Abstract
Evidently, the emergence of novel coronavirus disease (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) has rapidly blowout across the world. Since, the presence of coronaviruses, including SARS-CoV-2 in the fecal specimens and anal swabs of some infected patients, has raised emerging concern with the likelihood of fecal-based spread must be inspected and clarified. Therefore, herein, an effort has been made to spotlight the current scenarios and possible solutions to better understand the risks associated with the wastewater matrices as a potential source of SARS-CoV-2 transmission in the environment. The information reviewed here constitutes a paramount intellectual basis to sustenance ongoing research to tackle the SARS-CoV-2 issue. Thus, this overview indicates the most accessible frontiers related to the detection, quantification, and possible transmission of SARS-CoV-2 in the environment through water routes. The regulatory authorities and policymakers must assure the society via dissemination of evidence-based guidelines that the water matrices, including groundwater and drinking water resources are safe. Finally, we have identified and enlisted a number of pressing questions concerning the ongoing SARS-CoV-2 transmission or COVID-19 emergence issue that must be carefully answered to put further and deeper insight into SARS-CoV-2/COVID-19 in future studies.
Keywords: Water matrices, SARS-CoV-2, Transmission, Detection, Quantification, Environmental aspects
1. Introduction
To date, there is no evidence to suggest wastewater as a potential source for the transmission of SARS-CoV-2. Though some reports have prophesied wastewater as a poor risk of SARS-CoV-2 transmission, intensive research efforts are needed to corroborate these predictions. Virus-laden bio-aerosols from a drainage sewage pipe at Amoy Gardens complex in Hong Kong has been recognized as the transmission mode for coronaviruses during the outbreak of SARS in 2003 [1]. The virus can also find its way into the drinking water distribution infrastructure and might enter individual homes. The occurrence of SARS-CoV-2 may undesirably affect the water supply chain, which can compromise the integrity of water quality and human health. Therefore, the formation of aerosol during the wastewater treatment should be prudently inspected as a possible source of virus spread. Some evidence suggests the fecal-oral transmission of SARS-CoV-2. Besides, it is also essential to examine the adverse impacts of SARS-CoV-2-laden wastewater on soil and aquatic creatures. Along with the effective wastewater treatment, timely monitoring and proper control measures are required to limit the spread of SARS-CoV-2. Thus, robust analytical tools are required for cost-effective, sensitive, selective and multi-residue analysis [2].
2. Favorable conditions for SARS-CoV-2 in wastewater
Various earlier reports have demonstrated that the survival and persistence of SARS-CoV-2 in wastewater profoundly depends on the wastewater characteristics [3,4]. It is described that surrogate coronaviruses remain contagious in sewage and water for a few days to weeks [5]. In a recent investigation, the half-life of SARS-CoV-2 in wastewater has been estimated to be between 4.8 and 7.2 h [6]. Whereas, Barcelo [7] reported that the SARS-CoV-2 could persist in wastewater from hours to days. Therefore, it remains profoundly meaningful to apprehend the stability, fate, and decay mechanism of SARS-CoV-2 in water and wastewater. Influential parameters that can envisage the reduction kinetics should be assessed for establishing favorable and unfavorable conditions for SARS-CoV-2 survival in sewage. In order to evaluate the potential acquaintance risks of virus-polluted water, it is crucial to investigate the detailed physical and biological characteristics of various wastewaters. Fig. 1 shows Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) cross-transmission via building sanitary plumbing systems to wastewater sewage [8]. In an earlier study, Gundy et al. [9] reports the survival of coronaviruses in water and wastewater. The results obtained indicate that coronaviruses are much more sensitive to temperature than Poliovirus 1 LSc-2ab (PV-1) and that there is a considerable difference in survivability between PV-1 and the coronaviruses in wastewater.
Fig. 1.
