Highlights
-
•
Learning for Life (L4L) is a classroom-based program for grade 4–7 students.
-
•
L4L is flexibly taught by teachers and addresses gaps in current education.
-
•
L4L can increase digital health literacy and health knowledge in students.
-
•
L4L helps children develop healthy habits for their long-term wellbeing.
Abbreviations: BC, British Columbia; DHL, Digital health literacy; eHEALS, eHealth Literacy Scale; HKBC, Health knowledge and behaviour change; L4L, Learning for Life; SD, standard deviation
Keywords: School-based intervention, Healthy lifestyle behaviours, Child health promotion, Digital health literacy, Physical activity
Abstract
Promoting digital health literacy and healthy lifestyle behaviours in children can lead to positive long-term health outcomes and prevent chronic diseases. However, there are few school-based interventions promoting this education to intermediate elementary students. The objective of this study was to test the effectiveness of a novel intervention to increase students’ digital health literacy and health knowledge. Learning for Life is a classroom-based education program, developed for grade 4–7 students and delivered by teachers over six weeks. Three Canadian schools were recruited to deliver the intervention in 2018. This study had a pre-post design and no control group. Students’ self-reported digital health literacy and healthy lifestyle behaviours were measured at pre-intervention (n = 126), post-intervention (n = 119), and two-month follow-up (n = 104). Students at pre-intervention had a mean (SD) age of 10.98 (0.56) years (57.1% females). Almost all (97%) students had unsupervised access to the Internet through a computer or smartphone. From pre- to post-intervention, students’ digital health literacy increased (p = 0.009), but decreased from post-intervention to follow-up (p < 0.001). Post-intervention, the majority of students could identify at least one healthy behaviour (e.g., exercising one hour/day) and reported making at least one healthy change in their lives (e.g., eating more fruits/vegetables). This study demonstrated that the Learning for Life intervention can improve intermediate elementary students’ digital health literacy over the short-term and help them learn and retain healthy lifestyle knowledge and behaviours. These findings affirm the need for interventions promoting digital healthy literacy and healthy lifestyle behaviours for this age group.
1. Introduction
Health literacy is increasingly recognized as an important aspect of childhood; children who have high health literacy are better positioned to make positive choices for their health (Diamond et al., 2011). The significance of studying children’s health literacy has been widely appreciated in recent literature (DeWalt and Hink, 2009), as the incidence of chronic diseases and health conditions, such as type 2 diabetes and obesity, is rising in children worldwide (World Health Organization, 2015). In Canada, while the prevalence of overweight and obese 2–17 year old children has fallen slightly from 26% to 24% since 2004 (Statistics Canada, 2017), current trends indicate declining fitness levels (e.g., poorer cardiorespiratory fitness) (Colley et al., 2019). Childhood is a crucial period to shape health-related behaviours and focus on preventing the onset of chronic diseases (Yavuz et al., 2015), thereby potentially increasing children’s present and future health-related quality of life (World Health Organization, 2016), relieving healthcare systems of additional costs (Doucet and Beatty, 2010), and reducing health disparities (Paasche-Orlow and Wolf, 2010). Healthy lifestyle behaviours are important for not only long-term health, but also for academic success, which is a strong predictor of “future wealth, productivity and health” (Faught et al., 2017).
Digital health literacy (DHL) in children is emerging as a significant area of study and opportunity for interventions. DHL is a complex construct that depends on literacy in several other areas (i.e., traditional literacy and numeracy, as well as health, computer, information, media, and science literacies) and is a skillset concerning an individual’s ability to access, understand, and apply health information supplied via digital technologies (Norman and Skinner, 2006a). A person’s level of DHL is influenced by various factors (e.g., parental education, socioeconomic status) (Paakkari et al., 2018) and it is important that digital health interventions consider barriers related to culture, language, and accessibility (Zibrik et al., 2015). Emerging findings indicate that high DHL is associated with positive health behaviours and self-care across different populations (Fagnano et al., 2012, Mitsutake et al., 2016, Park et al., 2014).
With the widespread use and availability of various digital technologies (i.e., smartphones, computers) and platforms through which individuals can readily search for health information, it is clear that adequate DHL is important for enacting positive, evidence-based health behaviours and making well-informed decisions. Among school-age children, recent research indicates that technology use is high and many children regularly exceed daily limits of recreational screen-based activity recommended by national guidelines (Tremblay et al., 2011a). Furthermore, school-aged children typically have some degree of autonomy concerning their health-related behaviours (e.g., nutrition choices, sleep hygiene) (Coyne and Harder, 2011, Gruber et al., 2014). Thus, given the combined factors that children are regularly using digital technologies and have emerging autonomy, a child with high DHL may be better equipped to critically analyze poor versus high quality health information and balance their sedentary-based technology use with healthy behaviours.
DHL has typically been studied in older children and adolescents (i.e., 13–18 years old) (Fleary et al., 2018). However, as children access digital technologies at younger ages and without supervision (Smith et al., 2019), it is imperative to characterize the level of DHL in these younger populations and judge if interventions are warranted. Recent evidence of child health outcomes demonstrate a need for interventions that increase DHL and promote healthy behaviours. Strong evidence shows that high sedentary-based screen-time (i.e., >two hours/day of watching TV) is unfavourably associated with several important health indicators in children (e.g., body composition, academic achievement, cognition) (Carson et al., 2016, Tremblay et al., 2011b). Further, a very small proportion of Canadian children (9% of boys, 4% of girls) are engaging in at least 60 minutes of moderate-to-vigorous physical activity and they typically average 8–9 hours of sedentary time per day (Colley et al., 2011).
