Abstract
As the government's coronavirus (COVID-19) lockdown starts to be eased and the NHS starts entering phase two of its response to the COVID-19 pandemic, dental practices are expecting a sharp increase in the need for dental treatment. Dental care professionals will have legitimate concerns regarding the risk of transmission of COVID-19, particularly if required to respond to a medical emergency, such as a cardiac arrest. This article provides an overview on being prepared for, and responding to, such an emergency, with particular reference to recently published Resuscitation Council (UK) guidance. A suggested aide-memoire for managing a COVID-19 resuscitation situation is also included, which the authors hope will help dental practices to devise guidelines to meet their local needs, as well as promoting the team response to such a difficult and challenging event.
Key points
Understand the latest Resuscitation Council (UK) resuscitation guidance for COVID-19 patients.
Know what to include in an aide-memoire for resuscitation in COVID-19 patients.
Know the special COVID-19 considerations for management of individual medical emergencies.
Introduction
The dental team will have legitimate concerns regarding the risk of transmission of coronavirus (COVID-19) when treating patients. These anxieties will undoubtedly increase in a dental practice setting if they have to respond to a medical emergency, such as a cardiac arrest in a COVID-19 patient.
As the NHS starts entering phase two of its response to the COVID-19 pandemic and dental practices respond to the expected sharp increase in the need for dental treatment,1 the dental team needs to ensure they are prepared to respond safely to a medical emergency in a COVID-19 patient. With dental practices starting to reopen from 8 June 2020 for all face-to-face care,2 the undertaking of relevant risk assessments and ensuring readiness for a medical emergency in a COVID-19 patient is now paramount.3
The aim of this article is to provide an overview on the current guidelines relating to the management of medical emergencies in COVID-19 patients in the dental practice.
Background
During the NHS COVID-19 delay phase and the establishment of urgent dental care systems, NHS England and NHS Improvement4 advised relevant staff to prepare for the possibility of having to respond to a medical emergency in a COVID-19 patient. They advised teams to develop and rehearse their COVID-19 triage protocols and isolation procedures. This preparation should have included:4
Agreeing a practice approach for each stage of the potential scenarios
Confirming role and responsibilities for each member of the team
Appointing an incident manager - confirm lead for discussions with patients/NHS 111
Preparing an aide-memoire for staff - rehearse practice response.
The Chief Dental Officer (CDO) England, in her letter dated 1 May 2020,1 stated that, as the NHS enters the second phase of its response to COVID-19, public health measures were being reviewed and she expected the NHS urgent dental care system to expand, increasing non-COVID-19 urgent services. She estimated that several thousand COVID-19 patients will require dental care.1
The CDO subsequently wrote to all dental practices on 28 May 2020 requesting that dental practices commence opening from Monday, 8 June 2020 for all face-to-face care, once they have the necessary infection prevention and control and personal protective equipment (PPE) requirements in place.2
Although unlikely to happen, if a medical emergency did occur in the dental practice, it could have a significant impact on patient safety as well as the safety of the dental team if the appropriate PPE guidelines are not followed; the consequences could be potentially catestophic.3
Resuscitation Council (UK)'s guidelines for resuscitation have always stressed 'your personal safety and that of resuscitation team members is the first priority during any resuscitation attempt'.5 The current pandemic poses serious health risks to the whole dental team, particularly when resuscitating COVID-19 patients. However, the profession is reminded by the GDC Standard 6.2.6: 'Medical emergencies can happen at any time. You must make sure that there is at least one other person available within the working environment to deal with medical emergencies when you are treating patients'.6
Being prepared
The current planning phase involves being prepared to respond to a medical emergency, including a cardiac arrest, in a patient with COVID-19 or suspected to have COVID-19. The Resuscitation Council (UK) provides helpful guidance.5 It is paramount to undertake a risk assessment relating to a medical emergency in a COVID-19 patient. It is important to ensure the appropriate PPE is available and that staff understand their roles if such an event did happen.
