To the Editor,
In the amidst of coronavirus disease 2019 (COVID-19) pandemic, a variety of extrapulmonary manifestations have been reported in literature. Cardiovascular manifestations can be early extrapulmonary COVID-19 manifestations, and can present as acute coronary syndrome, stress cardiomyopathy, myocardial injury, heart failure, arrhythmias, pericardial effusion, cardiac tamponade, thromboembolic complications, and cardiogenic shock [1].
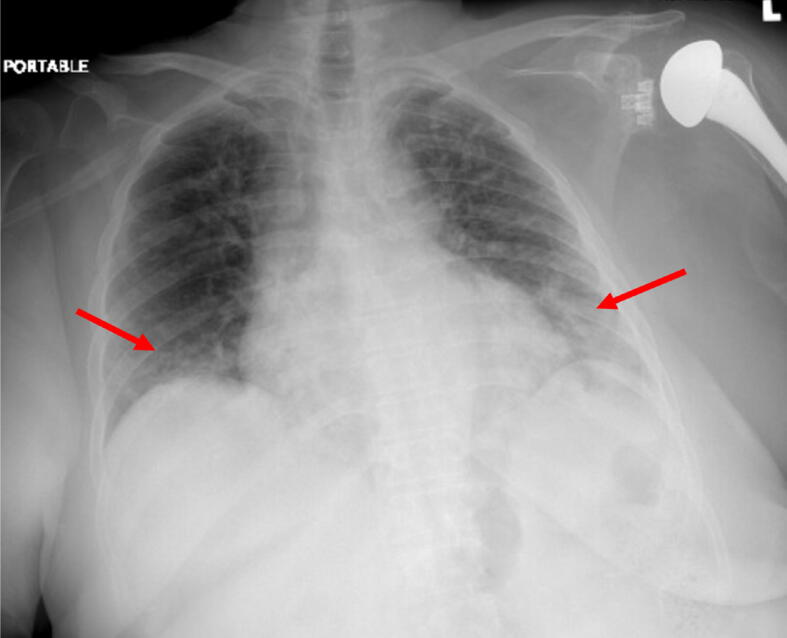
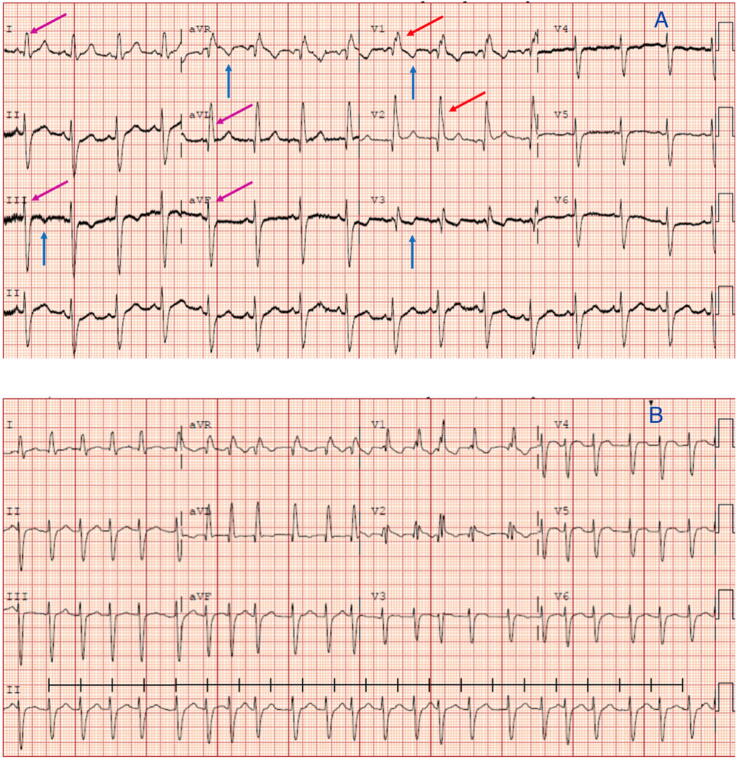
A 67-year-old woman presented to the emergency department (ED) with a complaint of fever, chills, cough, malaise, and myalgias for 2 weeks. She denied any diarrhea, constipation, sick contacts, recent travel, tobacco use, alcohol use, other illicit drug use, family history of cardiac disease, or prior cardiac disease. The patient’s past medical history included hypertension, and type 2 diabetes mellitus. Her medications included aspirin and a statin for CAD risk factor modifications and primary prevention. In ED her temperature was 98.5F°, blood pressure 133/64 mmHg, heart rate 114 beats per minute (BPM), respiratory rate 24 breaths/min, and blood oxygen saturation of 92% on ambient air. Physical examination revealed an anxious woman not in acute distress, and pulmonary exam was notable for bilateral coarse crackles most prominent in the lower lung fields. The differential diagnosis included community acquired pneumonia, COVID-19 pneumonia, acute coronary syndrome, Takotsubo cardiomyopathy, and myocarditis. Chest x-ray at presentation demonstrated bibasilar mixed ground glass opacities. (Fig. 1) Initial electrocardiogram (EKG) showed normal sinus rhythm (NSR) with heart rate (HR) of 93 bpm, normal intervals, right bundle branch block (RBBB), and T-wave inversions in the inferolateral leads (Fig. 2a). Pertinent laboratory results revealed leukocytosis of 18.87 K/uL, lymphopenia of 0.73 K/uL, elevated procalcitonin (PCT) of 82 ng/mL, high sensitivity C-reactive protein (hsCRP) of 222 mg/L, lactate dehydrogenase (LDH) of 442 U/L, ferritin of 591 ng/mL, D-dimer of 1,681 ng/mL, TSH 3.16 mIU/L, LDL 88.6 mg/dL, negative sputum and blood cultures. A nasopharyngeal swab for SARS CoV-2 reverse polymerase chain reaction (RT-PCR) returned positive. Three days following the initial presentation, the patient developed chest pain with EKG showing new-onset atrial fibrillation with a rapid ventricular response (RVR) and peak cardiac troponin T (cTnT) to 0.423 ng/mL (Fig. 2b). Transthoracic echocardiogram (TTE) demonstrated left ventricle ejection fraction (LVEF) of 30% with diffuse anterior wall and apical akinesia and apical ballooning. (Video 1) Initial therapy consisted of a five-day course