Abstract
Opioid use disorder (OUD) and opioid overdose deaths (OODs) are prevalent among US workers, but work-related factors have not received adequate attention as either risk factors or opportunities for OOD prevention. Higher prevalence of OOD in those with heavy physical jobs, more precarious work, and limited health care benefits suggest work environment and organizational factors may predispose workers to the development of OUD.
Organizational policies that reduce ergonomic risk factors, respond effectively to employee health and safety concerns, provide access to nonpharmacologic pain management, and encourage early substance use treatment are important opportunities to improve outcomes. Organizational barriers can limit disclosure of pain and help-seeking behavior, and opioid education is not effectively integrated with workplace safety training and health promotion programs.
Policy development at the employer, government, and association levels could improve the workplace response to workers with OUD and reduce occupational risks that may be contributing factors.
Opioid use disorder (OUD) is an overwhelming public health problem in the United States. Drug overdose is now the leading cause of accidental death in the United States, with two thirds of all drug overdose deaths involving an opioid.1 Many of these deaths result from use of prescription painkillers, and synthetic opioids (e.g., fentanyl, tramadol) have outpaced commonly prescribed opioids as the leading cause of opioid overdose deaths (OODs) since 2015.2 The dramatic increase in both prescription and illicit opioid use since 20003,4 is attributed, in part, to a marked liberalization of opioid prescribing practices for the treatment of acute and chronic pain.5,6 Opioid prescribing rates have shown a gradual decline since 2010,7,8 but opioid fatality rates have increased to 47 600 lives lost in 2017.1 Also, some policy changes designed to reduce opioid prescribing (e.g., prescription drug monitoring programs) may have contributed to individuals transitioning to use of illicitly manufactured opioids such as heroin and fentanyl.8 Alternative policy perspectives beyond prescribing limits should be explored.
Much of the public health response to the opioid crisis has been in the health care system. Besides policy changes to prevent multiple prescribers, the Centers for Disease Control and Prevention (CDC)9 and medical societies10 have revised medical guidelines for prescribing opioids for pain management, and more federal funds have been allocated to improve availability of OUD treatment.11 The complexity of this problem involving substance use behaviors, pain management, physician and insurer practices, community services, and other factors suggests a need for a comprehensive analysis of root causes to reduce OUD prevalence and OOD rates. One upstream cause rarely highlighted is the origin of pain symptoms for which individuals seek treatment and the extent to which these factors can be prevented or mitigated.
Relieving physical pain is the primary reason given (63.4%) for a recent episode of prescription pain reliever misuse among individuals aged 18 years or older.12 Forty percent of US workers report chronic or recurrent musculoskeletal pain,13,14 15% of workers report pain most days or every day,15 and work-related exacerbations of back pain account for $5.3 billion per year in lost work productivity.13 Work-related factors may also influence access to opioids as well as OUD treatments, as many US workers depend on employer-sponsored health insurance or workers’ compensation insurance.16 Attending to conditions of work may have significant potential for effective public health action to combat the opioid crisis.
The magnitude and specific causes of OUD in employed individuals have been difficult to pinpoint, in part because of difficulties in assessing substance use or addiction among working people and in part because of a common assumption that individuals struggling with substance use are not in the workforce. However, the workplace is an important public health venue and, to date, employers have not been adequately included in state and local efforts to combat the opioid crisis. We believe that this is a critical gap in prevention efforts. In this article, we seek to highlight the ways in which working conditions and work organization may contribute to initiation of pain medication and to chronic pain syndromes and the opioid use that may follow. We conclude with recommendations for public health researchers, practitioners, and employer organizations to incorporate workplace factors in prevention efforts.
WORKING CONDITIONS AND OPIOID USE
There are logical interrelationships between occupational risk factors and prescription drug use.17 In the case of chronic opioid use (using opioids most days > 3 months),9 there are at least 2 plausible causal pathways. One of these begins with physical injury at work or cumulative trauma from strenuous labor leading to pain and use of painkillers, either as prescribed treatment or for self-medication. The other has its origins in psychological stress from unmanageable job demands (including time pressure) or from economic insecurity and job instability, leading to depression and anxiety. These 2 pathways represent different mechanisms, but they also overlap somewhat, and there may be individuals who experience both in parallel or sequence, as discussed in the next paragraphs.
Work-Related Pain and Discomfort Pathway
Musculoskeletal injuries, whether resulting from chronic exposures to ergonomic risk factors or from acute incidents such as slips, trips, and falls or violent assault, are the leading cause of work-related injury and disability.18 Heavy physical work, high psychosocial work demands, excessive repetition of tasks, awkward postures, and heavy lifting are known workplace risk factors for musculoskeletal pain in prospective studies.19,20 Occupations such as construction, commercial fishing, and health care–support jobs such as nursing aides are physically demanding. They feature high rates of occupational injuries, as well as high prevalence of back and other musculoskeletal pain.