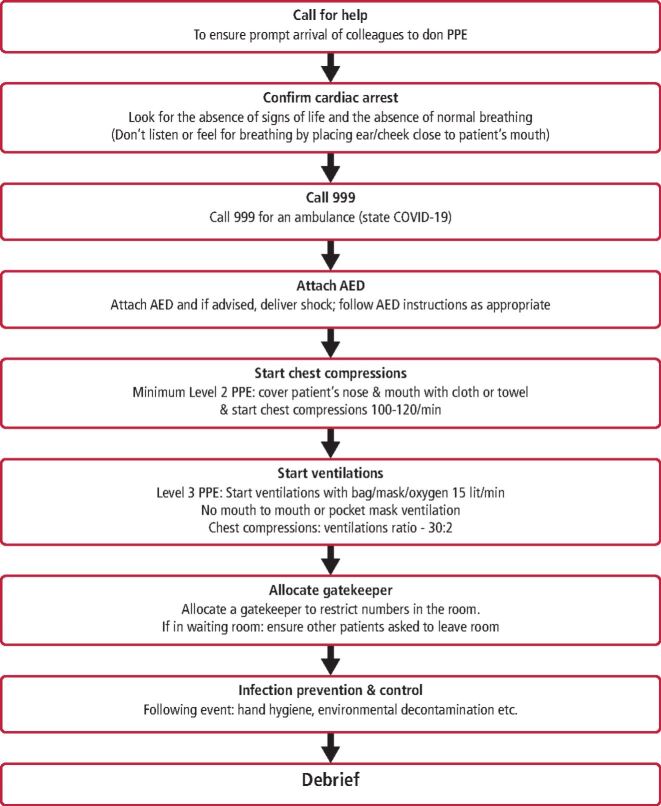
Devising an aide-memoire (Fig. 1) is recommended4 and will help an effective team response, so that 'all members of staff who might be involved in dealing with a medical emergency are trained and prepared to do so at any time, and practise together regularly in a simulated emergency so they know exactly what to do'.6 Running COVID-19 drills using the aide-memoire is recommended and should include the use of PPE.
Fig. 1.
COVID-19 resuscitation in the dental practice: aide-memoire
The Faculty of General Dental Practice (FGDP) UK has produced guidance to help the dental profession to identify risks and mitigate them appropriately, and to develop specific strategies for their individual practice needs.3 The British Dental Association's (BDA's) newly launched face-to-face care toolkit provides its members with helpful resources to help dental practices prepare for opening up again.7 The Scottish Dental Clinical Effectiveness Programme has also issued guidelines.8
Risk assessment
The GDC has stated that 'dental professionals will need to continue exercising their professional judgement and weigh the risks in any given situation',3 an approach endorsed by the FGDP(UK).3
Ideally, initial risk assessment should be undertaken by phone or other remote triage before entering the dental practice (or at two-metre social distance upon entering).9 The patient's COVID-19 status needs to be established and patients managed accordingly to national guidelines.8 Mitigating the risks of staff exposure to COVID-19 is paramount.
Personalised risk assessment for members of the dental team is also important, particularly relating to the increased risks associated with COVID-19 infection in certain groups (age, gender, ethnicity, pregnancy, co-morbidities etc).10 Safety applies to the team members at all times, which will involve the need to work as a team, and members must be trained for unprecedented events such as these so that they can 'support the patient and their colleagues if there is a medical emergency'.11
PPE
It is important to select the appropriate PPE after undertaking a risk assessment of the procedure, the staff and the patient, together with taking into account the current national COVID-19 alert level in order to best protect all concerned.3
Dental practices will need to follow national guidelines regarding what PPE should be available for managing a medical emergency, including a cardiac arrest.5,9,12 Whether an aerosol generating procedure (AGP) will be required to manage the emergency or not will determine what level of PPE will be required.9
Medical emergencies (not including resuscitation)
For most medical emergencies, risk assessment will probably indicate that level 2 PPE (Box 1) is advised.9 Particular care should be taken, however, if a patient on home oxygen is self-administering low-flow oxygen via a nasal cannula when they attend the dental practice. High-flow oxygen via a nasal cannula is an AGP.9
Resuscitation
There is currently conflicting advice concerning PPE for COVID-19 resuscitation.5,13 The Resuscitation Council (UK),5 in line with other national and international authoritative bodies, advises that chest compressions are an AGP, therefore requiring level 3 PPE (Box 2).