Developing appropriate sleep hygiene behaviours is now recognized as a crucial element for maintaining children’s health (Gruber et al., 2014), especially given the common presence of screens (i.e., TVs, computers, smartphones) in children’s bedrooms and high screen-time (Chahal et al., 2013). Reduced or poor quality sleep can hinder children’s development and daily cognitive abilities (Van Cauter and Knutson, 2008) and is associated with poor school achievement (Buckhalt et al., 2009), plus other downstream consequences (Gruber et al., 2014). Additionally, mounting evidence suggests that children’s social and emotional wellbeing are associated with disease risk in adulthood (Campbell et al., 2016). Thus, there is an urgent need for interventions targeting these modifiable cardio-metabolic risk factors and promoting DHL and healthy behaviours in children.
1.1. The Learning for Life program
School-based curriculum teaching DHL can be a powerful tool for providing children with a foundation for learning and implementing healthy lifestyles (Paakkari et al., 2018). Children typically spend 8–9 hours per day in school for half of a calendar year, thus, schools are responsible for a large proportion of contact time, but children receive varying degrees of health education (Centers for Disease Control and Prevention, 2011, Hills et al., 2015). Some guidelines exist for promoting physical activity, good nutrition, and other healthy behaviours in schools (Centers for Disease Control and Prevention, 2011, Ministry of Education, 2018), however, there is a lack of school-based curricula addressing even basic aspects of health literacy (Winkelman et al., 2016), and particularly so in intermediate grades, as we have found in British Columbia (BC). Given these circumstances, it is unsurprising that low health literacy is common in adolescents and adults and is associated with many poor health outcomes across the lifespan (Berkman et al., 2011). Thus, there is the opportunity and need to develop novel interventions integrated with a school’s curriculum for younger children that target DHL and promote healthy lifestyle behaviours.
The University of British Columbia’s Digital Emergency Medicine team developed and tested Learning for Life (L4L) as a school-based intervention for increasing DHL and healthy lifestyle behaviours in children aged 9–14 years (grades 4–7). L4L aims to develop different aspects of DHL and promote five important healthy lifestyle behaviours among students: physical activity, nutrition, sleep hygiene, stress management, and social connectedness. Teachers are provided with an educator ‘toolkit’, student workbook, and online, interactive graphic novels for students (see Supplementary Material; resources available at: https://digem.med.ubc.ca/projects/ubclearningforlife/). Teachers can flexibly deliver the program content, integrating it into their standard classroom curriculum, using a variety of delivery methods to meet the needs of their student learners and fit their teaching style.
The L4L intervention was comprehensively developed using iterative cycles of piloting and modification from 2014 to 2018. This involved extensive input from and collaboration with current and former teachers school administrators, child education and health experts, and health- and youth-focused organizations. The materials were piloted in several schools to further refine the content, resources, and integration into classroom planning, as well as ensuring that the materials were appropriate for the target ages. The piloting indicated that it was feasible to implement the intervention in the school setting, with teachers delivering the content to students in grades 4–7.
1.2. Aims
The first objective of this study was to characterize students’ present and past digital technology usage to better understand when DHL education should be introduced in the school system. The second aim was to test the effectiveness of the L4L intervention in increasing students’ DHL and improving modifiable risk factors (i.e., physical activity, sedentary behaviour, and social connectedness) for chronic diseases. In addition, we were interested in measuring students’ health knowledge and behaviour changes they implemented at the end of the intervention.
2. Methods
2.1. Study design
This study employed a pre-post design and was conducted from January to June 2018. The intervention was delivered over six weeks by teachers, with measures administered at pre-, post-intervention, and two-month follow-up.
The University of British Columbia’s Behavioural Research Ethics Board gave ethical approval for the conduct of the study (H17-01195). Participating schools gave approval for the delivery of the L4L program and conduct of research activities.
2.2. Setting and participants
We recruited three schools in BC according to schools’ interest (i.e., responses from school administrators to our initial invitation), readiness (i.e., to implement the study procedures according to our proposed timeline), and capacity for engagement (i.e., teachers had the time and resources to deliver the program and facilitate data collection). Additionally, we chose schools to reflect a broad demographic representation of the province: one inner-city school with a high immigrant population, one in rural BC with a higher-than-average population of Indigenous peoples, and one in a regional center with students predominantly from a European background. In each school, the principal identified eligible grade 4–7 classes. The research team then met with teachers to provide a 1.5-hour professional development orientation pertaining to the intervention’s purpose and learning objectives (see example of recorded orientation at: https://digem.med.ubc.ca/projects/ubclearningforlife/). The team also shared details of the study procedures and answered questions about the intervention.
2.3. Measures
This section briefly outlines the measures administered in the study. The Appendix provides further details. We collected the following data from student participants:
2.3.1. Demographics
Self-reported age and ethnicity. Teachers provided class lists with students’ birth-assigned gender and grade.
2.3.2. Technology usage
Self-reported past and current Internet usage and which devices they used to access the Internet.
2.3.3. Digital health literacy (DHL)
Measured using the eHealth Literacy Scale (eHEALS) (Norman and Skinner, 2006b). The scale asked participants to indicate their level of agreement with eight statements about online health information (total score range = 8–40; higher scores indicate greater DHL; sample question: “I know there is health information available online”).
