Abstract
Background
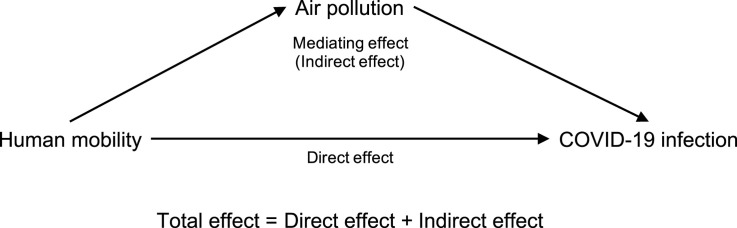
Previous studies have found that human mobility restrictions could not only prevent the spread of COVID-19, but also improve the air quality because of the reduction of industrial production, transportation and traffic. It is noteworthy that air quality is also closely related to the risk of COVID-19 infection. Therefore, we aimed to assess the mediating role of air quality on the association between human mobility and the infection caused by this novel coronavirus.
Methods
We collected daily confirmed cases, human mobility data, air quality data and meteorological variables in 120 cities from China between January 23, 2020 and February 29, 2020. We applied the generalized additive model to examine the association of human mobility index with COVID-19 confirmed cases, and to assess the mediating effects of air quality index and each pollutant.
Results
We observed a significant positive relationship between human mobility index and the daily counts of COVID-19 confirmed cases. A unit increase in human mobility index (lag0–14) was associated with a 6.45% increase in daily COVID-19 confirmed cases, and air quality index significantly mediated 19.47% of this association. We also observed a positive relationship between human mobility index and air quality index. In the pollutant level analyses, we found significant mediating effects of PM2.5, PM10, and NO2.
Conclusions
Our study suggests that limiting human movements could reduce COVID-19 cases by improving air quality besides decreasing social contact.
Keywords: Mediating effect, Air quality, Human mobility, Novel coronavirus pneumonia, COVID-19
Graphical abstract
Highlights
-
•
There was a positive relationship between human mobility and COVID-19 infection.
-
•
Human mobility was positively associated with the air quality index.
-
•
Air quality index partially mediated the association of human mobility with COVID-19 infection.
-
•
We also observed the significant mediating effects of PM2.5, PM10, and NO2.
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), continues to spread rapidly around the world (Chen et al., 2020a; Dong et al., 2020; Gilbert et al., 2020; Zhou et al., 2020). As of 28 May 2020, data from the World Health Organization have shown that more than 5,596,550 confirmed cases have been detected and 353,373 confirmed deaths worldwide. Most infected patients only have mild symptoms such as fever and dry cough, while some patients have fatal complications like Acute Respiratory Distress Syndrome (ARDS) (Chen et al., 2020c; Huang et al., 2020a; Sohrabi et al., 2020). Thus, exploring risk factors affecting the transmission of SARS-CoV-2 is a meaningful study.
Early studies have shown that human mobility plays an important role in the dispersal of infection since SARS-CoV-2 could spread by human-to-human transmission via direct contact or droplets (Chan et al., 2020; Kraemer et al., 2020; Li et al., 2020; Tian et al., 2020). Therefore, to make people stay at home and decrease social contact, various public health interventions have been implemented in many countries, such as prohibiting travel in and out of cities, banning mass gatherings, and closing schools and entertainment venues (Bayham and Fenichel, 2020; Chen et al., 2020d; Chinazzi et al., 2020). An empirical study found that the lockdown of Wuhan city on 23 January 2020 reduced outflows from Wuhan by 56.35%, inflow into Wuhan by 76.64%, and within-Wuhan movements by 54.15% (Fang et al., 2020).
It is noteworthy that human mobility restrictions could not only prevent the spread of COVID-19, but also improve the air quality because of the reduction of industrial production, transportation and traffic (Kerimray et al., 2020; Mahato et al., 2020; Nakada and Urban, 2020; Tobías et al., 2020). According to a study using data from 44 cities in China, the air quality index (AQI) decreased by 7.80% on average due to the implementation of travel restrictions (Bao and Zhang, 2020). Importantly, air quality is also closely related to the risk of COVID-19 infection, since air pollutants could affect body's immunity and carry virus (Bianconi et al.; Fattorini and Regoli, 2020; van Doremalen et al., 2020; Zhu et al., 2020). So, it is reasonable to hypothesize that air quality could partially mediate the association of human mobility with COVID-19 infection.