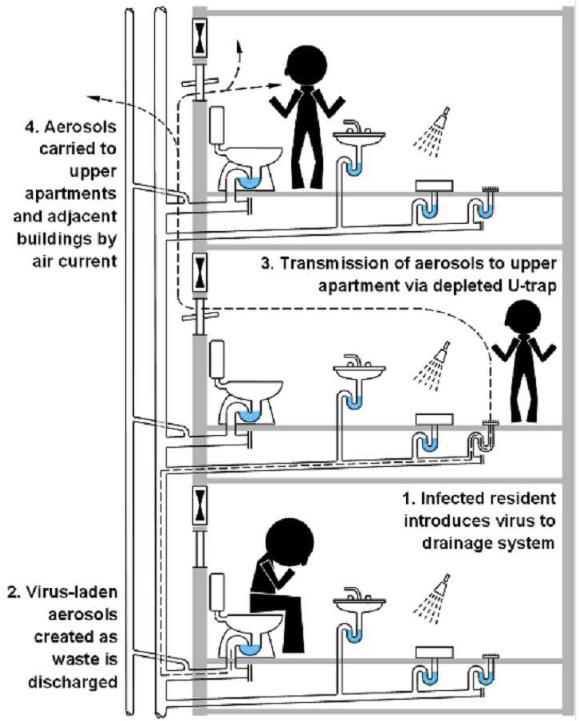
Shows Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) cross-transmission via building sanitary plumbing systems. Reprinted from Ref. [8] “Gormley, M., Aspray, T. J., Kelly, D. A., & Rodriguez-Gil, C. (2017). Pathogen cross-transmission via building sanitary plumbing systems in a full scale pilot test-rig. PloS One, 12(2), e0171556”, with permission under the terms of the Creative Commons Attribution License.
3. Detection strategies – General and biological perspective
Nevertheless, important issues remain, i.e., which pathogen-associated factors are responsible for the amplification effects? What cultural factors are different or have SARS and Middle East Respiratory Syndrome (MERS) changed? What metropolitan areas will Ro > 1 sustain and what are the drivers of this transmission rate? There are two types of factors and many methods before these questions are addressed [10].
The interaction factors between pathogen and hosts include the time of viral emergence, viral emergence (number of infectious particles releases), viral persistence (environment), and viral shedding (super propagators) heterogeneity. However, changes in the viral genome will alter the cumulative distribution of those factors over time because human adaptation is underway. Combined factors based on society include people by location (densities), everyday transport (housing and workplace structure), connections (more significant opportunities for transportation), emerging activity trends (urbanization and increased mobility), etc. Therapy (antivirals and antibodies) and vaccinations of the future. The latest studies have shown that COVID-19 has a normal or even “preclinical but communicable” period of viral dissemination and infection spread. Such features are known for humans and most other viral pathogens but not for SARS and MERS coronaviruses. Immunocompromised or semi-symptomatic individuals may also transmit SARS-CoV-2 [11]. In a recent study, Ahmed et al. [12] reported a comparison of virus concentration methods for the RT-qPCR-based recovery of murine hepatitis virus, a surrogate for SARS-CoV-2 from untreated wastewater.
Unique predictive equations for epidemiological outbreaks are being used to predict Ro, but pathogen-based variables cannot be determined. These forecasts include clinical results and the epidemiology of “shoe leather”. Population-related statistics should be inferred from current demographics, travel, and telecommunication estimates. Health authorities in China have already started to provide some of the necessary information with time-based mobile phone movements across geospatial regions. However, due to privacy and protection concerns, collection authorities, this data may not be shared in other countries – except in public health crises or emergencies.
In published articles, mathematical models which provide COVID-19 cases in the real-time forecast have begun to appear in the literature [13,14]. But even comprehensive mathematical models, involving complex pathogenic and social variables, can take considerable time and effort (often months or even years) to construct and validate. We can also use current mathematical models for recent influenza pandemics or outbreaks of SARS and MERS, including those produced in the United States. National Research Institute for Infectious Disease Systems. These differential models are responsible for differences in pathogenic, financial, and intervention variables. The effectiveness of the prediction of COVID-19 distribution will depend on the accuracy of transmission models and data [13].
We assume that research activities involve above and all other important variables identifying the values (and ranges). Information on these factors can also be spread through research and response and adaptation organizations, for example, the Red Cross, other NGOs, and agencies for emergency management. The most successful way to communicate these different statistics is to create a database for the co-ordination of information by pathogen-host, social mixing, and intervention modules. Such a bridge links all existing database networks. Moreover, such a bank may use digital software to find, arrange, and analyze data for eventual cure and relation. Several statistical simulation groups independently function in the prediction of the distribution of COVID-19 infections throughout China, the US, and Europe. We believe that priority should be aligned and supported by government agencies between these groups.
