Abstract
Introduction
Since the emergence of Coronavirus Disease 19 (COVID-19) pandemic, multiple neurologic complications in infected patients have been reported. Despite these reports, the mechanism of COVID-19 nervous system injury is not well understood. We report the case of a COVID-19 patient with diffuse microhemorrhages on brain MRI, positive anticardiolipin antibodies, and purpuric rash with biopsy showing a thrombotic vasculopathy, all features suggestive of secondary microangiopathy.
Case Report
A 69-year-old male with history of hypertension, chronic kidney disease, and hypothyroidism presented with one week of dyspnea, cough, diarrhea, and fevers. Chest x-ray demonstrated bibasilar consolidations and nasopharyngeal reverse transcriptase polymerase chain reaction confirmed SARS-CoV-2 infection. He had subsequent respiratory decline requiring intubation the day after admission. He developed a truncal morbilliform rash and diffuse purpura, a biopsy of which showed small dermal blood vessels with intraluminal microthrombi consistent with thrombotic vasculopathy. He was found to have elevated aCL IgM and IgG and equivocal lupus anticoagulant study. Brain MRI obtained for persistent encephalopathy showed innumerable areas of susceptibility weighted imaging changes throughout the bilateral juxtacortical white matter, corpus callosum, basal ganglia, and brainstem, as well as multiple small areas of FLAIR hyperintensities, consistent with microhemorrhage
Discussion
While there have been several reported cases of neurologic manifestations of COVID-19, the pathophysiology may not be related to neurotropism of the virus itself. The new development of antiphospholipid antibodies and thrombotic vasculopathy in dermal blood vessels in this patient suggest a secondary microangiopathy potentially related to a virally-induced inflammatory state.
Key Words: Cerebral Microhemorrhage, COVID-19, Antiphospholipid antibodies Microangiopathy, Magnetic Resonance Imaging
Abbreviations: MRI, magnetic resonance imaging; COVID-19, coronavirus disease 2019; SWI, susceptibility-weighted imaging; FLAIR, l fluid-attenuated inversion recovery; DWI, diffusion-weighted imaging; ADC, apparent diffusion coefficient
Introduction
Since the emergence of Coronavirus Disease 19 (COVID-19), there have been reports of neurological complications in infected patients (1, 2, 3). The mechanism of COVID-19 nervous system injury is not fully understood; however, brain magnetic resonance imaging (MRI) findings including diffuse microhemorrhages suggest hypoxia or small vessel vasculitis (4). We report a COVID-19 patient with diffuse microhemorrhages on brain MRI, positive anticardiolipin (aCL) antibodies, and purpuric rash with biopsy showing a thrombotic vasculopathy, all features suggestive of secondary microangiopathy.
Case Report
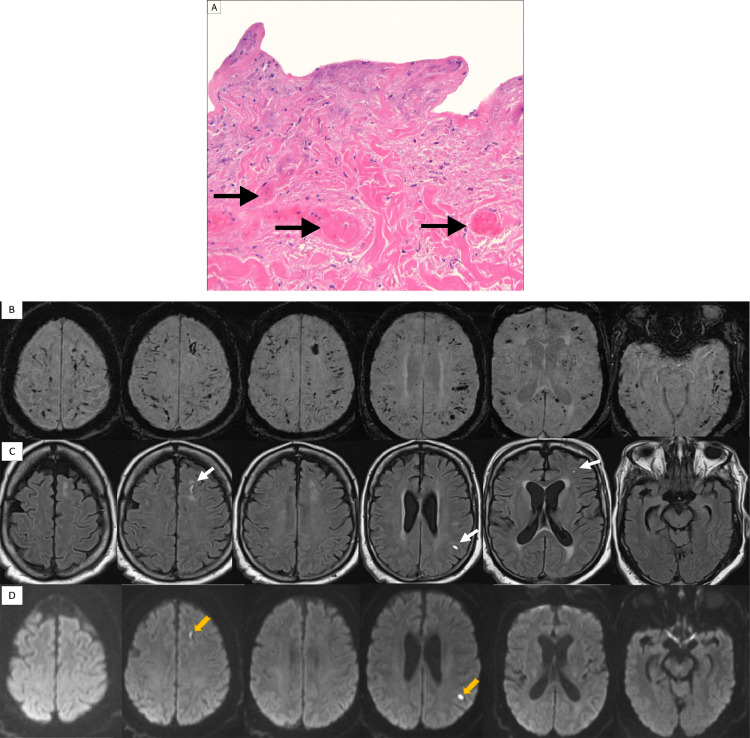
A 69-year-old male with history of hypertension, chronic kidney disease, and hypothyroidism presented with one week of dyspnea, cough, diarrhea, and fevers. His neurological examination was normal. Laboratory testing showed elevated procalcitonin (0.24 ng/mL, reference < 0.09), C-reactive protein (5.1 mg/dL, reference < 0.9), and hypoxemia. Chest x-ray demonstrated bibasilar consolidations and nasopharyngeal reverse transcriptase polymerase chain reaction confirmed SARS-CoV-2 infection. He had subsequent respiratory decline requiring intubation the day after admission. He was found to have elevated ferritin (1551 ng/mL, reference < 565.7), interleukin-6 (77.3 pg/mL, reference < 6.0), D-Dimer (11,360 ng/mL, reference < 500), and fibrinogen (821 mg/dL, reference < 400). Platelets remained normal throughout hospitalization. He developed a truncal morbilliform rash and diffuse purpura, a biopsy of which showed small dermal blood vessels with intraluminal microthrombi consistent with thrombotic