral lipid accumulation) and subclinical level (e.g., lipolytic rate, protein abundance of factors regulating mitochondrial respiration and muscle lipid metabolism, muscle lipid profile). These findings support the use of either HIIT or MICT to induce favorable short-term metabolic responses (i.e., improved insulin sensitivity after each session of exercise) and longer term subclinical adaptations with similar efficacy. Importantly, our findings also indicate that despite improvements in whole-body oxidative capacity and mitochondrial density after 12 weeks of HIIT and MICT (in absence of weight loss), insulin sensitivity returned to pre-training levels when measured 4 days after the most recent session of exercise. This is consistent with the notion that the main effect of exercise on insulin action stems from responses to the most recent session of exercise, rather than attributed to adaptations that accrue in response to exercise training, regardless of whether the training is HIIT or MICT.
Acknowledgments
We thank the study participants for their efforts. We are grateful to the exercise training coordinators and supervisors; Dr. Benjamin Carr, Dr. Jacob Haus, Jeffrey Wysocki, RN; the staff at the Michigan Clinical Research Unit; and all the members of the Substrate Metabolism Lab for study assistance.
Financial Support: This study was supported by the National Institutes of Health (R01DK077966, P30DK089503, U24DK097153, T32DK007245, F32DK117522) and the Canadian Institutes of Health Research (338735 and 146190).
Clinical Trials Information: Registered at www.clinicaltrials.gov as NCT02706093.
Glossary
Abbreviations
- AC
acylcarnitine
- ATGL
adipose triglyceride lipase
- BMI
body mass index
- DAG
diacylglycerol
- glucose Ra
glucose rate of appearance in plasma
- glycerol Ra
glycerol rate of appearance in plasma
- HIIT
high-intensity interval training
- HRmax
maximal heart rate
- HSL
hormone-sensitive lipase
- MICT
moderate-intensity continuous training
- MS
mass spectrometry
- PC
phosphatidylcholine
- PE
phosphatidylethanolamine
- TAG
triacylglycerol
- VO2peak
peak oxygen uptake
Additional Information
Disclosure Summary: The authors have no disclosures or conflicts of interest to report.
Data Availability: The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
- 1. Garber CE, Blissmer B, Deschenes MR, et al. ; American College of Sports Medicine American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334-1359. [DOI] [PubMed] [Google Scholar]
- 2. Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387(10031):1947-1956. [DOI] [PubMed] [Google Scholar]
- 3. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39:2065-2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25Suppl 3:1-72. [DOI] [PubMed] [Google Scholar]
- 5. Magkos F, Fraterrigo G, Yoshino J, et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016;23(4):591-601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heath GW, Gavin JR 3rd, Hinderliter JM, Hagberg JM, Bloomfield SA, Holloszy JO. Effects of exercise and lack of exercise on glucose tolerance and insulin sensitivity. J Appl Physiol Respir Environ Exerc Physiol. 1983;55(2):512-517. [DOI] [PubMed] [Google Scholar]
- 7. Perseghin G, Price TB, Petersen KF, et al. Increased glucose transport-phosphorylation and muscle glycogen synthesis after exercise training in insulin-resistant subjects. N Engl J Med. 1996;335(18):1357-1362. [DOI] [PubMed] [Google Scholar]
- 8. Newsom SA, Everett AC, Hinko A, Horowitz JF. A single session of low-intensity exercise is sufficient to enhance insulin sensitivity into the next day in obese adults. Diabetes Care. 2013;36(9):2516-2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. King DS, Dalsky GP, Clutter WE, et al. Effects of exercise and lack of exercise on insulin sensitivity and responsiveness. J Appl Physiol (1985). 1988;64(5):1942-1946. [DOI] [PubMed] [Google Scholar]
- 10. Segal KR, Edano A, Abalos A, et al. Effect of exercise training on insulin sensitivity and glucose metabolism in lean, obese, and diabetic men. J Appl Physiol (1985). 1991;71(6):2402-2411. [DOI] [PubMed] [Google Scholar]
- 11. Gillen JB, Gibala MJ. Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl Physiol Nutr Metab. 2014;39(3):409-412. [DOI] [PubMed] [Google Scholar]