Opioid overdose rates are highest among occupations with the greatest physical work demands and least access to paid sick leave.21–24 One study found that 57% of opioid-related overdose deaths occurred after a work injury, with 13% of overdose deaths preceded by a work injury within the past 3 years of death.25 A CDC analysis of 47 810 drug overdose deaths recorded in the National Occupational Mortality Surveillance system from 2007 to 201226 showed elevated proportional mortality ratios for 6 occupational groupings: construction, extraction (e.g., mining and petroleum drilling), food preparation and serving, health care practitioners and technicians, health care support, and personal care and service. All of these are physically strenuous occupations that have high injury rates.
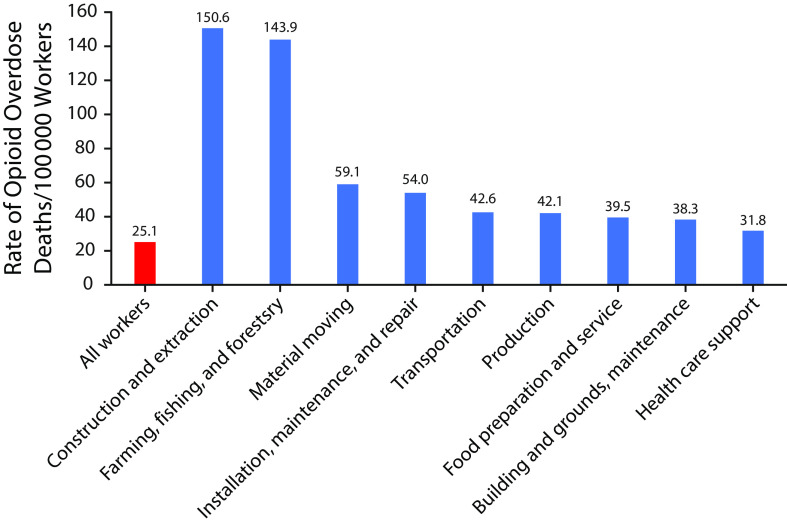
In Massachusetts, an indexing of 4302 death certificates (2011–2015) for opioid-related overdose deaths by industry and occupation27 showed similar results. The rate of fatal opioid overdose varied significantly (Table 1) by decedent industry and occupation of the decedents. Construction and extraction workers had both the highest rate and a high number of OODs (Figure 1). Construction workers accounted for about 23% of all OODs, and the OOD rate in commercial fishing was 4 times the average for all workers. Among women, those working in health care support and food preparation and serving-related occupations had markedly higher rates than the average for all female workers. These industries also have some of the highest rates of occupational injuries and illnesses nationally.18 In the Massachusetts study,27 industry sectors with an average of less than 2 injuries per 100 full-time equivalent workers had the lowest rate of OOD, and industries with more than 4 injuries per 100 full-time equivalent workers had the highest OOD rates.
TABLE 1—
Rate, Number, and Percentage of Opioid-Related Overdose Deaths by Selected Occupations: Massachusetts, 2011–2015
| Occupation | Opioid-Related Overdose Deaths, No. (%) | Rate of Overdose Death/100 000 Workers, Mean (95% CI) |
| Construction and extraction | 1096 (24.8) | 150.6 (146.0, 155.1) |
| Farming, fishing, and forestry | 61 (1.4) | 143.9 (125.4, 162.3) |
| Material moving | 167 (3.9) | 59.1 (54.5, 63.7) |
| Installation, maintenance, repair | 221 (5.1) | 54.0 (50.4, 57.6) |
| Transportation | 203 (4.7) | 42.6 (39.6, 45.6) |
| Production | 312 (7.3) | 42.1 (39.7, 44.5) |
| Food preparation and serving | 372 (8.6) | 39.5 (37.5, 41.6) |
| Building or grounds and maintenance | 230 (5.3) | 38.3 (35.8, 40.9) |
| Health care support | 146 (3.4) | 31.8 (29.2, 34.5) |
| All occupations | 4302 (100.0) | 25.1 (23.4, 26.8) |
Note. CI = confidence interval. Occupations shown have a significantly higher rate than does the “all occupations” category.
