Abstract
Background:
Mental health care providers commonly encounter suicide ideation and suicidal behaviors among their patients despite a frequent lack of adequate knowledge and competence regarding suicide risk management.
Aims:
This study examined the associations among self-perceived sufficiency of training, self-efficacy, anxiety, and attitudes related to working with suicidal individuals.
Method:
Participants were 289 mental health care providers who completed a self-report survey.
Results:
Path analysis results indicated that perceived sufficiency of training was indirectly associated with negative attitudes (i.e., avoidance and discomfort) and cognitive and somatic anxiety about working with suicidal individuals through assessment self-efficacy.
Limitations:
The current study utilized cross-sectional data, and there were occupational heterogeneity and geographical homogeneity among the mental health care providers sampled.
Conclusion:
These findings suggest that sufficient suicide-related training focused on risk assessment may decrease mental health professionals’ negative and anxious reactions toward suicidal individuals and enhance confidence in suicide risk management.
Keywords: Suicide, self-efficacy, training, risk assessment
Mental health care providers (henceforth referred to as providers) commonly encounter patients exhibiting suicide ideation and suicidal behaviors (Feldman & Freedenthal, 2006; Kleespies, Penk, & Forsyth, 1993; Ruskin, Sakinofsky, Bagby, Dickens, & Sousa, 2004). However, often, mental health training programs lack suicide-related training (see Schmitz et al., 2012 for a comprehensive review of this topic). Additionally, providers lack adequate knowledge and comfort regarding suicide risk management (Berman, Stark, Cooperman, Wilhelm, & Cohen, 2015). Hence, there is a need for improved suicide-related training to increase knowledge of suicide risk assessment and management, bolster providers’ confidence and self-efficacy (i.e., self-perceived ability to effectively complete a task), and reduce anxiety and negative attitudes regarding working with suicidal individuals. The current study examined the associations among self-perceived sufficiency of training, self-efficacy, anxiety, and attitudes related to working with suicidal individuals.
Suicide risk assessment and management is critical for graduate training and continuing education for providers (Mackelprang, Karle, Reihl, & Cash, 2014; Pisani, Cross, & Gould, 2011). However, only 50% of psychology interns (Dexter-Mazza & Freeman, 2003), 25% of social workers (Feldman & Freedenthal, 2006), 6% of marriage and family therapy programs (Wozny, 2005), and 2% of counselor education programs (Wozny, 2005) have had or offer suicide-related training. Although 91% of psychiatry residency programs offer suicide-related training, many participants considered the training insufficient (Melton & Coverdale, 2009). Recent data indicated that 20.9% of clinically oriented graduate programs that were surveyed did not offer suicidology training or were not aware whether their program included such training (Jahn et al., 2017). Despite these statistics indicating that many providers lack proper training, they continue to treat individuals with elevated suicide risk (Mackelprang et al., 2014; Schmitz et al., 2012).
Suicide-related training is effective, as it has been associated with increased knowledge (MacDonald, 2005), improved assessment and documentation skills (McNiel et al., 2008), greater self-perceived knowledge and competence, and fewer negative attitudes toward suicidal individuals (e.g., Chagnon, Houle, Marcoux, & Renaud, 2007; Jacobson, Osteen, Jones, & Berman, 2012; Muehlenkamp et al., 2013). As an example, among providers who completed a suicide-related training, 44% reported increased confidence in suicide risk assessment and 54% reported increased confidence in treating suicidal individuals at the 6-month follow-up (Oordt, Jobes, Fonseca, & Schmidt, 2009). Similarly, a recent review of suicide risk training programs among nurses indicated improved competence, knowledge, and attitudes that were related to the training (Ferguson et al., 2018). Relatedly, providers who felt that their suicide-related training was sufficient reported significantly lower fear of patient suicidal behavior, more knowledge about suicide risk and protective factors, and greater skill in working with suicidal individuals (Jahn, Quinnett, & Ries, 2016). Notably, the sufficiency of suicide-related training more strongly predicted these variables than years of professional experience working with suicidal individuals (Jahn et al., 2016). These studies suggest that suicide-related training can bolster providers’ knowledge, assessment and intervention skills, and confidence, as well as reduce negative reactions toward suicidal individuals.