- 12. Gibala MJ. Interval training for cardiometabolic health: why such a HIIT? Curr Sports Med Rep. 2018;17(5):148-150. [DOI] [PubMed] [Google Scholar]
- 13. Little JP, Gillen JB, Percival ME, et al. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J Appl Physiol (1985). 2011;111(6):1554-1560. [DOI] [PubMed] [Google Scholar]
- 14. Gillen JB, Percival ME, Ludzki A, Tarnopolsky MA, Gibala MJ. Interval training in the fed or fasted state improves body composition and muscle oxidative capacity in overweight women. Obesity (Silver Spring). 2013;21(11):2249-2255. [DOI] [PubMed] [Google Scholar]
- 15. Gerosa-Neto J, Panissa VLGP, Monteiro PA, et al. High- or moderate intensity training promotes change in cardiorespiratory fitness, but not visceral fat, in obese men: a randomized trial of equal energy expenditure. Resp Physiol Neurobiol. 2019;266:150-155. [DOI] [PubMed] [Google Scholar]
- 16. Gibala MJ, Little JP, Macdonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol. 2012;590(5):1077-1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34(12):1996-2001. [DOI] [PubMed] [Google Scholar]
- 18. Fisher G, Brown AW, Bohan Brown MM, et al. High intensity interval- vs moderate intensity- training for improving cardiometabolic health in overweight or obese males: a randomized controlled trial. Plos One. 2015;10(10):e0138853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Heiston EM, Eichner NZ, Gilbertson NM, Malin SK. Exercise improves adiposopathy, insulin sensitivity and metabolic syndrome severity independent of intensity. Exp Physiol. 2020;105(4):632-640. [DOI] [PubMed] [Google Scholar]
- 20. Francois ME, Durrer C, Pistawka KJ, Halperin FA, Chang C, Little JP. Combined interval training and post-exercise nutrition in type 2 diabetes: a randomized control trial. Front Physiol. 2017;8:528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Madsen SM, Thorup AC, Overgaard K, Jeppesen PB. High intensity interval training improves glycaemic control and pancreatic β cell function of type 2 diabetes patients. Plos One. 2015;10(8):e0133286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237(3):E214-E223. [DOI] [PubMed] [Google Scholar]
- 23. Moritz CP. Tubulin or not tubulin: heading toward total protein staining as loading control in Western blots. Proteomics. 2017;17:1600189. [DOI] [PubMed] [Google Scholar]
- 24. Nieman DC, Zwetsloot KA, Meaney MP, Lomiwes DD, Hurst SM, Hurst RD. Post-exercise skeletal muscle glycogen related to plasma cytokines and muscle IL-6 protein content, but not muscle cytokine mRNA expression. Front Nutr. 2015;2:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cheng AJ, Willis SJ, Zinner C, et al. Post-exercise recovery of contractile function and endurance in humans and mice is accelerated by heating and slowed by cooling skeletal muscle. J Physiol. 2017;595(24):7413-7426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Margolis LM, Wilson MA, Whitney CC, et al. Exercising with low muscle glycogen content increases fat oxidation and decreases endogenous, but not exogenous carbohydrate oxidation. Metabolism. 2019;97:1-8. [DOI] [PubMed] [Google Scholar]
- 27. Bligh EG, Dyer WJ. A rapid method of total lipid extraction and purification. Can J Biochem Physiol. 1959;37(8):911-917. [DOI] [PubMed] [Google Scholar]
- 28. Kind T, Liu KH, Lee DY, DeFelice B, Meissen JK, Fiehn O. LipidBlast in silico tandem mass spectrometry database for lipid identification. Nat Methods. 2013;10(8):755-758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mansell PI, Macdonald IA. Reappraisal of the Weir equation for calculation of metabolic rate. Am J Physiol. 1990;258(6 Pt 2):R1347-R1354. [DOI] [PubMed] [Google Scholar]
- 30. Steele R. Influences of glucose loading and of injected insulin on hepatic glucose output. Ann N Y Acad Sci. 1959;82:420-430. [DOI] [PubMed] [Google Scholar]
- 31. Bates D, Mächler M, Bolker BM, Walker SC. Fitting linear mixed-effects models using lme4. J Statistical Software. 2015;67: DOI: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 32. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B. 1995;57:289-300. [Google Scholar]