In this study, we aimed to investigate the relationship between human mobility and COVID-19 infection, and to assess the mediating role of air quality on this association, based on data from 120 cities in China.
2. Materials and methods
2.1. Study area
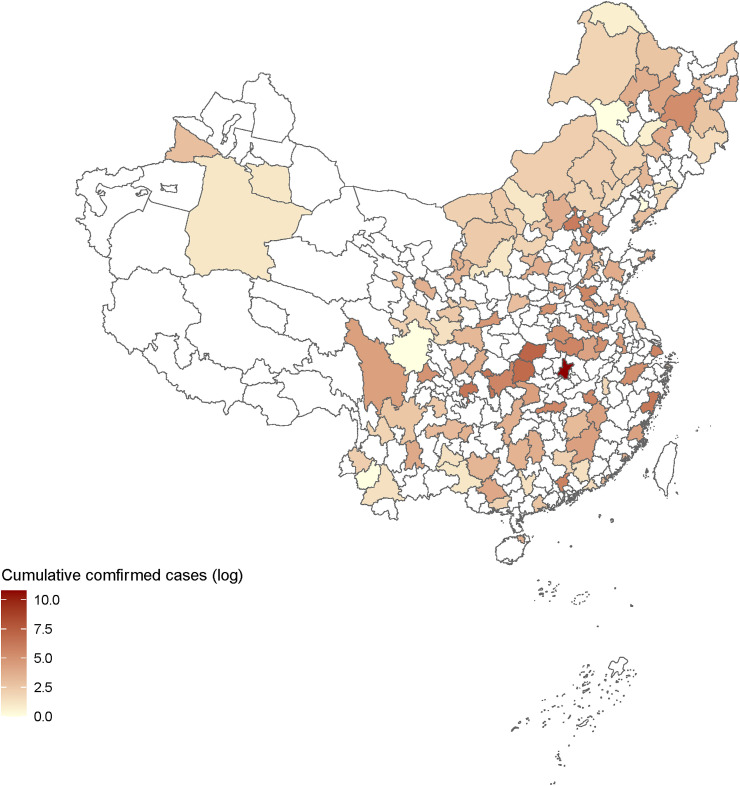
116 prefecture-level cities and 4 municipalities were included in this study, covering the majority of Chinese mainland (83.4°–131.6° east longitude, and 20.0°–51.4° north latitude). Fig. 1 plots the locations of these 120 cities and the cumulative COVID-19 confirmed cases in each city during our study period (i.e., January 23, 2020 to February 29, 2020). We focused our study on these cities because the air pollution data and the meteorological data were limited.
Fig. 1.
Locations of all 120 cities in our analyses and cumulative COVID-19 confirmed cases (log) in each city during our study period (i.e., January 23, 2020 to February 29, 2020).
2.2. Data collection
We collected daily confirmed new cases for each city between January 23, 2020 (i.e., the date of Wuhan lockdown) and February 29, 2020 from the official websites of local health commissions.
Human mobility was measured by the real-time intracity migration index calculated from the ratio of the number of people traveling in a city to the number of people living in that city (Bao and Zhang, 2020). Human mobility index data were obtained from the Baidu Qianxi online platform (http://qianxi.baidu.com), which tracked human movements by mobile phone data from Baidu location-based services.
Daily air quality data including air quality index (AQI), PM2.5, PM10, NO2, O3, SO2, and CO for each city were collected from an air quality monitor platform (https://www.aqistudy.cn/historydata/). The AQI is calculated by two steps, which could describe the level of air quality (larger AQI means more serious air pollution). The first step is to calculate the individual air quality index (IAQI) values for six pollutants (PM2.5, PM10, NO2, O3, SO2, and CO), and the second step is to choose the maximum of the six IAQI values as the AQI (Zhong, S., et al., 2019).
We obtained daily meteorological data on mean temperature, relative humidity, atmospheric pressure, and wind speed from the National Meteorological Information Center (http://data.cma.cn). We downloaded the dataset of daily climate data from Chinese surface stations for global exchange (http://data.cma.cn/data/cdcdetail/dataCode/SURF_CLI_CHN_MUL_DAY_CES_V3.0.html) on this platform. The surface stations could be matched with cities by the station number.