Source. Massachusetts Department of Public Health.27
FIGURE 1—
Occupation Groups With Opioid-Related Overdose Death Rates Significantly Higher Than the Average Rate for All Workers: Massachusetts, 2011–2015
Source. Massachusetts Department of Public Health.27
Opioids are frequently prescribed for pain control after occupational injuries,25 although the rate is gradually declining.28 Recently, the efficacy of opioids to provide more than modest, short-term pain control for chronic noncancer pain has been called into question,29–31 and taking opioid pain medications for more than a few days is associated with more disability and longer work absences in workers’ compensation,32 an effect that is not specific to occupational injuries.33 Applebaum et al.34 examined prospective associations between New Mexico Workers’ Compensation injuries and life expectancy over a 19-year follow-up period. Drug‐related causes of death accounted for 8.1% of deaths in this population. The risk of such mortality was increased 3-fold for women who sustained lost-time injuries compared with those who sought compensation for medical expenses only. In men, there was a 30% increase in drug-related mortality for workers with lost-time injuries, but this difference was not statistically significant after controlling for age and industry. Opioids accounted for 61% of drug-related deaths among workers with lost-time work injuries.
Other Work-Related Stressors Pathway
In 2015, an analysis of US death rates by 2 eminent economists called attention to an alarming increase in mortality among middle-aged White, non-Hispanic Americans, attributed to suicide and overuse of alcohol and other drugs.35 The authors referred to these conditions collectively as indicators of distress that amount to “deaths of despair.” They also cited data showing increased prevalence of physical pain in the general population and declines in self-reported health, mental health, and ability to work, along with a parallel growth in Social Security Disability Insurance claims in midlife adults, especially for musculoskeletal and mental health disabilities. They speculated about the impact of rising economic insecurity on population health and pointed to the likely role of depression and other ills stemming from the growth of socioeconomic disparities, noting that people with the lowest education levels had the worst general health, the most pain, and the greatest financial distress.
Many of these associations are evident from the substantial literature about the health effects of working conditions.36,37 For example, job insecurity and other forms of precarious work are associated with worse mental health and increased suicidal ideation.38,39 Psychosocial job stressors—such as the combination of high job demands, low job control, and low social support—have been linked with higher risk of depression40,41 and attempted and completed suicide.42,43 Added to these are the impact on mental health of workplace injury and its sequelae, including lost earnings, risk of reinjury, and long-term disability. An analysis of data from 2134 workers participating in the National Survey of Midlife Development in the United States (MIDUS) II study from 2004 to 200644 showed an OUD prevalence rate of 3.8% and significant associations of OUD with low skill discretion, high psychological demands, and job strain in addition to physical job demands.
The increasing prevalence of insecure work arrangements (e.g., on-call workers, independent contractors, temporary help) further exacerbates the pressure to work in pain. In these arrangements, as well as generally in seasonal occupations (e.g., construction and fishing), people work whenever a job is available or they risk losing income. In a study of automotive assembly plant closures between 1999 and 2016, Venkataramani et al.45 compared OOD rates in US manufacturing counties with and without plant closures. They found an 85% relative increase in OODs for counties with manufacturing plant closures in the previous 5 years.
WORKPLACE BARRIERS AND SOLUTIONS
One barrier for implementing organizational responses to the opioid crisis in the employment setting is the reticence of workers to report episodic or persistent workplace pain and discomfort and, of course, the social stigma and potential for job loss if opioid use (whether legal or illicit) becomes known to coworkers and supervisors. The underreporting of workplace injuries may further obscure relationships between work physical demands, pain, and opioid use. Injury underreporting is a well-documented phenomenon46 despite a no-fault approach to state workers’ compensation insurance systems and national legislation that protects injured workers’ jobs and requires reasonable accommodation for employees in recovery from injuries. As many as 70% of workplace injuries are never captured in the counts of administrative tracking systems.47 Apart from the apparent poor record keeping of employers,46 other factors behind underreporting include fears of retaliation and resentment by peers.48 Recurring pain problems, or work-aggravated conditions that are not bona fide or solely work-related may suffer even more significant underreporting if workers refrain from sharing private health information until their need for accommodation becomes severe. Finding ways for employees to communicate about pain problems, injuries, or substance use without suffering stigma or retaliation remains an important occupational health and safety challenge.
Another question is whether organizations might be able to exert influence on the help-seeking behaviors of employees at risk for overdose through workplace policies and practices. Given that workers are unlikely to report such a problem to their coworkers and supervisors, the effect of employer policies and practices must be indirect, with messages about pain and opioid use communicated across the entire workforce. There are several possibilities to influence health beliefs and behaviors through employer practices and health communications. First, workplace hazards that contribute to musculoskeletal pain and injury could be reduced. Second, the perceived seriousness of opioid use and susceptibility to addiction and overdose could be a target for health messaging in the workplace. Third, worker perceptions about the relative benefits and risks of seeking OUD treatment could be influenced by workplace health promotion efforts that encourage professional assessment and treatment of substance use problems or dose reduction. A fourth opportunity would be to increase the ease with which workers can access OUD treatment, preferably integrated with effective nonopioid pain management, thereby improving the self-efficacy for workers to seek help.