Several clinical trials are currently underway to identify treatments for COVID-19. Sadly, no medical vaccines or antiviral medications are officially approved on the medical front for the prevention of coronavirus infections [15]. The only therapeutic option is supportive treatment, including hospitalization and the operation of intensive care units. Besides, the risk of SARS-CoV-2 pneumonia leading to fatal secondary bacterial infections, including influenza, must be taken immediately into consideration. Fortunately, action can be taken in the area of public health to safeguard large populations, including travel prohibitions, quarantine, and isolation from contact/cases. However, the best intervention will require an understanding of the main factors driving outbreaks of COVID-19 and a monitoring of how the causes change over time and place [[16], [17], [18]]. The most concerned questions about the transmission, detection, and prevention of SARS-CoV-2 are summarized in Table 1 [17].
Table 1.
The most concerned questions about the transmission, detection, and prevention of SARS-CoV-2 [17].
| No. | The most concerned questions |
|---|---|
| 1. | How much do we know about the human-to-human transmission of SARS-CoV-2? |
| 2. | How much do we know about the water-based transmission of SARS-CoV-2? |
| 3. | Does the SARS-CoV-2 appear to be significantly contagious in a human-to-human context? |
| 4. | What makes SARS-CoV-2 strain significantly concerning, regardless of its resembling symptoms from the common cold to as severe as SARS-CoV? |
| 5. | How concerned should we be about the SARS-CoV-2 origin, although there are more confirmed cases around the globe and the infected cases are keep growing? |
| 6. | What are the main symptoms of SARS-CoV-2, and how are they distinguishable compared to the typical common cold and seasonal flu? |
| 7. | What do people need to know to take preventive measures to protect themselves and avoid getting sick? |
| 8. | Are the currently available viral vaccine development approaches good enough to tackle SARS-CoV-2, effectively? |
4. Detection and quantification of SARS-CoV-2 in wastewater
The identification and quantification of SARS-CoV-2 in sewage and wastewater is a challenging task, but it is important to track these emerging infectious diseases in a timely and effective manner. Many recent studies have reported that the novel SARS-CoV-2 in human stool and urban wastewater has been successfully detected [[19], [20], [21], [22]]. Nonetheless, all of the above studies are incomplete and several additional studies covering a large number of populations are required. Multidisciplinary research methodologies in this area could be successful in developing more efficient techniques for SARS-CoV-2 detection and quantification in water. Due to the shorter half-limit of the viable SARS-CoV-2 in wastewater, the detection strategy should be equally valid for both sustainable and non-viable virus particles. It is also shown that virus structure and assembly can be degraded into other items, so developing techniques capable of using degraded materials for the precise detection and quantitation of coronavirus is of great importance [23]. Based on significant advances in microbiology, a range of novel detection strategies techniques were proposed for robust identification and quantification of viral RNA in the scientific literature [24,25]. The development of innovative biosensor-based nanostructured materials has been found to promise waterborne pathogens in water samples [26].
5. Uneven consumption of disinfectants - assessment of adverse impacts and alternative solutions
One of the main environmental dilemmas of COVID-19 is the inappropriate use of disinfectants released to the sewage system. Careful monitoring of wastewater for possible contamination is, therefore, necessary to restrict the spread of SARS-CoV-2. In a recent report, Zhang et al. [19] revealed that 2000 tons of disinfectants are released merely in Wuhan city, which not only postures a potential impact to the aquatic system but can also contaminate natural resources of drinking water. Similarly, the presence of pharmaceutically active residues in wastewater may also influence human health and marine organisms. It is significant to evaluate the negative impacts of these discharges and develop newer and robust techniques for the proper treatment and safe disposal of wastewaters. Furthermore, multidisciplinary approaches are required for the development of environmentally friendly and more sustainable technologies to eliminate SARS-CoV-2 from water and other sources.
6. The hypothetical fate of the SARS-CoV-2 virus in the urban water cycle
The fate of the urban water cycle SARS-CoV-2 virus and its related possible health threats raise a great many concerns for environmental academics, especially the water science group. The existence and maintenance of the viability of coronaviruses in hospitals and wastewater from fecal emancipation of infected patients have been demonstrated in earlier reports [1,27,28]. Studies indicating coronavirus persistence in wastewater plants and aquatic matrices have also confirmed greater attention to this serious problem [5,29]. The SARS-CoV-2 virus may therefore still exist in wastewater, but it must be recognized and concentrated. Therefore, there is also the question of how long coronavirus can survive and remain contagious after wastewater discharge. Following the 2003 SARS epidemic, some studies have identified viral particulates in the household or sewage wastewater that, in the absence of suitable disinfection, are likely to survive at some level, thereby increasing the potential for infection [1,3,5,[30], [31], [32]]. The survival and persistence of coronaviruses in water systems depend however upon various factors, such as light familiarity (UV or solar inactivation), temperature (high-temperature coronaviruses are susceptible to), organic substance, and the occurrence of competitor microorganisms. Adequate monitoring program must, therefore, be developed during treatment of wastewater, to evaluate the destination of the urban water cycle.