2.3. Statistical analysis
Our statistical analysis included two parts. In the first part, we applied the generalized additive model (GAM) with a Gaussian distribution family to assess the association of human mobility index with daily COVID-19 confirmed cases (Hastie, 2017; Liu et al., 2020a; Xie and Zhu, 2020; Zhu et al., 2020). Since the incubation period of COVID-19 is estimated to range from 1 to 14 days and there is also a delay (mean: 4.95 days) between the onset of illness and being confirmed according to the National Health Commission in China (National Health Commission of the PRC, 2020a, 2020b), a moving-average approach was used to capture the moving average lag effect (lag0–7, lag0–14, lag0–21) of human mobility index on daily confirmed cases of COVID-19 (Duan et al., 2019; Li et al., 2018; Zhu et al., 2020). Our model was defined as follows:
| (1) |
Here, log(Y it ) indicates the logarithm of the number of confirmed new cases in city i on day t (plus 1 to avoid taking the logarithm of 0). α is the intercept. HMI il denotes the (l+1)-day moving average of human mobility index (lag0–l) in city i. We controlled for meteorological variables (M il) including mean temperature, relative humidity, atmospheric pressure, and wind speed during the same period according to previous studies, using s(∙) (the thin plate spline function with the 3 degrees of freedom) to account for non-linear effect (Xie and Zhu, 2020; Zhu et al., 2020). We also controlled the logarithm of the number of confirmed new cases in city i on day t–1 to account for potential serial correlation (Liu et al., 2020a). Time-invariant city characteristics such as population size were controlled by including city fixed effect (city i), and unobserved factors affecting all cities in each day such as Spring Festival were controlled by including day fixed effect (day t) (Amuakwa-Mensah et al., 2017; Lu and Lu, 2017).
In the second part, we conducted the mediation analysis to test our hypothesis that air quality could partially mediate the association of human mobility with COVID-19 infection. That is, human mobility is not only directly associated with COVID-19 infection, but also indirectly related to COVID-19 infection through air quality. According to previous studies (Baron and Kenny, 1986; Chen et al., 2020b), Equation (2) an Equation (3) were constructed:
| (2) |
| (3) |
Here, AQI il denotes the (l+1)-day moving average of air quality index (lag0–l) in city i. Therefore, the three Equations (1), (2), (3) constituted a complete mediation test based on three steps: the first step is to test whether the coefficient β in Equation (1) is statistically significant; the second step is to test whether the coefficient γ in Equation (2) is statistically significant; the third step is to test whether the coefficients δ and θ in Equation (3) were statistically significant. If β, γ, δ and θ are all significant, and the indirect effect (γ × θ) has the same sign as the direct effect (δ), our hypothesis is supported. The proportion of the association between human mobility and COVID-19 infection mediated was calculated by Equation (4) (Huang et al., 2020b; Liu et al., 2020b; Yin et al., 2018):
| (4) |
Specifically, the suppressing effect occurs when the indirect effect has the opposite sign of the direct effect (Shrout, P. E., Bolger, N., 2002). Including a suppressor in Equation (3) could make the direct effect greater in magnitude than the total effect (β) (Rucker, D. D., et al., 2011). Additionally, we also conducted the pollutant level analyses to examine the mediating effect of each pollutant by the same method.
In the sensitivity analysis, we excluded Wuhan city from our data to examine the robustness of our results because the number of confirmed cases in Wuhan was much larger than that in others. The “mgcv” package (version 1.8–31) in R software (version 4.0.0) was used to conduct the GAM in this study.
3. Results
3.1. Descriptive analysis
During the study period, our analysis included over 58,000 confirmed cases, covering 70% of confirmed cases in China. Table 1 presents the descriptive statistics of daily confirmed new cases, human mobility index, air quality index, air pollutants, and meteorological variables. The average of daily COVID-19 confirmed cases, human mobility index, and air quality index were 12.94, 2.74, and 70.72, respectively. Average daily concentrations of PM2.5, PM10, NO2, O3, SO2, and CO were 46.43 μg/m3, 62.97 μg/m3, 19.28 μg/m3, 78.22 μg/m3, 12.23 μg/m3 and 0.85 mg/m3, respectively. Average daily mean temperature, relative humidity, atmospheric pressure, and wind speed were 2.82 °C, 67.25%, 964.08 hPa, and 2.11 m/s, respectively.
Table 1.
