Abstract
India has the highest burden of incident tuberculosis (TB) cases and deaths globally. TB is strongly associated with poverty and this risk is largely mediated by undernutrition in India. COVID-19 response related lockdown has resulted in an economic crisis which may double levels of poverty, has exacerbated food insecurity, and disrupted TB services. These developments may have serious implications for TB progression and transmission in India. The nutritional status of a population is a strong determinant of the TB incidence, and undernutrition in adults alone accounts for 32–44% of TB incidence in India. A systematic review has shown that a 14% increase in TB incidence can occur per one unit decrease in body mass index (BMI), across the BMI range of 18.5–30 kg/m2. We believe that one unit decrease in BMI (corresponding to a 2–3 kg weight loss) may result in the poor in India as a result of the lockdown and its aftermath. This may result in an increase in estimated (uncertainty interval) incident TB by 185 610 (180 230, 190 990) cases. A 59% reduction in TB case detection between end March and May 2020, may result in an estimated (uncertainty interval) additional 87 711 (59 998, 120 630) TB deaths [19.5% increase (14.5, 24.7)] in 2020. Disadvantaged social groups and those living in states with higher levels of poverty, under-nutrition,and migrant workers are at particular risk. We suggest enhanced rations including pulses through the public distribution system and direct cash transfers to the poor pending restoration of livelihoods. TB services should be resumed immediately with enhanced efforts at case detection including active case finding. To prevent deaths among TB detected within the national TB programme, systemic identification, referral and management of severe disease at notification should be considered.
Keywords: Coronavirus, Tuberculosis epidemiology, Mortality, Lockdown, Perturbation, Impoverishment
1. Introduction
Ending tuberculosis (TB) globally is critically dependent on ending TB in India. More than a quarter of the world's 10 million estimated cases and 449,700 of the world's estimated 1.3 million TB related deaths occur in India.1 India has committed itself to the ambitious goal of meeting the SDG targets of reducing TB incidence by 80% and TB deaths by 90% by 2025, five years before the global deadline in 2030.2
The national response to the COVID-19 pandemic in India included a nationwide lockdown for 68 days (25 March to 31 May 2020) with phase-wise unlocking starting 01 June 2020. The two key transient changes that may affect TB epidemiology include lockdown induced worsening of poverty and undernutrition in the poor as well pushing those who live a fragile economic life into poverty, and lockdown induced under-detection of active TB. We discuss and attempt to quantify how these two changes can have a potential impact on TB incidence and mortality in India. India has one of the largest numbers of people with latent TB infection, an estimated 354 million (a population larger than that of the United States), who are at risk of developing TB.3 They can progress to active disease by any condition which impairs cell-mediated immunity, of which undernutrition is the most common at the population level in India and globally.4, 5, 6
2. Lockdown induced poverty and undernutrition and its impact on TB incidence
2.1. Poverty, nutrition and TB
Globally, India has the highest numbers of poor people according to the World Bank.7 Using a monthly per capita expenditure cut-off, the Government of India estimated in 2011–12 that 22% live below the poverty line.8
In India poverty is closely associated with childhood and adult undernutrition. According to the results of the National Family Health Survey-4 (NFHS-4), 23% of adult women and 19% of adult men have undernutrition defined as a body mass index (BMI) less than 18.5 kg/m2.9 The prevalence of under-nutrition is higher in rural India (especially in the states of Jharkhand, Bihar, Madhya Pradesh, Odisha and Uttar Pradesh), in women, in those belonging to scheduled tribes and scheduled castes, and in the poor. While 11.8% of women in the highest wealth index were underweight, in the lowest wealth index, 35.8% had a low BMI, with a similar differential in the men.9 According to the World Health Organization (WHO), when the population prevalence of low BMI is between 20 and 39 percent it indicates a serious situation.10
The undernutrition in the poor is linked to suboptimal dietary intakes and dietary diversity which results in chronic energy deficiency, and deficiency of nutrients (macronutrients and micronutrients).11 The National Nutritional Monitoring Board surveys in rural households of nine states have shown that apart from roots and tubers where the recommended dietary intakes are met, the intake of protective foods like pulses, green leafy vegetables, fruits is below recommended intakes. A particular concern is protein intake which is predominantly derived from cereals, and cereal proteins are of poorer quality unless supplemented by pulses or animal proteins12 In 2011–12, the consumption of energy and protein in poor people (lowest 30 percent of income class) were lower than the all-India average and the daily minimum consumption requirement.13 Recent data suggests that but for one state, none of the other states consumed the minimum recommended 40 g of pulses per capita per day.14