Convincing employers that opioid use prevention is within their possible scope of health promotion activities is, admittedly, an uphill battle. Even if new supportive policies are adopted by company leadership, the organizational culture of industries, corporations, and occupational trades can be deeply entrenched and difficult to change. In our interactions with business owners and managers, many place responsibility for the opioid crisis on the health care, insurance, and pharmaceutical industries. While 80% of business managers for large US employers recognize the seriousness of the opioid crisis, only 30% have altered their health plans to restrict use of prescription opioids, and only 21% have added programs to manage prescription opioid use.49 In another interview study with 501 human resources managers, only 61% indicated any concern with opioid pain reliever misuse in their workforce.50
Some employers ignore employee drug use, while others have doubled down on drug-free workplace policies that strive to weed out and dismiss employees at the first sign of a drug or alcohol problem. Employees and employers might benefit from, for example, a contract or agreement regarding continued employment while in treatment and recovery as verified with periodic drug screening and provider certification. Acknowledging that relapse is an expected part of recovery, employees may require shifting to tasks that do not involve the operation of machinery and other safety-sensitive operations. In our experience, employers are often reticent to include opioid prevention as part of worksite health education programs, even among industries and occupations with the highest OOD rates. Perhaps the most compelling case to engage employers in opioid prevention is a financial one, as employer costs for opioid use, OUD treatment, and related health care and disability insurance are substantial.51 Unfortunately, a more attractive financial option for some employers is firing or not hiring workers with opioid use or a substance use history.
Job insecurity may increase the need to work while in pain and thus increase reliance on pain medication. Fear of losing their jobs can lead people to return to work in pain or before they are healed, leading to use of and addiction to pain medication. Seasonal sectors such as construction and fishing operate in “boom and bust” cycles, creating pressure to work when there is work available and anxiety when there is not. A Massachusetts study found that many construction workers fail to seek or obtain medical treatment, suggesting that stigmatization and fear of job loss may interfere with help-seeking behaviors.52 Similarly, a recent study of lobstermen in the northeast United States showed that many workers with low back injuries did not seek medical treatment.53 Another aspect of precarious work is the lack of paid benefits. The unavailability of paid sick leave also has potential to increase the need to work while in pain and may increase reliance on pain medication. In the Massachusetts study,27 the OOD rate was 4 times higher for industries in which few individuals have access to paid sick leave.
A TOTAL WORKER HEALTH PERSPECTIVE
One method for engaging employers about opioid use and other worker health issues that span work and family life is the Total Worker Health (TWH) perspective recommended by the National Institute for Occupational Safety and Health.54 TWH is defined as “policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness prevention efforts to advance worker well-being.”54 The TWH perspective examines the shared responsibility and opportunity for health and well-being between those who control the conditions at work and the workers themselves, while clarifying employer responsibility for providing safe work. This is relevant to OUD because opioid use can involve both personal risk factors such as age, gender, fitness, occupational identity, and health history and workplace factors such as physical demands, hours of work, job insecurity, and time pressures. TWH approaches might help to draw employer attention to both personal and worksite factors to prevent OUD and overdose. Work-related back injuries, for example, are common in many types of jobs and frequently lead to opioid prescriptions.28,55 While heavy physical workload is an important risk factor, this workload hazard may interact with obesity, lack of aerobic fitness, and other personal health behaviors. The TWH framework may be useful to expand opioid discussions with employers.
RECOMMENDATIONS
The evidence linking the workplace as an exacerbating factor in opioid use is now beginning to coalesce, demonstrating a series of plausible steps in the pathway. Our recommendations (Table 2) address the role of individual employers, policy changes that could change the broader social and economic context, and research needs. Employers can play an important role, even a lifesaving one, at every stage along the continuum: prevention, intervention, treatment, and recovery. Primary prevention interventions include recognizing, evaluating, and controlling workplace hazards that might contribute to acute or chronic injury. While a regulatory structure is generally lacking to enforce employer action toward reducing injury risks from ergonomic hazards, such as lifting, or risks of violence, the Occupational Safety and Health Administration (OSHA) has developed extensive guidance for employers in other domains (e.g., ergonomic and violence prevention programs). Early intervention to reduce hazards contributing to pain and to avoid prescriptions that could potentially lead to a substance use disorder is the very ideal of a public health model of prevention at the source.