Descriptive statistics of daily confirmed new cases, human mobility index, air quality index, air pollutants and meteorological variables across all cities and days.
| Mean (SD) | Min | Max | |
|---|---|---|---|
| Daily confirmed cases | 12.94 (228.96) | 0 | 13,436 |
| Human mobility index | 2.74 (1.08) | 0.57 | 8.88 |
| Air quality index | 70.72 (45.34) | 13 | 500 |
| PM2.5 (μg/m3) | 46.43 (38.55) | 2 | 554 |
| PM10 (μg/m3) | 62.97 (49.76) | 4 | 632 |
| NO2 (μg/m3) | 19.28 (11.87) | 2 | 86 |
| O3 (μg/m3) | 78.22 (20.58) | 11 | 152 |
| SO2 (μg/m3) | 12.23 (9.90) | 2 | 87 |
| CO (mg/m3) | 0.85 (0.47) | 0.1 | 7.4 |
| Mean temperature (°C) | 2.82 (10.11) | −33.8 | 26.5 |
| Relative humidity (%) | 67.25 (17.42) | 17 | 100 |
| Atmospheric pressure (hPa) | 964.08 (76.15) | 668.1 | 1039 |
| Wind speed (m/s) | 2.11 (1.19) | 0 | 15.4 |
Table 2 shows the spearman correlation coefficients between human mobility index, air quality index, air pollutants, and meteorological variables. Human mobility index was positively correlated with air quality index (r = 0.05, p < 0.05), PM2.5 (r = 0.06, p < 0.05), PM10 (r = 0.08, p < 0.05), NO2 (r = 0.05, p < 0.05), CO (r = 0.04, p < 0.05), mean temperature (r = 0.18, p < 0.05) and relative humidity (r = 0.07, p < 0.05), while had negative correlations with O3 (r = −0.04, p < 0.05), SO2 (r = −0.03, p > 0.05), atmospheric pressure (r = −0.10, p < 0.05) and wind speed (r = −0.05, p < 0.05).
Table 2.
Spearman correlation coefficients between human mobility index, air quality index, air pollutants, and meteorological variables across all cities and days.
| Human mobility index | Air quality index | PM2.5 | PM10 | NO2 | O3 | SO2 | CO | Mean temperature | Relative humidity | Atmospheric pressure | Wind speed | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Human mobility index | 1.00 | |||||||||||
| Air quality index | 0.05* | 1.00 | ||||||||||
| PM2.5 | 0.06* | 0.92* | 1.00 | |||||||||
| PM10 | 0.08* | 0.93* | 0.91* | 1.00 | ||||||||
| NO2 | 0.05* | 0.60* | 0.64* | 0.65* | 1.00 | |||||||
| O3 | −0.04* | 0.29* | 0.13* | 0.19* | 0.08* | 1.00 | ||||||
| SO2 | −0.03 | 0.37* | 0.37* | 0.45* | 0.52* | 0.11* | 1.00 | |||||
| CO | 0.04* | 0.60* | 0.69* | 0.62* | 0.63* | −0.04* | 0.39* | 1.00 | ||||
| Mean temperature | 0.18* | −0.11* | −0.13* | −0.17* | −0.18* | 0.08* | −0.52* | −0.09* | 1.00 | |||
| Relative humidity | 0.07* | −0.06* | 0.08* | −0.08* | −0.07* | −0.40* | −0.41* | 0.12* | 0.34* | 1.00 | ||
| Atmospheric pressure | −0.10* | 0.03 | 0.07* | 0.02 | 0.04* | −0.04* | −0.21* | −0.04* | 0.15* | 0.27* | 1.00 | |
| Wind speed | −0.05* | −0.15* | −0.21* | −0.13* | −0.22* | 0.04* | −0.03 | −0.22* | −0.07* | −0.13* | 0.12* | 1.00 |
*p < 0.05.