It is common for providers to experience distress when working with suicidal individuals (e.g., Farber, 1983; Roush et al., 2018), as well as after a patient dies by suicide (see Séguin, Bordeleau, Drouin, Castelli-Dransart, & Giasson, 2014 for review). Most providers consider suicide-related statements made by patients to be the most stressful experience in therapy (Deutsch, 1984) and 67% reported that discussing patients’ suicide risk was anxiety-provoking (Menninger, 1991). Similarly, on average, providers reported a greater fear of patient suicidal behavior compared with other negative clinical outcomes, such as being sued or assaulted (Roush et al., 2018). Sufficient suicide-related training and increased self-efficacy in assessment and management of suicide risk may mitigate some of these sources of distress.
Self-efficacy may play a crucial role in providers’ training experience and reactions to suicidal individuals. Although training to build skills is important, Douglas and Morris (2015) assert that a psychotherapist “may possess adequate skill levels to assess a patient’s risk for suicide appropriately, but because of low self-efficacy, the counselor is not actually performing the assessment or performing it poorly” (p. 59). For example, experience with suicidal individuals and confidence in the knowledge of risk factors, but not suicide-related training and clinical supervision, were associated with more competent responses to hypothetical suicidal statements (Mackelprang et al., 2014). Similarly, Osteen, Frey, Woods, Ko, and Shipe (2017) found that self-efficacy related to suicide risk management longitudinally mediated the association between suicide risk assessment/response behaviors before and after a suicide-specific training program. Positive attitudes toward suicide prevention were also associated with the increased use of suicide risk assessment/response practices and increased self-efficacy regarding suicide risk management. These findings suggest that self-efficacy related to suicide risk management is linked to changes in suicide prevention-related practices and attitudes toward suicide prevention after a suicide-specific training; however, this study did not test self-efficacy as a mediator between suicide-related training and attitudes.
Collectively, prior research suggests that suicide-related training alone may be insufficient for effective practice and may be indirectly associated with providers’ reactions (e.g., distress, attitudes) to suicidal individuals through self-efficacy related to working with suicidal individuals; however, researchers have yet to test this postulation. The current study examined providers’ self-efficacy as a mediator between perceived sufficiency of training and emotional distress (e.g., anxiety) related to working with suicidal individuals. We hypothesized that perceived sufficiency of training would be negatively associated with anxiety and negative attitudes. We also hypothesized that the associations between perceived sufficiency of training (predictor variable) and anxiety and negative attitudes (criterion variables) would be indirectly linked via self-efficacy (mediating variable).
Method
Participants
Participants were mental health care providers (N = 289) who were predominantly women (n = 219, 75.8%) and from the United States (n = 263, 91.0%); the mean age of participants was 44.3 years (SD = 12.6). Most participants had a master’s (n = 192, 66.4%) or doctoral (n = 61, 21.1%) degree, followed by a 4-year college degree (n = 18, 6.2%), medical degree (n = 4, 1.4%), 2-year college degree (n = 3, 1.0%), and some college but no degree (n = 3, 1.0%); eight participants (2.8%) did not report education level. The professions represented in the sample were social worker (n = 73, 25.3%), psychologist (n = 68, 23.5%), mental health counselor (n = 67, 23.3%), marriage and family therapist (n = 15, 5.2%), chemical dependency counselor (n = 14, 4.8%), certified counselor (n = 13, 4.5%), psychiatric nurse practitioner (n = 6, 2.1%), psychiatrist (n = 4, 1.4%), pastoral counselor (n = 3, 1.0%), and other counselor (e.g., art therapist, sexual assault counselor, suicide postvention specialist; n = 26, 9.0%).
Measures
Suicidal Patient Comfort Survey (SPCS)
The SPCS is a self-report instrument containing five sections assessing providers’ discomfort when evaluating a suicidal individual (Jahn et al., 2016). The sections used in the current study were (1) demographic information, (2) knowledge and attitudes about suicide, (3) anxiety related to suicide risk, and (4) self-efficacy in assessment and management of suicide risk. See Electronic Supplementary Material 1 for the SPCS construct validity analyses and items.
Demographic information section.
We used the item, “Do you feel that you have received sufficient training in suicide risk assessment and risk reduction/intervention?” (yes/ no), to assess self-perceived sufficiency of suicide-related training. This item was chosen as a face-valid predictor of sufficiency of training in this domain. For this item, 200 (69.2%) responded yes, 86 (29.8%) responded no, and three (1.0%) did not respond.