- 33. Ryan BJ, Schleh MW, Ahn C, et al. Supplemental tables: moderate-intensity exercise and high-intensity interval training affect insulin sensitivity similarly in obese adults. JCEM 2020. DOI: 10.6084/m9.figshare.12316997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bergström J, Hultman E. Muscle glycogen synthesis after exercise: an enhancing factor localized to the muscle cells in man. Nature. 1966;210(5033):309-310. [DOI] [PubMed] [Google Scholar]
- 35. Bergström J, Hultman E, Roch-Norlund AE. Muscle glycogen synthetase in normal subjects. Basal values, effect of glycogen depletion by exercise and of a carbohydrate-rich diet following exercise. Scand J Clin Lab Invest. 1972;29(2):231-236. [DOI] [PubMed] [Google Scholar]
- 36. Fell RD, Terblanche SE, Ivy JL, Young JC, Holloszy JO. Effect of muscle glycogen content on glucose uptake following exercise. J Appl Physiol Respir Environ Exerc Physiol. 1982;52(2):434-437. [DOI] [PubMed] [Google Scholar]
- 37. Bogardus C, Thuillez P, Ravussin E, Vasquez B, Narimiga M, Azhar S. Effect of muscle glycogen depletion on in vivo insulin action in man. J Clin Invest. 1983;72(5):1605-1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schenk S, Horowitz JF. Acute exercise increases triglyceride synthesis in skeletal muscle and prevents fatty acid-induced insulin resistance. J Clin Invest. 2007;117(6):1690-1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bergman BC, Hunerdosse DM, Kerege A, Playdon MC, Perreault L. Localisation and composition of skeletal muscle diacylglycerol predicts insulin resistance in humans. Diabetologia. 2012;55(4):1140-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Perreault L, Newsom SA, Strauss A, et al. Intracellular localization of diacylglycerols and sphingolipids influences insulin sensitivity and mitochondrial function in human skeletal muscle. JCI Insight. 2018;3:e96805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chung JO, Koutsari C, Blachnio-Zabielska AU, Hames KC, Jensen MD. Intramyocellular ceramides: subcellular concentrations and fractional de novo synthesis in postabsorptive humans. Diabetes. 2017;66(8):2082-2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Morrison DJ, Kowalski GM, Grespan E, Mari A, Bruce CR, Wadley GD. Measurement of postprandial glucose fluxes in response to acute and chronic endurance exercise in healthy humans. Am J Physiol Endocrinol Metab. 2018;314(5):E503-E511. [DOI] [PubMed] [Google Scholar]
- 43. Ross R, Dagnone D, Jones PJ, et al. Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. A randomized, controlled trial. Ann Intern Med. 2000;133(2):92-103. [DOI] [PubMed] [Google Scholar]
- 44. Duncan GE, Perri MG, Theriaque DW, Hutson AD, Eckel RH, Stacpoole PW. Exercise training, without weight loss, increases insulin sensitivity and postheparin plasma lipase activity in previously sedentary adults. Diabetes Care. 2003;26(3):557-562. [DOI] [PubMed] [Google Scholar]
- 45. Bajpeyi S, Tanner CJ, Slentz CA, et al. Effect of exercise intensity and volume on persistence of insulin sensitivity during training cessation. J Appl Physiol (1985). 2009;106(4):1079-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Konopka AR, Asante A, Lanza IR, et al. Defects in mitochondrial efficiency and H2O2 emissions in obese women are restored to a lean phenotype with aerobic exercise training. Diabetes. 2015;64(6):2104-2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Prior SJ, Goldberg AP, Ortmeyer HK, et al. Increased skeletal muscle capillarization independently enhances insulin sensitivity in older adults after exercise training and detraining. Diabetes. 2015;64(10):3386-3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cartee GD, Young DA, Sleeper MD, Zierath J, Wallberg-Henriksson H, Holloszy JO. Prolonged increase in insulin-stimulated glucose transport in muscle after exercise. Am J Physiol. 1989;256(4 Pt 1):E494-E499. [DOI] [PubMed] [Google Scholar]
- 49. Newsom SA, Schenk S, Thomas KM, et al. Energy deficit after exercise augments lipid mobilization but does not contribute to the exercise-induced increase in insulin sensitivity. J Appl Physiol (1985). 2010;108(3):554-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Holloszy JO. Skeletal muscle “mitochondrial deficiency” does not mediate insulin resistance. Am J Clin Nutr. 2009;89(1):463S-466S. [DOI] [PubMed] [Google Scholar]