Declaration of competing interest
The listed author(s) declare that no conflicting interests exist in this work.
Acknowledgments
The listed author(s) appreciatively acknowledge the literature services provided by representative universities.
References
- 1.Hung L.S. The SARS epidemic in Hong Kong: what lessons have we learned? J. R. Soc. Med. 2003;96(8):374–378. doi: 10.1258/jrsm.96.8.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sims N., Kasprzyk-Hordern B. Future perspectives of wastewater-based epidemiology: monitoring infectious disease spread and resistance to the community level. Environ. Int. 2020;139 doi: 10.1016/j.envint.2020.105689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ye Y., Ellenberg R.M., Graham K.E., Wigginton K.R. Survivability, partitioning, and recovery of enveloped viruses in untreated municipal wastewater. Environ. Sci. Technol. 2016;50(10):5077–5085. doi: 10.1021/acs.est.6b00876. [DOI] [PubMed] [Google Scholar]
- 4.Annalaura C., Ileana F., Dasheng L., Marco V. Making waves: coronavirus detection, presence and persistence in the water environment: state of the art and knowledge needs for public health. Water Res. 2020;179 doi: 10.1016/j.watres.2020.115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casanova L., Rutala W.A., Weber D.J., Sobsey M.D. Survival of surrogate coronaviruses in water. Water Res. 2009;43(7):1893–1898. doi: 10.1016/j.watres.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hart O.E., Halden R.U. Computational analysis of SARS-CoV-2/COVID-19 surveillance by wastewater-based epidemiology locally and globally: feasibility, economy, opportunities and challenges. Sci. Total Environ. 2020;730 doi: 10.1016/j.scitotenv.2020.138875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barcelo D. An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J. Environ. Chem. Eng. 2020;8 doi: 10.1016/j.jece.2020.104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gormley M., Aspray T.J., Kelly D.A., Rodriguez-Gil C. Pathogen cross-transmission via building sanitary plumbing systems in a full scale pilot test-rig. PloS One. 2017;12(2) doi: 10.1371/journal.pone.0171556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gundy P.M., Gerba C.P., Pepper I.L. Survival of coronaviruses in water and wastewater. Food Environ. Virol. 2009;1(1):10. [Google Scholar]
- 10.Manderson L., Levine S. COVID-19, risk, fear, and fall-out. Med. Anthropol., Cross Cult. Stud. Health Illness. 2020;39:367–370. doi: 10.1080/01459740.2020.1746301. [DOI] [PubMed] [Google Scholar]
- 11.Ferretti L., Wymant C., Kendall M., Zhao L., Nurtay A., Abeler-Dörner L.…Fraser C. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020;368(6491) doi: 10.1126/science.abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed W., Bertsch P., Bivins A., Bibby K., Farkas K., Gathercole A.…Mueller J. Comparison of virus concentration methods for the RT-qPCR-based recovery of murine hepatitis virus, a surrogate for SARS-CoV-2 from untreated wastewater. Sci. Total Environ. 2020;739 doi: 10.1016/j.scitotenv.2020.139960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siddiqui M.K., Morales-Menendez R., Gupta P.K., Iqbal H.M., Hussain F., Khatoon K., Ahmad S. Correlation between temperature and COVID-19 (suspected, confirmed and death) cases based on machine learning analysis. J. Pure Appl. Microbiol. 2020;14:1017–1024. [Google Scholar]
- 14.Panwar H., Gupta P.K., Siddiqui M.K., Morales-Menendez R., Singh V. Application of deep learning for fast detection of COVID-19 in X-rays using nCOVnet. Chaos, Solit. Fractals. 2020;138 doi: 10.1016/j.chaos.2020.109944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao J., Tian Z., Yang X. Breakthrough: chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci. Trends. 2020;14:72–73. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 16.Cortegiani A., Ingoglia G., Ippolito M., Giarratano A., Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J. Crit. Care. 2020;57:279–283. doi: 10.1016/j.jcrc.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bilal M., Nazir M.S., Parra-Saldivar R., Iqbal H.M. 2019-nCoV/COVID-19 - approaches to viral vaccine development and preventive measures. J. Pure Appl. Microbiol. 2020;14(1):25–29. Article: 6168. [Google Scholar]
