Abstract
Background
Our study aimed to explore the anxiety levels and possible associated factors in the pediatric medical staff in Jiangsu province during an outbreak of Coronavirus Disease 2019 (COVID-19).
Methods
Pediatric medical staff (n=534) from nine hospitals in Jiangsu province were enrolled. Their anxiety levels and quality of sleep were assessed using the online SAS and PSQI questionnaires.
Results
The prevalence of anxiety was 14.0% among the medical staff. In children’s hospital staff, anxiety levels in outpatient and emergency departments were significantly higher than those in inpatient departments, except for the intensive care unit. The SAS scores were significantly associated with educational background, professional title, lifestyle, and physical condition. Stepwise multiple linear regression showed that physical condition, lifestyle, attention to the epidemic, professional title, and educational background all had a linear relationship with the individual’s anxiety levels. Pearson correlation analysis showed that sleep quality was moderately associated with anxiety levels.
Conclusions
The prevalence of anxiety was 14.0% in pediatric medical staff in Jiangsu province during an outbreak of COVID-19. Department, professional title, and educational background were associated with anxiety levels in these workers. More attention should be paid to staff who are in poor health, and this anxiety can also be accompanied by poor sleep quality. Peer support can assist with anxiety relief.
Keywords: Pediatrics, medical staff, anxiety, sleep quality, psychological problem
Introduction
In December 2019, an outbreak of COVID-19 occurred in Wuhan, China, and then spread quickly throughout the country. As of February 11, 2020, 44,730 patients with COVID-19 were confirmed in China, of whom 1,114 had died. Cases were later reported in more than 20 countries worldwide. The World Health Organization (WHO) designated COVID-19 as an emergent public health event on January 20, 2020. In the face of such a rapidly spreading infectious disease, the physical and mental health of medical staff might be threatened. According to the statistics from 422 medical institutions, 3,019 medical workers were infected, and 1,716 of them were confirmed by nucleic acid analysis (1). Currently, domestic health agencies are paying close attention to the isolation and prevention of COVID-19 among medical staff. However, Xiang et al. (2) pointed out that the mental health of the COVID-19-associated population, mainly the medical staff, has received less attention. During the outbreak of severe acute respiratory syndrome and the Middle East respiratory syndrome, many studies reported that medical staff appeared to suffer from several long-lasting psychological problems, including anxiety and panic attacks, and even developed physiological symptoms (3,4). For COVID-19, there have been no reports with extensive sample size surveys of the medical staff’s mental health status. Therefore, this cross-sectional study aimed to focus on anxiety and its associated factors in pediatric medical staff from Jiangsu province during the outbreak of COVID-19. The present study also aimed to supply a basis for targeted psychological intervention measures.
Methods
Participants
Pediatric medical staff from four children’s hospitals and five comprehensive hospitals in Jiangsu province were enrolled in this survey from February 9th to the 13th, 2020. All respondents had performed their regular on-the-job duties for nearly a month, and those who had ever had any mental illness before were excluded. Five hundred and thirty-four valid questionnaires were completed, including 289 from doctors and 245 from nurses. Among them, 419 questionnaires were completed by staff from four children’s hospitals, divided into respiratory medicine departments, infectious disease departments, outpatients and emergency departments, intensive care, and another group (such as kidney, digestive, and other departments) forming a total of five groups. Staff from comprehensive hospitals completed 115 questionnaires and were included in the general pediatric group.
Research methods
This study adopted an online questionnaire survey. Each unit had one person in charge to inform all the staff of the purpose of the questionnaire. All staff received simple training and had to complete the questionnaire independently to avoid interference. The questionnaire included four parts: general status, epidemic concern, self-rating anxiety scale (SAS) (5), and the Pittsburgh sleep quality index (PSQI) (6). General status included gender, age, educational background, professional title, lifestyle, with/without children, and physical condition. SAS assessed the feelings of anxiety of the respondents in the past week. A standard score of ≥50 showed that there might be anxiety, a score of 50–59 indicated mild anxiety, 60–69 indicated moderate anxiety, and ≥70 indicated severe anxiety. PSQI assessed the sleep quality of the respondents in the past month. The higher the score, the worse the sleep quality, while a score >7 showed that there was poor sleep quality.