Self-reported knowledge and attitudes about suicide.
The items in the knowledge and attitudes section contained various single-item questions and a modified version of the Approach to Death and Dying Patients Attitude Scale (ADDPAS; Kavas & Öztuna, 2011). The current study only used the modified version of the ADDPAS, which was adapted to focus on suicide risk, rather than on death and dying more generally. The modified ADDPAS consisted of 13 items with response options ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicated greater discomfort and avoidance related to working with suicidal individuals. Cronbach’s α coefficients were acceptable (.83 and .71 for the discomfort [eight items] and avoidance [five items] related to working with suicidal individuals scores, respectively).
Anxiety related to suicide risk section.
The items for the personal reactions to suicide and suicide risk section were adapted from the Cognitive-Somatic Anxiety Questionnaire (CSAQ; DeGood & Tait, 1987; Schwartz, Davidson, & Goleman, 1978). Rather than assessing cognitive and somatic generalized anxiety symptoms, we modified the CSAQ instructions to focus on cognitive and somatic anxiety related to encountering a suicidal patient and removed three items irrelevant to contexts in which a provider may encounter a suicidal individual. The modified CSAQ consisted of nine items with response options ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicated greater anxiety. Cronbach’s α coefficients were acceptable (.86 and .85 for the cognitive anxiety [five items] and somatic anxiety [four items] related to working with suicidal individuals scores, respectively).
Self-efficacy in the assessment and management of suicide risk section.
The self-efficacy section (i.e., Suicide Risk Management Self-Efficacy Scale) included six items with response options ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicated greater assessment self-efficacy and self-perceived competence. These items assessed self-efficacy regarding screening for suicide ideation, conducting a full risk assessment, reducing suicide risk, and general perceived competence in working with suicidal individuals. Cronbach’s α coefficients were acceptable to poor (.85 and .50 for assessment self-efficacy [three items] and self-perceived competence [threes items] related to working with suicidal individuals, respectively). We did not use self-perceived competence in the analyses due to the low internal consistency coefficient.
Procedures
The appropriate Institutional Review Board (IRB) reviewed and approved the procedures and materials used in this study. The IRB did not require an informed consent document for this study; instead, participants provided consent by reviewing an information page about the study and their rights as a participant before their participation. Participants were recruited through e-mails sent to professional listservs and individuals who had registered for a suicide prevention training program. Snowball sampling (i.e., chain referral sampling) methods were also utilized. We collected data anonymously using an online survey program. Participants could discontinue at any time and were not compensated. Data were collected cross-sectionally and administered in the same sequence for all participants.
Results
Table 1 shows bivariate correlations and descriptive statistics. We conducted bootstrapped regression-based path analyses to examine direct and indirect effects (i.e., the product of coefficients) using Mplus version 7.11. The examination of indirect effects does not require significant direct effects (Hayes, 2013). We utilized maximum likelihood estimation and 10,000 bootstrapped samples to obtain bootstrapped standard errors and bias-corrected bootstrapped 95% confidence intervals for the model parameter estimates; confidence intervals not containing 0 indicate statistically significant indirect effects (Hayes, 2013). Because our model was just identified, model fit indices are not reported.
Table 1.
Bivariate correlations and descriptive statistics for observed total scores
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Perceived training sufficiency+ | – | |||||
| 2. Assessment self-efficacy | .17** | – | ||||
| 3. Somatic anxiety | −.22*** | −.16* | – | |||
| 4. Cognitive anxiety | −.26*** | −.26*** | .55*** | – | ||
| 5. Avoidance | −.17** | −.33*** | .19** | .41*** | – | |
| 6. Discomfort | −.33*** | −.29*** | .49*** | .46*** | .39*** | – |
| M | – | 14.17 | 9.58 | 7.82 | 7.53 | 15.94 |
| SD | – | 1.62 | 3.52 | 2.86 | 2.37 | 4.75 |
| Observed range | – | 3–15 | 4–19 | 5–20 | 5–15 | 8–31 |
| Possible range | – | 3–15 | 4–20 | 5–25 | 5–25 | 8–40 |
Note. Perceived training sufficiency (1 = sufficient; 0 = insufficient). Assessment self-efficacy = the self-efficacy about assessment score from the Suicidal Patient Comfort Survey (SPCS). Somatic anxiety = the SPCS somatic anxiety score. Cognitive anxiety = the SPCS cognitive anxiety score. Avoidance = the SPCS avoidance score. Discomfort = the SPCS discomfort score. Perceived training sufficiency was correlated with the other variables using point-biserial correlation; all other correlations are Pearson’s r correlations.
p < .05.
p < .01.
p < .001.