The Indian Government implemented the National Food Security Act in 2014, and aimed to improve the coverage of the public distribution system (PDS) to 75% of the rural population and around half of the urban population. The PDS supplies five kg cereal per head (rice or wheat) at a highly subsided rate of INR three per kg (wheat) or INR two per kg (rice) (100 INR = US$ 1.32). Pulses which are an important source of protein are not part of this subsidised ration except in two states. The adverse nutritional implications of this cereal-centric approach have been highlighted by nutrition experts.15 Despite its potential, PDS has had a limited role in improving food security due to problems with targeting and operational inefficiencies.16
In India TB is still strongly associated with poverty and according to NFHS-4 the prevalence of self-reported TB was nearly four-fold higher in the lowest compared to the highest wealth quintile.17 According to a recent study, around half the TB patients belonged to below poverty line.18 Poverty can impact on TB risk by other means like overcrowding, but the strongest mediating effect of poverty on TB prevalence in India was by low BMI.19 In a systematic review of six large cohort studies, it was seen that BMI and TB incidence had a consistent and inverse exponential relationship and that low BMI was causally related to TB incidence.20 In the most recent cohort study which examined the effect of BMI and TB incidence, low BMI (<18.5 kg/m2) was associated with an adjusted hazard ratio of 12.4 [95% CI: 5.75,26.95] for development of TB.21 Undernutrition is strongly associated with development of active TB because undernutrition impairs the protective innate and adaptive immunity and allows TB infection to progress to active TB.5
In India, the large burden of active TB is driven by the high prevalence of latent TB infection (an estimated 354 million persons across all ages) and the high levels of undernutrition in adults.3 , 5 As per the Global TB report 2019, undernutrition accounted for the maximum proportion of TB incidence in India, approximating the combined effect of HIV, diabetes, smoking and harmful use of alcohol.1 Using adult undernutrition data from a 2005–06 nationally representative NFHS-3 and a risk ratio for low BMI for development of TB from a cohort study, Bhargava A et al predicted that 55% of adult TB is attributed to undernutrition.22 This figure reduces to approximately 44% (unpublished updated analysis) if we use the prevalence of undernutrition data from the 2015-16 survey, and the similar risk ratio related to undernutrition.9 Lonnroth K et al in 2010 predicted that around 32% of TB is attributable to undernutrition. This was lower than the prediction of Bhargava A et al because Lonnroth K et al used the Food and Agriculture Organization definition of undernutrition which is a modelled estimate, and a lower risk ratio.23
A number of studies have reported on the association of dietary protein intake with incident and prevalent TB. In a cohort study, protein intake less than 50% was strongly associated with TB incidence.21 Low levels of serum albumin and serum transferrin (both markers of protein nutritional status) were strongly associated with an increased risk of TB.21 In a case–control study in Zambia, the effect of household socioeconomic position on TB prevalence was largely mediated by protein intake (adjusted odds ratio 3.1). In this high HIV prevalence setting, the population attributable fraction for TB was higher for protein deficiency (42%) when compared to HIV (36%).24 In India (2011–12), as the poorest 30% of the population also consume less protein,16 , 25 therefore, low protein consumption may be a risk factor for development of TB.
2.2. Impact of lockdown
The COVID-19 pandemic has resulted in both a health shock and an economic shock. The lockdown in response to the pandemic and the events related to it can have an adverse epidemiologic impact on TB incidence through its effect on poverty, and dietary intakes.
This crisis has hit India when the GDP growth was already slowing for a few years and demand had slowed down with rising unemployment.26 According to the Centre for Monitoring Indian Economy, the estimated unemployment rate has touched 27% for the week ending on three May 2020 when compared to 6.7% for the week ending on 15 March 2020.27 According to the International Labour Organisation in India where 90% of the labour force is in the informal sector, almost 400 million informal sector workers may be pushed into poverty due to the lockdown.28 Estimates by economists in India indicate that a 25% reduction in annual income which is expected because of the COVID-19 lockdown, can push 354 million into poverty and result in doubling of poverty levels in India, negating the gains made since 2005.29 Lockdown may have a short term effect on reduced per capita calorie and protein consumption especially protein consumption in poorer sections of the society, as well as a long term outcome related to delayed recovery of the economy and unemployment. Around 13.9 million temporary or seasonal migrant workers have been worst affected by this crisis. A survey among migrant workers showed that around 21 days into lockdown, 96% workers had not received rations from the government, 70% had not received any cooked food and 50% had rations left only for one day.30
During the lockdown, the Government of India has suggested additional free rations of five kg cereal per head and one kg of pulse per family per month.31 This move is a welcome one, however the allocation of five kg rice in the PDS amounts to only 167 g or 500 calories per day, and this additional ration may add up to 1000 calories per day. The pulse ration amounts to eight g of pulses per day in a four member household, and these allocations are unlikely to supply adequate calories, proteins and micronutrients in the poor households. The recommended dietary intakes for Indians engaging in light work are 2320 calories in men and 1900 calories in women,32 and the nutritional stress related to the events of the lockdown are likely to witness substantial weight loss.