2.3.4. Physical activity
Five questions asked participants to indicate the amount of time spent doing physical activity in a typical week (Colley et al., 2011). Participants could select one of 4 or 5 options (e.g., never, <1 hour/week, 2 to 3 hours/week, etc.). We summarized and compared the responses by item.
2.3.5. Sedentary behavior
Participants were asked to report the amount of time spent doing each of the following activities for the past week: watching TV, playing videogames or watching DVDs/videos, and using the computer. Responses were averaged to derive a mean score (hours/day) for each screen-based activity and combined to form a total screen-time score.
2.3.6. Health knowledge and behaviour change (HKBC)
A 10-item questionnaire asked participants about their experience with the L4L intervention, as well as changes in their health behaviours and knowledge. Students were asked to indicate their level of agreement to five Likert-type statements about the L4L intervention and DHL (range = 1–5; higher scores indicate greater agreement). One Likert-type item asked if students had made any changes to stay healthy because of what they learned during the intervention. Four items were open-ended questions where students could provide free-text responses.
2.3.7. Social connectedness
This comprised a 15-item scale where students indicated their level of agreement with adult- or peer-oriented social connectedness statements. Scores for the peer and adult domains were calculated, as well as a total scale score of the mean of the 15 items, yielding a possible range of 1–5 and higher scores indicating greater social connectedness.
2.4. Procedures
To launch the L4L intervention, the Principal Investigator (KH) and research team joined each class during their school day as special guests to introduce L4L, the concept of DHL, and the research component. Following the launch, students completed pre-intervention measures (Appendix Table S1). At the intervention’s conclusion, a wrap-up workshop was held in each class by research staff, where students completed post-intervention measures. Approximately two months post-intervention, students completed follow-up measures during school-time.
2.5. Data analysis
Continuous and categorical variables were descriptively summarized using means (standard deviations (SD)) and counts (percentages), respectively. The degree of normality of continuous variables’ distributions was checked by computing their level of skewness and kurtosis and inspecting their QQ-plots. Variables with non-normal distributions were summarized using their medians (interquartile ranges).
Changes in outcomes with normal distributions were tested with paired t-tests; changes in outcomes with non-normal distributions or ordinal data were tested with Wilcoxon signed-rank tests. A two-tailed alpha-level of 0.05 was considered statistically significant for all tests.
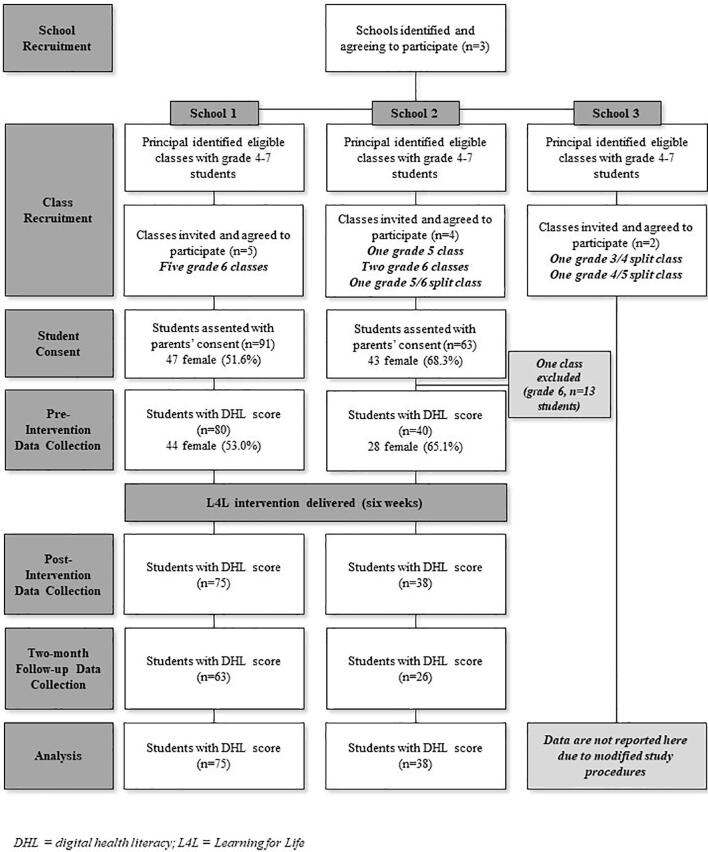
2.6. Modifications to the study
One school had student participants who were generally younger, with lower English fluency and more learning and social needs than students in the other two schools. We chose not to administer the two-month follow-up measures to students from this school to ensure the study was not excessively burdensome for the students. We ultimately excluded this school from the current analyses and these data are not reported here (Fig. 1). Additionally, at the conclusion of the L4L intervention, the research team was informed that one class of students had not received any of the program’s content, as the teacher was absent for the majority of the intervention. Data from this class were excluded from all analyses. See the Appendix for more details.
Fig. 1.
Flow chart showing the progression of schools and students through the study. DHL = digital health literacy; L4L = Learning for Life.
3. Results
Fig. 1 shows the flow of student participants through the study. From eight included classes, there were 261 eligible students, of which 126 (48.3%) consented and provided pre-intervention data. Table 1 presents the pre-intervention characteristics of students.
Table 1.