of off-label hydroxychloroquine (400 mg QD) and azithromycin (400 mg QD), as well as supplemental oxygen via nasal cannula at 4L/minute for treatment of COVID-19 pneumonia with hypoxemia. The TTC was managed with dual antiplatelet treatment (DAPT) using aspirin and clopidogrel and high dose statin therapy. Atrial fibrillation was managed with amiodarone loading dose, and then 200 mg OD. Due to the increased risk of thromboembolism from TTC, COVID-19, and AF, patient was started on rivaroxaban 20 mg PO QD. Her clinical symptoms, and oxygen requirement improved on the abovementioned regimen, and patient was subsequently discharged with home isolation precautions.
Fig. 1.
Chest X-ray anteroposterior (AP) view showing mixed ground-glass opacities more prominent on bases (red arrows). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
A) Initial EKG showing normal sinus rhythm with a heart rate of 93 beats per minute. T-wave inversions (TWI) in V1, V3 (blue arrows), right bundle branch block (red arrows), with left anterior fascicular block (LAFB, magenta arrows). B) Atrial fibrillation (AF) with irregular rhythm at a rapid ventricular response (RVR) at 143 beats per minute (black line). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Stress cardiomyopathy/ Takotsubo cardiomyopathy (TTC) is a regional wall motion abnormality that can present as transient apical ballooning in the setting of emotional or physical stressors including infections [2], [3]. TTC is more prevalent in females with a mean age range of 62–76 years [2]. A diagnosis of TTC can be made if the patient meets all four Mayo clinic diagnostic criteria including 1) Transient regional left ventricular wall dysfunction; 2) ST elevation/T-wave inversions on EKG or elevated cTNT; 3) Absence of angiographic evidence of coronary obstruction; 4) Absence of myocarditis or pheochromocytoma [3]. TTC can present with or without complications such as heart failure, cardiogenic shock, left ventricular outflow tract obstruction, arrhythmias, and thromboembolism [3]. Arrhythmic complications of TTC, and COVID-19 can include atrial fibrillation, sinus node dysfunction, conductive tissue dysfunction, and ventricular tachyarrhythmias [1], [4]. AF can be the first presentation of TTC and can be present in up to 4.7% of cases [4]. COVID-19 may cause arrhythmias via downregulation of ACE-2 and subsequent increased angiotensin-II type-1 receptor (AT-1R) pathway activation. This increased AT-1R activation and associated cytokine storm induce oxidation of Ca2+/calmodulin dependent protein kinase II (CAMK-II). CAMK-II overly sensitizes cardiomyocytes to activating signals, which triggers inappropriate early cardiomyocyte depolarization leading to AF [5], [6].
