Abstract
Acute esophageal necrosis, also known as black esophagus or acute necrotizing esophagitis is a rare condition with roughly 154 cases reported in the literature. This condition is classically diagnosed on its endoscopic findings of a circumferentially black esophagus that abruptly ends at the gastroesophageal junction and transitions to normal gastric mucosa. When present, acute esophageal necrosis potentially signifies a poor prognosis with an overall mortality up to 36%. This case report describes a critically ill patient with multiple comorbidities that was found to have acute esophageal necrosis the entire length of the esophagus secondary to ischemia/hypoperfusion that was caused by diabetic ketoacidosis. The patient had a prolonged hospitalization but was ultimately discharged in stable condition. We also review the literature of this rare esophageal condition.
Key words: Acute esophageal necrosis, black esophagus, acute necrotizing esophagitis, diabetic ketoacidosis, upper gastrointestinal bleed
Introduction
Acute esophageal necrosis (AEN), also known as black esophagus or acute necrotizing esophagitis is an extremely rare condition that frequently carries a poor prognosis. AEN was first described in the literature in the 1960s but did not gain more widespread recognition until the 1990s.1 As of 2019, roughly 154 cases of AEN have been reported.2 Due to the paucity of data on this condition, a medical therapy gold standard has not been established but treatment usually focuses on the causative condition.3,4 We present a case of a 56-year-old male presenting with diabetic ketoacidosis, shock, and coffee ground emesis that was found to have AEN. Considering the rarity of this condition, future clinical trials will likely not be possible. It is important that this case help expand the slowly growing literature of this condition to include the presentation, comorbidities, management, and outcome of our patient.
Case Report
56-year-old male with history of poorly controlled diabetes mellitus type 2, Gold stage IIID COPD, hypertension, chronic pain syndrome with long-term opiate use, and previous alcohol abuse (5 years sober) without cirrhosis presented with toxic/metabolic encephalopathy and acute hypoxic respiratory failure for which he was intubated prior to arrival. The patient had not been taking his medications, to include insulin, for several days. Vital signs demonstrated hypotension (86/45 mmHg), tachycardia (heart rate 116 beats per minute) and tachypnea (respirations 30 breaths per min). Oxygen saturation was 96% on room air. Physical exam demonstrated a cachectic appearing individual that responded to painful stimuli but would not follow commands, coarse lung sounds, and dry mucous membranes without peripheral edema, skin rashes, or induration. Laboratory results were consistent with diagnoses of diabetic ketoacidosis and acute kidney injury (creatinine 3.1 mg/dL) with an average of 38 mL/hr of urine output. Blood pressure did not initially respond to intravenous fluids and the patient was started on pressor support medications. While in the emergency department, the patient had an episode of coffee ground emesis. Hemoglobin was stable at 12.0 G/dL but INR was 1.9 due to vitamin K deficiency secondary to prolonged poor oral intake.
Once the patient was stabilized, an esophagogastroduodenoscopy (EGD) was performed which revealed diffuse circumferential blackish, necrotic-appearing mucosa of the entire length of esophagus and mild gastroduodenitis (Figure 1). Biopsies were taken of the esophagus, which did not induce bleeding. Pathology report described fragments of inflammatory and ulcer debris and fungal organisms consistent with Candida species, but no viable epithelium was present for evaluation. Immunohistochemical staining was negative for CMV and HSV (type I or II). These findings were consistent with the diagnosis of acute esophageal necrosis (AEN) caused by the presenting perfusion deficit and magnified by the patient’s multiple chronic illnesses. Patient was treated with fluconazole 200mg daily for two weeks and an extended course of pantoprazole 40mg twice daily. Approximately 16 hours after the EGD on day four of hospitalization, the patient was started on nasogastric tube feedings for nutrition as the patient suffered from oralpharyngeal dysphagia related to his acute illness. His swallowing slowly recovered and was able to resume a regular diet 3.5 weeks later. The patient had prolonged hospitalization due to difficulty weening from ventilator and required tracheostomy for a short period of time but eventually recovered to return home. It was recommended he return in 6 weeks for repeat EGD, but he was lost to follow-up.