TABLE 2—
Recommendations to Address Workplace Factors in the Prevention of Opioid Overdose Deaths: United States, 2020
| Agent | Problem | Actions |
| Government | Lack of regulatory structures and employer guidelines | Enlist OSHA and other federal regulatory bodies to issue guidance and certifications on employer practices to prevent OUD and improve employee access to evidence-based treatments for OUD. |
| Government | Absence of research on workplace factors and interventions to prevent OUD and OOD | NIOSH and other federal funding agencies to prioritize opioid education and OUD prevention as a worksite wellness issue using a TWH framework. |
| Employer | Lack of employer-based policies and actions to address the opioid crisis | Adopt and implement changes to drug-free workplace policies that acknowledge OUD as a medical problem requiring treatment and provide pathways for recovery while preserving workplace safety and productivity. |
| Employer | Limited access of workers to effective OUD treatment | Coordinate with health insurers and benefit managers to increase access to OUD treatment. |
| Employer | Workers receive little education about opioid risks and treatments for OUD | Expand existing safety and wellness training programs to incorporate information about opioid risks, nonpharmacological pain management alternatives, and how to access confidential care. |
| Employer | Few nonpharmacological treatment options available for acute or chronic pain | Impose on health insurers to provide local access to high-quality pain management programs applying behavioral principles, interdisciplinary care, and a biopsychosocial framework. |
| Associations | Absence of peer-based best-practice guidelines for effective employer response to the opioid crisis | Encourage employer-facing associations related to health, disability, and insurance benefits to develop and disseminate effective policies and programs that promote worker health and address organizational barriers and constraints. |
Note. CDC = Centers for Disease Control and Prevention; NIOSH = National Institute for Occupational Safety and Health; OOD = opioid overdose death; OSHA = Occupational Safety and Health Administration; OUD = opioid use disorder; TWH = Total Worker Health.
Return-to-work or stay-at-work accommodations for injured employees are essential to prevent permanent disability and opioid dependence. Too many employees are told there are no job modifications or alternate duty positions available,56 and a return to safe work for those who are in recovery from OUD or injury is essential to prevent a downward spiral of high medical costs, permanent disability, and even death. A 4-way conversation with the supervisor, the employee, the employee’s health care provider, and the employer representative can clarify the return-to-work plan. In the case of substance use disorders, issues of health privacy, stigma, and disclosure pose significant barriers to return-to-work communication,57 so special precautions are necessary. Employers should work with their benefits manager to ensure that employees have access to nonopioid treatments for pain and appropriate and effective care for injuries and for treatment of OUD.
Many people are unaware of which prescriptions contain opioids and their addictive properties. Furthermore, physicians may write opioid prescriptions in ways that do not conform to best-practice guidelines or the needs of workers. Thus, individuals would benefit from opioid hazard awareness programs including skills-based training in how to ask physicians about pain medication and how to access nonopioid pain treatment. Other topics could include safe prescription storage and disposal, awareness of employee assistance programs, health care benefits for treatment of substance use disorders, leave policies, and community resources. Training about use of naloxone to reverse opioid overdoses may be appropriate for certain workplaces and for those employees who are already trained and responsible for first aid.
Opioid education in the workplace could be integrated into health and safety training or wellness education. Such training can cover employer policies and employee rights and communicate a supportive message to combat stigma and fears of retaliation. In the OSHA health and safety management parlance, that means demonstrating management commitment to worker well-being and encouraging employee participation in a nonstigmatizing and recovery-friendly workplace—one that supports recognizing substance use disorder as a disease and supports raising concerns about and addressing working conditions that may be hazardous. Workers should receive treatment without blame, especially when medication overuse has resulted from a painful workplace injury.
More in-depth research should characterize the potential contribution of workplace and job factors to opioid overuse and overdose. Of course, these relationships should be evaluated while accounting for a host of other factors, such as access to medical care, organizational constraints, treatment preferences, and sociocultural influences. Intervention studies should examine the effectiveness of eliminating workplace hazards that cause injuries for which opioids are prescribed, providing appropriate pain management following work injury, finding ways to offer safer opioid prescribing, and providing overdose prevention education and resources. This research should not be limited to individual-level interventions but also should include organizational educational and policy changes to protect high-risk worker populations, such as guaranteed paid sick leave, best-practice pain management and treatment guidelines for work-related injuries that reduce opioid use and addiction risk, and return-to-work accommodations that protect continued healing and avoid injury recurrence.
CONCLUSION
The correspondence between industries with high injury rates and high OOD rates suggests an association between workplace physical demands, workplace pain and injuries, and risk of developing OUD. We recommend stronger regulatory guidance to strengthen employer policies, develop and disseminate best practices for employers within high-risk industries, improve employee education and resources, expand health care benefits to support nonpharmacological pain management approaches and rehabilitation options for OUD, and provide increased funding to develop and test workplace policies and programs related to opioid use. There is a clear need to develop public health interventions in the employment setting to help reverse the continuing opioid crisis.
ACKNOWLEDGMENTS
At the time of the writing of this analytic essay, W. S. Shaw and L. Punnett were receiving funding support from the Center for the Promotion of Health in the New England Workplace, supported by grant 5 U19 OH008857 from the National Institute for Occupational Safety and Health (NIOSH).
Note. This work is solely the responsibility of the authors and does not necessarily represent the official views of NIOSH.