Pre-intervention demographic characteristics of the student participants.
| Total sample (n = 126) | School 1 (n = 83) | School 2 (n = 43) | |
|---|---|---|---|
| Age, years | 10.98 (0.56) | 11.13 (0.41) | 10.67 (0.68) |
| Gender, female | 72 (57.1%) | 44 (53.0%) | 28 (65.1%) |
| Grade | |||
| 5 | 21 (16.7%) | 0 | 21 (48.8%) |
| 6 | 105 (83.3%) | 83 (100.0%) | 22 (51.2%) |
| Ethnicity1 | |||
| Aboriginal/Indigenous | 14 (11.2%) | 12 (14.5%) | 2 (4.8%) |
| African | 3 (2.4%) | 2 (2.4%) | 1 (2.4%) |
| European | 64 (51.2%) | 41 (49.4%) | 23 (54.8%) |
| East Asian | 6 (4.8%) | 3 (3.6%) | 3 (7.1%) |
| South Asian | 5 (4.0%) | 3 (3.6%) | 2 (4.8%) |
| Southeast Asian | 2 (1.6%) | 1 (1.2%) | 1 (2.4%) |
| West Asian | 1 (0.8%) | 1 (1.2%) | 0 |
| Latin/South/Central American | 4 (3.2%) | 2 (2.4%) | 2 (4.8%) |
| Australian/Pacific Islander | 6 (4.8%) | 3 (3.6%) | 3 (7.1%) |
| Other | 4 (3.2%) | 1 (1.2%) | 3 (7.1%) |
| Unsure | 39 (31.2%) | 31 (37.4%) | 8 (19.1%) |
| Missing | 1 | 0 | 1 |
Cell values are mean (SD) or counts (percentages), as appropriate. Percentages were calculated after removing missing values from the denominator.
Ethnicity counts for each column may not sum to the column’s respective sample size, as students were able to select more than one ethnicity.
3.1. Technology usage
Students self-reported first using the Internet and a smartphone/computer without adult supervision at approximately seven years old (Table 2). Ninety-three (78.8%) students had access to a personal computer and/or smartphone to access the Internet and almost all (115 (97.5%)) had access to a personal or shared device to access the Internet.
Table 2.
Summary of technology usage.
| Total sample (n = 126) | School 1 (n = 83) | School 2 (n = 43) | |
|---|---|---|---|
| Age first using Internet without supervision, years | 6.75 (1.72) | 6.76 (1.84) | 6.74 (1.42) |
| Never | 5 (4.2%) | 2 (2.5%) | 3 (8.1%) |
| Missing | 8 | 2 | 6 |
| Age first using a smartphone/ computer alone, years | 7.05 (1.73) | 6.91 (1.84) | 7.34 (1.46) |
| Missing | 8 | 3 | 5 |
| Accessing the Internet outside of school1 | |||
| Personal smartphone | 67 (56.8%) | 50 (64.1%) | 17 (42.5%) |
| Personal portable computer (e.g., laptop, tablet) | 55 (46.6%) | 40 (51.3%) | 15 (37.2%) |
| Shared desktop computer | 47 (39.8%) | 35 (44.9%) | 12 (30.0%) |
| Internet usage at home without supervision | |||
| Never | 4 (3.3%) | 4 (5.1%) | 0 |
| Sometimes | 27 (22.5%) | 13 (16.5%) | 14 (34.1%) |
| Usually | 48 (40.0%) | 32 (40.5%) | 16 (39.0%) |
| Always | 41 (34.2%) | 30 (38.0%) | 11 (26.8%) |
| Missing | 6 | 4 | 2 |
Cell values are mean (SD) or counts (percentages), as appropriate. Percentages were calculated after removing missing values from the denominator.
Each percentage reflects the proportion of students selecting that option out of the total number that completed the questionnaire.
3.2. Digital health literacy, physical activity, sedentary behaviour, and social connectedness
Table 3 presents a descriptive summary of the outcomes by time point. Students generally reported having high DHL at each time point; we found that students’ eHEALS score increased pre- to post-intervention (p = 0.009) and decreased post-intervention to follow-up (p < 0.001). The majority of students indicated being physically active at least four days per week (Table S2). However, they also engaged in screen-related sedentary behaviour for approximately three hours per day, with 75 (63.6%), 70 (65.4%), and 66 (67.4%) students exceeding two hours of daily screen-time at pre-, post-intervention, and follow-up, respectively. Participants reported, on average, high levels of social connectedness with their peers and moderate levels with adults. Students’ time spent playing videogames or watching DVDs increased from pre-intervention to follow-up (p = 0.021). We observed no other changes over time.
Table 3.
Summary of outcomes by time point.
| Pre-intervention | Post-intervention | Two-month follow-up | |
|---|---|---|---|
| DHL (eHEALS; total score)1, 2 | 32.00 (27.00–35.00), n = 120 | 33.00 (30.00–37.00), n = 113 | 31.00 (27.00–35.00), n = 89 |
| Sedentary behaviour (screen-time; hours/day)1 | |||
| Total | 2.82 (1.47–4.34), n = 118 | 2.93 (1.61–4.88), n = 107 | 2.95 (1.62–5.04), n = 98 |
| Using a computer | 0.23 (0.00–1.29), n = 104 | 0.26 (0.00–1.14), n = 99 | 0.00 (0.00–1.00), n = 90 |
| Playing videogames or watching DVDs | 1.00 (0.32–2.29), n = 107 | 1.39 (0.42–2.61), n = 100 | 2.00 (0.52–2.68), n = 90 |
| Watching TV | 1.00 (0.50–1.66), n = 116 | 1.00 (0.43–1.57), n = 105 | 1.00 (0.50–1.71), n = 94 |
| Social connectedness (total score)1, 3 | |||
| Combined domains | 3.86 (3.47–4.13), n = 126 | 3.93 (3.50–4.31), n = 119 | 4.00 (3.53–4.27), n = 104 |
| Peer domain | 4.50 (4.00–4.83), n = 125 | 4.67 (4.17–5.00), n = 118 | 4.67 (4.17–5.00), n = 104 |
| Adult domain | 3.44 (3.00–3.78), n = 126 | 3.56 (3.00–4.00), n = 116 | 3.56 (3.19–3.89), n = 104 |
Median (IQR) reported as these variables are non-normally distributed.