Discussion
AEN, also known as black esophagus or acute necrotizing esophagitis, is a rare clinical entity and can carry a poor prognosis. Up to 36% of patients will succumb to their underlying critical illness; however, AEN specific mortality is approximately 6%.2,3,5 The typical patient is an elderly male (mean age 68; male to female ratio 4:1) that presents with signs and symptoms of upper gastrointestinal bleeding (65-90% of cases) but AEN can be an incidental finding during endoscopy.5-7 Though the exact etiology is unclear, it is likely multifactorial consisting largely of tissue hypoperfusion/mucosal ischemia, decreased mucosal buffering, and gastric content reflux that acutely exceeds the protective and regenerative properties of vulnerable esophageal mucosa enabling significant ischemic/chemical injury of the esophagus.3,5-7
In critical illness, chronic physiologic process changes that occur such as poor nutritional status and deconditioning likely potentiate esophageal injury in these patients. Additional risk factors include malignancy, cirrhosis, chronic pulmonary disease, renal failure, vascular or cardiac disease, diabetes mellitus, immunosupression or immunodeficiency, recent surgical procedure, and sepsis.5,6 Based on review of the literature, there appears to be a particularly strong association of AEN with diabetic ketoacidosis (DKA) in the setting of acute gastrointestinal bleeding.5,8
Our patient presented with diabetic ketoacidosis, shock, severe COPD, renal failure, poor nutritional status, and deconditioning placing him at high risk for ischemic injury. Our patient was also colonized with Candida species, which is commonly associated with AEN. Additional common pathogens include cytomegalovirus, herpes simplex virus, Klebsiella species, and Penicillium chrysogenum. 4,5
The most significant contributing factor identified in previous studies was hypotension. 6 The esophagus has a diverse blood supply. The distal esophagus has the least vascularized segment deriving its blood supply from the branches of the left gastric artery making it more sensitive to flucuations in tissue perfusion.7 As a result, AEN demonstrates a penchant for and tends to be more severe in the distal esophagus.6 Panesophageal disease may present in up to 36% of cases but is rarely isolated to the proximal esophagus (2% of cases).2
Diagnosis is based on endoscopic findings which consist of a circumferentially black esophagus that abruptly ends at the gastroesophageal junction and transitions to normal gastric mucosa in the absence of caustic ingestion.1,4-6 Differential diagnosis should include other causes of black colored esophagus, such as malignant melanoma, acanthosis nigricans, esophageal melanocytosis, and pseudomelanosis. 3,5,6
Histological findings include necrosis of the mucosa with severe inflammatory changes that may extend into the submucosa and muscularis propria in the absence of viable epithelium; vascular thrombi or heavy leukocytic infiltrate may also be visible. 5-7,9 Histological examination is not required for diagnosis but may be useful to evaluate for associated pathogens or to rule out other differential diagnoses.5,7 For example, negative staining on Perl’s Prussian blue likely excludes iron pill injury while negative staining on Fontana-Masson likely exludes esophageal melanocytosis.3
In contrast to caustic esophagitis, which portends a surgical intevention, AEN is typicaly treated medically though it should be noted that there are no established guidelines on management due to the rarity of this condition.3,4 Considering the potential poor prognosis, treatment should be directed toward the critical illness. Intravenous fluid resuscitation, anemia correction, gastric acid suppression, sucralfate, and bowel rest play an important role in treatment.3,5,6 Temporary parenteral nutrition may be required. It is our view that that nasogastric tube placement be absolutely avoided in any patient where AEN is diagnosed or suspected. One of the most critical complications of AEN is esophageal perforation which requires emergent surgical intervention and rapid initation of antibiotics.3,5 Perforation should be considered in any rapidly decompensating patient.
A potential long-term complication is stenosis/stricture of the esophagus, which may occur in 10-25% of patients.3,5 This complication is typically amendable to the traditional treatments of acid suppression and endoscopic balloon dilation.
This case helps contribute to the small but growing literature of this rare condition. A clinician must consider AEN when faced with an elderly, possibly poorly controlled diabetic patient presenting with acute upper gastrointestinal bleeding and hypotension/shock, particularly in the setting of chronic illness or when additional significant comorbid conditions are present.4-6,8 Despite its rarity, prompt diagnosis is imperative as AEN portends a significant increase in overall mortality.
Figure 1.
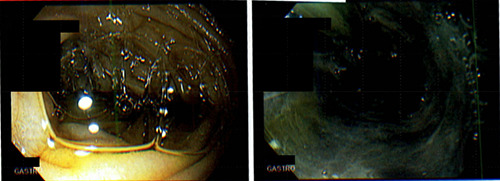
Esophagogastroduodenoscopy demonstrating circumferentially black pigmentation of the middle (left image) and lower (right image) third of the esophagus.
References
- 1.Shah A, Thoguluva Chandreskar V, Doobay R, et al. Acute esophageal necrosis in an alcoholic after successful resuscitation from cardiac arrest. Case Rep Gastrointest Med 2017;2017: 5092906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abdullah HM, Ullah W, Abdallah M, et al. Clinical presentations, management, and outcomes of acute esophageal necrosis: a systemic review. Expert Rev Gastroenterol Hepatol 2019;13:507-14. [DOI] [PubMed] [Google Scholar]
- 3.Kalva NR, Tokala MR, Dhillon S, et al. An unusual cause of acute upper gastrointestinal bleeding: acute esophageal necrosis. Case Rep Gastrointest Med 2016;2016:6584363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lahbabi M, Ibrahimi A, Aqodad N. Acute esophageal necrosis: a case report and review. Pan Afr Med J 2013; 14:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol 2010;16:3219-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zacharia GS, Sandesh K, Ramachandran T. Acute esophageal necrosis: an uncommon cause of hematemesis. Oman Med J 2014;29: 302-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maubert A, Frey S, Rahili A, et al. Acute esophageal necrosis: Case report of an unknown entity. Int J Surg Case Rep 2019;61:188-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inayat F, Hurairah A, Virk HU. Acute esophageal necrosis: an update. N Am J Med Sci 2016;8:320-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butler DC, Batalis NI. Acute esophageal necrosis. Acad Forensic Pathol 2017;7:312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