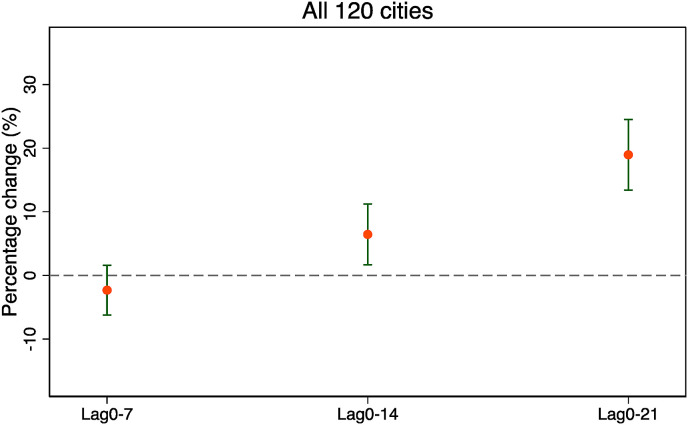
3.2. Relationship between human mobility index and COVID-19 confirmed cases
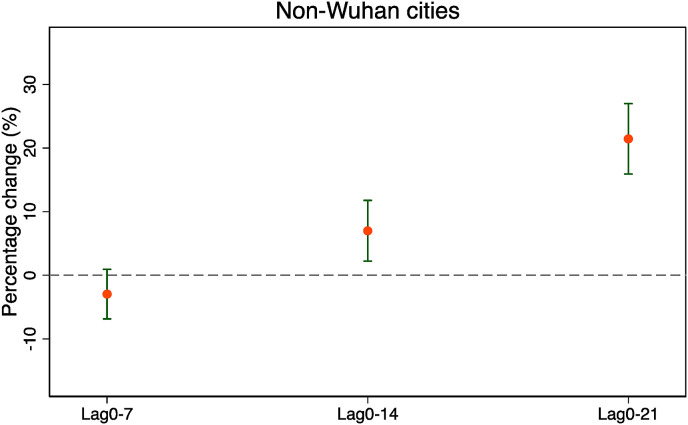
Fig. 2 shows the moving average lag effects (lag0–7, lag0–14, lag0–21) of human mobility on confirmed cases of COVID-19 using Equation (1). We observed significant positive relationships between human mobility index and the daily counts of COVID-19 confirmed cases at lag0–14 and lag0–21. A unit increase in human mobility index was associated with a 6.45% (95% CI: 1.66 to 11.23) increase in daily COVID-19 confirmed cases at lag0–14, and a 18.95% (95% CI: 13.41 to 24.50) increase in confirmed cases at lag0–21. In the sensitivity analysis, the relationship between COVID-19 confirmed cases and human mobility index was robust after excluding Wuhan (Fig. 3 ).
Fig. 2.
Percentage change (%) and 95% confidence interval of daily COVID-19 confirmed cases associated with a unit increase in human mobility index using Equation (1).
Fig. 3.
Percentage change (%) and 95% confidence interval of daily COVID-19 confirmed cases associated with a unit increase in human mobility index using Equation (1) after excluding Wuhan.
3.3. The mediating effect of air quality index
Table 3 shows the results of our mediation analysis. We found that air quality index partially mediated the association of human mobility index with COVID-19 confirmed cases, supporting our hypothesis. At lag 0–14, air quality index significantly mediated 19.47% of the relationship between human mobility and COVID-19 infection, and the direct effect of human mobility indicated that a unit increase in human mobility index (lag 0–14) was associated with a 5.15% (95% CI: 0.31 to 10.00) increase in daily COVID-19 confirmed cases. At lag 0–21, the proportion of the relationship between human mobility and COVID-19 infection mediated by air quality index was 9.98%. The direct effect showed that a unit increase in human mobility index (lag 0–21) was associated with a 17.16% (95% CI: 11.55 to 22.77) increase in daily COVID-19 confirmed cases. We also observed a positive relationship between human mobility index and air quality index. As shown in Table 4 , the results of the mediation analysis were still robust and the proportions of the association between human mobility and COVID-19 infection mediated by air quality index were also similar (19.14% at lag 0–14 and 8.87% at lag 0–21) after excluding Wuhan.
Table 3.
Mediating effects of air quality index on the association between human mobility and COVID-19 confirmed cases.
| Lag0–14 |
Lag0–21 |
|||||
|---|---|---|---|---|---|---|
| Variables | Confirmed cases (log) | Air quality index | Confirmed cases (log) | Confirmed cases (log) | Air quality index | Confirmed cases (log) |
| Human mobility index | 0.0645* (0.0166–0.1123) | 7.8500* (6.3898–9.3102) | 0.0515* (0.0031–0.1000) | 0.1895* (0.1341–0.2450) | 7.5640* (6.2369–8.8911) | 0.1716* (0.1155–0.2277) |
| Air quality index | 0.0016* (0.0007–0.0026) | 0.0025* (0.0012–0.0037) | ||||
| Control variables | YES | YES | YES | YES | YES | YES |
Note: This table reports Equation (1) – (3) estimated coefficients and 95% confidence intervals of interest variable and mediator.