- 51. Holloszy JO. “Deficiency” of mitochondria in muscle does not cause insulin resistance. Diabetes. 2013;62(4):1036-1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Muoio DM, Neufer PD. Lipid-induced mitochondrial stress and insulin action in muscle. Cell Metab. 2012;15(5):595-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Goodpaster BH. Mitochondrial deficiency is associated with insulin resistance. Diabetes. 2013;62(4):1032-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kelley DE, Goodpaster B, Wing RR, Simoneau JA. Skeletal muscle fatty acid metabolism in association with insulin resistance, obesity, and weight loss. Am J Physiol. 1999;277(6):E1130-E1141. [DOI] [PubMed] [Google Scholar]
- 55. Goodpaster BH, Katsiaras A, Kelley DE. Enhanced fat oxidation through physical activity is associated with improvements in insulin sensitivity in obesity. Diabetes. 2003;52(9):2191-2197. [DOI] [PubMed] [Google Scholar]
- 56. Kanaley JA, Weatherup-Dentes MM, Alvarado CR, Whitehead G. Substrate oxidation during acute exercise and with exercise training in lean and obese women. Eur J Appl Physiol. 2001;85(1-2):68-73. [DOI] [PubMed] [Google Scholar]
- 57. van Aggel-Leijssen DP, Saris WH, Wagenmakers AJ, Senden JM, van Baak MA. Effect of exercise training at different intensities on fat metabolism of obese men. J Appl Physiol (1985). 2002;92(3):1300-1309. [DOI] [PubMed] [Google Scholar]
- 58. Santomauro AT, Boden G, Silva ME, et al. Overnight lowering of free fatty acids with Acipimox improves insulin resistance and glucose tolerance in obese diabetic and nondiabetic subjects. Diabetes. 1999;48(9):1836-1841. [DOI] [PubMed] [Google Scholar]
- 59. Magkos F, Fabbrini E, Conte C, Patterson BW, Klein S. Relationship between adipose tissue lipolytic activity and skeletal muscle insulin resistance in nondiabetic women. J Clin Endocrinol Metab. 2012;97(7):E1219-E1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Van Pelt DW, Guth LM, Wang AY, Horowitz JF. Factors regulating subcutaneous adipose tissue storage, fibrosis, and inflammation may underlie low fatty acid mobilization in insulin-sensitive obese adults. Am J Physiol Endocrinol Metab. 2017;313(4):E429-E439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Horowitz JF, Coppack SW, Paramore D, Cryer PE, Zhao G, Klein S. Effect of short-term fasting on lipid kinetics in lean and obese women. Am J Physiol. 1999;276(2):E278-E284. [DOI] [PubMed] [Google Scholar]
- 62. Schenk S, Harber MP, Shrivastava CR, Burant CF, Horowitz JF. Improved insulin sensitivity after weight loss and exercise training is mediated by a reduction in plasma free fatty acid mobilization, not enhanced oxidative capacity. J Physiol. 2009;587:4949-4961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Horowitz JF, Leone TC, Feng W, Kelly DP, Klein S. Effect of endurance training on lipid metabolism in women: a potential role for PPARalpha in the metabolic response to training. Am J Physiol Endocrinol Metab. 2000;279(2):E348-E355. [DOI] [PubMed] [Google Scholar]
- 64. Hickner RC, Racette SB, Binder EF, Fisher JS, Kohrt WM. Effects of 10 days of endurance exercise training on the suppression of whole body and regional lipolysis by insulin. J Clin Endocrinol Metab. 2000;85(4):1498-1504. [DOI] [PubMed] [Google Scholar]
- 65. Church TS, Martin CK, Thompson AM, Earnest CP, Mikus CR, Blair SN. Changes in weight, waist circumference and compensatory responses with different doses of exercise among sedentary, overweight postmenopausal women. Plos One. 2009;4(2):e4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Jakicic JM, Otto AD, Lang W, et al. The effect of physical activity on 18-month weight change in overweight adults. Obesity (Silver Spring). 2011;19(1):100-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Thorogood A, Mottillo S, Shimony A, et al. Isolated aerobic exercise and weight loss: a systematic review and meta-analysis of randomized controlled trials. Am J Med. 2011;124(8):747-755. [DOI] [PubMed] [Google Scholar]
- 68. Donnelly JE, Hill JO, Jacobsen DJ, et al. Effects of a 16-month randomized controlled exercise trial on body weight and composition in young, overweight men and women: the Midwest Exercise Trial. Arch Intern Med. 2003;163(11):1343-1350. [DOI] [PubMed] [Google Scholar]