vasculopathy (Fig. 1 -A). He required continuous renal replacement therapy for worsening kidney injury which was complicated by frequent dialysis line clotting. He was found to have elevated aCL IgM and IgG and equivocal lupus anticoagulant study. Despite respiratory improvement, his mental status deteriorated. Brain MRI obtained for persistent encephalopathy showed innumerable areas of susceptibility weighted imaging changes throughout the bilateral juxtacortical white matter, corpus callosum, basal ganglia, and brainstem (Fig. 1–B) as well as multiple small areas of FLAIR (Fig. 1–C) and DWI (Fig. 1–D) hyperintensities, consistent with microhemorrhage. Ultimately, his respiratory and neurologic status declined over the following days resulting in death.
Fig. 1.
Skin biopsy and brain MRI findings in a patient with COVID-19.
Fig. 1-A: A photomicrograph (100x) of a punch biopsy taken from the border of a livedoid plaque involving the patient's buttocks and sacrum demonstrating fibrin thrombi (black arrows) in numerous blood vessels, consistent with a thrombotic vasculopathy. B: Brain MRI SWI sequences demonstrating innumerable areas of microhemorrhage throughout the bilateral juxtacortical white matter, corpus callosum, basal ganglia, brainstem, and cerebellum without clear asymmetry. C: Brain MRI FLAIR sequences showing discrete areas of FLAIR hyperintensity (white arrows) correlating with some of the larger areas of SWI changes suggesting larger macrohemorrhage. D: Brain MRI DWI sequences showing areas of diffusion restriction (yellow arrows) correlating with the FLAIR, ADC (not pictured), and with some of the SWI abnormalities.
Discussion
While there have been several reported cases of neurologic manifestations of COVID-19, the pathophysiology remains unclear and may not be related to neurotropism of the virus itself. COVID-19 has been linked to new development of antiphospholipid antibodies (5), which are known to result in microangiopathy and capillaroscopic microhemorrhages and linked to thrombotic events in patients with rheumatologic diseases (6,7). The finding of thrombotic vasculopathy in dermal blood vessels in this patient may provide insight into the pathophysiology of COVID-19-associated cerebral microhemorrhages and suggests a secondary microangiopathy potentially related to the formation of aCL antibodies and inflammatory state.
Declarations of Competing Interest
None
References
- 1.Politi L.S., Salsano E., Grimaldi M. Magnetic resonance imaging alteration of the brain in a patient with Coronavirus disease 2019 (COVID-19) and Anosmia. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.2125. [DOI] [PubMed] [Google Scholar]
- 2.Poyiadji N., Shahin G., Noujaim D. COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mao L., Jin H., Wang M. Neurologic manifestations of hospitalized patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radmanesh A., Derman A., Lui Y.W. COVID-19 -associated diffuse Leukoencephalopathy and Microhemorrhages. Radiology. 2020 doi: 10.1148/radiol.2020202040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y., Xiao M., Zhang S. Coagulopathy and antiphospholipid antibodies in patients with covid-19. New England Journal of Medicine. 2020;382:E38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang S., Wu Z., Li P. Evaluation of the clinical performance of a novel chemiluminescent immunoassay for detection of anticardiolipin and anti-beta2-glycoprotein 1 antibodies in the diagnosis of antiphospholipid syndrome. Med. (United States) 2015;94:e2059. doi: 10.1097/MD.0000000000002059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sibbitt W.L., Brooks W.M., Kornfeld M. Magnetic Resonance Imaging and Brain Histopathology in Neuropsychiatric Systemic Lupus Erythematosus. Semin. Arthritis Rheum. 2010;40:32–52. doi: 10.1016/j.semarthrit.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]