CONFLICTS OF INTEREST
All authors report that they have no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
There was no review by an institutional review board because this analytic essay involves no human participants.
REFERENCES
- 1.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419–1427. doi: 10.15585/mmwr.mm675152e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality. CDC WONDER. US Department of Health and Human Services. 2020. Available at: https://wonder.cdc.gov. Accessed March 10, 2020.
- 3.Pezalla EJ, Rosen D, Erensen JG et al. Secular trends in opioid prescribing in the USA. J Pain Res. 2017;10:383–387. doi: 10.2147/JPR.S129553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rudd RA, Seth P, David F et al. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–1452. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- 5.Mundkur ML, Franklin JM, Abdia Y et al. Days’ supply of initial opioid analgesic prescriptions and additional fills for acute pain conditions treated in the primary care setting—United States, 2014. MMWR Morb Mortal Wkly Rep. 2019;68(6):140–143. doi: 10.15585/mmwr.mm6806a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenblum A, Marsch LA, Joseph H et al. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. 2008;16(5):405–416. doi: 10.1037/a0013628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strickler GK, Kreiner PW, Halpin JF et al. Opioid prescribing behaviors—prescription behavior surveillance system, 11 states, 2010–2016. MMWR Surveill Summ. 2020;69(1):1–14. doi: 10.15585/mmwr.ss6901a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meadowcroft D, Whitacre B. Do prescription drug monitoring programs encourage prescription—or illicit—opioid abuse? Subst Abus. 2019;10:1–11. doi: 10.1080/08897077.2019.1695707. [DOI] [PubMed] [Google Scholar]
- 9.Dowell D, Haegerich TM, Chou R et al. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 10.Qaseem A, Wilt TJ, McLean RM et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services. HHS awards nearly $400 million to combat the opioid crisis. August 8, 2019. Available at: https://www.hhs.gov/about/news/2019/08/08/hhs-awards-nearly-400-million-to-combat-opioid-crisis.html. Accessed March 10, 2020.
- 12. Results from the 2012 National Survey on Drug Use and Health: summary of national findings. HHS Publication no. SMA 13-4795. Rockville, MD: Center for Behavioral Health Statistics and Quality; 2013.
- 13.Ricci JA, Stewart WF, Chee E, Leotta C, Foley K, Hochberg MC. Back pain exacerbations and lost productive time costs in United States workers. Spine. 2006;31(26):3052–3060. doi: 10.1097/01.brs.0000249521.61813.aa. [DOI] [PubMed] [Google Scholar]
- 14.Burton WN, Pransky G, Conti DJ, Chen CY, Edington DW. The association of medical conditions and presenteeism. J Occup Environ Med. 2004;46(6 suppl):S38–S45. doi: 10.1097/01.jom.0000126687.49652.44. [DOI] [PubMed] [Google Scholar]
- 15.US Department of Health and Human Services. QuickStats: Age-adjusted percentage of adults aged ≥ 18 years who were never in pain, in pain some days, or in pain most days or every day in the past 6 months, by employment status—National Health Interview Survey, United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(29):796. doi: 10.15585/mmwr.mm6629a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buchmueller TC, Valletta RG. Work, health, and insurance: a shifting landscape for employers and workers alike. Health Aff (Millwood) 2017;36(2):214–221. doi: 10.1377/hlthaff.2016.1200. [DOI] [PubMed] [Google Scholar]
- 17.Kowalski-McGraw M, Green-McKenzie J, Pandalai SP, Schulte PA. Characterizing the interrelationships of prescription opioid and benzodiazepine drugs with worker health and workplace hazards. J Occup Environ Med. 2017;59(11):1114–1126. doi: 10.1097/JOM.0000000000001154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bureau of Labor Statistics, US Department of Labor. 2016 Survey of Occupational Injuries & Illnesses Charts Package. November 9, 2017. Available at: https://www.bls.gov/iif/osch0060.pdf. Accessed March 1, 2020.
- 19.National Research Council, Institute of Medicine. Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities. Panel on Musculoskeletal Disorders and the Workplace. Commission on Behavioral and Social Sciences and Education. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 20.da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med. 2010;53(3):285–323. doi: 10.1002/ajim.20750. [DOI] [PubMed] [Google Scholar]
- 21.Dissel R. Ohio construction workers seven times more likely to die of an opioid overdose in 2016. Plain Dealer. November 5, 2017. Available at: https://www.cleveland.com/metro/index.ssf/2017/11/ohio_construction_workers_seven_times_more_likely_to_die_of_an_opioid_overdose_in_2016.html. Accessed March 7, 2018.
