Abstract
Objective
To explore if the modified cervical and shoulder retraction exercise program restores cervical lordosis and reduces neck pain in patients with loss of cervical lordosis.
Methods
This study was a retrospective analysis of prospectively collected data. Eighty-three patients with loss of cervical lordosis were eligible. The eligible patients were trained to perform the modified cervical and shoulder retraction exercise program by a physiatrist, and were scheduled for a follow-up 6 to 8 weeks later to check the post-exercise pain intensity and lateral radiograph of the cervical spine in a comfortable position. The parameters of cervical alignment (4-line Cobb’s angle, posterior tangent method, and sagittal vertical axis) were measured from the lateral radiograph.
Results
Forty-seven patients were included. The mean age was 48.29±14.47 years. Cervical alignment and neck pain significantly improved after undergoing the modified cervical and shoulder retraction exercise program (p≤0.001). The upper cervical lordotic angle also significantly improved (p=0.001). In a subgroup analysis, which involved dividing the patients into two age groups (<50 years and ≥50 years), the change of the sagittal vertical axis was significantly greater in the <50 years group (p=0.021).
Conclusion
The modified cervical and shoulder retraction exercise program tends to improve cervical lordosis and neck pain in patients with loss of cervical lordosis.
Keywords: Spine, Lordosis, Neck pain, Exercise, Education
INTRODUCTION
Cervical lordosis is a physiological curvature of the cervical spine. The loss of cervical lordosis is associated with various musculoskeletal health problems, including neck pain, headaches, temporomandibular joint dysfunction, and reduced quality of life [1-3]. In healthy spines, the axial load along the cervical spine is supported along the ventral column of the spine. However, in spines with the loss of lordosis, the load moves more anteriorly, and the torque on the cervical spine becomes larger [4]. According to a study of Hansraj [5] in 2014, when the neck is bent at 15°, 30°, 45°, and 60°, the cervical spine receives approximately 3, 4, 5, and 6 times more weight, respectively than at lordosis. This increased torque stresses the surrounding bony structure. Disc damage and severe problems like cervical radiculopathy and myelopathy may result [6,7]. Without the restoration of the lordotic posture, further axial load could induce the progression of the kyphotic posture [4]. Therefore, the loss of cervical lordosis with neck pain should receive greater attention.
Loss of cervical lordosis can be caused by several conditions: neuromuscular disease, congenital deformity, infection, tumor, trauma, rheumatic disease, and other various post-surgical conditions [1,8]. Although the mechanism of loss of cervical lordosis remains unclear [8], some factors are known to induce it. The most important factor may be the postural habit, such as a forward head posture. The prolonged adoption of a forward head posture can cause neck muscle imbalance [9]. As this imbalance persists, the cervical spine can lose lordosis.
Numerous exercises have been studied and used to treat these problems. Pearson and Walmsley [10] found that 3 sets of 10 repeated neck retractions resulted in a significant change in resting neck posture. Harman et al. [9] suggested that a home-based targeted exercise program, including deep cervical flexor and shoulder retractor strengthening, along with cervical extensor and pectoral muscle stretching can improve postural alignment. In a recent randomized controlled study, Alpayci and Ilter [1] found that isometric neck extension exercise improves cervical lordosis and pain.
However, while the exercises mentioned above can restore cervical lordosis, they also risk damaging the disc. Neck retraction helps recover the lordotic curve in the lower cervical portion, but kyphotic changes may occur at the upper cervical level [10,11]. When a strong force acts on the neck muscles, it can be delivered directly to the disc. Therefore, neck muscle strengthening has to be done carefully.
A modified cervical and shoulder retraction exercise program that can improve cervical lordosis while preventing disc damage was developed. The present study aims to explore whether the modified cervical and shoulder retraction exercise program restores cervical lordosis and reduces neck pain in patients with loss of cervical lordosis.
MATERIALS AND METHODS
This study was a retrospective analysis of prospectively collected datafrom April 2016 to July 2017. Eight-three patients with complaints of neck pain and cervical kyphosis in the lateral radiograph of the cervical spine were registered as part of the cervical kyphosis list and enrolled in the present study. The enrolled patients were trained to perform the modified cervical and shoulder retraction exercise program by a physiatrist. They were scheduled for a follow-up 6 to 8 weeks later to review the post-exercise pain intensity and lateral radiograph of the cervical spine in a usual, comfortable position. After obtaining approval from the local Institutional Review Board of Seoul National University Bundang Hospital, the chart and radiographic data were reviewed retrospectively (No. B-1708/412-103).