The potential impact of weight loss in the poor households on TB incidence can be estimated using the results of a systematic review of cohort studies linking BMI to TB incidence.20 The average slope gave a reduction of TB incidence of 13.8% [95% CI: 13.4, 14.2] for an increase of BMI by one kg/m2 for BMIs in the range of 18.5–30 as well as the converse increase in TB incidence by 13.8% for one unit decrease of BMI.20 Therefore, a reduction in BMI at population level due to reduction in consumption among the poorest sections of the society is also conversely expected to be associated with a 13.8% increase in TB incidence in the poorest sections.
The mean heights of adult Indian men and women are 164 cm and 152 cm and the mean weights are 56.07 kg and 48.75 kg respectively.9 For these heights a unit decrease in BMI would amount to a loss of 2.7 kg and 2.3 kg respectively. The average per capita energy intake in India in the bottom 30% of the population in terms of monthly per capita expenditure was estimated to be less than 2000 calories in the National Sample Survey's 68th round in 2011–12.33 In the 68 days of lockdown even a calorie deficit of 250 calories per day compared to caloric expenditure could potentially lead to two kg weight loss in the two months, since one kg weight loss corresponds to a caloric deficit of 7500 calories.
The degree of weight loss would of course be modified by a number of other factors. If a person is consuming less energy as a result of food shortage, the decreased activity as a result of being inactive at home, may limit their caloric expenditure and weight loss. However, if a person engaged in unskilled labour continues to limit his activity, he will not be productive in an economic sense. Some of the migrant workers underwent even greater calorie deprivation and in fact had to increase their activity too in the attempts to reach home, and may have experienced greater weight loss. Also the coming months will require farm-related activity at a time of coexisting food insecurity34 and the daily deficit of calories may exceed 250 calories a day. Also a quarter of the women and one-fifth of men according to NFHS-4 already have a low BMI, suggestive of chronic energy deficiency. In those below the BMI of 18.5 kg/m2, the risk of TB is even higher.21 Overall, our assumption of a weight loss corresponding to a one unit decrease in BMI, in poor households appears reasonable. We could expect a 13.8% [95% CI: 13.4, 14.2] increase in TB incidence in India in these households in the coming months ahead.
Assuming that half of the TB is related to undernutrition and poverty and caloric deficits which may vary between 250 and 500 calories a day over the two months of lockdown, we can assume an increase (uncertainty interval) in incident TB by 185 610 (180 230, 190 990) cases in a worst case scenario [(0.138∗estimated annual TB incidence)/two]. We have taken the estimated annual incident TB in India (2.69 million in 2018) from the recent WHO Global TB report.1 If we consider the effects of reduced protein consumption in addition to the lower caloric intake due to lockdown, the estimated increase in incident TB could be higher.