Possible score range of 8–40, with higher scores indicating better DHL.
Possible score range of 1–5, with higher scores indicating more connectedness.
3.3. Health knowledge and behaviour change (HKBC)
Based on the five HKBC statements, students positively rated the L4L intervention and what they learned, both at post-intervention (M = 3.84, SD = 0.81) and two-month follow-up (M = 3.70, SD = 0.97). When asked if they were making any changes to stay healthy, 69 (61.6%) and 73 (70.8%) of the students at post-intervention and two-month follow-up, respectively, indicated that they were making changes.
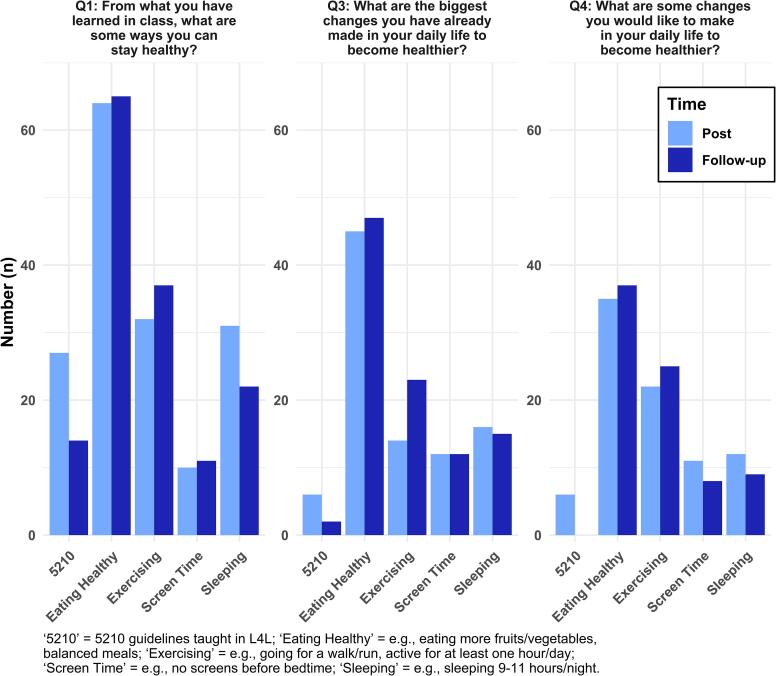
For the four open-ended questions asking students to identify healthy behaviours and any changes they had made or wanted to make to be healthier, we found that the majority could identify at least one healthy behaviour or change at both post-intervention and two-month follow-up (Table S3). The number of healthy behaviours/changes identified did not differ over time, except for question three (What are the biggest changes you have already made in your daily life to become healthier?), with students indicating significantly more healthy changes at two-month follow-up (p = 0.015).
For the three questions pertaining to students’ health knowledge and already undertaken and planned health-related behaviour changes, the most common responses were related to: i) eating healthier (e.g., more fruits/vegetables, fewer sugary drinks); ii) exercising more (e.g., playing outside more); iii) limiting technology use (e.g., not using screens before bedtime); iv) better sleep hygiene (e.g., sleeping the recommended amount of 9–11 hours per night); and, v) the ‘5-2-1-0’ guidelines taught in the intervention (i.e., a mnemonic for eating ≥ 5 fruits/vegetables, ≤2 hours of screen-time, ≥1 hour of physical activity, and zero sugary drinks per day) (SCOPE, 2019) (Fig. 2). For question two (From what you have learned in class, how can you use technology to help you stay healthy?), students’ responses were primarily related to: i) using a pedometer, smartphone app, etc. for tracking steps or other activity; ii) using apps or websites for finding health information (e.g., exercises, recipes); and, iii) how to identify reliable websites for finding good quality health information.
Fig. 2.
Number of student responses by type, HKBC question, and time point. ‘5210′ = 5210 guidelines taught in L4L; ‘Eating Healthy’ = e.g., eating more fruits/vegetables, balanced meals; ‘Exercising’ = e.g., going for a walk/run, active for at least one hour/day; ‘Screen Time’ = e.g., no screens before bedtime; ‘Sleeping’ = e.g., sleeping 9–11 h/night.
4. Discussion
We have developed and tested a school-based intervention to promote digital health literacy (DHL) and several key healthy lifestyle behaviours in a sample of students in intermediate elementary grades, with the goal of reducing their modifiable risk factors for chronic diseases. The Learning for Life (L4L) intervention was designed to integrate into existing school programming and be delivered flexibly by teachers. This was a pragmatic study set in the real-world where various barriers were encountered, yet, we found that the L4L intervention could be feasibly delivered by teachers without extensive preparation/training and to a generalizable sample of students to build DHL skills and positively influence healthy behaviours.