As seen in Figure 1, all paths were in the expected direction and statistically significant (p < .05), except for the nonsignificant direct path from perceived sufficiency of training to avoidance. Furthermore, there were significant specific indirect effects from perceived sufficiency of training to somatic anxiety, cognitive anxiety, avoidance, and discomfort through assessment self-efficacy (see Table 2).
Figure 1.
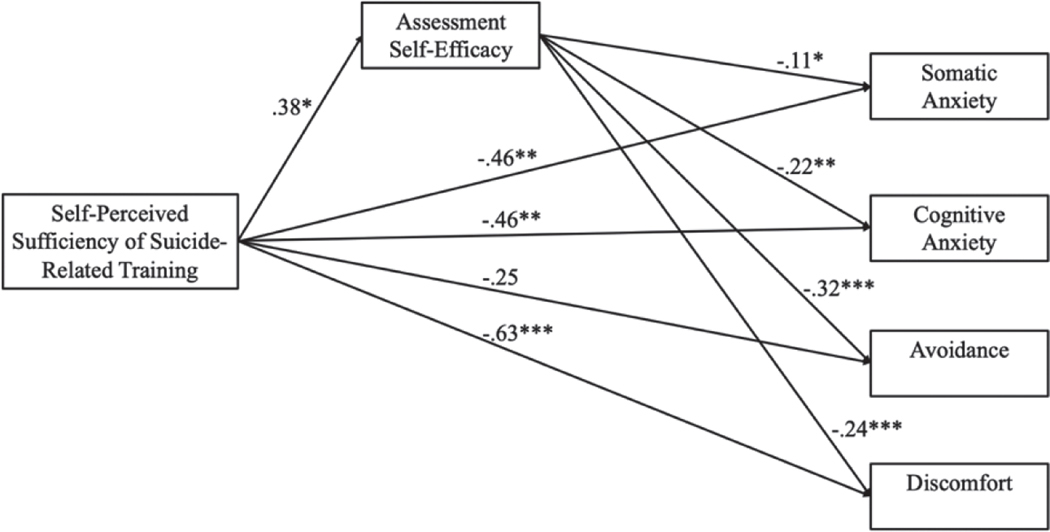
Standardized coefficients (STDY) for the path analysis model.
*p < .05; **p < .01; ***p < .001.
Table 2.
Specific indirect effects from the path analysis model (the indirect associations between self-perceived sufficiency of suicide-related training and the criterion variables through assessment self-efficacy)
| Criterion variables | Estimate | SE | Lower 5% | Upper 5% | R2 |
|---|---|---|---|---|---|
| Anxiety | |||||
| Somatic anxiety | −.04 | .03 | −.10 | −.01 | .06 |
| Cognitive anxiety | −.08 | .05 | −.18 | −.02 | .10 |
| Attitudes | |||||
| Discomfort | −.09 | .04 | −.17 | −.03 | .16 |
| Avoidance | −.12 | .06 | −.22 | −04 | .13 |
Note. Standardized estimates (STDY) are presented. Estimate - indirect effect estimate. Lower 5% and Upper 5% = lower and upper limit of the 95% bootstrapped CI. Somatic anxiety = somatic anxiety score from the anxiety section of the Suicidal Patient Comfort Survey (SPCS). Cognitive anxiety = the SPCS cognitive anxiety score. Avoidance = the SPCS avoidance score. Discomfort = the SPCS discomfort score.
As an exploratory sensitivity analysis, we included years of professional experiences as a covariate in the model, which did not change the statistical significance or the pattern of the path coefficients or indirect effects from the original model. Years of professional experience was significantly negatively associated with somatic anxiety, discomfort, and avoidance but not cognitive anxiety. Furthermore, years of professional experience merely increased the predicted variance in these criterion variables by 2–3% beyond the other predictors in the model. Therefore, perceived sufficiency of training is an important and unique predictor of self-efficacy, anxiety, and attitudes related to working with suicidal individuals.
