The first case of COVID-19 in Turkey was announced on March 11, 2020, by the Ministry of Health. In response, on March 20, 2020, the state and private hospitals that contain infectious diseases and clinical microbiology, pulmonology, at least two physicians from internal medicine department and third-degree adult intensive care service, have been declared as “the Pandemic Hospital" in the country (Pandemic Hospitals, Ministry of Health-Turkey, 2020). After becoming a pandemic hospital, Ege University Medical Faculty Hospital has been the only university hospital in Turkey that continued the child and adolescent psychiatry inpatient service during the outbreak. Also, it has been the only child and adolescent psychiatry inpatient clinic in the Region. During this period, new arrangements and additional measures were regarded as a necessity in the management of both new and present patients who will be admitted to the service. The first objective of this article; is to define, as the child psychiatry inpatient service team, the approaches to patients who need both professional help and treatment in terms of mental health and need protection from an infection during the Covid-19 outbreak. Secondly, to evaluate the adaptation of the clinical skills (mechanism) to this critical process.
The Clinical Global Impression Scale (CGIS) (Forkmann et al., 2011) was applied during the hospitalization and discharge of our cases. Children and parents participated in a semi-structured, face to face diagnostic interview (K-SADS-PL; Schedule for Affective Disorders and Schizophrenia for School-Aged Children - Present and Lifetime Version) (Kaufman et al., 2000). "Coronavirus Risk Assessment Form" was prepared for the new patients according to the possible case definition of the Ministry of Health prior to hospitalization (Covid-19 Guideline, Ministry of Health-Turkey, 2020). In the ” Coronavirus Risk Assessment Form ” issued; it was aimed to evaluate the exposure of patients and companions with people returning from abroad and risk group, questioning the symptoms of the disease and other medical conditions. In this process, the 'Hospitalization Consent Form' was received from new inpatients, where it is informed that the hospital is a pandemic hospital and there are hygiene and social isolation rules to be followed.
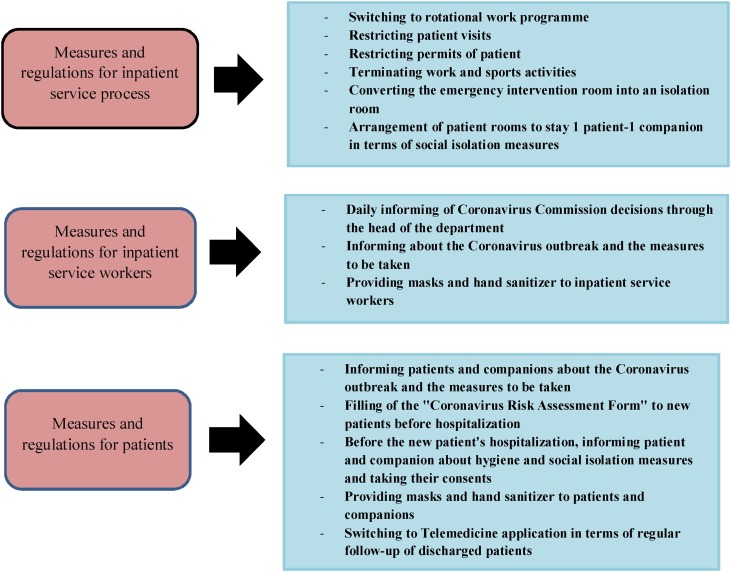
After the announcement of Ege University Medical Faculty Hospital to be a pandemic hospital in March 2020, some changes are made in the operation of the inpatient service. The patients who are in the recovery process that may be suitable for outpatient treatment have been discharged and it has been decided to continue their psychiatric monitoring with the practice of "Tele-Medicine" at regular intervals. Inpatient service treatment has been continued for patients whose discharge is not suitable. Our clinic worked at full capacity, with one patient and accompanying person in each room. Psychosocial studies are planned as activities for the individual or organized by means to protect social distance for patients; individual work schedulings such as recognizing emotions, writing stories, reading books, creating behavioural charts have been performed. Patients are provided with surgical masks for their protection (Fig. 1 ).
Fig. 1.