- 69. Johnson NA, Sachinwalla T, Walton DW, et al. Aerobic exercise training reduces hepatic and visceral lipids in obese individuals without weight loss. Hepatology. 2009;50(4):1105-1112. [DOI] [PubMed] [Google Scholar]
- 70. Sullivan S, Kirk EP, Mittendorfer B, Patterson BW, Klein S. Randomized trial of exercise effect on intrahepatic triglyceride content and lipid kinetics in nonalcoholic fatty liver disease. Hepatology. 2012;55(6):1738-1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Brouwers B, Hesselink MK, Schrauwen P, Schrauwen-Hinderling VB. Effects of exercise training on intrahepatic lipid content in humans. Diabetologia. 2016;59(10):2068-2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Brouwers B, Schrauwen-Hinderling VB, Jelenik T, et al. Exercise training reduces intrahepatic lipid content in people with and people without nonalcoholic fatty liver. Am J Physiol Endocrinol Metab. 2018;314(2):E165-E173. [DOI] [PubMed] [Google Scholar]
- 73. Devries MC, Samjoo IA, Hamadeh MJ, Tarnopolsky MA. Effect of endurance exercise on hepatic lipid content, enzymes, and adiposity in men and women. Obesity (Silver Spring). 2008;16(10):2281-2288. [DOI] [PubMed] [Google Scholar]
- 74. Slentz CA, Aiken LB, Houmard JA, et al. Inactivity, exercise, and visceral fat. STRRIDE: a randomized, controlled study of exercise intensity and amount. J Appl Physiol (1985). 2005;99(4):1613-1618. [DOI] [PubMed] [Google Scholar]
- 75. Kiens B. Skeletal muscle lipid metabolism in exercise and insulin resistance. Physiol Rev. 2006;86(1):205-243. [DOI] [PubMed] [Google Scholar]
- 76. Goodpaster BH, He J, Watkins S, Kelley DE. Skeletal muscle lipid content and insulin resistance: evidence for a paradox in endurance-trained athletes. J Clin Endocrinol Metab. 2001;86(12):5755-5761. [DOI] [PubMed] [Google Scholar]
- 77. van Loon LJ, Koopman R, Manders R, van der Weegen W, van Kranenburg GP, Keizer HA. Intramyocellular lipid content in type 2 diabetes patients compared with overweight sedentary men and highly trained endurance athletes. Am J Physiol Endocrinol Metab. 2004;287(3):E558-E565. [DOI] [PubMed] [Google Scholar]
- 78. Bruce CR, Thrush AB, Mertz VA, et al. Endurance training in obese humans improves glucose tolerance and mitochondrial fatty acid oxidation and alters muscle lipid content. Am J Physiol Endocrinol Metab. 2006;291(1):E99-E107. [DOI] [PubMed] [Google Scholar]
- 79. Bajpeyi S, Reed MA, Molskness S, et al. Effect of short-term exercise training on intramyocellular lipid content. Appl Physiol Nutr Metab. 2012;37(5):822-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Shepherd SO, Cocks M, Meikle PJ, et al. Lipid droplet remodelling and reduced muscle ceramides following sprint interval and moderate-intensity continuous exercise training in obese males. Int J Obes (Lond). 2017;41(12):1745-1754. [DOI] [PubMed] [Google Scholar]
- 81. Goodpaster BH, Theriault R, Watkins SC, Kelley DE. Intramuscular lipid content is increased in obesity and decreased by weight loss. Metabolism. 2000;49:467-472. [DOI] [PubMed] [Google Scholar]
- 82. Jensen MD, Haymond MW, Rizza RA, Cryer PE, Miles JM. Influence of body fat distribution on free fatty acid metabolism in obesity. J Clin Invest. 1989;83(4):1168-1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Erion DM, Shulman GI. Diacylglycerol-mediated insulin resistance. Nat Med. 2010;16(4):400-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Chavez JA, Summers SA. A ceramide-centric view of insulin resistance. Cell Metab. 2012;15(5):585-594. [DOI] [PubMed] [Google Scholar]
- 85. Koves TR, Ussher JR, Noland RC, et al. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab. 2008;7(1):45-56. [DOI] [PubMed] [Google Scholar]