Discussion
The findings largely supported our hypothesis that the associations between perceived sufficiency of training and anxiety and negative attitudes would be indirectly linked via self-efficacy. Results indicated significant indirect effects, such that perceived sufficiency of suicide-related training was associated with attitudes toward working with suicidal individuals (i.e., avoidance and discomfort related to working with suicidal individuals) through assessment self-efficacy. Similarly, significant indirect effects also indicated that perceived sufficiency of suicide-related training was associated with cognitive and somatic anxiety related working with suicidal individuals through assessment self-efficacy. The path analysis model indicated significant direct effects, such that providers who perceived their training as sufficient reported greater assessment self-efficacy, lower somatic and cognitive anxiety, and less discomfort in working with suicidal individuals; however, there was no significant direct path from perceived sufficiency of suicide-related training to avoidance.
These findings suggest that providers who perceive themselves as having sufficient training in suicide risk management also report less anxiety (i.e., cognitive and somatic anxiety) and fewer negative attitudes (i.e., discomfort) regarding working with suicidal individuals. Additionally, the significant indirect effects in this study suggest that providers who perceived that they had received sufficient suicide-related training may have felt more efficacious in the assessment of suicidal individuals (i.e., assessment self-efficacy), thereby improving attitudes and lowering anxiety regarding working with suicidal individuals. These results are consistent with prior findings that indicate providers’ self-efficacy in managing suicidal individuals is the bridge between skills and executing effective actions (Douglas & Morris, 2015; Larson & Daniels, 1998). Given that our study indicated that assessment self-efficacy was a significant mediator of the relation between perceived sufficiency of suicide-related training and attitudes and anxiety toward working with suicidal individuals, assessing perceived assessment self-efficacy throughout training may be more useful than merely querying whether the trainee perceives that his or her training was adequate.
The findings of this study have important implications for training in suicide risk assessment and management. Consistent with previous findings, the perception of having obtained didactic knowledge alone may be insufficient to promote effective work with suicidal individuals (Mackelprang et al., 2014; Schmitz et al., 2012). Instead, it appears that suicide risk assessment self-efficacy drives the association between perceptions of sufficient training and providers’ reduced avoidance, anxiety, and discomfort regarding interfacing with suicidal individuals. Therefore, applied clinical experience with suicidal individuals may be crucial in promoting feelings of self-efficacy regarding suicide risk assessment and management in the context of training (Mackelprang et al., 2014; Schmitz et al., 2012).
Furthermore, greater emphasis should be placed on competence related to one’s training rather than the quantity of training that is offered to providers (Schmitz et al., 2012). Specifically, these findings suggest that assessing providers’ suicide risk assessment self-efficacy may be an essential first step to understanding the extent to which providers feel able to execute learned skills and willing to use them as needed. Implementing and adhering to training in core competencies for suicide risk assessment and management may enhance training and supervision (Rudd, Cukrowicz, & Bryan, 2008). Training developers should consider conducting pre and posttraining assessments of suicide risk assessment and management skills, as well as assessing the components of training that are directly associated with increased self-efficacy. Including training components that promote feelings of effectiveness in executing suicide risk assessment and management may improve suicide-related training (e.g., role-plays). Academic training programs should also consider the addition of a graduate course in suicide theory, risk assessment, and management training, which has been shown to improve students’ factual knowledge and ability to estimate suicide risk (Cramer, Bryson, Stroud, & Ridge, 2016). Such approaches could be implemented with providers who are striving to advance their suicide risk assessment and management skills via continuing education courses or with graduate trainees in the context of supervision- and classroom-based instruction.
Limitations
This study has several strengths, including the use of a large sample of providers, the use of validated suicide-related training assessments, and the examination of a possible mediating factor between training and reactions to suicidal individuals that could inform future training programs. Although there are many merits of the current study, limitations should be noted. First, this study utilized cross-sectional data, which precludes causal inference and the examination of mediation through temporal associations (as opposed to indirect effects). Therefore, future studies should utilize longitudinal methods and randomized study designs. Second, there was occupational heterogeneity among the providers, and most providers were from the United States. Future studies should replicate the current study among more homogeneous groups of providers and test the generalizability of our findings to other countries. Additionally, common method variance may have influenced the results, and participants may have engaged in biased reporting about behaviors. Thus, future studies should utilize multimethod assessment, such as objective evaluations of training sufficiency (e.g., training that includes evidence-based practices) and competence in working with suicidal individuals (e.g., objective coding of providers’ behavior in interactions with suicidal individuals). Similarly, we assessed self-perceived sufficiency of suicide-related training using a question about both assessment and intervention. Future studies should consider evaluating assessment and intervention training separately to identify any unique effects. Future research may also examine the impact of specific tools and training on competence in working with suicidal individuals. For example, specific and concrete assessment algorithms (e.g., the Suicide Risk Decision Tree; Joiner, Walker, Rudd, & Jobes, 1999) and empirically supported suicide interventions (e.g., Safety Planning Intervention; Stanley & Brown, 2012) may increase self-efficacy and appropriate risk management strategies, thereby reducing anxiety and behavioral avoidance of suicidal individuals.
