Abstract
A 78-year-old man with no surgical history or recent trauma presented to the emergency department with sudden onset right-sided chest pain and dyspnoea. He was admitted under the physicians for investigations and was subsequently diagnosed with empyema of the right thorax. After no improvement with intravenous antibiotics, a chest drain was inserted; no pus was drained. He worsened clinically; a repeated CT scan demonstrated an incarcerated loop of small bowel within the right thoracic cavity secondary to a diaphragmatic hernia (DH). The patient had emergency surgery to remove necrotic small bowel and to lavage the thorax. Strangulated DH should be considered as a differential diagnosis where presentation is unusual and empyema does not improve after initial management.
Keywords: empyema, surgery, gastrointestinal surgery, general surgery, radiology
Background
Diaphragmatic hernia (DH) is rarely seen clinically. Strangulation is a serious complication which puts the patient at high risk of mortality without surgical intervention.1 2 Early diagnosis can be difficult.
Most present with abdominal pain and vomiting;1 3 DH can be congenital or caused by direct trauma to, or surgery involving, the diaphragm, thorax or abdomen.2 3
Case presentation
A 78-year-old man presented to the emergency department with a 2-day history of sharp right-sided chest pain and dyspnoea. There was no history of trauma, he denied abdominal pain or vomiting. His medical history was unremarkable, with no previous surgeries.
Chest examination revealed bronchial breathing at the right base. His C-reactive protein and white blood cells were elevated measuring 267 mg/L and 16×109/L, respectively. Based on his presentation, clinical examination and imaging (figure 1), demonstrating an air–fluid level in the right basal pleura, the patient was admitted under the medical team and treated with intravenous antibiotics for presumed right basal pneumonia and empyema.
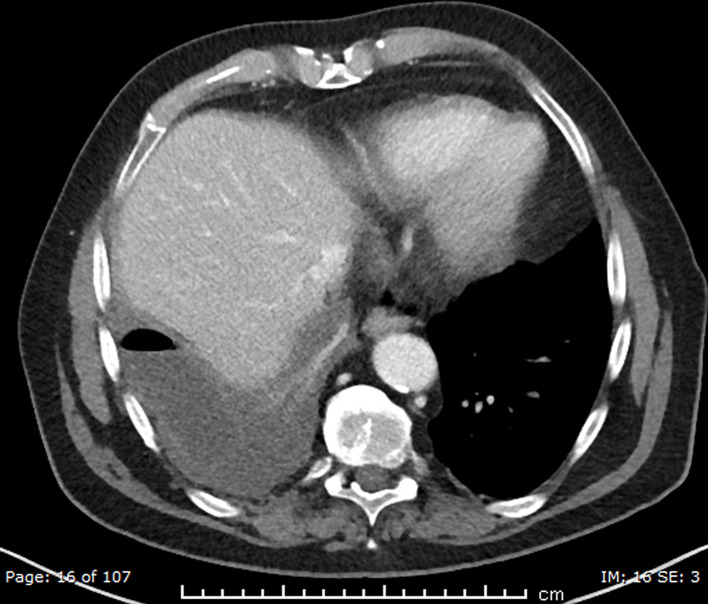
Figure 1.
Initial CT scan on admission: raised right haemidiaphragm with right basal effusion with an air–fluid level and consolidation.
After 4 days of treatment, there was no clinical improvement. Ultrasound-guided aspiration of the right pleural cavity was performed. Blood-stained serosanguinous fluid was aspirated, however there was no pus. A chest drain was inserted, and the patient was continued on intravenous antibiotics. After treatment with multiple antibiotics including piperacillin/tazobactam, metronidazole and gentamicin for a total of 10 days, there was still no clinical improvement. His inflammatory markers remained significantly raised and he had now developed abdominal pain and mild distension. This was thought to be a paralytic ileus.
The patient had a nasogastric tube inserted and was monitored for 3 more days; he became increasingly septic. His chest drain had been removed given no improvement in clinical picture. Another CT scan (figure 2) now demonstrated small bowel obstruction with a likely transition point in the right hypochondrium; air–fluid levels were seen in the right thorax.
Figure 2.

Repeated CT scan: coronal plane: right diaphragmatic hernia containing a necrotic loop of small bowel in right haemithorax.
The patient underwent an emergency laparotomy. The liver was retracted inferiorly revealing a 2×2 cm defect in the lateral aspect of the right diaphragm through which a 30 cm segment of small bowel has herniated through into the right thoracic cavity. On retrieval of the herniated contents, a necrotic loop of small bowel was discovered along with approximately 600 mL of liquid stool (figure 3). The necrotic bowel was resected, an end ileostomy was fashioned. Thorough saline lavage of the thoracic cavity was performed and two chest drains were reintroduced. The diaphragmatic defect was closed with non-absorbable sutures. Postoperatively he was transferred to Intensive therapy unit (ITU) for organ support. After 2 months, he was discharged home.
Figure 3.