A well-documented impact of undernutrition on TB incidence, is the experience of Cuba during the food and economic crisis of the early 1990s.35 Following the collapse of the Soviet Union, Cuba had an economic and food crisis in the early 1990s, exacerbated by the US embargo on Cuba. Per capita calorie and protein availability decreased, only about 1200 calories a day were available through the rationed distribution,35 and per capita availability of energy declined to the lowest figure of 1940 Kcal/day, a 32% reduction in four years. Cuba had witnessed an annual decrease in notification of 5% for three decades till 1991, but from 1991 to 1994 the annual notification rate increased by 49.7% (average annual increase of smear positive cases was 23.6%)36 and TB notification rates increased from 5.5 cases/100,000 three-fold to 15.3 cases/100,000 in 1994.35 TB mortality also increased significantly in Cuba but that was also related to under-detection of cases and diagnostic delays, and medication shortages.35
Another experience of increase in incidence of TB following economic and nutritional crisis is Zimbabwe in the years 2008–09. In two rural hospitals, the TB notification increased by up to 35% without any accompanying rise in HIV prevalence in the population and the notification rates declined shortly after the economic recovery.37
3. Under-detection due to lockdown and its impact on TB epidemiology
3.1. Reduction in TB detection
During lockdown, the priorities shifted towards COVID-19 with an adverse impact on TB related diagnosis, treatment and prevention services. A reduction in TB detection could occur because of reduction in diagnosis or lack of time for the nodal health programme staff to update in the electronic information management system (possibly preoccupied in COVID-19 related response). A reduction in diagnosis could be due to restricted movement, increased time spent indoors and fear of travelling to health facilities during lockdown. Reduction in TB detection contributes to increased transmission which may reflect as increased incidence at a later time period. This may also contribute to increased deaths due to lack of treatment or delayed treatment initiation resulting in greater severity of disease. WHO has circulated an information note on TB and COVID-19 emphasising the need to avoid disruption of TB services during the COVID-19 pandemic.38
In India, there was a 59% decrease in TB case detection over a period of eight weeks of lockdown (25 Mar to 19 May 2020) as compared to the level of detection eight weeks before the lockdown (29 Jan to 24 Mar 2020). The decrease in TB case detection was 62% when compared to the level one year before (25 Mar to 19 May 2019). This was calculated based on notification data extracted on 11 June 2020 from the NIKSHAY website (a case-based electronic TB notification system of India's National TB elimination Programme).39
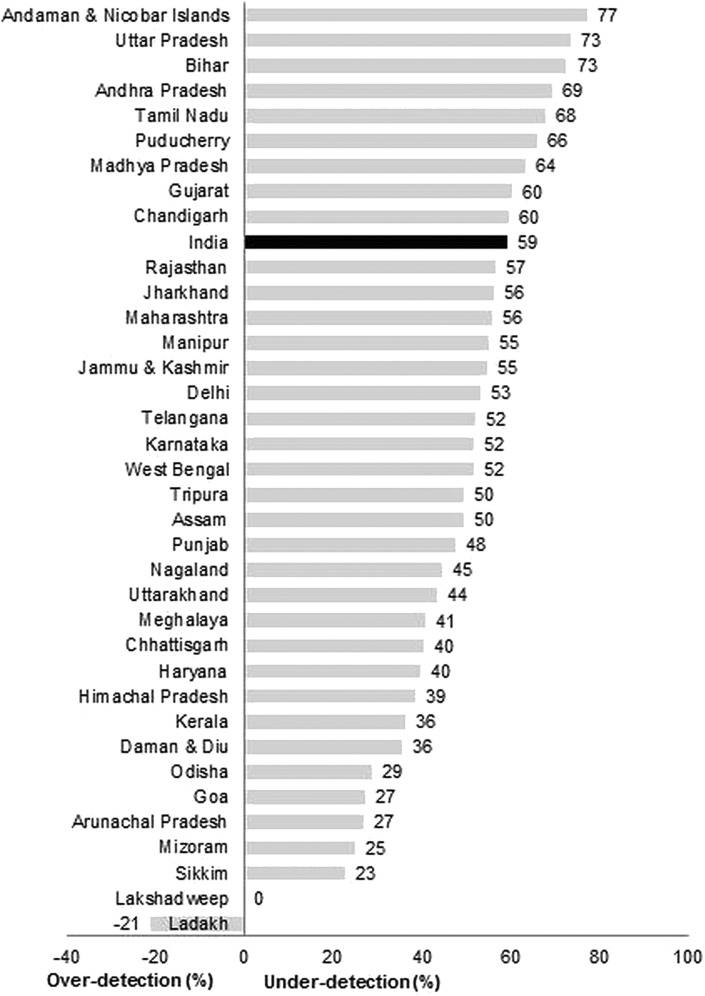
The under-detection was more than 70% in Andaman & Nicobar, Uttar Pradesh and Bihar; and less than 30% in Odisha, Goa, Arunachal Pradesh, Mizoram and Sikkim. There was no effect of lockdown on TB under-detection in Lakshadweep (0%) and Ladakh (21% over-detection) (see Table 1 and Fig. 1 ). Bihar and Uttar Pradesh constitute around one-fourth of India's population and have both high undernutrition status and under-detection.9
Table 1.