Statistical methods
SPSS 23.0 statistical software (IBM Corp., Armonk, NY, USA) was used for data processing. The measurement data were expressed by x±s, and the homogeneity of normal distribution and variance were evaluated. A t-test was used for comparison between two groups, and the least significant difference (LSD) test or Kruskal-Wallis rank-sum test was used for comparisons among multiple groups. Pearson linear correlation analysis was used to analyze the relationship between two factors. Stepwise multiple linear regression analysis was used to evaluate the associated factors of anxiety. The standard of significance was P<0.05.
Results
Concerns and opinions on the epidemic situation
In this survey, no respondents chose to pay only occasional attention to the epidemic, 219 (41.0%) respondents chose to pay significant attention to the epidemic, 196 respondents (36.7%) chose to pay close attention to it as long as they had time, and 143 people (26.6%) thought about the epidemic for more than 3 hours per day. No respondents thought that the epidemic was not serious, 209 respondents (39.1%) thought it was severe, and 272 respondents (50.9%) thought it was very severe.
The relationship between departments and anxiety level
Among 534 medical staff, the average SAS standard score was 39.34±9.30, 75 people (14.0%) had anxiety, of whom 57 (10.7%) had mild anxiety, 14 (2.6%) had moderate anxiety, and 4 (0.7%) had severe anxiety. There was no significant difference in the proportion of doctors and nurses with anxiety between departments (χ2=18.667, P<0.05); however, there was a significant difference in anxiety level between departments (F=32.550, P<0.01). Among them, in children’s hospitals, the anxiety level of outpatient and emergency staff was significantly higher than that of the staff of respiratory medicine departments, infectious disease departments, and another group (P<0.05). The anxiety level of the general pediatric group was also higher than that in the respiratory and another group (P<0.05). Table 1 shows the specific personnel distribution and anxiety scores.
Table 1. Comparison of department distribution and anxiety level of survey objects.
| Department | n | Doctors/nurses | SAS standard score |
|---|---|---|---|
| Respiratory medicine department | 62 | 28/34 | 36.19±8.05 |
| Infectious diseases department | 71 | 34/37 | 37.43±8.15 |
| Outpatient and emergency | 100 | 47/53 | 42.18±9.11a |
| Intensive care | 79 | 38/41 | 40.62±10.55 |
| Another group | 107 | 71/36 | 36.85±7.20 |
| General pediatric | 115 | 71/44 | 41.21±10.37b |
| χ2/F | 18.667 | 32.550 | |
| P | 0.005 | <0.001 |
a, compared with group 1, 2, and 5, P<0.05; b, compared with group 1 and group 5, P<0.05.
The relationship between the respondents’ typical characteristics and anxiety levels
The results showed that there was no significant difference in anxiety levels between doctors and nurses, and there was no significant difference between genders, those with/without children, or role Anxiety levels increased first and then decreased with age, education, and professional title, and the difference was statistically significant (P<0.05). For lifestyle factors, the score of living together with colleagues was significantly lower than that of living alone or with family (P<0.05). There was a significant difference in anxiety levels among the groups with different physical conditions (P<0.05): The worse the respondent’s physical condition, the higher their level of anxiety. Table 2 shows the specific results.