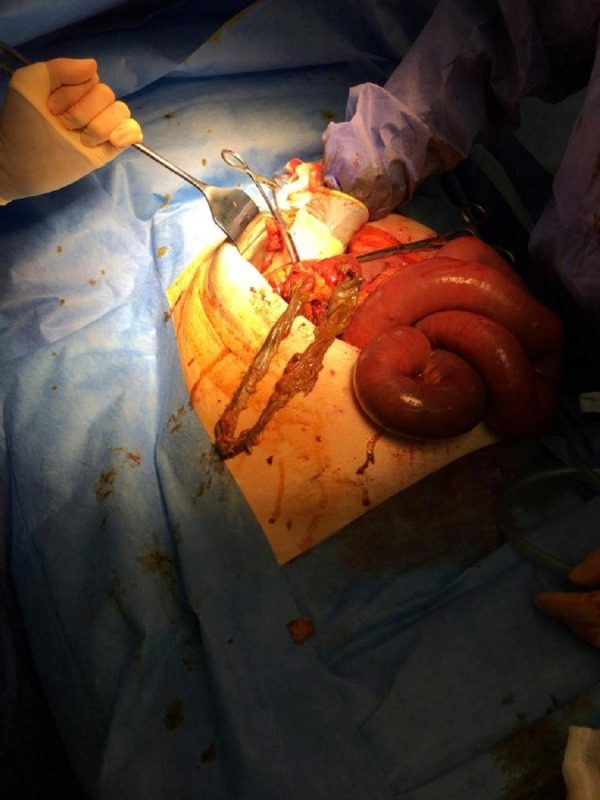
Intraoperative findings: necrotic small bowel removed from the right side of the chest.
Review of the initial CT scan showed subtle signs of a small right DH which was not identified in the first instance.
Investigations
Initial blood tests demonstrated raised inflammatory markers suggestive of bacterial infection. Chest X-ray was performed, identifying right-sided consolidation with effusion.
A CT thorax demonstrated a right basal consolidation and empyema with air–fluid level. The right haemidiaphragm was not initially visualised which in hindsight could have suggested a DH.
Pleural fluid sent for microbiology had no growth.
Repeated CT imaging showed atelectasis of the right upper and lower lobes and a large pleural effusion. Small bowel obstruction was demonstrated with the transition point in the right upper quadrant with an incarcerated DH and abnormal loops of bowel occupying most of the right side of the thorax.
Differential diagnosis
Given the raised inflammatory markers and imaging results, the diagnosis of severe pneumonia or thoracic empyema was the most likely.
The initial lack of abdominal signs and symptoms on admission excluded an obvious surgical differential.
The diagnosis of DH with bowel strangulation was not clear until the CT scan was repeated on day 13 of admission.
Treatment
After failed medical management and eventual confirmation of the diagnosis of strangulated DH, the patient underwent an emergency laparotomy. The hernia was defined and its contents were reduced with resection of necrotic small bowel, lavage of the gross faecal contamination of the pleural cavity and suture closure of the diaphragmatic defect.
Outcome and follow-up
Unsurprisingly, the elderly patient had a prolonged ITU stay for organ support. Postdischarge, he received stoma care and ongoing rehabilitation in the community.
Discussion
Bochdalek hernia (BH) is the most common type of DH (85% of total cases). They result from failure of fusion of the pleuroperitoneal canal during fetal development and as consequence from a posterior–lateral diaphragmatic defect.4
Most BHs present in infancy with an incidence of 1 in 4000,5 6 but 5%–25% are discovered later in life. Some present in adulthood7 8 or as an incidental finding on imaging studies.9
At birth or early infancy, BH presents with life-threatening respiratory distress.10 Symptomatic adults present with vague gastrointestinal problems that include abdominal pain, vomiting and postprandial fullness. Less commonly, patients present with respiratory symptoms9 including chest pain, dyspnoea, pleural effusion6 9 and breathlessness which can often be mistaken for pneumonia, especially when there is no history of injury.
Symptomatic BH most often occurs on the left5 6 whereas right-sided BH (30%) is rarely reported in the literature. Right-sided BH is thought to be less common due to the right pleuroperitoneal canal closing earlier in development and the reduced risk of abdominal viscera protrusion by the liver underpinning the right diaphragm.5 6 9 However, right-sided BH has been found coincidentally; a large retrospective study of over 13 000 abdominal CT scans demonstrated a prevalence of 0.17%.11 Interestingly, incidental asymptomatic BH appears to be predominantly right sided,6 9 possibly due to the protective barrier formed by the liver. On development of symptoms, however, right-sided herniation is usually associated with only respiratory symptoms, as seen in the patient discussed in this case report (until strangulation occurred). Most concerning is that a late presenting right-sided hernia is almost always associated with bowel strangulation.5
Chest X-ray and CT imaging studies should be considered if the diagnosis of DH is suspected.5 7 9 The classic findings of DH on chest X-ray are an air–fluid level or a gastric tube coiled in the chest. Incorrect interpretation of the chest X-ray is frequent, however, a normal chest X-ray does not exclude DH.9 The rare finding of dilated bowel above the haemidiaphragm makes the diagnosis more obvious.12 It was unclear in this patient if the bowel perforation was a result of chest drain insertion, given the clinical timeline ischaemic perforation remains more likely.