Public Health England (PHE)9 states that 'chest compressions and defibrillation (as part of resuscitation) are not considered AGPs; first responders (any setting) can commence chest compressions and defibrillation without the need for AGP PPE while awaiting the arrival of other clinicians to undertake airway manoeuvres'; that is, level 2 PPE is required for chest compressions only.9
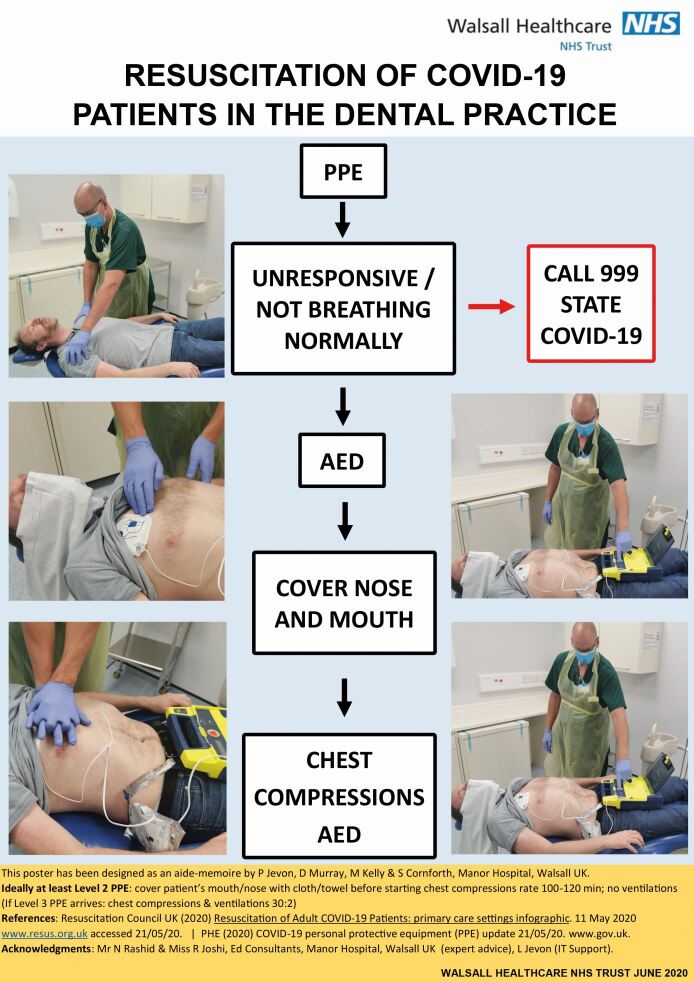
It is perplexing why PHE and the Resuscitation Council (UK) have not agreed on this important issue, but speculating the possible reasons for this is not helpful here and is beyond the scope of this article. However, the conflicting advice has been 'resolved' by the Resuscitation Council (UK) issuing common sense advice, recommending covering the patient's nose and mouth with a cloth or towel (as a bare minimum) and ideally donning at least level 2 PPE (Box 1) before starting chest compression-only CPR (Fig. 2).12 This sensible, practical and safe advice has been endorsed by the FGDP(UK).3
Fig. 2.
Resuscitation of COVID-19 patients in the dental practice
Manual ventilation is an AGP, requiring all dental team members present to don level 3 PPE (Box 2) before ventilations are started (ratio of 30 compressions to two ventilations).