Conclusion
Given the inherent challenges in working with suicidal individuals, it is understandable that anxiety and avoidance are common responses among providers. However, this study suggests that when providers feel sufficiently trained and efficacious in their work with suicidal patients, there may be a reduction in emotional and behavioral impediments. More research is needed in this area, however, to best understand the effectiveness of suicide-related training and the mechanistic role of self-efficacy. By arming providers with both the knowledge and self-efficacy to assess and manage suicide risk, strategic and targeted suicide-related training may assist clinicians in assessing and working more effectively with suicidal individuals, which may help in saving lives.
Acknowledgments
Funding
This work was supported by a grant from the National Institute of Mental Health (T32 MH020061).
Biography
Sean M. Mitchell, PhD, is Assistant Professor in the Department of Psychological Sciences at Texas Tech University. He earned his PhD in Clinical Psychology at Texas Tech University in 2018. He completed a postdoctoral fellowship in suicide prevention research at the University of Rochester Medical Center in 2019.
Nathanael Taylor, PhD, is a staff psychologist at Denver Health and also holds an instructorship position at the University of Colorado School of Medicine. He completed his PhD in Clinical Psychology at Texas Tech University in 2017. His research interests include suicide risk in severe mental illness populations.
Danielle R. Jahn, PhD, is a psychologist at the Orlando VA Medical Center’s Mental Health Center for Acute Recovery Empowerment. She received her PhD in Clinical Psychology from Texas Tech University. She completed her postdoctoral fellowship at the VA VISN 5 MIRECC.
Jared F. Roush, PhD, is a clinical psychology fellow at the South Texas Veterans Healthcare System. He earned his PhD in Clinical Psychology at Texas Tech University in 2018.
Sarah L. Brown, PhD, is a postdoctoral research associate at the University of Pittsburgh Department of Psychiatry. She completed her PhD in Clinical Psychology at Texas Tech University in 2019. Her research focuses on theoretical risk factors for suicide and issues related to assessment.
Richard Ries, MD, is Professor of Psychiatry at the University of Washington Medical School. He is specialty boarded in psychiatry, addiction medicine, and addiction psychiatry. His research focuses on suicide prevention for those with addiction and other disorders, contingency management for drugs and alcohol, and other topics.
Paul Quinnett, PhD, is President and CEO of the QPR Institute in Spokane, WA, and Clinical Assistant Professor in the Department of Medicine and Behavioral Sciences at the University of Washington School of Medicine. His interests lie in public health education and evidence-based training of health care professionals.