Under-detection of Tuberculosis in India during COVID-19 pandemic response related lockdown - eight week lockdown period 25 March to 19 May 2020 compared with eight week pre-lockdown period 29 January to 24 March 2020∗.39
| State (in alphabetical order) | Notifications (n) |
Case detection (%) (c = b/a) | Under-detection (%) (d = 100 – c) | |
|---|---|---|---|---|
| Pre-lockdown (a) | During lockdown (b) | |||
| Andaman & Nicobar Islands | 101 | 23 | 23 | 77 |
| Andhra Pradesh | 15,194 | 4658 | 31 | 69 |
| Arunachal Pradesh | 478 | 349 | 73 | 27 |
| Assam | 7533 | 3799 | 50 | 50 |
| Bihar | 19,654 | 5374 | 27 | 73 |
| Chandigarh | 1008 | 405 | 40 | 60 |
| Chhattisgarh | 6655 | 3966 | 60 | 40 |
| Daman & Diu | 213 | 137 | 64 | 36 |
| Delhi | 17,973 | 8390 | 47 | 53 |
| Goa | 322 | 234 | 73 | 27 |
| Gujarat | 26,897 | 10,646 | 40 | 60 |
| Haryana | 12,424 | 7492 | 60 | 40 |
| Himachal Pradesh | 2757 | 1695 | 61 | 39 |
| Jammu & Kashmir | 2009 | 905 | 45 | 55 |
| Jharkhand | 8616 | 3767 | 44 | 56 |
| Karnataka | 14,468 | 6960 | 48 | 52 |
| Kerala | 4045 | 2575 | 64 | 36 |
| Ladakh | 33 | 40 | 121 | −21 |
| Lakshadweep | 2 | 2 | 100 | 0 |
| Madhya Pradesh | 29,101 | 10,616 | 36 | 64 |
| Maharashtra | 32,717 | 14,447 | 44 | 56 |
| Manipur | 305 | 137 | 45 | 55 |
| Meghalaya | 800 | 474 | 59 | 41 |
| Mizoram | 425 | 318 | 75 | 25 |
| Nagaland | 649 | 360 | 55 | 45 |
| Odisha | 8701 | 6197 | 71 | 29 |
| Puducherry | 745 | 254 | 34 | 66 |
| Punjab | 9852 | 5144 | 52 | 48 |
| Rajasthan | 26,418 | 11,462 | 43 | 57 |
| Sikkim | 284 | 219 | 77 | 23 |
| Tamil Nadu | 17,025 | 5466 | 32 | 68 |
| Telangana | 12,985 | 6221 | 48 | 52 |
| Tripura | 451 | 227 | 50 | 50 |
| Uttar Pradesh | 77,887 | 20,692 | 27 | 73 |
| Uttarakhand | 4200 | 2373 | 57 | 44 |
| West Bengal | 17,098 | 8261 | 48 | 52 |
| Total | 380,025 | 154,285 | 41 | 59∗∗ |
∗notification data extracted on 11 June 2020 from the NIKSHAY website 39; ∗∗when compared with previous year (25 March to 19 May 2019), the national under-detection was 62%.
Fig. 1.
Bar diagram depicting under-detection (%) of Tuberculosis in India during COVID-19 pandemic response related lockdown - eight week lockdown period (25 March to 19 May 2020) compared with eight week pre-lockdown period (29 January to 24 March 2020)∗.39
∗notification data extracted on 11 June 2020 from the NIKSHAY website39; ∗∗when compared with previous year (25 March to 19 May 2019), the national under-detection was 62%.
3.2. Impact of under-detection
Globally, it has been predicted that an average 25% decrease in TB case detection over a period of three months of lockdown will lead to an additional 190 000 (13% increase) deaths in 2020. This is assuming an absence of a rebound in case detection above values prior to the lockdown.40 We applied the same model to India using 2018 estimates.1 Considering the observed 59% reduction in detection over an eight week period, there will be an estimated (uncertainty interval) additional 87 711 (59 998, 120 630) TB deaths [19.5% increase (14.5, 24.7)], bringing the total to 537 411 (473 698, 607 630) TB deaths in 2020. These estimated total number of deaths will surpass the estimated deaths in 2015 (n = 517 000).
Assuming a two month lockdown and two month recovery period, a recently released report by the WHO Stop TB Partnership has predicted four percent excess deaths globally and 5.7% excess deaths in India during 2020–25. During the same period, the predicted excess incident cases is 3.1% globally and 3.6% in India. Both the models do not account for potential increase in TB incidence and death due to increasing impoverishment arising from economic disruption due to lockdown.41 In addition to the direct effect of impoverishment on TB severity and death,42 , 43 it could also have an indirect effect through delayed health care seeking.
Another modelling study using data from South Africa, India and China predicts that the benefits of COVID-19 response related social distancing on reducing TB deaths are likely to be outweighed by health service disruption. In India assuming TB health services are badly affected (which is the case), an additional 149 448 (range 85 000, 233 602) TB deaths have been predicted during 2020–24.20
4. Recommendations
Due to the COVID-19 related lockdown, the potential increase in incidence and mortality due to TB may wipe out the gains made in the last few years.
To address the issue of excess mortality due to lockdown related under-detection, adequate planning and preparation for routine implementation of national programmes should be done. To begin with it is imperative that we first restore routine TB services. This has to be followed by a combination of measures: access to food through universal PDS, direct cash transfers and making gainful employment available.