It is important that all members of the dental team are trained in the use of PPE, including:8
When to use it
What PPE is required
Safe donning, using and doffing of PPE to prevent self-contamination and contamination of others.
The BDA provides its members with a video on how to use PPE safely, in order to help dental practices to prepare for opening up again.7 The use of PPE should be incorporated into COVID-19 medical emergencies training for the dental team.
Box 1 Recommended PPE for non-AGPs3,9,12.
Gloves
Apron
Fluid-resistant surgical mask
Eye/face protection.
Box 2 Recommended PPE for full AGPs3,9,12.
Single use disposable gloves
Single use disposable fluid-resistant overall/gown
Single use filtering face piece respirator
Eye/face protection
(Reusable PPE now also available).
Prevention of cardiac arrest
Prevention of cardiac arrest and avoiding the need to perform CPR is the ideal scenario. It is important to follow the 'Airway, Breathing, Circulation, Disability, Exposure' (ABCDE) approach to assess and treat the acutely ill patient.14
In hospitalised COVID-19 patients, the respiratory function can quickly deteriorate, leading to a rapid increase in oxygen requirements.15 It is possible that this may also happen in the dental practice, so it is imperative to call 999 in a timely manner and, while waiting for the paramedics, ensure the patient is in an optimum position to help their breathing (usually sitting upright with feet on the floor) and administer oxygen (15 litres/min). This may prevent deterioration to cardiac arrest.
Resuscitation Council (UK) COVID-19 guidelines
The Resuscitation Council (UK) has provided a number of helpful statements relating to CPR and resuscitation in COVID-19 patients in different settings; for example, acute/non-acute hospital settings, first aid and community settings.5 Although there is no specific guidance for dental practices, the overall common themes of the statements can be easily applied to dental practice settings. The revised procedure for COVID-19 resuscitation in the dental practice (Fig. 1) will now be described.
Call for help
If a patient collapses, immediately summon help from colleagues. This will usually involve shouting for help. This will ensure the prompt arrival of colleagues who can start to don appropriate PPE if necessary.
Confirm cardiac arrest
Cardiac arrest should be confirmed by looking for the absence of signs of life and the absence of normal breathing. Refrain from listening or feeling for breathing by placing your ear and cheek close to the patient's mouth.
Call 999
Call 999 for an ambulance (inform the ambulance service that COVID-19 is suspected).
Attach automated external defibrillator
As defibrillation is not an AGP, if wearing level 2 PPE, attach the automated external defibrillator (AED) and, if advised, deliver shock. Early use of the AED significantly increases the patient's chances of survival and does not increase the risk of infection. Continue to follow AED voice prompts as appropriate.
Start chest compressions
If level 2 PPE (Box 1) is available, cover the patient's nose and mouth with a cloth or towel (as this may limit aerosol spread) and start chest compressions at a rate of 100-120 per minute
If level 3 PPE (Box 2) is available, start chest compressions and ventilations at a ratio of 30:2.
Start ventilations
Ventilations are considered an AGP,5,9 so all team members present must be wearing level 3 PPE before ventilations are started. Start ventilations with a bag/mask device, ideally a two-person technique, with supplementary oxygen (15 litres/min) attached. Mouth-to-mouth ventilation or ventilation via a pocket mask should not be undertaken. The ratio of chest compressions to ventilations is still 30:2.
Allocate gatekeeper
Dental surgeries are generally quite small and it is important to limit numbers entering the room. It may be necessary to allocate a gatekeeper to restrict numbers. In an emergency in the waiting room, it is important to ensure all other patients are asked to leave the room.
Aide-memoire
As advised by NHS England and NHS Improvement,2 a suggested aide-memoire 'COVID-19 Resuscitation in the Dental Practice' is detailed in Figure 1. The poster 'Resuscitation of COVID-19 Patients in the Dental Practice' (Fig. 2) is designed to be a visual reminder of the key points (when level 3 PPE is unavailable i.e. no ventilations). The poster is available in PDF format from Walsall Healthcare NHS Trust (please email phil.jevon@walsallhealthcare.nhs.uk).