The inclusion criteria were as follows: (1) patients who had cervical pain, (2) patients who received a cervical spine radiograph and were diagnosed with the loss of cervical lordosis from a cervical spine radiograph, (3) patients who received education on the modified cervical and shoulder retraction exercise program, (4) patients who agreed to attend a follow-up 6 to 8 weeks later, (5) patients who attended a follow-up within 12 months, and (6) patients who were more than 18 years old at the start of the exercise regimen.
The exclusion criteria were as follows: (1) patients who refused to attend a follow-up 6 to 8 weeks later, (2) patients who did not undergo lateral radiography of the cervical spine, and (3) patients who had radiculopathy, myelopathy, structural disorders of the cervical spine, history of cervical trauma or surgery, or inflammatory rheumatic diseases.
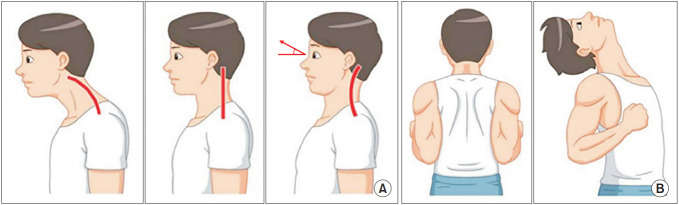
The modified cervical and shoulder retraction exercise program involved two steps. First, patients either sat or stood in an upright position while pushing their chin backward and simultaneously raising their head within the pain-free range (3 seconds) (Fig. 1A). The retraction used in a study of Pearson and Walmsley [10], which was developed by Mckenzie, involves pulling the head and neck back while the head remains level. However, since it can cause upper cervical flexion, we modified the movement to include the raising of the head. Second, in a seated or standing position, patients maintained an upright posture and tried to pull back their shoulders and extend their neck within the pain-free range (10 seconds) (Fig. 1B). Patients were instructed to perform each exercise step at least 10 times a day.
Fig. 1.
The modified cervical and shoulder retraction exercise. Two steps: raise head up and push the chin backward simultaneously within the pain free range (A), and keep upright and try to pull back the shoulder and head within the pain free range (B).
Information, such as sex, age, and severity of neck pain, was recorded. The severity of neck pain was recorded on a numerical rating scale (NRS, score 0–10). The lateral view of the cervical spinal radiograph from before the exercise was compared with that from after the exercise.
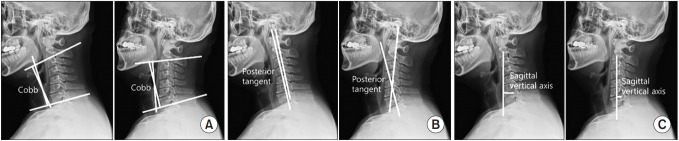
The whole and segmental cervical lordotic angle and head position in the sagittal plane were measured using a radiographic evaluation. To investigate the cervical lordotic angle, the 4-line Cobb’s angle (Fig. 2A) and posterior tangent method between C2 and C7 (Fig. 2B) were measured. Using these methods, the lordotic angles were considered as negative numbers, whereas the kyphotic angles were considered as positive numbers. The 4-line Cobb’s angle and posterior tangent method have been known to have good intra-observer and inter-observer reliabilities [12]. To check the occurrence of segmental kyphosis in the upper cervical level (C2–C4), the 4-line Cobb’s angle and posterior tangent method between C2 and C4 were measured. To investigate the position of the head in the sagittal plane, the sagittal vertical axis (SVA)— distance between the posterior superior corner of C7 and a plumb line dropped from C2 (Fig. 2C)—were measured. The SVA is widely used to evaluate the sagittal alignment of the spine, which is known to be correlated with myelopathy severity [13].
Fig. 2.
Radiologic parameters: the 4-line Cobb’s angle (A), posterior tangent method (B), and sagittal vertical axis (C).
Additionally, a subgroup analysis was performed to compare the improvement according to age. The patients were divided into two age groups (<50 years and ≥50 years). The degree of improvement in cervical lordosis between the two groups was compared.