Our patient presentation of apical wall motion abnormalities, troponemia, psychosocial and mechanical/inflammatory stress caused TTC with AF in the setting of confirmed COVID-19. TTC can often mimic ST-elevation myocardial infarction (STEMI), and coronary angiography should be performed to rule out coronary artery obstruction. However, normal coronary arteries do not preclude the diagnosis of TTC [2]. In our case, angiography for STEMI and cardiac medical resonance imaging for myocarditis were not performed as per our patient preference, to avoid the risk of procedural transmission of COVID, and to lower potentially unnecessary testing. AF can be treated by rhythm control, rate control or by ablation [7]. Our patient was treated with rhythm control, and mural thrombus was ruled out before the start of medications to prevent stroke. Furthermore, patients are at increased risk of stroke from COVID-19-induced hypercoagulability, TTC induced blood stasis, and AF, which can all potentiate thromboembolism [6], [7], [8]. Our patient was initially started on enoxaparin and later changed to rivaroxaban, a direct oral anticoagulant (DOAC), to manage her increased risk of thrombosis. The patient was treated with hydroxychloroquine and azithromycin as per our hospital protocol, as it is the standard of care of all COVID-19 patients in our hospital. For TTC and AF, we continued the patient on an optimal medical regimen with DAPT, statin, amiodarone, and anticoagulation. Patient reported no notable interval complaints on tele follow up visit. Takotsubo cardiomyopathy with atrial fibrillation can be an early presentation of COVID-19 as an extrapulmonary manifestation, and diagnosis should be kept in mind, and optimal medical treatment should be started.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2020.100580.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Video clip of transthoracic echocardiogram (TTE) demonstrated apical ballooning characteristics of Takotsubo cardiomyopathy using Definity™ contrast dye.
References
- 1.Hendren Nicholas S, Drazner Mark H, Bozkurt B, Cooper JLT. Description and Proposed Management of the Acute COVID-19 Cardiovascular Syndrome. Circulation. 0. [DOI] [PMC free article] [PubMed]
- 2.Scantlebury D.C., Prasad A. Diagnosis of Takotsubo cardiomyopathy. Circ J. 2014;78:2129–2139. doi: 10.1253/circj.cj-14-0859. [DOI] [PubMed] [Google Scholar]
- 3.Sattar Y., Siew K.S.W., Connerney M., Ullah W., Alraies M.C. Management of takotsubo syndrome: a comprehensive review. Cureus. 2020;12:e6556-e. doi: 10.7759/cureus.6556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Syed F.F., Asirvatham S.J., Francis J. Arrhythmia occurrence with takotsubo cardiomyopathy: a literature review. EP Europace. 2010;13:780–788. doi: 10.1093/europace/euq435. [DOI] [PubMed] [Google Scholar]
- 5.Purohit A., Rokita Adam G., Guan X., Chen B., Koval Olha M., Voigt N. Oxidized Ca2+/calmodulin-dependent protein kinase II triggers atrial fibrillation. Circulation. 2013;128:1748–1757. doi: 10.1161/CIRCULATIONAHA.113.003313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc. Res. 2020 doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lip G.Y.H., Al-Khatib S.M., Cosio F.G., Banerjee A., Savelieva I., Ruskin J. Contemporary management of atrial fibrillation: what can clinical registries tell us about stroke prevention and current therapeutic approaches? J. Am. Heart Assoc. 2014;3 doi: 10.1161/JAHA.114.001179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Gregorio C. Cardioembolic outcomes in stress-related cardiomyopathy complicated by ventricular thrombus: a systematic review of 26 clinical studies. Int. J. Cardiol. 2010;141:11–17. doi: 10.1016/j.ijcard.2009.09.468. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video clip of transthoracic echocardiogram (TTE) demonstrated apical ballooning characteristics of Takotsubo cardiomyopathy using Definity™ contrast dye.