Lone rescuer
If the dental care professional (DCP) is alone, then it would be reasonable to follow the above procedure except for providing ventilations (AED and chest compressions only). It would be helpful to cover the patient's nose and mouth with a towel or similar.
Post-resuscitation infection prevention and control
It is important to dispose of, or clean, all resuscitation equipment following the manufacturer's recommendations and local guidelines.
PPE should be removed safely to avoid self-contamination and clinical waste bags disposed of as per local guidelines. PHE's COVID-19 infection prevention and control guidance should be followed.9
After the procedure, wash hands thoroughly with soap and water (alternatively use alcohol hand gel) and seek advice from NHS 111 COVID-19 advice service or medical adviser.
Post-resuscitation debrief
A post-resuscitation debrief should be planned and undertaken following a COVID-19 resuscitation attempt. In particular, it is really important to look after staff's mental health and wellbeing, and it may be necessary to seek local specialist help and advice. It is also important to learn from the resuscitation attempt in order to try and improve for next time. A significant event analysis can be done, but is probably best undertaken at a later date to encourage reflection from the event and enable the team to be better prepared should a similar situation arise in the future.
Communication in a COVID-19 emergency
Communication in any medical emergency can be difficult, but particularly so during a COVID-19 resuscitation attempt where team members could be wearing PPE that they are not used to. Talking through FFP3 masks can be challenging and the fact that facial expressions can be obscured can make communication even trickier. The senior general dental practitioner present should make an extra effort to ensure adequate communication and effective team communication.
Particular care with communication should be taken when calling 999 for an ambulance for any medical emergency. The use of the 'Situation-Background-Assessment-Recommendation' (SBAR) communication tool is strongly advised, as well as asking the 999 call operator to repeat back what they have been told to confirm understanding and minimise the risk of misunderstanding happening.
Management of medical emergencies in a patient with COVID-19
As mentioned above, the effective management of medical emergencies to prevent deterioration to cardiac arrest and avoiding the need to perform CPR in COVID-19 patients is clearly the ideal scenario. It is important to continue to undertake medical risk assessments and, if possible, take appropriate action to prevent medical emergencies.
In COVID-19 patients, the national guidelines for the management of medical emergencies still apply, but it is important to follow recommended PPE requirements which, in medical emergencies (not involving CPR), will probably be guidelines for non-AGPs (PHE).
There are also a few extra considerations to bear in mind, which are detailed below.
Adrenal crisis
Patients with Addison's disease or adrenal insufficiency are considered to be within the group of vulnerable persons who are at an increased risk from COVID-19 infection,16 which may be complicated by adrenal crisis.17
Anaphylaxis
Usually, the optimum position for a patient in anaphylaxis is supine. However, a COVID-19 patient may have an existing chest infection and could develop breathlessness when lying down. It may be necessary to compromise on the recommend usual position in anaphylaxis and sit the patient up slightly.
Asthma
A chest infection is a known trigger for an asthma attack. An asthmatic patient with COVID-19 infection is therefore more likely to have an asthma attack. It has been reported that, although the inhaler may be effective at relieving the respiratory symptoms (breathlessness, coughing and chest tightness) associated with asthma, it may be ineffective at relieving the similar symptoms that can be associated with COVID-19 infection due to differing pathophysiology.18
It is particularly important for asthma patients to bring their own inhaler and space device with them to their dental appointment. If the dental practice's own inhaler and space device are used, they will need to be replaced, which could prove difficult in the current climate.
Cardiac emergencies
Concerns have been raised regarding the 50% drop in the number of patients attending A&E with a suspected heart attack.19 The associated risks of non-attendance and not getting medical help include long-term myocardial muscle damage and sudden cardiac death. Call 999 for an ambulance if a heart attack is suspected.