Statistical analysis
Statistical Package for Social Sciences for Windows version 18.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. The normality of the data was checked with the Kolmogorov–Smirnov test. All results of the variables for the cervical lordotic angle, position of the head, and pain severity were analyzed using the paired t-test and independent t-test. Values are presented as a mean±standard deviation. Statistical significance was to at a p-value of <0.05.
RESULTS
A total of 83 patients were screened. Among them, 32 patients were excluded due to loss to follow-up. Four patients were excluded due to radiculopathy (n=1) and lack of radiograph (n=3). The remaining 47 patients were included in the final analysis.
Demographic data are presented in Table 1. The mean age of the patients who were included was 48.29±14.47 years (range, 19–73 years); 21 patients were male and 26 were female. All results of the variables for the cervical lordotic angle, position of the head, and pain severity were normally distributed.
Table 1.
Demographic data
| Variable | Male (n=21) | Female (n=26) | Total (n=47) |
|---|---|---|---|
| Age (yr) | 46.90±14.74 | 48.57±15.73 | 48.29±14.47 |
| Follow-up length (day) | 114.90±92.78 | 117.95±73.90 | 126.38±88.90 |
| Four-line Cobb’s angle (º) | -2.10±9.31 | 0.73±10.66 | -0.53±10.07 |
| Posterior tangent method (º) | -7.68±9.43 | -2.87±8.44 | -5.02±9.12 |
| SVA (mm) | 21.58±15.14 | 17.12±6.62 | 19.11±11.33 |
| Pain (NRS, 0–10) | 6.03±2.36 | 6.00±1.85 | 6.04±1.93 |
Values are presented as mean±standard deviation.
SVA, sagittal vertical axis; NRS, numerical rating scale.
There were no significant differences in age, follow-up length, 4-line Cobb’s angle, posterior tangent method, SVA, and pain between male and female groups.
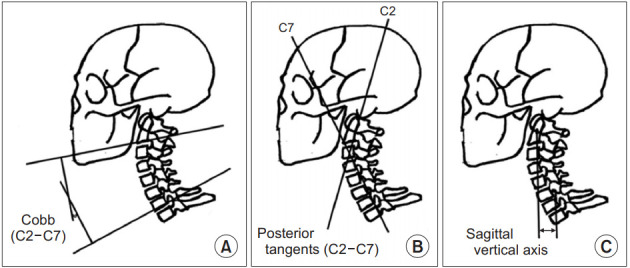
The degree of pain severity was significantly decreased, from 6.04±1.93 before the exercise regimen to 3.06±2.06 after (p<0.001). Table 2 displays the radiological changes in the variables between C2 and C7 from before and after the exercise regimen. Compared to before, the cervical lordosis angle, as measured by the 4-line Cobb’s angle, significantly improved after the exercise regimen (p=0.001). The cervical lordosis angle, as measured by the posterior tangent method, also significantly improved (p<0.001). Changes of the cervical lordosis angle were -3.60°±6.83° based on the 4-line Cobb’s angle and -3.88°±6.94° based on the posterior tangent method. The position of the head in the sagittal plane, as measured by SVA, also significantly improved after the exercise regimen (p=0.001). The change of SVA was -3.52±6.71 mm. Fig. 3 displays the improvement of cervical lordosis in patients after the modified cervical and shoulder retraction exercise program.
Table 2.
The change of radiologic parameters (between C2 and C7) and pain score after exercise
| Before exercise | After exercise | Change | p-value | |
|---|---|---|---|---|
| Four-line Cobb’s angle (º) | -0.53±10.07 | -4.14±11.09 | -3.60±6.83 | 0.001 |
| Posterior tangent method (º) | -5.02±9.12 | -8.90±10.83 | -3.88±6.94 | <0.001 |
| SVA (mm) | 19.11±11.33 | 15.59±13.76 | -3.52±6.71 | 0.001 |
| Pain (NRS, 0–10) | 6.04±1.93 | 3.06±2.06 | -2.99±1.99 | <0.001 |
Values are presented as mean±standard deviation.
SVA, sagittal vertical axis; NRS, numerical rating scale.
Fig. 3.
Improvement of cervical lordosis in the patients after the exercise: the 4-line Cobb’s angle (A), posterior tangent method (B), and sagittal vertical axis (C).
