Abstract
Several cases have recently been reported concerning the development of a syndrome of acute lung injury associated with the use of electronic cigarettes, leading to respiratory failure and several deaths. We present a case of a young veteran who presented with e-cigarette vaping associated lung injury (EVALI) to a primary care clinic and who required subsequent inpatient admission and home oxygen therapy after discharge. The patient afterwards improved after a three-month course of steroids and cessation of THC-containing electronic cigarettes, consistent with previously reported cases. Furthermore, evidence on bronchoscopy and biopsy demonstrated intracellular lipid droplets in the patient's macrophages. This outpatient case of EVALI prompts primary care providers to raise suspicion of this condition, and enquire about the use of e-cigarettes, particularly THC-containing vaping products. Furthermore, in the setting of the COVID-19 pandemic, similar clinical and radiographic presentations between COVID-19 and EVALI can be seen.
Keywords: EVALI, e-cigarettes, THC e-Cigarettes, Hypoxemic respiratory failure
1. Background
Recently, several cases have been reported concerning the development of a syndrome of acute lung injury associated with the use of electronic cigarettes (e-cigarettes), leading to severe respiratory failure and several deaths. Most cases were associated with tetrahydrocannabinol (THC) -containing vaping products [1].
Prompt recognition of this clinical picture and aggressive supportive therapy may in some fortunate cases lead to a satisfactory reversion of lung pathology. Awareness of the catastrophic risks associated with this habit must be recognized by primary care providers in order to adopt policies to support patients to cease its use. We present here a case of a young veteran that presented with e-cigarette vaping associated lung injury (EVALI) in an outpatient clinical setting.
2. Case presentation
A 36-year-old male with a past medical history of irritable bowel syndrome and major depressive disorder was referred to the pulmonary clinic because of worsening dyspnea on exertion.