Inpatient service regulations during the pandemic.
When the first case occurred on March 11, 2020, there were 9 patients in the Ege University Faculty of Medicine Child and Adolescent Psychiatry Inpatient Service. Of these patients, 3 were eating disorders, 3 were mood disorders, 2 were psychotic disorders, and 1 was autism spectrum disorders. 14 of the 19 patients who were hospitalized during this period have been discharged. Six patients who improved according to their hospitalization status have been discharged with the consent and cooperation of the family, considering that the conditions of environmental therapy could not be maintained and quarantine treatment at home would be better for the family. Eight patients requested discharging voluntarily. The family of 4 of the 8 patients (Patient 6,7,9 and 10) wanted to discharge their children even though the inpatient service treatment was recommended by the team. They were discharged by explaining the possible risks. A total of 5 cases are still monitored, including 1 anorexia nervosa, 1 schizophrenia and 2 unspecified bipolar and related disorders, and 1 autism spectrum disorder (Table 1 ).
Table 1.
The profile and CGI-S scores of patients treated in inpatient service during the pandemic period.
| Patient No | Age | Sex | Psychiatric Diagnosis | CGI-S Score In Hospitalization | Medications | Length of Stay /The DayOf Discharge | CGI-S Score In Discharge | Scales/Measurements Administered After 1 Month |
|---|---|---|---|---|---|---|---|---|
| 1 | 14 | Female | Anorexia Nervosa MDD* Social Anxiety Disorder |
6 | Sertaline, Risperidone, Aripiprazole, Lorazepam,Biperiden |
58 days / 9th day | 3 | CGI-S:4 Discharged BMI:16,8 |
| 2 | 7 | Male | ADHD* +CD* ASD* |
5 | Methylphenidate, Risperidone, Aripiprazole |
8 days / 9th day | 3 | CGI-S:3 |
| 3 | 15 | Female | Unspecified BD* ADHD* CD* |
6 | Methylphenidate, Risperidone, Olanzapine, Zuclopenthixol, Aripiprazole,Lorazepam, Escitalopram |
38 days / 10th day | 3 | CGI-S:3 |
| 4 | 15 | Male | MDD* Social Anxiety Disorder |
6 | Sertaline, Risperidone, Aripiprazole, Lorazepam |
24 days / 10th day | 3 | U |
| 5 | 14 | Female | Schizophreniform Disorder | 6 | Paliperidone,Olanzapine Lorazepam, Biperiden |
24 days / 10th day | 3 | CGI-S:3 |
| 6a | 17 | Female | Unspecified Psychotic Disorder Mild ID* |
5 | Risperidone, Quetiapine | 22 days / 15th day | 4 | CGI-S:3 |
| 7a | 14 | Male | ADHD* CD* OCD* |
6 | Risperidone,Aripiprazole Olanzapine,Biperiden Escitalopram |
19 days / 21 st day | 4 | U |
| 8 | 17 | Female | Unspecified BD* | 5 | Sertraline, Risperidone Aripiprazole Lorazepam |
8 days / 13rd day | 3 | CGI-S:3 |
| 9a | 16 | Male | Schizophreniform Disorder | 4 | Olanzapine, Risperidone Lorazepam |
2 days / 9th day | 4 | CGI-S:3 |
| 10a | 17 | Female | Unspecified BD* ADHD* Bulimia Nervosa |
6 | Risperidone, Lorazepam | 3 days / 13rd day | 5 | CGI-S:5 |
| 11 | 8 | Female | Coffin Siris Type1 ASD* Mild ID* |
7 | Risperidone, Escitalopram Melatonin, Oxcarbazepine |
41 days / 8th day | 3 | CGI-S:3 |
| 12 | 16 | Male | Bulimia Nevrosa ADHD* |
6 | Escitalopram, Valproic acid, Methylphenidate, Haloperidol,Clomipramine, Lorazepam, Topiramate, Biperiden | 63 days / 6th day | 3 | CGI-S:3 |
| 13 | 13 | Female | Unspecified BD* | 5 | Sertraline, Risperidone, Aripiprazole, Lorazepam, Olanzapine | 38 days / 2nd day | 3 | CGI-S:3 |
| 14 | 15 | Female | Anorexia Nervosa | 7 | Sertraline, Aripiprazole, Risperidone | The 10th day of the pandemic hospitalized, the hospitalization continues | 4** | |
| 15 | 17 | Female | MDD*,with psychotic features | 7 | Risperidone, Olanzapine, Lorazepam, Fluoxetine | 22 gün/ 41 st day | 3 | CGI-S:3 |
| 16 | 14 | Female | ADHD* Unspecified BD* |