Table 3 displays the changesin the radiological parameters between C2 and C4 from before and after the exercise regimen. Based on the posterior tangent method, the cervical lordosis angle between C2 and C4 was significantly improved (p=0.001). There was an improvement of cervical lordosis at the upper cervical level after the exercise regimen.
Table 3.
The change of radiologic parameters (between C2 and C4) after exercise
| Before exercise | After exercise | Change | p-value | |
|---|---|---|---|---|
| Four-line Cobb’s angle (º) | 3.42±6.46 | 2.60±7.34 | -0.82±3.60 | 0.125 |
| Posterior tangent method (º) | -0.42±6.50 | -2.05±6.76 | -1.62±3.12 | 0.001 |
Values are presented as mean±standard deviation.
The comparisons of the improvement between the two age groups, <50 years and ≥50 years, are shown in Table 4. Based on the 4-line Cobb’s angle and posterior tangent method, there was no significant difference between the two age groups. However, the change of SVA was significantly greater in the <50 years group than in the ≥50 years group (p=0.021).
Table 4.
Comparison of degree of change of cervical alignment between <50 and ≥50 years
| Aged <50 yr (n=25) | Aged ≥50 yr (n=22) | p-valuea) | ||
|---|---|---|---|---|
| Four-line Cobb’s angle (º) | Before exercise | 0.49±8.42 | -1.70±11.78 | 0.463 |
| After exercise | -4.18±11.14 | -4.09±11.29 | 0.977 | |
| p-valueb) | 0.002 | 0.109 | ||
| Change | -4.67±6.91 | -2.39±6.70 | 0.258 | |
| Posterior tangent method (º) | Before exercise | -4.86±9.01 | -5.21±9.46 | 0.900 |
| After exercise | -9.26±11.32 | -8.50±10.49 | 0.815 | |
| p-valueb) | 0.005 | 0.034 | ||
| Change | -4.39±7.15 | -3.30±6.81 | 0.595 | |
| SVA (mm) | Before exercise | 16.78±10.41 | 21.77±11.99 | 0.134 |
| After exercise | 11.17±11.57 | 20.62±14.56 | 0.017 | |
| p-valueb) | <0.001 | 0.357 | ||
| Change | -5.62±6.96 | -1.14±5.68 | 0.021 |
Values are presented as mean±standard deviation.
SVA, sagittal vertical axis.
Intergroup comparison,
before and after exercise intragroup comparison.
DISCUSSION
In the present study, patients with a loss of cervical lordosis and neck pain underwent the modified cervical and shoulder retraction exercise program. This program had significant positive effects on cervical sagittal alignment and neck pain severity. Moreover, there was an improvement of cervical lordosis at the upper cervical level after the exercise regimen.
Given that lordosis is the normal physiological state of the cervical regions of the spine, the loss of cervical lordosis implies a disease state and can result in various musculoskeletal health problems. When cervical lordosis is lost, vertical loads are redistributed along the anterior part of the cervical spine, overloading the surrounding soft tissue and bones. The vertical loads are known to be at least 10 times heavier at the apex of kyphosis than lordosis. This overloading worsens the degenerative changes of the cervical spine, like osteophytes and posterior disc herniation [4,7]. Therefore, the recovery of lordosis is important for musculoskeletal health.
Numerous methods of exercise have been studied to restore proper posture. However, there can be side effects of any exercise, even if it improves posture or curvature. Pearson and Walmsley [10] in 1995, showed that repeated neck retractions resulted in a significant change in resting neck posture. However, after neck retractions, upper cervical flexion can occur [10,11]. Therefore, neck retraction requires modification.
Postural habits may be a major cause of loss of lordosis. According to a study of Hansraj [5], the weight on the spine increases when flexing the head forward. Therefore, positioning the head forward in daily life, such as driving, watching TV or computer, and reading a book, may stress the cervical spine and cause lordosis. Notably, a forward head posture is becoming more common because smartphone use has increased dramatically in recent years. Park et al. [14] showed that heavy smartphone use could produce stresses on the cervical spine, thus changing the cervical curvature and resulting in neck pain.