Table 2. Comparison of typical characteristics and anxiety level of respondents.
| Item | n | SAS standard score | t/F | P |
|---|---|---|---|---|
| Occupation | 0.963 | 0.336 | ||
| Doctor | 289 | 38.99±9.22 | ||
| Nurse | 245 | 39.77±9.40 | ||
| Gender | 0.569 | 0.569 | ||
| Male | 94 | 39.84±9.12 | ||
| Female | 440 | 39.24±9.34 | ||
| Age (years) | 1.800 | 0.146 | ||
| 20–30 | 197 | 39.17±10.02 | ||
| 31–40 | 237 | 40.20±8.90a | ||
| 41–50 | 72 | 37.57±9.04 | ||
| >50 | 28 | 39.34±9.30 | ||
| Education | 7.501 | 0.024 | ||
| Junior college | 66 | 38.43±8.66 | ||
| Bachelor | 303 | 40.50±10.15a | ||
| Master or above | 165 | 37.59±7.46 | ||
| Positional title | 5.668 | 0.004 | ||
| Junior or below | 250 | 39.20±9.72 | ||
| Intermediate | 187 | 40.80±9.26a | ||
| Senior | 97 | 36.93±7.68 | ||
| Post | 0.888 | 0.375 | ||
| General | 489 | 39.45±9.44 | ||
| Manager | 45 | 38.17±7.58 | ||
| Living style | 8.488 | 0.014 | ||
| Alone | 55 | 41.61±10.97 | ||
| Family | 410 | 39.50±9.21 | ||
| Dormitory | 69 | 36.65±7.76b | ||
| Children | 0.831 | 0.407 | ||
| No | 200 | 38.91±9.78 | ||
| Yes | 334 | 39.60±9.00 | ||
| Physical condition | 26.825 | <0.001 | ||
| Quite good | 177 | 36.22±7.86c | ||
| Good | 238 | 39.10±8.35c | ||
| Common | 106 | 43.36±10.34c | ||
| Bad | 13 | 53.55±10.80c | ||
a, compared with the third group, P<0.05; b, compared with group 1 and 2, P<0.05; c, there were significant differences among all groups (P<0.05).
Stepwise multiple linear regression analysis of the factors related to anxiety levels
A stepwise multiple linear regression model was established with the anxiety level of the respondents as the dependent variable, and the general status, attention to the epidemic, and their department as the independent variables (Input F≤0.050, removed F≥0.100). There was a linear relationship between physical condition, lifestyle, attention to the epidemic, professional title, educational background, and anxiety level (P<0.05). Table 3 shows the specific results.
Table 3. Multiple linear regression analysis of factors related to anxiety level.
| Item | B | SE | β | t | P |
|---|---|---|---|---|---|
| Constant | 33.951 | 3.600 | – | 9.430 | <0.001 |
| Physical condition | 4.035 | 0.472 | 0.342 | 8.546 | <0.001 |
| Living style | –2.506 | 0.783 | –0.130 | –3.198 | 0.001 |
| Attention to the epidemic | 1.982 | 0.617 | 0.131 | 3.214 | 0.001 |
| Positional title | –1.308 | 0.525 | –0.106 | –2.493 | 0.013 |
| Education | –1.209 | 0.607 | –0.082 | –1.993 | 0.047 |
Correlation between sleep quality and anxiety levels
The average PSQI score of the 534 medical staff was 6.07±3.40. The PSQI score of 160 respondents (30.0%) was more than 7, showing poor sleep quality. The score of items in the scale also showed that 196 staff had difficulty falling asleep, and 82 staff had low sleep efficiency. Pearson linear correlation was used to analyze the relationship between anxiety levels and sleep quality. The results showed that anxiety levels were correlated moderately with sleep quality (r=0.544, Figure 1).
Figure 1.