CT and MRI can be used to evaluate the location, size and contents of the diaphragmatic defect. Neither modality is perfect. CT has a reported sensitivity and specificity of 14%–82% and 87%, respectively. CT scans have detection sensitivities of 78% for left-sided hernias and 50% for right-sided hernias.7
Unfortunately, the difficulty obtaining a timely diagnosis can lead to the mortality being high in those who have an emergency presentation, often due to inevitable bowel strangulation.6 Laparotomy with or without thoracotomy can be used to repair the defect. Successful laparoscopic and thoracoscopic repairs of BH have been reported, but with limited application in cases of right-sided BH.7 Incidental large BH should be repaired due to potential associated risks including bowel strangulation and resultant fatality.9
In summary, right-sided BHs in adults are rare entities. Diagnosis can be difficult due to a wide range of presenting symptoms and non-specific imaging signs. These hernias are frequently associated with bowel strangulation, therefore prompt diagnosis is essential for early surgical management and improved patient outcome.
Learning points.
Strangulated diaphragmatic hernia (DH) should be considered as a diagnosis in patients presenting with atypical chest pain or respiratory compromise and an atypical response to initial medical management.
Consider an early surgical review in such patients especially when signs of obstruction are developing.
Careful interpretation of imaging is essential. A high index of suspicion by clinicians and radiologists is needed. DH can be easily missed clinically and radiologically, with potentially dire consequences.
An early repeated CT chest and abdomen should be considered if the first scan is inconclusive or does not relate with the clinical findings.
Consider DH as an underlying or differential diagnosis prior to insertion of chest drains in severe empyema.
Footnotes
Contributors: SG: writing case report, planning, conduct, design. DW: acquisition of data, editing. LS: acquisition of data, design. GLW: planning, conception, editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Carter R, Brewer LA. Strangulating diaphragmatic hernia. Ann Thorac Surg 1971;12:281–90. 10.1016/S0003-4975(10)65126-0 [DOI] [PubMed] [Google Scholar]
- 2.Sun Y, Yin L, Xue H, et al. Unusual delayed presentation of diaphragmatic hernia complicated by transverse colon and total small-bowel obstruction after postoperative chemotherapy of esophageal cancer. Ther Clin Risk Manag 2017;13:691–5. 10.2147/TCRM.S135677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callister ME, Lawrence H, Gill K, et al. Ischaemic bowel within the thoracic cavity-An unusual cause of a pleural effusion. Respir Med CME 2008. [Google Scholar]
- 4.Chandrasekharan PK, Rawat M, Madappa R, et al. Congenital diaphragmatic hernia – a review. Matern Health Neonatol Perinatol 2017;3 10.1186/s40748-017-0045-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurt A, Yazıcıoğlu KR, İpek A, et al. Right sided diaphragmatic hernia in an adult with no history of trauma: unusual CT findings. Electron J Gen Med [Internet] 2018;1. [Google Scholar]
- 6.Kanazawa A, Yoshioka Y, Inoi O, et al. Acute respiratory failure caused by an incarcerated right-sided adult Bochdalek hernia: report of a case. Surg Today 2002;32:812–5. 10.1007/s005950200156 [DOI] [PubMed] [Google Scholar]
- 7.Hamid KS, Rai SS, Rodriguez JA. Symptomatic Bochdalek hernia in an adult. JSLS 2010;14:279–81. 10.4293/108680810X12785289144719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suzuki T, Okamoto T, Hanyu K, et al. Repair of Bochdalek hernia in an adult complicated by abdominal compartment syndrome, gastropleural fistula and pleural empyema: report of a case. Int J Surg Case Rep 2014;5:82–5. 10.1016/j.ijscr.2013.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slesser AA, Ribbans H, Blunt D, et al. A spontaneous adult right-sided Bochdalek hernia containing perforated colon. JRSM Short Rep 2011;2:1–5. 10.1258/shorts.2011.011056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas S, Kapur B. Adult Bochdalek hernia--clinical features, management and results of treatment. Jpn J Surg 1991;21:114–9. 10.1007/BF02470876 [DOI] [PubMed] [Google Scholar]
- 11.Mullins ME, Stein J, Saini SS, et al. Prevalence of incidental Bochdalek's hernia in a large adult population. AJR Am J Roentgenol 2001;177:363–6. 10.2214/ajr.177.2.1770363 [DOI] [PubMed] [Google Scholar]
- 12.Rout S, Foo FJ, Hayden JD, et al. Right-Sided Bochdalek hernia obstructing in an adult: case report and review of the literature. Hernia 2007;11:359–62. 10.1007/s10029-007-0188-5 [DOI] [PubMed] [Google Scholar]