We recommend that in India, with the largest population of malnourished people in the world, enhanced entitlements and improved diversity of diet enabled by India's large PDS is an urgent imperative. This will improve economic productivity of the poor as well as mitigate the nutritional crisis that is now unfolding and may have secondary effects of prevention of increased morbidity due to TB and other infections. The allocation for cereals will have to be increased till the normalcy returns. The PDS should start making pulses available at subsidised prices to enable intake in quantities sufficient to meet the daily requirement of 40 g per day per adult.25 In addition, the Government must also consider transferring a fixed amount of money directly to the bank accounts of those below poverty line or using any other feasible economic cut-off (social protection). Similar to the 22.5 billion US$ economic relief package that was announced for the poor on 26 March 2020 (included direct benefit transfer of 6.6US$ per month for three months for more than 0.3 billion beneficiaries), the Government should consider more direct income transfers to the poor while the economic stimulus restarts the economy.31 , 44 Livelihoods are critical in this phase, and measures to reduce unemployment in the poor, including opportunities for rural employment through the Mahatma Gandhi National Rural Employment Guarantee Scheme will be crucial.44
Short, medium and long-term measures for improving coverage and efficiency of PDS along with measures for social protection of migrant daily wage labourers are recommended. Urgently implementing the short term measures are important considering food availability is poorer in the months of June to September (during monsoons) as illustrated in the higher underweight seen in tribal children from Odisha in these months.34 This attention to diets and social protection will have an impact not only on TB burden and mortality but also on morbidity and mortality to a range of infectious diseases.
This should be supported by supplementary measures like intensive community engagement, maintaining awareness of the importance of TB services while emerging from the COVID-19 response, and ramped-up active case-finding, including rapid scale-up of contact tracing to compensate for missed diagnoses during the lockdown period.41
Among patients detected with TB, the programme should consider an operational plan to ensure systematic detection, referral and management of severe TB including strengthening of clinical care at district hospitals. As of now severe TB is not routinely reported within India's national TB elimination programme. This should be done at the time of notification. TB deaths occur predominantly within the first two months (early deaths).42 , 43 Most TB deaths in India occur outside health facilities and could be prevented by timely referral and comprehensive care including treatment of comorbidities like severe undernutrition.45
These measures may be implemented at least in the states with higher under-detection (see Table 1 and Fig. 1) and states with poor nutritional indicators and high load of reverse distress migration back to the rural areas (Jharkhand, Bihar, Odisha, Uttar Pradesh, Madhya Pradesh and Rajasthan).
5. Limitations
The purpose of this manuscript is to bring to attention the lockdown induced impoverishment, development and worsening of malnutrition, disruption of TB services and their potential impact on TB incidence and mortality. The numbers for India predicted in this manuscript are estimates based on modelling data from other studies. The log–linear relationship between TB and BMI is based on six studies, all from high-income countries.20 We have assumed similar under-detection among TB patients living with and without HIV. We have not provided a combined increase in TB incidence and mortality due to lockdown induced impoverishment and under-detection. Despite this, the numbers estimated and presented are significant enough for the programme to act.
The present situation is dynamic and evolving. There are many other factors that can modify the final impact. Among these, the response of the public health system, the social protection provided by different state governments to the poor and the responsiveness of the economy to the stimulus offered will shape the future of the TB epidemic.
6. Conclusion
To conclude, there has been a large scale disruption in TB services and worsening of socio-economic determinants of TB in the poor in India. COVID-19 induced shock though transient may take a significant time to return to normalcy and could have significant impact on TB incidence and mortality. Lockdown associated worsening of undernutrition and poverty along with perturbation of TB detection can result in a significant increase in TB incidence and mortality. A similar increase in TB incidence and mortality was documented in Cuba in the 1990s following an economic crisis. There is a need to prevent this reversal of gains made in reduction of TB incidence and mortality over the past five years. The Government should immediately consider steps to counter the economic and nutritional impact of this crisis by social protection measures (through cash transfers), restoring livelihoods, improving quantity and quality of diets through changes in the PDS, ramped up enhanced (community involvement) and active case finding initiatives in high risk groups and emphasis on identification and management of severe TB disease.
Disclaimer
The contents of this paper do not necessarily reflect the views of the organizations the authors are affiliated to.
Author contributions
Conception of the article: AB; preparing the first draft: HDS; AB and HDS critically reviewed the paper and approved the final draft.
Conflicts of interest
All authors have none to declare.
Acknowledgements
We acknowledge the following for providing critical inputs: Sundari Ravindran, Principal Visiting Fellow, United Nations University - International Institute for Global Health; Padmini Swaminathan, Former Director and RBI Professor, Madras Institute of Development Studies, Chennai; and Satya Sivaraman, Public Health Researcher.