Three weeks prior he was admitted to another institution because of shortness of breath, cough and myalgias treated as community acquired pneumonia. There he was found to be hypoxemic, with an oxygen saturation of around 86% on room air. On interrogation he endorsed to occasionally smoke. His chest radiograph had an indeterminate infiltrate. Two days after staring antibiotics and supportive care, a 6-min-walk test demonstrated no need for supplemental oxygen use and was discharged with a 7-day course of antibiotics and prednisone.
Because of progression of dyspnea on exertion he was referred to our clinic by his primary provider for pulmonary evaluation. At that time he admitted continuing smoking, and on further questioning admitted vaping THC-containing e-cigarettes, as recent as during the past month. Vital signs demonstrated fevers (101.5 °F) and desaturation (SpO2 56%) on room air. Decision was made to refer to the emergency department to admit.
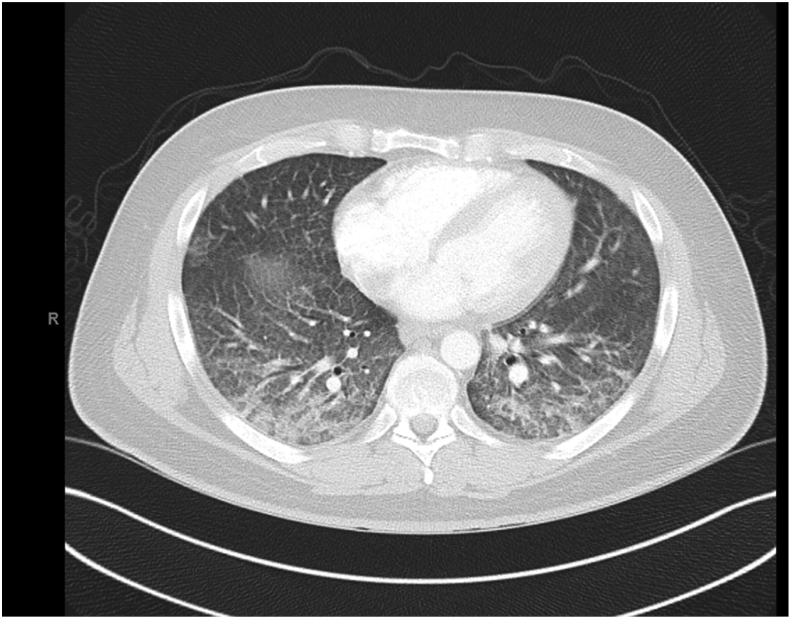
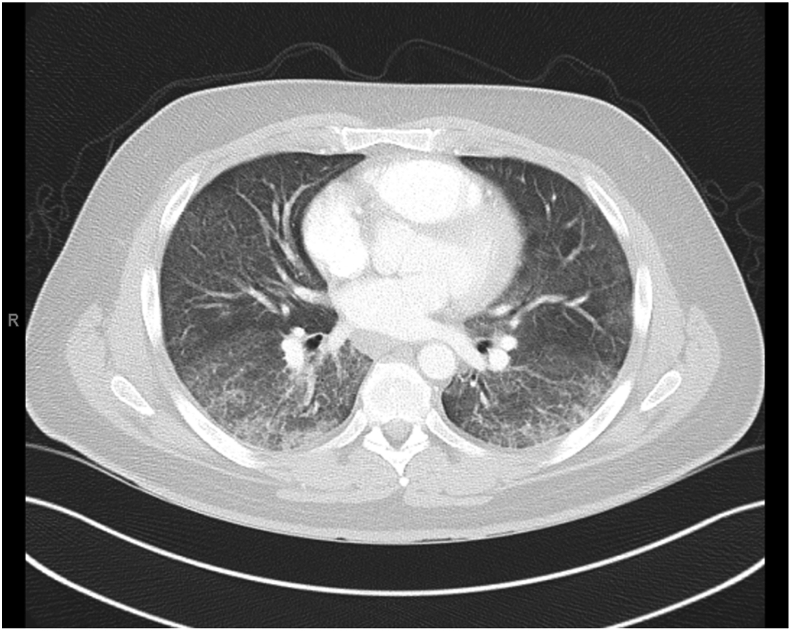
A chest computerized tomography with and without contrast showed bilateral peripheral and basilar ground glass opacities with mediastinal adenopathy and no evidence of pulmonary embolism (Fig. 1, Fig. 2). With the impression of possible non-specific interstitial pneumonitis, an autoimmune panel was obtained with negative results (negative p-ANCA, c-ANCA, anti Ro/La and ANA), albeit a positive C-reactive protein of 269mg/L.
Fig. 1.
CT Chest without contrast on presentation showing diffuse lung disease.
Fig. 2.
CT Chest without contrast on presentation demonstrating bilateral middle lobes diffuse disease.
A bronchoscopy with bronchoalveolar lavage (BAL) was performed which demonstrated clusters of small foamy macrophage with intracellular lipid droplets positive on oil red O stain. All microbiologic studies were negative.
The patient was started on systemic steroids and slowly began to improve. He was able to undergo pulmonary function testing, which showed no evidence of obstructive or restrictive lung disease, but a moderate loss of diffusing capacity of carbon monoxide (DLCO, 44%). Oxygen requirements through nasal cannula were calculated to be 2 L/m at rest and 5 L/m during ambulation. He was discharged to continue a one-month course of prednisone with supplemental oxygen.
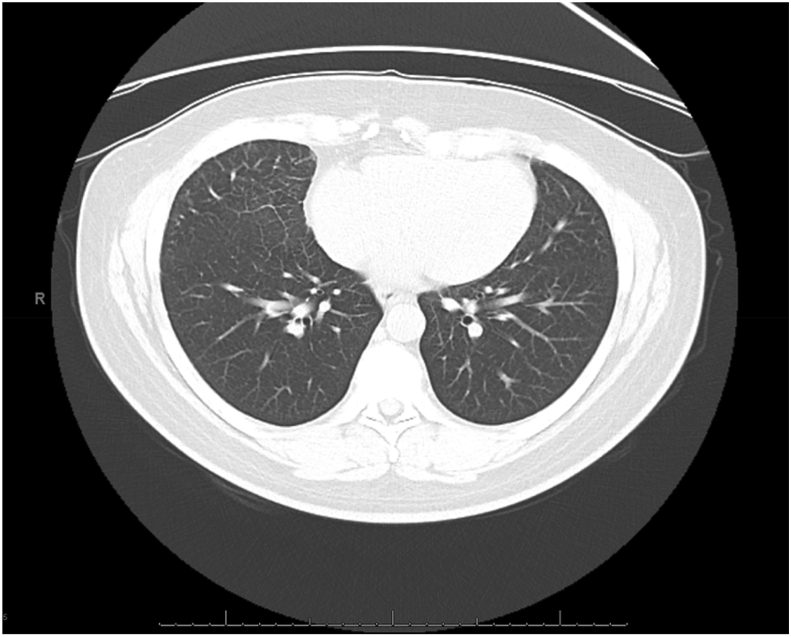
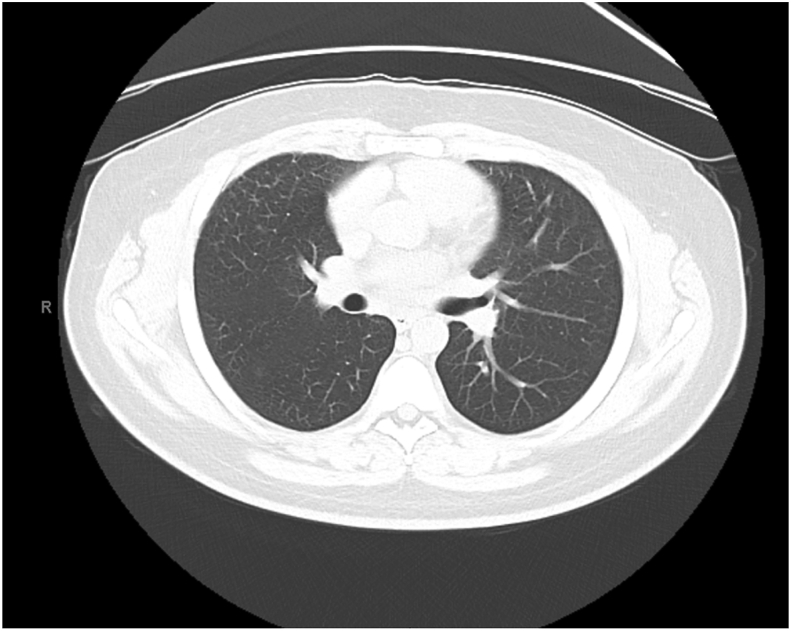