Footnotes
Electronic Supplementary Material
The electronic supplementary material is available with the online version of the article at https://doi.org/10.1027/0227-5910/a000647
ESM 1. Additional construct validity analyses and results for the SPCS sections, and the SPCS items
References
- Berman NC, Stark A, Cooperman A, Wilhelm S, & Cohen IG (2015). Effect of patient and therapist factors on suicide risk assessment. Death Studies, 39, 433–441. 10.1080/07481187.2014.958630 [DOI] [PubMed] [Google Scholar]
- Chagnon F, Houle J, Marcoux I, & Renaud J. (2007). Control-group study of an intervention training program for youth suicide prevention. Suicide and Life-Threatening Behavior, 37, 135–144. 10.1521/su1i.2007.37.2.135 [DOI] [PubMed] [Google Scholar]
- Cramer RJ, Bryson CN, Stroud CH, & Ridge BE (2016). A pilot test of a graduate course in suicide theory, risk assessment, and management. Teaching of Psychology, 43, 238–242. 10.1177/0098628316649483 [DOI] [Google Scholar]
- DeGood DE, & Tait RC (1987). The Cognitive-Somatic Anxiety Questionnaire: Psychometric and validity data. Journal of Psychopathology and Behavioral Assessment, 9, 75–87. 10.1007/BF00961633 [DOI] [Google Scholar]
- Deutsch CJ (1984). Self-reported sources of stress among psychotherapists. Professional Psychology: Research and Practice, 15, 833–845. 10.1037/0735-7028.15.6.833 [DOI] [Google Scholar]
- Dexter-Mazza ET, & Freeman KA (2003). Graduate training and the treatment of suicidal clients: The students’ perspective. Suicide and Life-Threatening Behavior, 33, 211–218. 10.1521/su1i.33.2.211.22769 [DOI] [PubMed] [Google Scholar]
- Douglas KA, & Morris CW (2015). Assessing counselors’ self-efficacy in suicide assessment and intervention. Counseling Outcome Research and Evaluation, 6, 58–69. 10.1177/2150137814567471 [DOI] [Google Scholar]
- Farber BA (1983). Psychotherapists’ perceptions of stressful patient behavior. Professional Psychology: Research and Practice, 14, 697–705. 10.1037/0735-7028.14.5.697 [DOI] [Google Scholar]
- Feldman BN, & Freedenthal S. (2006). Social work education in suicide intervention and prevention: An unmet need? Suicide and Life-Threatening Behavior, 36, 467–480. 10.1521/su1i.2006.36.4.467 [DOI] [PubMed] [Google Scholar]
- Ferguson MS, Reis JA, Rabbetts L, Ashby H-J, Bayes M, McCracken T, … Procter NG (2018). The effectiveness of suicide prevention education programs for nurses: A systematic review. Crisis, 39, 96–109. 10.1027/0227-5910/a000479 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: The Guilford Press. [Google Scholar]
- Jacobson JM, Osteen P, Jones A, & Berman A. (2012). Evaluation of the recognizing and responding to suicide risk training. Suicide and Life-Threatening Behavior, 42, 471–485. 10.1111/j.1943-278X.2012.00105.x [DOI] [PubMed] [Google Scholar]
- Jahn DR, Drapeau CW, Wacha-Montes A, Grant BL, Nadorff MR, Pusateri MJ Cukrowicz KC (2017). Characteristics of and barriers to suicidology training in undergraduate and clinically-oriented graduate-level psychology programs. Suicidology Online, 8, 104–113. [Google Scholar]
- Jahn DR, Quinnett P, & Ries R. (2016). The influence of training and experience on mental health practitioners’ comfort working with suicidal individuals. Professional Psychology:Research and Practice, 47, 130–138. 10.1037/pro0000070 [DOI] [Google Scholar]
- Joiner TE, Walker RL, Rudd MD, & Jobes DA (1999). Scientizing and routinizing the assessment of suicidality in outpatient practice. Professional Psychology: Research and Practice, 30, 447–453. 10.1037/0735-7028.30.5.447 [DOI] [Google Scholar]
- Kavas MV, & Oztuna D. (2011). Thanatophobia in medical students: Approach to Death and Dying Patients Attitude Scale (ADDPAS) for undergraduate years in medicine. Journal of Cancer Education, 26, 774–781. 10.1007/s13187-011-0197-z [DOI] [PubMed] [Google Scholar]
- Kleespies PM, Penk WE, & Forsyth JP (1993). The stress of patient suicidal behavior during clinical training: Incidence, impact, and recovery. Professional Psychology: Research and Practice, 24, 293–303. 10.1037/0735-7028.24.3.293 [DOI] [Google Scholar]
- Larson LM, & Daniels JA (1998). Review of the counseling self-efficacy literature. Counseling Psychologist, 26, 179–218. 10.1177/0011000098262001 [DOI] [Google Scholar]