References
- 1.World Health Organization (WHO) 2019. Global Tuberculosis Report 2019. Geneva, Switzerland. [Google Scholar]
- 2.Revised National Tuberculosis Control Programme (RNTCP); Central TB Division . 2017. National Strategic Plan for TB Elimination 2017-25. New Delhi, India. [Google Scholar]
- 3.Houben R., Dodd P. The global burden of latent tuberculosis infection: a Re-estimation using mathematical modelling. PLoS Med. 2016;13(10):e1002152. doi: 10.1371/journal.pmed.1002152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma N., Basu S., Chopra K.K. Achieving TB elimination in India: the role of latent TB management. Indian J Tubercul. 2019;66(1):30–33. doi: 10.1016/j.ijtb.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Bhargava A. Undernutrition, nutritionally acquired immunodeficiency, and tuberculosis control. BMJ. 2016;355 doi: 10.1136/bmj.i5407. i5407. [DOI] [PubMed] [Google Scholar]
- 6.Shaji B., Arun Thomas E.T., Sasidharan P.K. Tuberculosis control in India: refocus on nutrition. Indian J Tubercul. 2019;66(1):26–29. doi: 10.1016/j.ijtb.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Katayama R., Wadhawa D. Half of the world's poor live in just 5 countries. World Bank Blogs. 2019 https://blogs.worldbank.org/opendata/half-world-s-poor-live-just-5-countries [Google Scholar]
- 8.Ministry of Statistics And Programme Implementation; Government of India . 2018. India in figures. 2018. New Delhi, India. [Google Scholar]
- 9.Indian Institute of Population Sciences . 2017. National family and health survey (NFHS-4), 2015-16. Mumbai, India. [Google Scholar]
- 10.World Health Organization (WHO) 1995. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva, Switzerland. [PubMed] [Google Scholar]
- 11.National Sample Survey Office; Ministry of Statistics and Programme Implementation; Government of India . 2015. National Sample Survey 68th Round: Public Distribution System and Other Sources of Household Consumption, 2011-12. New Delhi, India. [Google Scholar]
- 12.National Nutrition Monitoring Bureau . 2012. India rural third repeat survey of diet and nutritional status 2011–12. Hyderabad, India. [Google Scholar]
- 13.Rampal P. An analysis of protein consumption in India through plant and animal sources. Food Nutr Bull. 2018;39(4):564–580. doi: 10.1177/0379572118810104. [DOI] [PubMed] [Google Scholar]
- 14.Tata NIN Centre of excellence in public health nutrition. Overview Food Nutrition India. 2020 https://www.dashboard.nintata.res.in/#/dashboard/food-intake [Google Scholar]
- 15.Varadharajan K.S., Thomas T., Kurpad A. The Indian national food security Act, 2013: a commentary. Food Nutr Bull. 2014;35(2):253–265. doi: 10.1177/156482651403500212. [DOI] [PubMed] [Google Scholar]
- 16.George N.A., McKay F.H. The public distribution system and food security in India. Int J Environ Res Publ Health. 2019;16(17):3221. doi: 10.3390/ijerph16173221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mazumdar S., Satyanarayana S., Pai M. Self-reported tuberculosis in India: evidence from NFHS-4. BMJ Glob Heal. 2019;4(3) doi: 10.1136/bmjgh-2018-001371. e001371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shewade H.D., Gupta V., Satyanarayana S., et al. Active case finding among marginalised and vulnerable populations reduces catastrophic costs due to tuberculosis diagnosis. Glob Health Action. 2018;11(1):1494897. doi: 10.1080/16549716.2018.1494897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oxlade O., Murray M. Tuberculosis and poverty: why are the poor at greater risk in India? PloS One. 2012;7(11):e47533. doi: 10.1371/journal.pone.0047533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lönnroth K., Williams B.G., Cegielski P., Dye C. A consistent log-linear relationship between tuberculosis incidence and body mass index. Int J Epidemiol. 2010;39(1):149–155. doi: 10.1093/ije/dyp308. [DOI] [PubMed] [Google Scholar]
- 21.Cegielski J.P., Arab L., Cornoni-Huntley J. Nutritional risk factors for tuberculosis among adults in the United States, 1971–1992. Am J Epidemiol. 2012;176(5):409–422. doi: 10.1093/aje/kws007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhargava A., Benedetti A., Oxlade O., Pai M., Menzies D. Undernutrition and the incidence of tuberculosis in India: national and subnational estimates of the population-attributable fraction related to undernutrition. Natl Med J India. 2014;27(3):128–133. [PubMed] [Google Scholar]
- 23.Lönnroth K., Castro K.G., Chakaya J.M., et al. Tuberculosis control and elimination 2010–50: cure, care, and social development. Lancet. 2010;375(9728):1814–1829. doi: 10.1016/S0140-6736(10)60483-7. [DOI] [PubMed] [Google Scholar]