During the development of the L4L intervention, input from child education and health stakeholders indicated that a program promoting DHL and healthy behaviours would be appropriate for grade 4–7 students and address current gaps in programming. Our findings concerning students’ technology usage robustly support this, namely, the majority of students indicated currently having a personal device to access the Internet, and typically accessed the Internet autonomously. This result reinforces the primary motivation for creating L4L: young children already have the opportunity to actively search online for health information, and therefore need to develop skills to distinguish between good versus poor quality online health information.
We found that student self-reported DHL significantly increased from pre- to post-intervention, though this effect was not maintained at follow-up, suggesting that L4L had a positive short-term impact on students’ DHL. Relatedly, the majority of students were able to identify ways that technology can help with their health and how to distinguish good from poor quality health information online, corroborating their self-assessed DHL skills. Limited but growing evidence indicates that having high DHL is associated with various positive health outcomes across the lifespan (Fagnano et al., 2012, Mitsutake et al., 2016, Park et al., 2014). Coupled with our finding that children are first using smartphones/computers by approximately seven years old, these elements strongly indicate that students could receive DHL education regularly in school to develop and maintain these skills for future health and wellbeing.
At the two-month follow-up, students reported making more healthy changes in their daily lives compared to post-intervention. Students potentially may need some time before they can translate their learning into healthy behaviours, again reinforcing the implication that teaching DHL throughout the year in a school setting may result in more long-term positive outcomes in students’ health behaviours. We measured several modifiable risk factors for chronic disease and found that the L4L intervention did not have an immediate positive effect on students’ physical activity levels, screen-based sedentary behaviour, or social connectedness levels.
Students indicated that they regularly used technology, with over 60% of the sample engaging in screen-based sedentary activities for more than the recommended amount of two hours/day (Tremblay et al., 2011a). Unsurprisingly, we found a wide range of time spent using screens, with some students engaging in very little use, while some reported excessive use (e.g., >6 hours/day). These findings echo previous literature concerning high technology use in children (Colley et al., 2011, Tremblay et al., 2011a) and reaffirm the need for interventions to address these sedentary-based behaviours that may be displacing opportunities for being physically active (Carson et al., 2016, Tremblay et al., 2011b). Interestingly, computer use remained low over time, TV watching was consistently one hour/day, but time playing videogames doubled from pre-intervention to follow-up. While there may be various reasons for these trends, it is worth considering that videogame playing may be a key area to address in future L4L implementation (Taverno Ross et al., 2013). It is also important to consider the potential benefits of screen-time for children (e.g., increasing cognitive skills, time with peers/family), echoed in the updated position statement of the Canadian Pediatric Society (Ponti and Digital Health Task Force, 2019), which no longer emphasizes less than two hours/day of screen-time for children 5–17 years old, but rather recommends developing appropriate screen-use behaviours through “healthy management, meaningful screen use, positive modelling, and balanced, informed monitoring.”
Importantly, many of the students following the L4L intervention were able to identify healthy guidelines around screen use (e.g., limiting time to ≤2 hours/day) (Tremblay et al., 2011a) and indicated that they made or wanted to make such changes in their own lives. Related to this, students were also able to identify ways that technology could help them be healthier, such as using activity tracking devices/apps, searching for healthy recipes or exercises online, and finding indicators of good quality health information online. Thus, it seems that students were able to distinguish between subtle learning concepts around healthy versus unhealthy screen use (Straker et al., 2018). This is a positive first step, given that recent research into 12–18 year old students highlight important associations between technology use, sleep hygiene, physical activity, nutrition, and mental health (Smith et al., 2019), reiterating the need for appropriate health promotion interventions targeted at younger children who are developing these interconnected health behaviours (Borzekowski, 2009, Yavuz et al., 2015).
4.1. Strengths and limitations
The L4L intervention was delivered pragmatically in the real-world setting of the classroom, with purposively sampled schools to represent BC’s diverse population. Thus, we can be confident that the intervention can be readily implemented by other schools and teachers. Unfortunately, we were not able to fully test the intervention in the target population, as grade 7 classes were not recruited and we were unable to include the data from grade 4 students in the present analyses, thus limiting external validity.
Limitations of the study were the lack of a control group for comparative purposes and use of self-report measures for students. However, it is important to note that one of the primary goals of this study was to identify the ideal ages/grades for delivering the L4L intervention. Importantly, our findings around students’ technology usage and DHL suggest that the L4L intervention is appropriate for grade 5–6 students. Thus, future work could more comprehensively test the effectiveness of L4L in a randomized controlled trial, as well as stratify by age/grade to pinpoint when it is optimal to deliver L4L. Additionally, assessing teacher fidelity to the program delivery is an important future consideration.
4.2. Implications
The L4L program has the potential to be a very cost-effective intervention, not only in terms of long-term savings by preventing chronic disease onset, but also in terms of delivery as it is taught by teachers (with minimal L4L-specific training), who can flexibly use the material over their preferred duration throughout the school year, and integrated with standard school programming.
An important aspect of the L4L intervention was the development of age-appropriate lesson materials, particularly the online graphic novel, which are interactive and illustrate learning concepts around stress management, sleep hygiene and nutrition. There is a need for digital health platforms to develop their content and messaging so that it is appropriate for their audience. In particular, there is a need for these platforms to adequately address the needs of at-risk, low literacy, or underserved populations, who may be more likely to experience health disparities and who may benefit from health interventions (Jacobs et al., 2016).