Epilepsy
Some patients with epilepsy who develop a fever are more likely to have an epileptic seizure; as fever can occur with COVID-19, this could trigger seizures for some people with epilepsy.20
Hypoglycaemia
Diabetic patients (particularly type 1) who have COVID-19 are more likely to have an unstable blood sugar level and will need close monitoring in the dental practice.21 Both hypoglycaemia and hyperglycaemia can occur.
Sepsis
COVID-19 can cause sepsis; patients who have previously had sepsis may be at increased risk of developing severe illness (including sepsis) if they have COVID-19.22 Remember to refer to the UK Sepsis Trust's sepsis decision support tools specifically for use in dental practices for guidance.23
Stroke
Patients who have previously had a stroke are more likely to develop chest complications, such as pneumonia.24
Vasovagal syncope
Unwell patients are more likely to suffer vasovagal syncope.
Redeployment and managing a medical emergency
Large numbers of DCPs, particularly those working in secondary care settings, have been redeployed in the NHS to support the wider COVID-19 response.4 This initiative is supported by the GDC,25 but DCPs need to be aware that, when providing support to the wider NHS, the GDC's expected standards of care still apply as in any other situation - the test is whether they are trained, competent and indemnified for the tasks they undertake.6 DCPs also need to know their role in a medical emergency (for example, how to call for help, where the defibrillator is, PPE responsibilities etc) within their temporary clinical work areas. DCPs must ensure they continue to work as a team and have undergone simulation as recommended by the GDC.6
Further information
This COVID-19 pandemic is a fast-moving situation and, as such, guidelines are being updated and revised on a regular basis. For the latest information regarding resuscitation and the COVID-19 patient, visit the Resuscitation Council (UK)'s website (www.resus.org.uk).
Conclusion
The COVID-19 outbreak presents dental staff with unprecedented challenges and difficulties. They must ensure that they remain up-to-date with national guidelines and that they are prepared to respond effectively should a COVID-19 patient suffer a medical emergency in the dental practice. A summary of the key points is listed in Box 3.
Box 3 A summary of the key points.
Individualised risk assessments - patents
Individualised risk assessments - staff
Risk assessment - equipment, PPE
Staff training - particular PPE and response to medical emergency in COVID-19 patients
Mitigate risks of exposure to COVID-19 patients
Aide-memoire of modified resuscitation procedure
Debrief, staff support and medical advice.
Acknowledgements
Throughout this article, COVID-19 refers to both confirmed and suspected cases of COVID-19.
References
- 1.Chief Dental Officer England. Letter to dental teams (1 May 2020). 2020. Available at http://www.bsdht.org.uk/Covid/20200501-%20CDO%20England%20-%20COVID-19.pdf (accessed June 2020).
- 2.Chief Dental Officer England. Letter to dental practices: Resumption of Dental services in England (28 May 2020). 2020. Available at https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/Urgent-dental-care-letter-28-May.pdf (accessed June 2020).
- 3.College of General Dentistry and Faculty of General Dental Practice (UK). Implications of COVID-19 for the safe management of general dental practice - a practical guide. 2020. Available online at https://www.fgdp.org.uk/implications-covid-19-safe-management-general-dental-practice-practical-guide(accessed May 2020).
- 4.NHS England and NHS Improvement. COVID-19 guidance and standard operating procedure. 2020. Available at https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/06/C0581-covid-19-urgent-dental-care-sop-update-16-june-20-.pdf (accessed May 2020).
- 5.Resuscitation Council (UK). COVID-19 Resources: Healthcare settings. 2020. Available online at https://www.resus.org.uk/covid-19-resources (accessed June 2020).
- 6.General Dental Council. Standards. 2013. Available online at https://standards.gdc-uk.org/ (accessed May 2020).
- 7.British Dental Association. Face-to-face care toolkit. 2020. Available online at https://bda.org/advice/Coronavirus/Pages/returningtowork.aspx (accessed June 2020).