In addition, even though Alpayci and Ilter [1] showed that isometric neck extension exercise could strengthen the neck extensor and restore cervical lordosis, it may also accelerate disc degeneration, especially when performed in a flexed posture. The disc can be damaged when it is subjected to a strong force at once or with sustained pressure [15]. The force that presses on the disc is the sum of the weight of the head and the contractile force on the neck muscles, which act to put the head in place. Since the weight of the head is constant, the tension on the neck muscles may be the main factor responsible for disc degeneration. Accordingly, although there was an improvement of cervical lordosis and neck pain in patients after 3 months of exercising in a study of Alpayci and Ilter [1], long-term follow-up studies are required to evaluate its impact on disc degeneration or herniation.
Considering the above problems, an exercise program for patients with loss of lordosis and neck pain was developed. We modified the neck retraction. While pushing the head and neck backward, instead of keeping the head level, we modified the exercise to include the head going up so as to prevent upper cervical flexion. As neck muscle strengthening may damage the disc, we did not include neck muscle strengthening exercises in the program. However, the second exercise involved strengthening the shoulder retraction muscle. In general, rounded shoulders are observed in people with a forward head posture [9]. As rounded shoulders are accompanied by thoracic hyperkyphosis, this should also be of interest. Protracted shoulders are associated with tightness of the pectoralis minor and weakness of the mid-thoracic scapular retractors [9,16]. Therefore, our exercise program included an exercise in which the patient would pull back their shoulders and head. This was done to strengthen the shoulder retractors and stretch the pectoralis minor.
Although the present study has a shorter duration of exercise, less quantified amount of exercise and less intense intensity of exercise than those of Alpayci and Ilter [1], and the results were similar to those of Alpayci and Ilter [1] tried to improve lordosis by strengthening the neck extensor. However, correction of thoracic hyperkyphosis is also important, because it is known that the worse thoracic kyphosis is, the less cervical lordosis of lower segments [16]. In the present study, a retraction exercise of the shoulder and back was done to correct forward head posture and thoracic hyperkyphosis. This would have made a difference.
In the present study, the change of the cervical lordotic angle between C2 and C4 were checked. Our results showed an improvement of cervical lordosis at the upper cervical level after the exercise. This suggests that the modified cervical and shoulder retraction exercise can not only prevent upper cervical kyphosis but can also improve the entire cervical lordosis.
We also compared the effect of the modified cervical and shoulder retraction exercise regimen based on age. It is known that disc degeneration becomes worse with age [17]. Given that the location and height of the disc are important factors for the maintenance of cervical lordosis, we thought that the ability to recover lordosis would decrease with the progression of disc degeneration. In this study, the improvement of cervical alignment was greater in younger patients (<50 years) than in older patients (≥50 years). This result suggests that cervical lordotic curvature should be maintained before disc damage since exercise is less effective after disc degeneration.
This study has some limitations regarding its study design and content. First, given the retrospective nature of our study, 32 of the 83 patients were lost to follow-up. There can be selection bias. Second, there was no control group, and therefore the efficacy of the exercise program, in particular, cannot be ascertained. Future studies should include a control group. Third, another limitation was the variable follow-up period. We planned to conduct a follow-up after 6 to 8 weeks. However, the follow-up time ranged from 1 to 12 months. Future studies should have a more definitive follow-up range with less variability. Fourth, we were unable to measure the precise amount of exercise undertaken. Fifth, in the present study, we did not use the formetric method. The formetric method is more objective than radiographic measurements. However, because the study is a retrospective study of patients who had visited a clinic, we could not apply the formetric method. The only objective data was the radiograph when we retrospectively reviewed the data. It will be more appropriate to use formetric methods if a prospective study is conducted in the future. Sixth, in the present study, there were no serious side effects in the reviewed medical records. Although there were no serious side effects, it is necessary to check the side effects in future studies as a detailed history may not have been recorded. Finally, the compliance of the patients to the exercise program could not be checked. As the exercises are easy and straightforward, we predict that the compliance would have been reasonable. However, in future studies, compliance with the exercise program should be checked. For these reasons, a randomized controlled study is required in the future to confirm the findings of this study.
Acknowledgments
The authors would like to thank the Medical Research Collaborating Center at Seoul National University Bundang Hospital for their help regarding the statistical analyses. This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No. NRF-2016R1D1A1B03935130).
Footnotes
No potential conflict of interest relevant to this article was reported.