- 22.Bunn T, Bush A, Slavova S. Drug overdose deaths by specific employment industry, occupation, and drug type. J Ky Med Assoc. 2014;112:201–211. [Google Scholar]
- 23.Harik V, Janiszewski M, Allen N. Analysis of opioid-related overdose deaths on Cape Cod, 2004–2014: implications for trades/service workers and the straight-to-work population. Barnstable County Regional Substance Use Council, Barnstable County Department of Human Services. October 5, 2017. Available at: http://www.bchumanservices.net/library/2018/02/BCDHS-Death-Certificate-Analysis-Final-Report-10-5-17-Update-1.pdf. Accessed April 23, 2018.
- 24.Funaiole P, Dustin L, Spencer P. Harnessing the tradition of brotherhood to reduce opioid overdose deaths among trades workers in Massachusetts. Presented at the annual meeting of the National Prevention Network; September 2017; Anaheim, CA. Available at: http://www.npnconference.org/wp-content/uploads/2017/09/Funaiole-Dustin-Spencer.pdf. Accessed May 12, 2018.
- 25.Cheng M, Sauer BC, Johnson E, Porucznik C, Hegmann K. Comparison of opioid-related deaths by work-related injury. Am J Ind Med. 2013;56(3):308–316. doi: 10.1002/ajim.22138. [DOI] [PubMed] [Google Scholar]
- 26.Harduar Morano L, Steege AL, Luckhaupt SE. Occupational patterns in unintentional and undetermined drug-involved and opioid-involved overdose deaths—United States, 2007–2012. MMWR Morb Mortal Wkly Rep. 2018;67(33):925–930. doi: 10.15585/mmwr.mm6733a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Opioid-related overdose deaths in Massachusetts by industry and occupation 2011–2015. Boston, MA: Massachusetts Department of Public Health, Occupational Health Surveillance Program; 2018.
- 28.Pensa MA, Galusha DH, Cantley LF. Patterns of opioid prescribing and predictors of chronic opioid use in an industrial cohort, 2003–2013. J Occup Environ Med. 2018;60(5):457–461. doi: 10.1097/JOM.0000000000001231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Els C, Jackson TD, Hagtvedt R et al. High-dose opioids for chronic non-cancer pain: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;10:CD012299. doi: 10.1002/14651858.CD012299.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abdel Shaheed C, Maher CG, Williams KA, Day R, McLachlan AJ. Efficacy, tolerability, and dose-dependent effects of opioid analgesics for low back pain: a systematic review and meta-analysis. JAMA Intern Med. 2016;176(7):958–968. doi: 10.1001/jamainternmed.2016.1251. [DOI] [PubMed] [Google Scholar]
- 31.Busse JW, Wang L, Kamaleldin M et al. Opioids for chronic noncancer pain: a systematic review and meta-analysis. JAMA. 2018;320(23):2448–2460. doi: 10.1001/jama.2018.18472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Busse JW, Ebrahim S, Heels-Ansdell D, Wang L, Couban R, Walter SD. Association of worker characteristics and early reimbursement for physical therapy, chiropractic and opioid prescriptions with workers’ compensation claim duration, for cases of acute low back pain: an observational cohort study. BMJ Open. 2015;5(8):e007836. doi: 10.1136/bmjopen-2015-007836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chou R, Turner JA, Devine EB et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015;162(4):276–286. doi: 10.7326/M14-2559. [DOI] [PubMed] [Google Scholar]
- 34.Applebaum KM, Asfaw A, O’Leary PK, Busey A, Tripodis Y, Boden LI. Suicide and drug‐related mortality following occupational injury. Am J Indus Med. 2019 doi: 10.1002/ajim.23021. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Case A, Deaton A. Rising morbidity and mortality in midlife among White non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.LaMontagne AD, Keegel T, Louie AM, Ostry A. Job stress as a preventable upstream determinant of common mental disorders: a review for practitioners and policy-makers. Adv Ment Health. 2014;9(1):17–35. [Google Scholar]
- 37.Stansfeld S, Candy B. Psychosocial work environment and mental health—a meta-analytic review. Scand J Work Environ Health. 2006;32(6):443–462. doi: 10.5271/sjweh.1050. [DOI] [PubMed] [Google Scholar]
- 38.Rönnblad T, Grönholm E, Jonsson J et al. Precarious employment and mental health: a systematic review and meta-analysis of longitudinal studies. Scand J Work Environ Health. 2019;45(5):429–443. doi: 10.5271/sjweh.3797. [DOI] [PubMed] [Google Scholar]
- 39.Milner A, LaMontagne AD, Spittal MJ, Pirkis J, Currier D. Job stressors and employment precarity as risks for thoughts about suicide: an Australian study using the Ten to Men cohort. Ann Work Expo Health. 2018;62(5):583–590. doi: 10.1093/annweh/wxy024. [DOI] [PubMed] [Google Scholar]