- 18.Iqbal H.M., Romero-Castillo K.D., Bilal M., Parra-Saldivar R. The emergence of novel-coronavirus and its replication cycle-an overview. J. Pure Appl. Microbiol. 2020;14(1):13–16. Article: 6146. [Google Scholar]
- 19.Zhang H., Tang W., Chen Y., Yin W. Disinfection threatens aquatic ecosystems. Science. 2020;368:146–147. doi: 10.1126/science.abb8905. [DOI] [PubMed] [Google Scholar]
- 20.Lodder W., de Roda Husman A.M. SARS-CoV-2 in wastewater: potential health risk, but also data source. Lancet Gastroenterol. Hepatol. 2020 doi: 10.1016/S2468-1253(20)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed W., Angel N., Edson J., Bibby K., Bivins A., O’Brien J.W., Choi P.M., Kitajima M., Simpson S.L., Li J., Tscharke B., Verhagen R., Smith W.J.M., Zaugg J., Dierens L., Hugenholtz P., Thomas K.V., Mueller J.F. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang A., Tong Z., Wang H., Dai Y., Li K., Liu J., Wu W., Yuan C., Yu M., Li P., Yan J. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg. Infect. Dis. J. 2020;26 doi: 10.3201/eid2606.200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daughton C. The international imperative to rapidly and inexpensively monitor community-wide Covid-19 infection status and trends. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rong Z., Wang Q., Sun N., Jia X., Wang K., Xiao R., Wang S. Smartphone-based fluorescent lateral flow immunoassay platform for highly sensitive point-of-care detection of Zika virus nonstructural protein 1. Anal. Chim. Acta. 2019;1055:140–147. doi: 10.1016/j.aca.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 25.Gunnarsdottir M.J., Gardarsson S.M., Figueras M.J., Puigdomènech C., Juárez R., Saucedo G., Arnedo M.J., Santos R., Monteiro S., Avery L., Pagaling E., Allan R., Abel C., Eglitis J., Hambsch B., Hügler M., Rajkovic A., Smigic N., Udovicki B., Albrechtsen H.-J., López-Avilés A., Hunter P. Water safety plan enhancements with improved drinking water quality detection techniques. Sci. Total Environ. 2020;698 doi: 10.1016/j.scitotenv.2019.134185. [DOI] [PubMed] [Google Scholar]
- 26.Bhardwaj N., Bhardwaj S.K., Bhatt D., Lim D.K., Kim K.-H., Deep A. Optical detection of waterborne pathogens using nanomaterials. Trac. Trends Anal. Chem. 2019;113:280–300. [Google Scholar]
- 27.Leung W.K., To K.F., Chan P.K., Chan H.L., Wu A.K., Lee N.…Sung J.J. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology. 2003;125(4):1011–1017. doi: 10.1016/j.gastro.2003.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amirian E.S. Potential fecal transmission of SARS-CoV-2: current evidence and implications for public health. Int. J. Infect. Dis. 2020;95:363–370. doi: 10.1016/j.ijid.2020.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fong T.T., Lipp E.K. Enteric viruses of humans and animals in aquatic environments: health risks, detection, and potential water quality assessment tools. Microbiol. Mol. Biol. Rev. 2005;69(2):357–371. doi: 10.1128/MMBR.69.2.357-371.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Poon L.L., Chan K.H., Wong O.K., Cheung T.K., Ng I., Zheng B.…Peiris J.S. Detection of SARS coronavirus in patients with severe acute respiratory syndrome by conventional and real-time quantitative reverse transcription-PCR assays. Clin. Chem. 2004;50(1):67–72. doi: 10.1373/clinchem.2003.023663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wigginton K.R., Ye Y., Ellenberg R.M. Emerging investigators series: the source and fate of pandemic viruses in the urban water cycle. Environ. Sci.: Water Res. Technol. 2015;1(6):735–746. [Google Scholar]
- 32.Choudri B.S., Charabi Y. Health effects associated with wastewater treatment, reuse, and disposal. Water Environ. Res. 2019;91(10):976–983. doi: 10.1002/wer.1157. [DOI] [PubMed] [Google Scholar]