- MacDonald MG (2005). Attitudes of trainees in suicide intervention toward euthanasia and suicide among the nonterminally ill. Psychological Reports, 96, 709–712. 10.2466/PR0.96.3.709-712 [DOI] [PubMed] [Google Scholar]
- Mackelprang JL, Karle J, Reihl KM, & Cash R. (2014). Suicide intervention skills: Graduate training and exposure to suicide among psychology trainees. Training and Education in Professional Psychology, 8, 136–142. 10.1037/tep0000050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNiel DE, Fordwood SR, Weaver CM, Chamberlain JR, Hall SE, & Binder RL (2008). Effects of training on suicide risk assessment. Psychiatric Services, 59, 1462–1465. 10.1176/appi.ps.59.12.1462 [DOI] [PubMed] [Google Scholar]
- Melton BB, & Coverdale JH (2009). What do we teach psychiatric residents about suicide? A national survey of chief residents. Academic Psychiatry, 33, 47–50. 10.1176/appi.ap.33.1.47 [DOI] [PubMed] [Google Scholar]
- Menninger WW (1991). Patient suicide and its impact on the psychotherapist. Bulletin of the Menninger Clinic, 55, 216–227. [PubMed] [Google Scholar]
- Muehlenkamp JJ, Claes L, Quigley K, Prosser E, Claes S, & Jans D. (2013). Association of training on attitudes towards self-injuring clients across health professionals. Archives of Suicide Research, 17, 462–468. 10.1080/13811118.2013.801815 [DOI] [PubMed] [Google Scholar]
- Oordt MS, Jobes DA, Fonseca VP, & Schmidt SM (2009). Training mental health professionals to assess and manage suicidal behavior: Can provider confidence and practice behaviors be altered? Suicide and Life-Threatening Behavior, 39, 21–32. 10.1521/su1i.2009.39.1.21 [DOI] [PubMed] [Google Scholar]
- Osteen P,Frey JM,Woods MN,Ko J, & Shipe S.(2017).Mode1ing the longitudinal direct and indirect effects of attitudes, self-efficacy, and behavioral intentions on practice behavior outcomes of suicide intervention training. Suicide and Life-Threatening Behavior, 47, 410–420. 10.1111/s1tb.12288 [DOI] [PubMed] [Google Scholar]
- Pisani AR, Cross WF, & Gould MS (2011). The assessment and management of suicide risk: State of workshop education. Suicide and Life-Threatening Behavior, 41, 255–276. 10.1111/j.1943-278X.2011.00026.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roush JF, Brown SL, Jahn DR, Mitchell SM, Taylor NJ, Quinnett P, & Ries R. (2018). Mental health professionals’ suicide risk assessment and management practices: The impact of fear of suicide-related outcomes and comfort working with suicidal individuals. Crisis, 39, 55–64. 10.1027/0227-5910/a000478 [DOI] [PubMed] [Google Scholar]
- Rudd MD, Cukrowicz KC, & Bryan CJ (2008). Core competencies in suicide risk assessment and management: Implications for supervision. Training and Education in Professional Psychology, 2, 219–228. 10.1037/1931-3918.2A219 [DOI] [Google Scholar]
- Ruskin R, Sakinofsky I, Bagby RM, Dickens S, & Sousa G. (2004). Impact of patient suicide on psychiatrists and psychiatric trainees. Academic Psychiatry, 28, 104–110. 10.1176/appi.ap.28.2.104 [DOI] [PubMed] [Google Scholar]
- Schmitz WJ, Allen MH, Feldman BN, Gutin NJ, Jahn DR, Kleespies PM Simpson S. (2012). Preventing suicide through improved training in suicide risk assessment and care: An American Association of Suicidology Task Force report addressing serious gaps in U. S. mental health training. Suicide and Life-Threatening Behavior, 42, 292–304. 10.1111/j.1943-278X.2012.00090.x [DOI] [PubMed] [Google Scholar]
- Schwartz GE, Davidson RJ, & Goleman DJ (1978). Patterning of cognitive and somatic processes in the self-regulation of anxiety: Effects of meditation versus exercise. Psychosomatic Medicine, 40, 321–328. [DOI] [PubMed] [Google Scholar]
- Séguin M, Bordeleau V, Drouin M-S, Castelli-Dransart DA, & Giasson F (2014). Professionals’ reactions following a patient’s suicide: Review and future investigation. Archives of Suicide Research, 18, 340–362. 10.1080/13811118.2013.833151 [DOI] [PubMed] [Google Scholar]
- Stanley B, & Brown GK (2012). Safety planning intervention: A brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19, 256–264. 10.1016/j.cb-pra.2011.01.001 [DOI] [Google Scholar]
- Wozny DA (2005). The prevalence of suicide and violence assessment/intervention courses in CACREP and COAMFTE-accredited counseling curriculums In Waltz GR & Yep R. (Eds.), VISTAS: Compelling perspectives on counseling (pp. 271–274). Alexandria, VA: American Counseling Association. [Google Scholar]