- 40.LaMontagne AD, Milner A. Working conditions as modifiable risk factors for suicidal thoughts and behaviors. Occup Environ Med. 2017;74(1):4–5. doi: 10.1136/oemed-2016-104036. [DOI] [PubMed] [Google Scholar]
- 41.Stansfeld SA, Shipley MJ, Head J, Fuhrer R. Repeated job strain and the risk of depression: longitudinal analyses from the Whitehall II study. Am J Public Health. 2012;102(12):2360–2366. doi: 10.2105/AJPH.2011.300589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nishimura M, Terao T, Soeda S, Nakamura J, Iwata N, Sakamoto K. Suicide and occupation: further supportive evidence for their relevance. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28(1):83–87. doi: 10.1016/j.pnpbp.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 43.Tsutsumi A, Kayaba K, Ojima T, Ishikawa S, Kawakami NB Jichi Medical School Cohort Study Group. Low control at work and the risk of suicide in Japanese men: a prospective cohort study. Psychother Psychosom. 2007;76(3):177–185. doi: 10.1159/000099845. [DOI] [PubMed] [Google Scholar]
- 44.Choi B. Opioid use disorder, job strain, and high physical job demands in US workers. Int Arch Occup Environ Health. 2020 doi: 10.1007/s00420-019-01514-4. epub ahead of print January 9, 2020. [DOI] [PubMed] [Google Scholar]
- 45.Venkataramani AS, Bair EF, O’Brien RL, Tsai AC. Association between automotive assembly plant closures and opioid overdose mortality in the United States. JAMA Intern Med. 2019;180(2):254–262. doi: 10.1001/jamainternmed.2019.5686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wuellner SE, Bonauto DK. Exploring the relationship between employee recordkeeping and underreporting in the BLS Survey of Occupational Injuries and Illnesses. Am J Ind Med. 2014;57(10):1133–1143. doi: 10.1002/ajim.22350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rosenman KD. OSHA, well past its infancy, but still learning how to count injuries and illnesses. Am J Ind Med. 2016;59(8):595–599. doi: 10.1002/ajim.22623. [DOI] [PubMed] [Google Scholar]
- 48.Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am J Public Health. 2002;92(9):1421–1429. doi: 10.2105/ajph.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miller S. Employers take steps to address opioid crisis. Society of Human Resources Management. November 28, 2017. Available at: https://www.shrm.org/resourcesandtools/hr-topics/benefits/pages/steps-to-address-opioid-crisis.aspx. Accessed March 1, 2020.
- 50.Abd-Elsayed A, Fischer M, Dimbert J, Fiala KJ. Prescription drugs and the US workforce: results from a National Safety Council survey. Pain Physician. 2020;23(1):1–16. [PubMed] [Google Scholar]
- 51.Rice JB, Kirson NY, Shei A et al. Estimating the costs of opioid abuse and dependence from an employer perspective: a retrospective analysis using administrative claims data. Appl Health Econ Health Policy. 2014;12(4):435–446. doi: 10.1007/s40258-014-0102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moore JT, Ciguloarov KP, Sampson JM, Rosecrance JC, Chen PJ. Construction workers’ reasons for not reporting work-related injuries; an exploratory study. Int J Occup Saf Ergon. 2013;19(1):97–105. doi: 10.1080/10803548.2013.11076969. [DOI] [PubMed] [Google Scholar]
- 53.Lavin RA, Kalia N, Yuspeh L, Barry JA, Bernacki EJ, Tao XG. Work enabling opioid management. J Occup Environ Med. 2017;59(8):761–764. doi: 10.1097/JOM.0000000000001080. [DOI] [PubMed] [Google Scholar]
- 54.Tamers SL, Chosewood LC, Childress A, Hudson H, Nigam J, Chang C. Total Worker Health® 2014–2018: the novel approach to worker safety, health and well-being evolves. Int J Environ Res Public Health. 2019;16(3):E321. doi: 10.3390/ijerph16030321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lin DH, Jones CM, Compton WM et al. Prescription drug coverage for treatment of low back pain among US Medicaid, Medicare Advantage, and commercial insurers. JAMA Netw Open. 2018;1(2):e180235. doi: 10.1001/jamanetworkopen.2018.0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shaw WS, Pransky G, Fitzgerald TE. Early prognosis for low back disability: intervention strategies for health care providers. Disabil Rehabil. 2001;23(18):815–828. doi: 10.1080/09638280110066280. [DOI] [PubMed] [Google Scholar]
- 57.Crapanzano KA, Hammarlund R, Ahmad B, Hunsinger N, Kullar R. The association between perceived stigma and substance use disorder treatment outcomes: a review. Subst Abuse Rehabil. 2018;10:1–12. doi: 10.2147/SAR.S183252. [DOI] [PMC free article] [PubMed] [Google Scholar]