*p < 0.05.
Table 4.
Mediating effects of air quality index on the association between human mobility and COVID-19 confirmed cases after excluding Wuhan.
| Lag0–14 |
Lag0–21 |
|||||
|---|---|---|---|---|---|---|
| Variables | Confirmed cases (log) | Air quality index | Confirmed cases (log) | Confirmed cases (log) | Air quality index | Confirmed cases (log) |
| Human mobility index | 0.0699* (0.0222–0.1176) | 7.8680* (6.3986–9.3374) | 0.0565* (0.0082–0.1048) | 0.2144* (0.1591–0.2698) | 7.6040* (6.2659–8.9421) | 0.1964* (0.1404–0.2524) |
| Air quality index | 0.0017* (0.0007–0.0026) | 0.0025* (0.0013–0.0037) | ||||
| Control variables | YES | YES | YES | YES | YES | YES |
Note: This table reports Equation (1) – (3) estimated coefficients and 95% confidence intervals of interest variable and mediator.
*p < 0.05.
3.4. The mediating effect of each air pollutant
Table 5 shows a summary of our pollutant level analyses, and the full results are shown in Tables S1–S2. At lag 0–14, PM2.5, PM10 and NO2 significantly mediated 18.23%, 12.72% and 27.82% of the relationship between human mobility and COVID-19 infection, respectively. At lag 0–21, the proportions of the relationship between human mobility and COVID-19 infection mediated by PM2.5, PM10 and NO2 were 8.91%, 7.64% and 22.64%. However, we did not find the mediating effects of SO2 and CO. We also observed that human mobility was negatively associated with O3 while O3 was positively related to COVID-19 infection (Tables S1–d). Therefore, O3 had a statistically significant suppressing effect. These results were robust after excluding Wuhan city.
Table 5.
The proportion of the association between human mobility and COVID-19 infection mediated by separate air pollutant.
| All 120 cities |
Non-Wuhan cities |
|||
|---|---|---|---|---|
| Lag0–14 | Lag0–21 | Lag0–14 | Lag0–21 | |
| PM2.5 | 18.23% | 8.91% | 17.72% | 7.94% |
| PM10 | 12.72% | 7.64% | 11.77% | 6.80% |
| NO2 | 27.82% | 22.64% | 26.02% | 19.34% |
| O3 | Suppressing effect | Suppressing effect | Suppressing effect | Suppressing effect |
| SO2 | / | / | / | / |
| CO | / | / | / | / |
4. Discussion
The purpose of this paper was to determine the underlying mechanism of the association between human mobility and the spread of COVID-19 by assessing the mediating effect of air quality, different from our previous work (Zhu et al., 2020) which aimed to examine the relationship between air pollution and COVID-19 infection. In this study, we found that human mobility was positively associated with COVID-19 confirmed cases using a generalized additive model. The mediation analysis showed that air quality index, PM2.5, PM10, and NO2 significantly mediated the association between human mobility and COVID-19 infection. However, we also found the suppressing effect of O3. These results providing evidence that human mobility restrictions could not only control the epidemic by decreasing social contact, but also affect the risk of COVID-19 infection by changing air quality.
Our results are consistent with previous studies. First, for the positive relationship between human mobility and the spread of COVID-19, Tian et al. (2020) found that mobility restriction policies like suspending intracity public transport, banning public gatherings and closing entertainment venues were associated with reductions in case incidence of COVID-19. Additionally, a study also reported that these old-style public health measures could play an important role in the novel coronavirus epidemic (Wilder-Smith and Freedman, 2020). Second, for the association of human mobility with air quality, Bao and Zhang (2020) showed that the reductions in PM10 and NO2 during the city lockdown could be completely explained by variations in human mobility, and they also indicated that 44.9% and 9.3% of the variations in AQI and PM2.5 were attributed to human mobility, respectively. The reason is that air pollution generated by consumption activities and industrial productions decreased due to the travel restrictions. Other studies reported that O3 concentration increased during the COVID-19 lockdown, which may be caused by the increased garden and home activities (e.g. cleaning and biomass burning) (Shi, X., Brasseur, G. P., 2020; Sicard, P., et al., 2020). Third, for the association between air quality and COVID-19 infection, Zhu et al. (2020) suggested that short-term exposure to higher concentrations of air pollutants (such as PM2.5, PM10, NO2 and O3) is associated with a higher risk of COVID-19 infection, since ambient air pollutants could make pathogens more invasive to humans by carrying them and make people more susceptible by affecting body's immunity (Becker and Soukup, 1999; Horne et al., 2018; Xu et al., 2016).