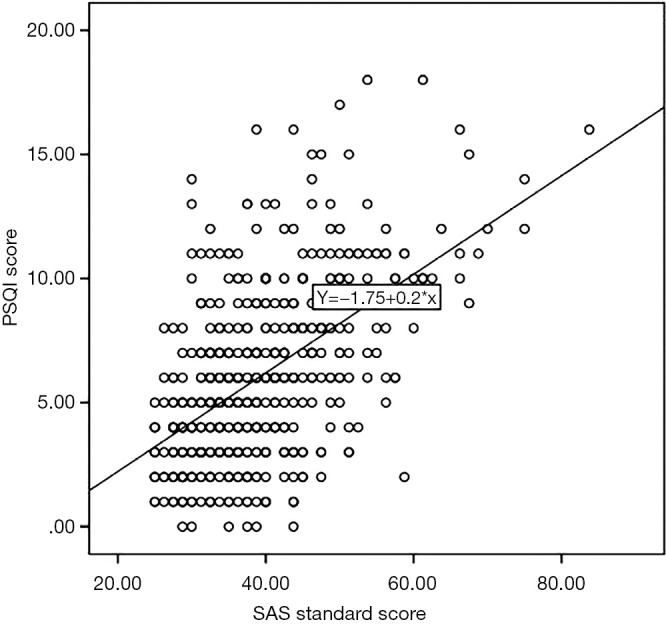
Correlation Analysis between Sleep quality and anxiety level.
Discussion
The pathogen of COVID-19 is severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a new type of β-coronavirus. It is transmitted through respiratory droplets and close contact. Its R0 value is predicted to be higher than that of SARS CoV (7). In this survey, 50.9% of the medical staff thought the epidemic was very severe. There was a linear relationship between their attention to the epidemic and their anxiety level (P<0.05). COVID-19 has posed a threat to the mental health of these medical staff.
As of February 11, 2020, 956 cases under the age of 20 have been reported by Chinese medical institutions (1). The clinical characteristics of pediatric cases are different from adults (8), although this difference is not fully understood at present. Asymptomatic patients and those who are in the incubation period are also known to be infectious, and 1 or 2 family members usually accompany pediatric patients; therefore, the possibility of transmission is further increased. All these factors have threatened the health of and challenged the mental resilience of pediatric medical staff. Stress events can cause significant anxiety. During the epidemic period, medical staff might have anxiety about their illness and whether they could spread the virus to their families and friends.
Earlier studies showed that the anxiety level of medical staff was significantly higher than the national norm (9,10). However, little data for pediatric medical staff have been published. During the COVID-19 outbreak, we conducted an online SAS questionnaire survey of 534 pediatric medical staff. The results showed that 14% of them had anxiety, with most having mild anxiety. The anxiety level of the staff in outpatient and emergency departments was significantly higher than that in respiratory medicine departments, infectious disease departments, and another group. This phenomenon was related to the large numbers of child patients and their families, the intensity of the work, and the noisy working environment.
In Jiangsu Province, once the novel coronavirus pneumonia was diagnosed, the designated hospital for treatment of COVID-19 was a local infectious disease hospital. The patients in the respiratory medicine departments and other departments were screened through the outpatient and emergency departments. In the other departments, the possibility of disease transmission is reduced; therefore, the level of anxiety is lower than that in outpatient and emergency. The anxiety levels of the general pediatric staff were also higher, which might be related to the following factors: (I) the general pediatric staff needs to rotate to the outpatient and emergency department; and (II) the incidence of COVID-19 in adults is higher than that in children, and the risk of exposure is higher in comprehensive hospitals.
In the survey, anxiety levels were also associated with age, education, and professional title and were shown to have a trend of first increasing and then decreasing. Multiple linear regression analysis showed that there was a linear relationship between educational background and anxiety. The probable causes include: (I) different knowledge levels; (II) different departmental work responsibilities; (III) some staff may be in the rising stage of their career, with more competitive pressure; and (IV) different family and social pressures. In this survey, the anxiety level of medical staff living with colleagues was significantly lower than that of those living alone or with their family. These findings have suggested that communication between colleagues can be a protective emotional factor, which could buffer stress. The research by Ye et al. (11) showed that social support favored supporting mental health. Physical condition was closely related to the level of anxiety during the epidemic. The worse the individual’s physical quality, the higher their level of anxiety. Thus, we need to consider the anxiety caused by physical discomfort. Furthermore, we cannot exclude the possibility that the higher incidence and mortality of COVID-19 occurred in the population with underlying diseases.