After a month of steroids and vaping cessation, he noticed a marked improvement of symptoms. At his three-month follow up, he no longer needed supplemental oxygen and a new chest CT showed complete resolution of the lung infiltrates (Fig. 3, Fig. 4). Repeat pulmonary function tests revealed correction of the previously noted diffusion abnormality.
Fig. 3.
CT Chest post-steroid course at 3 months demonstrating normalization of lung changes during EVALI.
Fig. 4.
CT Chest post-steroid course at 3 months demonstrating normalization of lung changes in middle lobes.
3. Discussion
This patient presented with clinical and epidemiologic features of EVALI. The CDC recently published guidelines for the identification of EVALI, which includes: (1) use of an e-cigarette (vaping) in 90 days before symptom onset, (2) pulmonary infiltrates (ground-glass opacities), and (3) absence of a pulmonary infection, or alternative plausible diagnosis (cardiac, rheumatologic or neoplastic process) [2]. Our patient also presented with the classic symptoms described in recent reports of more than 1000 cases, including dyspnea, cough, hypoxemia, and bilateral pulmonary infiltrates, with recovery after cessation of vaping [3].
Of interest in this case was the omission of diagnosis during a recent admission and during a first primary care visit (by a provider who referred to pulmonary evaluation). As he continued to use these products, he presumably developed a more aggressive presentation of EVALI. Although other conditions can be considered with this presentation, given his classic history of THC containing e-cigarette, his clinical presentation, the oily nature of the bronchoalveolar fluid obtained, and his improvement after a month-long trial of systemic steroids and discontinuation of THC e-cigarette vaping makes the diagnosis of EVALI more likely. Of note, a recent case report in close-by University of Florida also demonstrated rapid resolution of vaping-induced acute pneumonia following steroid treatment [4]. Given the current COVID-19 pandemic, which presentation can overlap with the presentation of EVALI, it is necessary of clinicians to maintain a high index of suspicion and rule out the possibility of COVID-19. Pulmonary infiltrates such as ground-glass opacities, fever, and cough were often part the initial presentation of COVID-19 cases in China [5]. Lastly, clinicians should be aware of the commonality of disease manifestations between EVALI and COVID-19 as a patient could present with both conditions.