6 | Escitalopram, Methylphenidate, Paliperidone, Zuclopenthixol, Lorazepam | The 34th day of the pandemic hospitalized, the hospitalization continues | 4** | |
| 17 | 17 | Male | Schizophrenia | 7 | Valproic acid, Olanzapine, Quetiapine, Haloperidol, Lorezapam, Escitalopram, Zuclopenthixol | The 48th day of the pandemic hospitalized, the hospitalization continues | 6** | |
| 18 | 17 | Male | ASD* OCD* Unspecified BD* |
7 | Valproaic acid, Paliperidone, Olanzapine Chlorpromazine, Lorazepam, Biperiden | The 59th day of the pandemic hospitalized, the hospitalization continues | 6** | |
| 19 | 15 | Female | Unspecified BD* | 7 | Olanzapine, Sertraline, Lorezepam | The 62nd day of the pandemic hospitalized, the hospitalization continues | 6** |
aPatients who wanted to discharged voluntarily even though was recommended to continue inpatient treatment.
bThe day when discharged after the first case announced on March 11, 2020 in Turkey.
cScales and its scores administered in 1 st month Telemedicine interview after discharging.
*: ADHD:Attention-Deficit/Hyperactivity Disorder, CD:Conduct Disorder, Unspecified BD: Unspecified Bipolar and Related Disorder, ASD: Autism Spectrum Disorder; Mild ID: Mild Intellectual Disability, OCD:Obsessive-Compulsive Disorder MDD:Major Depressive Disorder.
U: Patients who unreached by Telemedicine.
**: CGI-S scores of patients who continued hospitalization.
The mean value of the CGI-S scores, evaluated in the examination during the first hospitalization of nineteen patients, has been determined as 6 ± 0,88 while the mean value of 14 patients after discharge is 3.35 ± 0,63. 12 of the 14 patients whose follow-up continued with the Telemedicine method have been reached regularly. The CGI-S mean value of these 12 patients, evaluated by Telemedicine interview in the 1 st month after their discharge, is 3.25 ± 0,62. While there is a significant difference between the CGI-S scores of hospitalization and discharge and 1 st Month Telemedicine CGI-S (p < 0.001), there is no significant difference found between discharge CGI-S and 1 st Month Telemedicine CGI-S scores. There is no statistically significant difference between the CGI-S scores of the patients who are hospitalized to the service after the first occurrence of the case in Turkey and the CGI-S scores of the patients who are hospitalized before the outbreak (p = 0.179).
The correlation between the length of hospitalization and the CGI-S scores of discharge were examined. A significant negative correlation detected between CGI-S scores; as the duration of hospitalization of the inpatients prolonged during the pandemic period, the discharge score of CGI-S showed a negative correlation (r = −0,622).
The average length of stay of patients discharged after the first case appeared in Turkey is 26.4 days. On the other hand, the average length of stay of the patients who are hospitalized after the outbreak occurred is 10.3 days. The length of the stays varies in child and adolescent inpatient services. While in countries such as the USA, Australia, or New Zealand, the average length of stay is usually less than four weeks due to health insurance systems; longer length of stay has been reported in Europe (Mayes et al., 2001; Gavidia-Payne et al., 2003; Swadi and Bobier, 2005). Considering the necessity of protection of some patients from the virus in the difficult pandemic period, not being able to maintain the environmental therapy conditions for improving patients, deciding that the quarantine at home would be better for the family and some patients requesting to discharge voluntarily; the length of the stay times have been shorter in the epidemic period.