- 24.Boccia D., Hargreaves J., de Stavola B.L., et al. The association between household socioeconomic position and prevalent tuberculosis in Zambia: a case-control study. PloS One. 2011;6(6) doi: 10.1371/journal.pone.0020824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Statistics and Programme Implementation & World Food Programme . 2019. Food and Nutrition Security Analysis, India, 2019. New Delhi, India. [Google Scholar]
- 26.Dev S., Sengupta R. 2020. “Covid-19: impact on the Indian economy,” Indira Gandhi Institute of development research, Mumbai working papers 2020-013. Mumbai, India. [Google Scholar]
- 27.ENS Economic Bureau Unemployment rate soars to 27.11% amid COVID-19 pandemic: CMIE. The Indian Express. 2020 [Google Scholar]
- 28.International Labour Organization (ILO) 2nd Ed. 2020. ILO Monitor: COVID-19 and the World of Work. Geneva, Switzerland. [Google Scholar]
- 29.Saini S., Khatri P. COVID 19 may double poverty in India. Financ Express. April 30, 2020 [Google Scholar]
- 30.Stranded Workers Action Network 21 Days and counting: COVID-19 lockdown, migrant workers, and the inadequacy of welfare measures in India. 2020. https://www.thehindu.com/news/resources/article31442220.ece/binary/Lockdown-and-Distress_Report-by-Stranded-Workers-Action-Network.pdf
- 31.Press Information Bureau; Government of India Finance minister announces rs 1.70 lakh crore relief package under pradhan mantri garib kalyan yojana for the poor to help them fight the battle against corona virus. 2020. https://www.mohfw.gov.in/pdf/MoFPMGaribKalyanYojanaPackage.pdf
- 32.National Institute of Nutrition . 2010. Dietary guidelines for Indians. Hyderabad, India. [Google Scholar]
- 33.National Sample Survey Office; Ministry of Statistics and Programme Implementation; Government of India . 2014. Nutritional intake in India 2011-2012. Report No. 560(68/1.0/3) Mumbai, India. [Google Scholar]
- 34.Meshram, Balakrishna N., Arlappa N. Mallikarjun Rao K, Laxmaiah A, Brahmam GN V. Prevalence of undernutrition, its determinants, and seasonal variation among tribal preschool children of Odisha state, India. Asia Pac J Publ Health. 2014;26(5):470–480. doi: 10.1177/1010539512441492. [DOI] [PubMed] [Google Scholar]
- 35.Garfield R., Santana S. The impact of the economic crisis and the US embargo on health in Cuba. Am J Publ Health. 1997;87(1):15–20. doi: 10.2105/ajph.87.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marrero A., Caminero J.A., Rodríguez R., Billo N.E. Towards elimination of tuberculosis in a low income country: the experience of Cuba, 1962-97. Thorax. 2000;55(1):39–45. doi: 10.1136/thorax.55.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burke S.J., Lass E., Thistle P., et al. Increased incidence of tuberculosis in Zimbabwe, in association with food insecurity, and economic collapse: an ecological analysis. PloS One. 2014;9(2) doi: 10.1371/journal.pone.0083387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization (WHO) Updated WHO information note: ensuring continuity of TB services during the COVID-19 pandemic. 2020. https://www.who.int/news-room/detail/12-05-2020-updated-who-information-note-ensuring-continuity-of-tb-services-during-the-covid-19-pandemic
- 39.National TB . Nikshay Reports; India: 2020. Elimination Programme.https://reports.nikshay.in/Reports/TBNotification [Google Scholar]
- 40.Glaziou P. Predicted impact of the COVID-19 pandemic on global tuberculosis deaths in 2020. medRxiv. 2020 doi: 10.1101/2020.04.28.20079582. [DOI] [Google Scholar]
- 41.Stop TB Partnership in collaboration with Imperial College;Avenir Health . Johns Hopkins University and USAID; Geneva, Switzerland: 2020. The Potential Impact of the COVID-19 Response on Tuberculosis in High-Burden Countries: A Modelling Analysis. [Google Scholar]
- 42.Min J., Kim J.S., Kim H.W., et al. Clinical profiles of early and tuberculosis-related mortality in South Korea between 2015 and 2017: a cross-sectional study. BMC Infect Dis. 2019;19(1):735. doi: 10.1186/s12879-019-4365-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oliveira SP de, Silveira JTP da, Beraldi-Magalhães F., Oliveira RR de, Andrade L de, Cardoso R.F. Early death by tuberculosis as the underlying cause in a state of Southern Brazil: profile, comorbidities and associated vulnerabilities. Int J Infect Dis. 2019;80:S50–S57. doi: 10.1016/j.ijid.2019.02.043. [DOI] [PubMed] [Google Scholar]
- 44.Press Information Bureau Government of India. Ministry of finance: finance minister announces government reforms and enablers across seven sectors under aatma nirbhar bharat abhiyaan. 2020. https://pib.gov.in/PressReleasePage.aspx?PRID=1624661
- 45.Bhargava A., Bhargava M. Tuberculosis deaths are predictable and preventable: comprehensive assessment and clinical care is the key. J Clin Tuberc Other Mycobact Dis. 2020;19:100155. doi: 10.1016/j.jctube.2020.100155. [DOI] [PMC free article] [PubMed] [Google Scholar]