E-cigarettes are battery-operated devices that produces an aerosol when heating a liquid or wax containing different substances ranging from nicotine to cannabinoids with flavors and additives such as glycerol or propylene glycol [6]. They reached the US market in 2007 and from 2014, they have been the most commonly used tobacco product among U.S. youth [7]. It has since continued to grow and is now a multibillionaire industry. In 2018, more than 3.6 million U.S. youth, including 1 in 5 high school students and 1 in 20 middle school students, currently use e-cigarettes [8] and this trend keeps growing despite new regulations.
The pathogenesis of EVALI is still unknown. It is now considered to be a spectrum of illness rather than a single process. Appears that more than one pathogenic mechanism is involved, including acute eosinophilic pneumonia [9], diffuse alveolar hemorrhage [10], lipoid pneumonia [[11], [12], [13]], and respiratory-bronchiolitis interstitial lung disease.
The potential acute and long-term consequences of e-cigarettes use is not fully elucidated and while further research must be conducted, healthcare personnel must attain a sharp clinical judgment to suspect these entities and educate the public to avoid these devices.
4. Conclusion
This outpatient case presentation of EVALI prompts to raise suspicion of this condition by primary care providers, who should inquire about use of e-cigarettes, in particular THC-containing vaping products. EVALI has become a serious health issue and hundreds of thousands vapers are at risk to develop this spectrum of lung conditions. In the current COVID-19 pandemic, a high index of suspicion is needed by clinicians to rule out COVID-19 as a possible coexisting infection. This report hopes to raise awareness of this devastating but preventable condition and the need to further control and regulate this dangerous product that regrettably end in young hands.
Ethical statement
I testify on behalf of all co-authors that our article submitted to SSM-Population Health.
Declaration of competing interest
We have no conflicts of interest to disclose. All authors have approved this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2020.101154.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Navon L. Risk factors for E-cigarette, or vaping, product use-associated lung injury (EVALI) among adults who use E-cigarette, or vaping, products - Illinois, july-october 2019. MMWR Morb. Mortal. Wkly. Rep. 2019;68(45):1034–1039. doi: 10.15585/mmwr.mm6845e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Casanova G.S. An imported case of e-cigarette or vaping associated lung injury (EVALI) in Barcelona. Eur. Respir. J. 2020 Feb 6;55(2) doi: 10.1183/13993003.02076-2019. Print 2020 Feb. [DOI] [PubMed] [Google Scholar]
- 3.Kalininskiy A. E-cigarette, or vaping, product use associated lung injury (EVALI): case series and diagnostic approach. Lancet Respir. Med. 2019;7(12):1017–1026. doi: 10.1016/S2213-2600(19)30415-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alzghoul B.N. Rapid resolution of severe vaping induced acute lipoid pneumonia following corticosteroid treatment. Am. J. Respir. Crit. Care Med. 2020 Mar 6 doi: 10.1164/rccm.201909-1826IM. Ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Guan W.J. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gotts J.E. What are the respiratory effects of e-cigarettes? BMJ. 2019;366:l5275. doi: 10.1136/bmj.l5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.reportE-Cigarette Use Among Youthand Young Adults: A Report Ofthe Surgeon General.
- 8.Cullen K.A. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students - United States, 2011-2018. MMWR Morb. Mortal. Wkly. Rep. 2018;67(45):1276–1277. doi: 10.15585/mmwr.mm6745a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thota D., Latham E. Case report of electronic cigarettes possibly associated with eosinophilic pneumonitis in a previously healthy active-duty sailor. J. Emerg. Med. 2014;47(1):15–17. doi: 10.1016/j.jemermed.2013.09.034. [DOI] [PubMed] [Google Scholar]
- 10.Agustin M. Diffuse alveolar hemorrhage induced by vaping. Case Rep, Pulmonol. 2018;2018:9724530. doi: 10.1155/2018/9724530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Viswam D. Respiratory failure caused by lipoid pneumonia from vaping e-cigarettes. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2018-224350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCauley L., Markin C., Hosmer D. An unexpected consequence of electronic cigarette use. Chest. 2012;141(4):1110–1113. doi: 10.1378/chest.11-1334. [DOI] [PubMed] [Google Scholar]
- 13.Davidson K. Outbreak of electronic-cigarette-associated acute lipoid pneumonia - North Carolina, july-august 2019. MMWR Morb. Mortal. Wkly. Rep. 2019;68(36):784–786. doi: 10.15585/mmwr.mm6836e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.