Among the respondents, 30% had poor sleep quality, and their level of anxiety was moderately associated with sleep quality. Several studies showed that anxiety could be accompanied by significant sleep changes (12,13). Stewart et al. showed that negative emotions such as anxiety could control the central secretion of 5-hydroxytryptamine, prolonging the time of falling asleep or reducing the depth of sleep (13). By contrast, poor sleep quality could aggravate anxiety via mutual cause and effect, forming a vicious circle.
Long-term high anxiety levels of medical staff are likely to be accompanied by physical symptoms and cognitive changes that will affect work attitude and efficiency, and interpersonal relations; therefore, there is an urgent need to carry out a timely mental health assessment for medical staff affected by the COVID-19 epidemic. The survey results of 534 pediatric medical staff showed that levels of anxiety were higher in staff from outpatient and emergency departments and those with a bachelor’s degree. Anxiety can be accompanied by poor sleep quality, and peer support can alleviate anxiety. We hope that the results of the present study will supply the basis for professional mental health guidance services. This study involved a limited number of hospitals. As a cross-sectional survey, it had no data on the basic anxiety levels of pediatric medical staff. Therefore, we propose to use the SAS questionnaire again after the outbreak.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: The research was funded by Research project of China Disabled Persons’ Federation (2019&ZC006) and Suzhou emergency control technology special project of SARS-COV-2 (SYS2020028).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Institutional Review Board approved this study of Children’s Hospital of Soochow University (NO.2020-21).
Footnotes
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tp.2020.04.02). The authors have no conflicts of interest to declare.
References
- 1.Epidemiology Working Group for NCIP Epidemic Response . The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chinese Journal of Epidemiology 2020;41:145-51.32064853 [Google Scholar]
- 2.Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020;7:228-9. 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 2009;54:302-11. 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alsubaie S, Hani Temsah M, Al-Eyadhy AA, et al. Middle East Respiratory Syndrome Coronavirus epidemic impact on healthcare workers' risk perceptions, work and personal lives. J Infect Dev Ctries 2019;13:920-6. 10.3855/jidc.11753 [DOI] [PubMed] [Google Scholar]
- 5.Zung WW. A Rating Instrument For Anxiety Disorders. Psychosomatics 1971;12:371-9. 10.1016/S0033-3182(71)71479-0 [DOI] [PubMed] [Google Scholar]
- 6.Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193-213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 7.Chen J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect 2020;22:69-71. 10.1016/j.micinf.2020.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen ZM, Fu JF, Shu Q, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr 2020. [Epub ahead of print]. 10.1007/s12519-020-00345-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.He YJ, Lu MM, Chen GM, et al. Correlation between anxiety among public hospital medical personnel and social support, perceived social support and coping styles. Chin J Dis Control Prev 2019;23:328-31. [Google Scholar]
- 10.Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: A systematic review and meta-analysis. JAMA 2015;314:2373-83. 10.1001/jama.2015.15845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ye LY, Li J, Wu MD. The effect of social support on coping style and quality of life of elderly patients with coronary heart disease. Pract Prev Med 2018,25:863-5. [Google Scholar]
- 12.Zhang WJ, Yan C, Shum D, et al. Responses to academic stress mediate the association between sleep difficulties and depressive/anxiety symptoms in Chinese adolescents. J Affect Disord 2020;263:89-98. 10.1016/j.jad.2019.11.157 [DOI] [PubMed] [Google Scholar]
- 13.Stewart JC, Rand KL, Hawkins Misty AW, et al. Associations of the shared and unique aspects of positive and negative emotional factors with sleep quality. Pers Individ Dif 2011;50: 609-14. 10.1016/j.paid.2010.12.004 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