Our study has several contributions. First, to the best of our knowledge, this is the first multi-city study to assess the mediating effect of air quality on the association between human mobility and COVID-19 infection, indicating that affecting air quality is a potential mechanism besides decreasing social contact. Second, this study contributes to the integration of literature investigating three associations (i.e., the association of human mobility with COVID-19 infection, the association of human mobility with air quality, and the association of air quality with COVID-19 infection). Third, our study provides new evidence that human mobility restrictions are useful for controlling the epidemic but could increase O3 pollution.
There are also some limitations. First, the human mobility index from Baidu does not represent the real number of people going outside. Second, subgroup analysis by age group or gender to explore the sensitive population could not be conduct due to the lack of related information. Third, only cities in China were included in this study, so our findings were not globally representative. For those countries that do not have serious pollution issues, the mediating effect of air quality may be different. Future studies are needed to overcome these limitations.
5. Conclusion
In conclusion, our study suggests that limiting human movements is related to the reduction in COVID-19 confirmed cases and indicates that affecting air quality is a potential mechanism besides decreasing social contact. Therefore, human mobility restrictions and other public health interventions encouraging people to stay at home are useful for controlling the epidemic. However, this is a preliminary study, and large datasets should be used to conduct global analyses in the future since the mediating effect of air quality may not exist in those countries that do not have serious pollution issues.
Declaration of competing interest
The authors declare no competing interests.
Acknowledgements
This research was supported by the National Natural Science Foundation of China (grant no. 71571176).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.109911.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Amuakwa-Mensah F. Climate variability and infectious diseases nexus: evidence from Sweden. Infect. Dis. Model. 2017;2:203–217. doi: 10.1016/j.idm.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao R., Zhang A. Science of The Total Environment; 2020. Does lockdown reduce air pollution? Evidence from 44 cities in northern China; p. 139052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51:1173. doi: 10.1037//0022-3514.51.6.1173. https://psycnet.apa.org/buy/1987-13085-001 [DOI] [PubMed] [Google Scholar]
- Bayham J., Fenichel E.P. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. Lancet Publ. Health. 2020 doi: 10.1016/S2468-2667(20)30082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S., Soukup J.M. Exposure to urban air particulates alters the macrophage-mediated inflammatory response to respiratory viral infection. J. Toxicol. Environ. Health Part A. 1999;57:445–457. doi: 10.1080/009841099157539. [DOI] [PubMed] [Google Scholar]
- Bianconi, V., et al., Particulate matter pollution and the COVID-19 outbreak: results from Italian regions and provinces. Arch. Med. Sci.. 16. doi: 10.5114/aoms.2020.95336. [DOI] [PMC free article] [PubMed]
- Chan J.F.-W. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J. Science of The Total Environment; 2020. The influence of increased population density in China on air pollution; p. 139456. [DOI] [PubMed] [Google Scholar]
- Chen N. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395:764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinazzi M. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020 doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E. The Lancet Infectious Diseases. 2020. An interactive web-based dashboard to track COVID-19 in real time. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan Y. Effect of changes in season and temperature on cardiovascular mortality associated with nitrogen dioxide air pollution in Shenzhen, China. Sci. Total Environ. 2019;697:134051. doi: 10.1016/j.scitotenv.2019.134051. [DOI] [PubMed] [Google Scholar]
- Fang H. National Bureau of Economic Research; 2020. Human Mobility Restrictions and the Spread of the Novel Coronavirus (2019-ncov) in china. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;114732 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert M. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395:871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastie T.J. Routledge; 2017. Generalized Additive Models. Statistical Models in S; pp. 249–307. [Google Scholar]