A significant difference has been found when the hospitalization and discharge CGI-S scores were compared. Despite the decrease in length of hospitalization and restrictions in the functioning of the service due to the outbreak, the significant improvement has been observed exhibits that inpatient treatment is effective in children and adolescents. There has been no statistically significant difference between the CGI-S scores and length of stay before and after the outbreak was announced. A significant negative correlation relationship has been detected between the duration of hospitalization and CGI-S scores of discharge. As the length of stay prolongs, decreased CGI-S scores can indicate that the patients who continued hospitalization are benefiting from the treatment.
Taking into account the recommendations of the Turkish Psychiatric Association for the work order in the psychiatric inpatient services during the COVİD-19 outbreak (Psychiatric Association of Turkey, 2020), swab samples have been taken from four patients who were admitted from the outside. Both PCR tests of the first day of hospitalization and the 4th-day control have been resulted in negative. The absence of positive patients may depend on the measures taken and the success of the applied isolation rules.
A great burden is imposed on health systems during COVID-19 Pandemic. In this process, it is essential to follow the guidelines on transmission of infection and provide inpatient service treatment for child and adolescent in urgent need of mental health treatment. Length of hospitalization may be shorter in the pandemic period and high rate of antipsychotic use and predominance of patients with insufficient response to monotherapy may be related to hospitalization of patients with more severe disease during pandemic period. Timely organized regulations in psychiatry clinics can be effective against risk of transmission. This study shows the importance of how the pandemic process and the psychiatric disease treatment process can be carried out together. The continuation of the treatment services with infectious prevention measures in the field of mental health during pandemic times has an crucial place. As the healthcare professionals in the field of Child and Adolescent Mental Health, we think that it may be important to share inpatient service functioning and experiences in the face of the COVID-19.
Ethical standards
The study was initiated with the approval of the Ege University Ethical Committee of Clinical Research (decision no: 20-5T/55).
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
The authors would like to thank Doga Feltham for English language editing.
References
- Ministry of Health; Turkey: 2020. Covid-19 Guideline.https://covid19bilgi.saglik.gov.tr/depo/rehberler/COVID-19_Rehberi.pdf [updated on 14.04.2020]; Available from: [Google Scholar]
- Forkmann T., Scherer A., Boecker M. The clinical global impression scale and the influence of patient or staff perspective on outcome. BMC Psychiatry. 2011;11:83–85. doi: 10.1186/1471-244X-11-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavidia-Payne S., Littlefiield L., Hallgren M., Jenkins P., Coventry N. Outcome evaluation of a statewide child inpatient mental health unit. Aust. N. Z. J. Psychiatry. 2003;37:204–211. doi: 10.1046/j.1440-1614.2003.01124.x. 2003. [DOI] [PubMed] [Google Scholar]
- Kaufman J., Birmaher B., Brent D.A., Ryan N.D., Rao U. K-SADS-PL. J. Am. Acad. Child Adolesc. Psychiatry. 2000;39(10):1208. doi: 10.1097/00004583-200010000-00002. 2000. [DOI] [PubMed] [Google Scholar]
- Mayes D.S., Calhoun S.L., Krecko V.F., Vesell H.P., Hu J. Outcome following child psychiatric hospitalization. J. Behav. Health Serv. Res. 2001;28:96–103. doi: 10.1007/BF02287238. 2001. [DOI] [PubMed] [Google Scholar]
- Ministry of Health; Turkey: 2020. Pandemic Hospitals.https://hasta.saglik.gov.tr/TR,64565/pandemi-hastaneleri.html [cited 2020 Mar 20]; Available from: [Google Scholar]
- Psychiatric Association of Turkey . 2020. Inpatient Psychiatry Clinic Model.https://www.psikiyatri.org.tr/uploadFiles/2142020175718-YatakliPsikiyatriModelEkli21042020.pdf [cited 2020 Apr 9]; Available from: [Google Scholar]
- Swadi H., Bobier C. Hospital admission in adolescents with acute psychiatric disorders: how long should it be? Australas. Psychiatry. 2005;13:165–168. doi: 10.1080/j.1440-1665.2005.02181.x. 2005. [DOI] [PubMed] [Google Scholar]