- 8.Scottish Dental Clinical Effectiveness Programme. Resuming General Dental Services Following COVID-19 Shutdown. 2020. Available online at https://www.sdcep.org.uk/published-guidance/covid-19-practice-recovery/ (accessed June 2020).
- 9.Public Heath England. COVID-19: infection prevention and control guidance. 2020. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/886668/COVID-19_Infection_prevention_and_control_guidance_complete.pdf (accessed June 2020).
- 10.Public Health England. Disparities in the risk and outcomes of COVID-19. 2020. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/891116/disparities_review.pdf (accessed June 2020).
- 11.General Dental Council. Scope of Practice. 2013. Available online at https://www.gdc-uk.org/informationstandardsguidance/standardsandguidance/scopeofpractice (accessed May 2020).
- 12.Resuscitation Council (UK). COVID-19 Resources: Primary care settings. 2020. Available online at at https://www.resus.org.uk/media/statements/resuscitation-council-uk-statements-on-covid-19-coronavirus-cpr-and-resuscitation/ (accessed June 2020).
- 13.Public Health England. PHE statement regarding NERVTAG review and consensus on cardiopulmonary resuscitation as an aerosol generating procedure (AGP). 2020. Available online at https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/phe-statement-regarding-nervtag-review-and-consensus-on-cardiopulmonary-resuscitation-as-an-aerosol-generating-procedure-agp (accessed May 2020).
- 14.Resuscitation Council (UK). Resuscitation guidelines. 2015. Available online at https://www.resus.org.uk/resuscitation-guidelines/ (accessed May 2020).
- 15.Royal College of Physicians. NEWS2 and deterioration in COVID-19. 2020. Available online at https://www.rcplondon.ac.uk/news/news2anddeteriorationcovid19 (accessed June 2020).
- 16.Addison's Self-Help Group. Novel coronavirus (COVID-19). 2020. Available at https://www.addisonsdisease.org.uk/news/novelcoronaviruscovid-19 (accessed May 2020).
- 17.Arlt W, Baldeweg S E, Pearce S H S, Simpson H L. Endocrinology in the time of COVID-19: management of adrenal insufficiency. Eur J Endocrinol 2020; DOI: 10.1530/EJE-20-0361. [DOI] [PMC free article] [PubMed]
- 18.Asthma UK. Coronavirus (COVID-19): Health advice for people with asthma. 2020. Available online at https://www.asthma.org.uk/advice/triggers/coronaviruscovid19/ (accessed May 2020).
- 19.British Heart Foundation. Lives at risk due to 50% drop in heart attack A&E attendances. 2020. Available at https://www.bhf.org.uk/whatwedo/newsfromthe-bhf/news-archive/2020/april/dropinheartattackpatientsamidstcoronavirus-outbreak (accessed May 2020).
- 20.Diabetes UK. Updates: Coronavirus and diabetes. 2020. Available at https://www.diabetes.org.uk/about_us/news/coronavirus (accessed May 2020).
- 21.Epilepsy Action. Coronavirus (COVID-19) and epilepsy. 2020. Available at https://www.epilepsy.org.uk/info/daily-life/safety/coronavirus-covid-19 (accessed May 2020).
- 22.UK Sepsis Trust. COVID-19 Recovery Response. 2020. Available online at https://sepsistrust.org/covid19recovery-response/ (accessed May 2020).
- 23.UK Sepsis Trust. Clinical Tools.2020. Available online at https://sepsistrust.org/professional-resources/clinical-tools/ (accessed May 2020).
- 24.Stroke Association. Stroke survivors and coronavirus (COVID-19). 2020. Available online at https://www.stroke.org.uk/finding-support/information-coronavirus-stroke-survivors (accessed May 2020).
- 25.General Dental Council. Responding to COVID-19: providing treatment in uncertain times. 2020. Available at https://www.gdc-uk.org/news-blogs/blog/detail/blogs/2020/03/26/respondingtocovid19providingtreatmentin uncertaintimes (accessed May 2020).