- Horne B.D. Short-term elevation of fine particulate matter air pollution and acute lower respiratory infection. Am. J. Respir. Crit. Care Med. 2018;198:759–766. doi: 10.1164/rccm.201709-1883OC. [DOI] [PubMed] [Google Scholar]
- Huang C. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W.-Z. Association between community greenness and obesity in urban-dwelling Chinese adults. Sci. Total Environ. 2020;702:135040. doi: 10.1016/j.scitotenv.2019.135040. [DOI] [PubMed] [Google Scholar]
- Kerimray A. Science of The Total Environment; Kazakhstan: 2020. Assessing air quality changes in large cities during COVID-19 lockdowns: the impacts of traffic-free urban conditions in Almaty; p. 139179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer M.U. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020 doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y. Impact of weather factors on influenza hospitalization across different age groups in subtropical Hong Kong. Int. J. Biometeorol. 2018;62:1615–1624. doi: 10.1007/s00484-018-1561-z. [DOI] [PubMed] [Google Scholar]
- Liu K. Climate factors and the East Asian summer monsoon may drive large outbreaks of dengue in China. Environ. Res. 2020:109190. doi: 10.1016/j.envres.2020.109190. [DOI] [PubMed] [Google Scholar]
- Liu P. The association between metal exposure and semen quality in Chinese males: the mediating effect of androgens. Environ. Pollut. 2020:113975. doi: 10.1016/j.envpol.2020.113975. [DOI] [PubMed] [Google Scholar]
- Lu S.F., Lu L.X. Do mandatory overtime laws improve quality? Staffing decisions and operational flexibility of nursing homes. Manag. Sci. 2017;63:3566–3585. doi: 10.1287/mnsc.2016.2523. [DOI] [Google Scholar]
- Mahato S. Science of The Total Environment; 2020. Effect of lockdown amid COVID-19 pandemic on air quality of the megacity Delhi, India; p. 139086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakada L.Y.K., Urban R.C. Science of The Total Environment; 2020. COVID-19 pandemic: impacts on the air quality during the partial lockdown in São Paulo state, Brazil. 139087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of the PRC . vol. 26. 2020. p. 2020.http://www.nhc.gov.cn/xcs/fkdt/202001/12ec9062d5d041f38e210e8b69b6d7ef.shtml (The Press Conference of the State Council Information Office on January). [Google Scholar]
- National Health Commission of the PRC . 2020. The Press Conference of the Joint Prevention and Control Mechanism of the State Council on February 17, 2020.http://www.nhc.gov.cn/xcs/fkdt/202002/f12a62d10c2a48c6895cedf2faea6e1f.shtml Accessed date. [Google Scholar]
- Rucker D.D. Mediation analysis in social psychology: current practices and new recommendations. Soc. Person. Psychol. Comp. 2011;5:359–371. doi: 10.1111/j.1751-9004.2011.00355.x. [DOI] [Google Scholar]
- Shi X., Brasseur G.P. The response in air quality to the reduction of Chinese economic activities during the COVID‐19 outbreak. Geophys. Res. Lett. 2020 doi: 10.1029/2020GL088070. e2020GL088070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sicard P. Science of The Total Environment; 2020. Amplified ozone pollution in cities during the COVID-19 lockdown; p. 139542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout P.E., Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol. Methods. 2002;7:422. doi: 10.1037/1082-989X.7.4.422. [DOI] [PubMed] [Google Scholar]
- Sohrabi C. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020 doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobías A. Changes in air quality during the lockdown in Barcelona (Spain) one month into the SARS-CoV-2 epidemic. Sci. Total Environ. 2020:138540. doi: 10.1016/j.scitotenv.2020.138540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Trav. Med. 2020;27 doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q. Fine particulate air pollution and hospital emergency room visits for respiratory disease in urban areas in Beijing, China, in 2013. PloS One. 2016;11 doi: 10.1371/journal.pone.0153099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin W. Obesity mediated the association of exposure to polycyclic aromatic hydrocarbon with risk of cardiovascular events. Sci. Total Environ. 2018;616:841–854. doi: 10.1016/j.scitotenv.2017.10.238. [DOI] [PubMed] [Google Scholar]
- Zhong S. Study of the effects of air pollutants on human health based on Baidu indices of disease symptoms and air quality monitoring data in Beijing, China. Int. J. Environ. Res. Publ. Health. 2019;16:1014. doi: 10.3390/ijerph16061014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y. Science of The Total Environment; 2020. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China; p. 138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.