5. Conclusions
There is a current and pressing need for high-quality, comprehensive, and cost-effective interventions to address 9–14 year old children’s DHL and promote healthy lifestyle behaviours. Such interventions have the potential to increase children’s health-related skills and behaviours in the short-term. The L4L intervention is one such possibility and we have demonstrated its potential in increasing students’ DHL and positively influencing their health knowledge and behaviours. Future implementations of the L4L intervention will need to consider a longer duration of the intervention and repeating measurements after a longer follow-up.
6. Submission declaration
The work described in this submission has not been published previously, is not considered for publication elsewhere, is approved by all authors, and will not be published elsewhere.
7. Ethics approval and consent to participate
The University of British Columbia’s Behavioural Research Ethics Board gave ethical approval for the conduct of the study (H17-01195). Each school and its school district gave approval for the delivery of the L4L intervention and the conduct of the research activities. All student participants assented to participating in the research and their parents/legal guardians provided informed consent.
8. Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
9. Authors’ contributions
AH assisted with data collection, data analysis, and writing the manuscript. KS assisted with the statistical analyses and writing the manuscript. AMJ, HNL, ES, GK and KH assisted with project planning, data collection, and reviewing and editing the manuscript. All authors read and approved the final manuscript.
Funding
Provided by the Lawson Foundation (Canada; grant number: 20R75337). The funder had no role in the design of the study, collection, analysis, or interpretation of the data, writing the manuscript, or decision to submit for publication.
Conflict of interest
The authors have none to declare.
Acknowledgments
We are incredibly grateful to the time and effort put in by the teachers, administrators, and other school staff to help facilitate the conduct of this study. We wish to thank the many stakeholders that contributed their expertise to developing the Learning for Life intervention. And, lastly, we thank the many students that participated in the research study and Learning for Life intervention and provided their feedback.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101149.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann. Intern. Med. 2011;155:97. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Borzekowski D.L.G. Considering children and health literacy: a theoretical approach. Pediatrics. 2009;124(Suppl):S282–S288. doi: 10.1542/peds.2009-1162D. [DOI] [PubMed] [Google Scholar]
- Buckhalt J.A., El-Sheikh M., Keller P.S., Kelly R.J. Concurrent and longitudinal relations between children’s sleep and cognitive functioning: the moderating role of parent education. Child Dev. 2009;80:875–892. doi: 10.1111/j.1467-8624.2009.01303.x. [DOI] [PubMed] [Google Scholar]
- Campbell J.A., Walker R.J., Egede L.E. Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. Am. J. Prev. Med. 2016;50:344–352. doi: 10.1016/j.amepre.2015.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson V., Hunter S., Kuzik N., Gray C.E., Poitras V.J., Chaput J.-P., Saunders T.J., Katzmarzyk P.T., Okely A.D., Connor Gorber S., Kho M.E., Sampson M., Lee H., Tremblay M.S. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl. Physiol. Nutr. Metab. 2016;41:S240–S265. doi: 10.1139/apnm-2015-0630. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2011. School health guidelines to promote healthy eating and physical activity.
- Chahal H., Fung C., Kuhle S., Veugelers P.J. Availability and night-time use of electronic entertainment and communication devices are associated with short sleep duration and obesity among Canadian children. Pediatr. Obes. 2013;8:42–51. doi: 10.1111/j.2047-6310.2012.00085.x. [DOI] [PubMed] [Google Scholar]
- Colley, R.C., Clarke, J., Doyon, C.Y., Janssen, I., Lang, J.J., Timmons, B.W., Tremblay, M.S., 2019. Trends in physical fitness among Canadian children and youth. Heal. Reports. Doi:10.25318/82-003-x201901000001-eng. [DOI] [PubMed]
- Colley R.C., Garriguet D., Janssen I., Craig C.L., Clarke J., Tremblay M.S. Physical activity of Canadian children and youth: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Heal. Rep. 2011;22:15–23. [PubMed] [Google Scholar]
- Coyne I., Harder M. Children’s participation in decision-making. J. Child Heal. Care. 2011;15:312–319. doi: 10.1177/1367493511406570. [DOI] [PubMed] [Google Scholar]
- DeWalt D.A., Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124:S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- Diamond C., Saintonge S., August P., Azrack A. The development of building wellnessTM, a youth health literacy program. J. Health Commun. 2011;16(Suppl 3):103–118. doi: 10.1080/10810730.2011.604385. [DOI] [PubMed] [Google Scholar]
- Doucet G., Beatty M. The cost of diabetes in canada: the economic Tsunami. Can. J. Diabetes. 2010;34:27–29. doi: 10.1016/S1499-2671(10)41005-9. [DOI] [Google Scholar]
- Fagnano M., Halterman J.S., Conn K.M., Shone L.P. Health literacy and sources of health information for caregivers of urban children with asthma. Clin. Pediatr. (Phila) 2012;51:267–273. doi: 10.1177/0009922811421413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faught E.L., Ekwaru J.P., Gleddie D., Storey K.E., Asbridge M., Veugelers P.J. The combined impact of diet, physical activity, sleep and screen time on academic achievement: a prospective study of elementary school students in Nova Scotia, Canada. Int. J. Behav. Nutr. Phys. Act. 2017;14:29. doi: 10.1186/s12966-017-0476-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleary S.A., Joseph P., Pappagianopoulos J.E. Adolescent health literacy and health behaviors: a systematic review. J. Adolesc. 2018;62:116–127. doi: 10.1016/j.adolescence.2017.11.010. [DOI] [PubMed] [Google Scholar]
- Gruber R., Carrey N., Weiss S.K., Frappier J.Y., Rourke L., Brouillette R.T., Wise M.S. Position statement on pediatric sleep for psychiatrists. J. Can. Acad. Child Adolesc. Psychiatry. 2014;23:174–195. [PMC free article] [PubMed] [Google Scholar]
- Hills A.P., Dengel D.R., Lubans D.R. Supporting public health priorities: recommendations for physical education and physical activity promotion in schools. Prog. Cardiovasc. Dis. 2015;57:368–374. doi: 10.1016/j.pcad.2014.09.010. [DOI] [PubMed] [Google Scholar]
- Jacobs R.J., Lou J.Q., Ownby R.L., Caballero J. A systematic review of eHealth interventions to improve health literacy. Health Informatics J. 2016;22:81–98. doi: 10.1177/1460458214534092. [DOI] [PubMed] [Google Scholar]
- Ministry of Education, 2018. Physical & Health Education Curriculum [WWW Document].