- 86. Muoio DM, Noland RC, Kovalik JP, et al. Muscle-specific deletion of carnitine acetyltransferase compromises glucose tolerance and metabolic flexibility. Cell Metab. 2012;15(5):764-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Newsom SA, Brozinick JT, Kiseljak-Vassiliades K, et al. Skeletal muscle phosphatidylcholine and phosphatidylethanolamine are related to insulin sensitivity and respond to acute exercise in humans. J Appl Physiol (1985). 2016;120(11):1355-1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Lee S, Norheim F, Gulseth HL, et al. Skeletal muscle phosphatidylcholine and phosphatidylethanolamine respond to exercise and influence insulin sensitivity in men. Sci Rep. 2018;8(1):6531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Burgomaster KA, Howarth KR, Phillips SM, et al. Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. J Physiol. 2008;586(1):151-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Scribbans TD, Edgett BA, Vorobej K, et al. Fibre-specific responses to endurance and low volume high intensity interval training: striking similarities in acute and chronic adaptation. Plos One. 2014;9(6):e98119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Gillen JB, Martin BJ, MacInnis MJ, Skelly LE, Tarnopolsky MA, Gibala MJ. Twelve weeks of sprint interval training improves indices of cardiometabolic health similar to traditional endurance training despite a five-fold lower exercise volume and time commitment. Plos One. 2016;11(4):e0154075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. MacInnis MJ, Gibala MJ. Physiological adaptations to interval training and the role of exercise intensity. J Physiol. 2017;595(9):2915-2930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Gollnick PD, Piehl K, Saltin B. Selective glycogen depletion patterns in human skeletal muscle fibres after exercise of varying intensity and at varying pedalling rates. J Physiol. 1974;241:45-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Vøllestad NK, Blom PC. Effect of varying exercise intensity on glycogen depletion in human muscle fibres. Acta Physiol Scand. 1985;125(3):395-405. [DOI] [PubMed] [Google Scholar]
- 95. Wojtaszewski JF, MacDonald C, Nielsen JN, et al. Regulation of 5’AMP-activated protein kinase activity and substrate utilization in exercising human skeletal muscle. Am J Physiol Endocrinol Metab. 2003;284(4):E813-E822. [DOI] [PubMed] [Google Scholar]
- 96. Hansen AK, Fischer CP, Plomgaard P, Andersen JL, Saltin B, Pedersen BK. Skeletal muscle adaptation: training twice every second day vs. training once daily. J Appl Physiol (1985). 2005;98(1):93-99. [DOI] [PubMed] [Google Scholar]
- 97. Yeo WK, McGee SL, Carey AL, et al. Acute signalling responses to intense endurance training commenced with low or normal muscle glycogen. Exp Physiol. 2010;95(2):351-358. [DOI] [PubMed] [Google Scholar]
- 98. Hawley JA, Lundby C, Cotter JD, Burke LM. Maximizing cellular adaptation to endurance exercise in skeletal muscle. Cell Metab. 2018;27(5):962-976. [DOI] [PubMed] [Google Scholar]
- 99. Nana A, Slater GJ, Stewart AD, Burke LM. Methodology review: using dual-energy x-ray absorptiometry (DXA) for the assessment of body composition in athletes and active people. Int J Sports Nutr Exerc Metab. 2014;24:198-215. [DOI] [PubMed] [Google Scholar]
- 100. Malin SK, Gerber R, Chipkin SR, Braun B. Independent and combined effects of exercise training and metformin on insulin sensitivity in individuals with prediabetes. Diabetes Care. 2012;35(1):131-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Mikus CR, Boyle LJ, Borengasser SJ, et al. Simvastatin impairs exercise training adaptations. J Am Coll Cardiol. 2013;62(8):709-714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Newman AA, Grimm NC, Wilburn JR, et al. Influence of sodium glucose cotransporter 2 inhibition on physiological adaptation to endurance exercise training. J Clin Endocrinol Metab. 2019;104(6):1953-1966. [DOI] [PubMed] [Google Scholar]
- 103. Konopka AR, Laurin JL, Schoenberg HM, et al. Metformin inhibits mitochondrial adaptations to aerobic exercise training in older adults. Aging Cell. 2019;18(1):e12880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Koh HE, Ørtenblad N, Winding KM, Hellsten Y, Mortensen SP, Nielsen J. High-intensity interval, but not endurance, training induces muscle fiber type-specific subsarcolemmal lipid droplet size reduction in type 2 diabetic patients. Am J Physiol Endocrinol Metab. 2018;315(5):E872-E884. [DOI] [PubMed] [Google Scholar]
- 105. Pino MF, Stephens NA, Eroshkin AM, et al. Endurance training remodels skeletal muscle phospholipid composition and increases intrinsic mitochondrial respiration in men with type 2 diabetes. Physiol Genomics. 2019;51:586-595. [DOI] [PubMed] [Google Scholar]