Conceptualization: Ohn SH. Methodology: Cha E, Song J, Jung IH, Lee HY, Jung KI, Yoo WK. Formal analysis: Baek S. Conceptualization: Ryu JS, Lee MY. Methodology: Ryu JS, Lee MY. Formal analysis: Lee MY. Funding acquisition: Ryu JS. Project administration: Park Y, Lee MY, Ryu JS. Visualization: Lee MY, Jeon H. Writing – original draft: Ryu JS, Lee MY, Jeon H. Writing – review, and editing: Ryu JS, Lee MY, Choi JS. Approval of the final manuscript: all authors.
REFERENCES
- 1.Alpayci M, Ilter S. Isometric exercise for the cervical extensors can help restore physiological lordosis and reduce neck pain: a randomized controlled trial. Am J Phys Med Rehabil. 2017;96:621–6. doi: 10.1097/PHM.0000000000000698. [DOI] [PubMed] [Google Scholar]
- 2.Been E, Shefi S, Soudack M. Cervical lordosis: the effect of age and gender. Spine J. 2017;17:880–8. doi: 10.1016/j.spinee.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 3.McAviney J, Schulz D, Bock R, Harrison DE, Holland B. Determining the relationship between cervical lordosis and neck complaints. J Manipulative Physiol Ther. 2005;28:187–93. doi: 10.1016/j.jmpt.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Ferrara LA. The biomechanics of cervical spondylosis. Adv Orthop. 2012;2012:493605. doi: 10.1155/2012/493605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014;25:277–9. [PubMed] [Google Scholar]
- 6.Iwasaki M, Yamamoto T, Miyauchi A, Amano K, Yonenobu K. Cervical kyphosis: predictive factors for progression of kyphosis and myelopathy. Spine (Phila Pa 1976) 2002;27:1419–25. doi: 10.1097/00007632-200207010-00009. [DOI] [PubMed] [Google Scholar]
- 7.Okada E, Matsumoto M, Ichihara D, Chiba K, Toyama Y, Fujiwara H, et al. Does the sagittal alignment of the cervical spine have an impact on disk degeneration? Minimum 10-year follow-up of asymptomatic volunteers. Eur Spine J. 2009;18:1644–51. doi: 10.1007/s00586-009-1095-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alpayci M, Senkoy E, Delen V, Sah V, Yazmalar L, Erden M, et al. Decreased neck muscle strength in patients with the loss of cervical lordosis. Clin Biomech (Bristol, Avon) 2016;33:98–102. doi: 10.1016/j.clinbiomech.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve forward head posture in normal adults: a randomized, controlled 10-week trial. J Man Manip Ther. 2005;13:163–76. [Google Scholar]
- 10.Pearson ND, Walmsley RP. Trial into the effects of repeated neck retractions in normal subjects. Spine (Phila Pa 1976) 1995;20:1245–51. doi: 10.1097/00007632-199506000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Ordway NR, Seymour RJ, Donelson RG, Hojnowski LS, Edwards WT. Cervical flexion, extension, protrusion, and retraction: a radiographic segmental analysis. Spine (Phila Pa 1976) 1999;24:240–7. doi: 10.1097/00007632-199902010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Ohara A, Miyamoto K, Naganawa T, Matsumoto K, Shimizu K. Reliabilities of and correlations among five standard methods of assessing the sagittal alignment of the cervical spine. Spine (Phila Pa 1976) 2006;31:2585–92. doi: 10.1097/01.brs.0000240656.79060.18. [DOI] [PubMed] [Google Scholar]
- 13.Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38(22 Suppl 1):S149–60. doi: 10.1097/BRS.0b013e3182a7f449. [DOI] [PubMed] [Google Scholar]
- 14.Park J, Kim J, Kim J, Kim K, Kim N, Choi I, et al. The effects of heavy smartphone use on the cervical angle, pain threshold of neck muscles and depression. Adv Sci Technol Lett. 2015;91:12–7. [Google Scholar]
- 15.Wilder DG, Pope MH, Frymoyer JW. The biomechanics of lumbar disc herniation and the effect of overload and instability. J Spinal Disord. 1988;1:16–32. [PubMed] [Google Scholar]
- 16.Ruivo RM, Pezarat-Correia P, Carita AI. Effects of a resistance and stretching training program on forward head and protracted shoulder posture in adolescents. J Manipulative Physiol Ther. 2017;40:1–10. doi: 10.1016/j.jmpt.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 17.Buckwalter JA. Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976) 1995;20:1307–14. doi: 10.1097/00007632-199506000-00022. [DOI] [PubMed] [Google Scholar]