- Mitsutake S., Shibata A., Ishii K., Oka K. Associations of eHealth literacy with health behavior among adult internet users. J. Med. Internet Res. 2016;18 doi: 10.2196/jmir.5413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman C.D., Skinner H.A. eHealth literacy: essential skills for consumer health in a networked world. J. Med. Internet Res. 2006;8 doi: 10.2196/jmir.8.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman C.D., Skinner H.A. eHEALS: the eHealth literacy scale. J. Med. Internet Res. 2006;8 doi: 10.2196/jmir.8.4.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paakkari O., Torppa M., Villberg J., Kannas L., Paakkari L. Subjective health literacy among school-aged children. Health Educ. 2018;118:182–195. doi: 10.1108/HE-02-2017-0014. [DOI] [Google Scholar]
- Paasche-Orlow M.K., Wolf M.S. Promoting health literacy research to reduce health disparities. J. Health Commun. 2010;15(Suppl 2):34–41. doi: 10.1080/10810730.2010.499994. [DOI] [PubMed] [Google Scholar]
- Park H., Moon M., Baeg J.H. Association of eHealth literacy with cancer information seeking and prior experience with cancer screening. Comput. Informatics, Nurs. 2014;32:458–463. doi: 10.1097/CIN.0000000000000077. [DOI] [PubMed] [Google Scholar]
- Ponti, M., Digital Health Task Force, 2019. Digital media: Promoting healthy screen use in school-aged children and adolescents [WWW Document]. URL https://www.cps.ca/en/documents/position/digital-media (accessed 6.11.19). [DOI] [PMC free article] [PubMed]
- SCOPE, 2019. About Live 5-2-1-0 [WWW Document]. URL https://www.live5210.ca/about-live-5-2-1-0/ (accessed 6.1.19).
- Smith, A., Forsyth, K., Poon, C., Peled, M., Saewyc, E., McCreary Centre Society, 2019. Balance and connection in BC: The health and well-being of our youth. Vancouver, BC.
- Statistics Canada, 2017. Canadian Community Health Survey - Nutrition [WWW Document]. URL https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1310079701 (accessed 10.10.19).
- Straker L., Zabatiero J., Danby S., Thorpe K., Edwards S. Conflicting guidelines on young children’s screen time and use of digital technology create policy and practice dilemmas. J. Pediatr. 2018;202:300–303. doi: 10.1016/j.jpeds.2018.07.019. [DOI] [PubMed] [Google Scholar]
- Taverno Ross S.E., Byun W., Dowda M., McIver K.L., Saunders R.P., Pate R.R. Sedentary behaviors in fifth-grade boys and girls: where, with whom, and why? Child. Obes. 2013;9:532–539. doi: 10.1089/chi.2013.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay M.S., Leblanc A.G., Janssen I., Kho M.E., Hicks A., Murumets K., Colley R.C., Duggan M. Canadian sedentary behaviour guidelines for children and youth. Appl. Physiol. Nutr. Metab. 2011;36(59–64):65–71. doi: 10.1139/H11-012. [DOI] [PubMed] [Google Scholar]
- Tremblay M.S., LeBlanc A.G., Kho M.E., Saunders T.J., Larouche R., Colley R.C., Goldfield G., Gorber S. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2011;8:98. doi: 10.1186/1479-5868-8-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Cauter E., Knutson K.L. Sleep and the epidemic of obesity in children and adults. Eur. J. Endocrinol. 2008;159:S59–S66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkelman T.N.A., Caldwell M.T., Bertram B., Davis M.M. Promoting health literacy for children and adolescents. Pediatrics. 2016;138:e20161937. doi: 10.1542/peds.2016-1937. [DOI] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Copenhagen: 2016. Growing up unequal: gender and socioeconomic differences in young people’s health and well-being. [Google Scholar]
- World Health Organization, 2015. Interim Report of the Commission on Ending Childhood Obesity.
- Yavuz H.M., van Ijzendoorn M.H., Mesman J., van der Veek S. Interventions aimed at reducing obesity in early childhood: a meta-analysis of programs that involve parents. J. Child Psychol. Psychiatry. 2015;56:677–692. doi: 10.1111/jcpp.12330. [DOI] [PubMed] [Google Scholar]
- Zibrik L., Khan S., Bangar N., Stacy E., Novak Lauscher H., Ho K. Patient and community centered eHealth: Exploring eHealth barriers and facilitators for chronic disease self-management within British Columbia’s immigrant Chinese and Punjabi seniors. Heal. Policy Technol. 2015;4:348–356. doi: 10.1016/j.hlpt.2015.08.002. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.