Abstract
Background
Mediastinal myelolipoma is extremely rare. It is a benign nonfunctioning tumor composed of hematopoietic tissue and mature fatty tissue. Although computed tomography and magnetic resonance imaging are effective in diagnosing mediastinal myelolipoma, a definitive diagnosis is difficult to establish for rare extra-adrenal myelolipomas by imaging alone. Such tumors are often misdiagnosed as malignant retropleural liposarcoma, denoting a poor prognosis.
Case presentation: We herein describe a 72-year-old man with multiple bilateral paravertebral mediastinal myelolipomas and discuss the imaging findings and differential diagnoses. We used a computed tomography-guided core biopsy to attain a preoperative diagnosis. Using this technique, we avoided an unnecessary surgical procedure for the patient’s asymptomatic and relatively small lesions.
Conclusions
Instead of biopsy by lesion excision, we advocate conducting a precisely targeted, minimally invasive computed tomography-guided core biopsy to obtain a definitive preoperative diagnosis and thus avoid unnecessary surgery for mediastinal myelolipoma, a benign nonfunctioning tumor.
Keywords: Mediastinum, myelolipoma, diagnosis, biopsy, imaging, treatment
Background
Myelolipoma was first reported by the pathologist Edgar von Gierke in 1905.1 It is usually a nonfunctioning benign tumor that is incidentally detected in the adrenal gland during routine computed tomography (CT). The occurrence of myelolipoma in an extra-adrenal site is rare. A summary of 37 extra-adrenal myelolipomas (EAMLs) was reported in 2003, and nearly half of these lesions were located in the presacral area.2 Only 3% of reported EAMLs were located in the mediastinum.3 A definitive diagnosis is difficult to establish for EAMLs by imaging alone. Such tumors are often misdiagnosed as malignant retropleural liposarcoma, denoting a poor prognosis. We herein describe a 72-year-old man with multiple bilateral paravertebral mediastinal myelolipomas and discuss the imaging characteristics and differential diagnoses. We used a CT-guided core biopsy to attain a preoperative diagnosis.
Case presentation
A 72-year-old man presented to the rheumatology department with a 1-month history of acute polyarthralgia involving the bilateral shoulders, knees, wrists, elbows, and metacarpophalangeal joints. He had been smoking 20 cigarettes per day for the last 40 years and had mild respiratory symptoms including an occasional cough. He had no history of morning joint stiffness, oral ulcers, Raynaud’s phenomenon, low back pain, heel pain, xerostomia, or xerophthalmia.
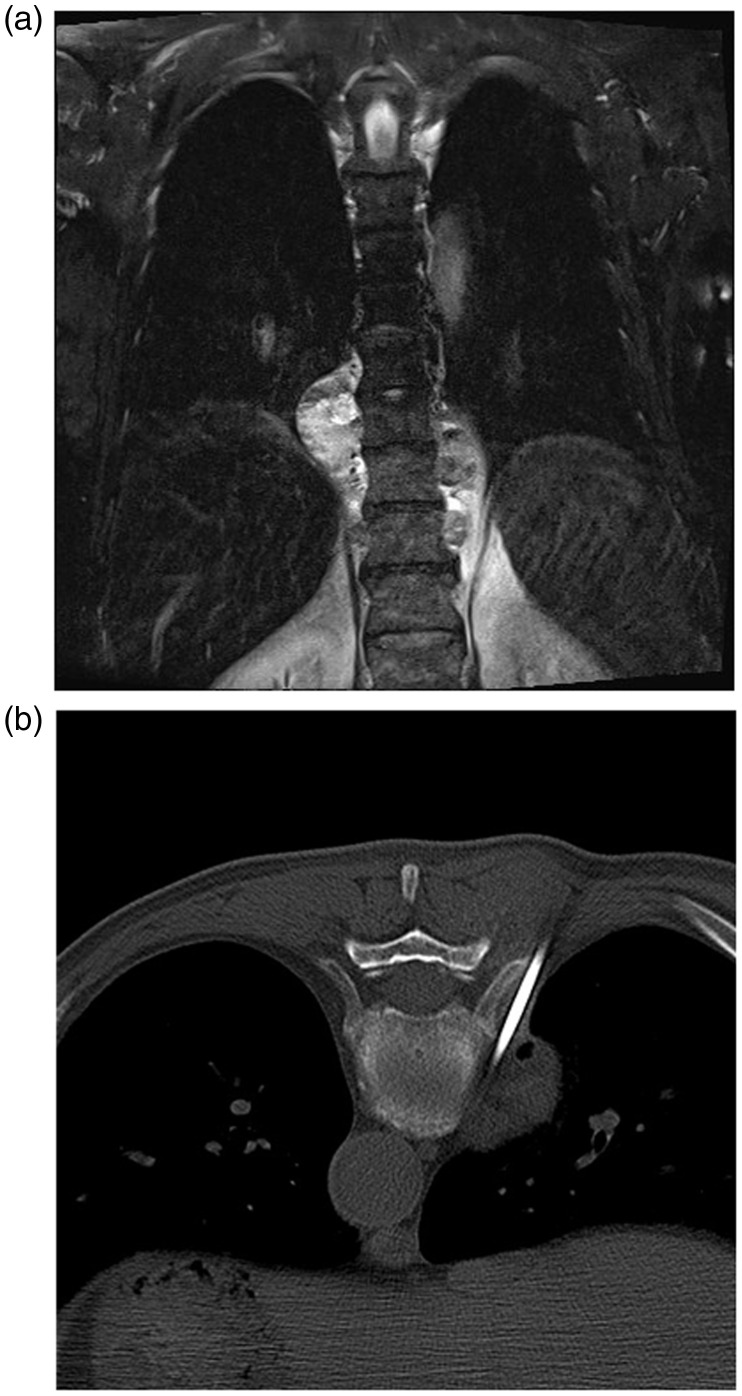
On physical examination, all superficial lymph nodes were normal, but his peripheral joints appeared mildly red, swollen, warm, and tender. Laboratory findings revealed an erythrocyte sedimentation rate of 60 mm/h (reference, <20 mm/h) and C-reactive protein concentration of 68.70 mg/L (reference, <8 mg/L). The results of all other tests were within the reference range. Plain radiographs of the patient’s painful joints revealed moderate degenerative changes. A plain chest radiograph showed a paravertebral spindle high-density shadow at the thoracic 8 to 11 spinal levels. Single-photon emission computed tomography with a technetium-99m methylene diphosphonate bone scan showed hypermetabolic changes in the right sternoclavicular and left knee joint, indicating benign degenerative changes. Noncontrast chest CT showed multiple bilateral paravertebral lesions of heterogeneous density and well-defined margins in the posterior mediastinum at the thoracic 8 to 11 spinal levels. The density of the lesions ranged from −97.0 to +70.0 Hounsfield units, and the largest section was 4.4 × 2.9 cm in diameter. None of the lesions contained calcification or heterogeneous contents. Thoracic magnetic resonance imaging (MRI) showed bilateral foci with an inhomogeneous signal (Figure 1(a)). The lesions were oval, asymmetric, fat-containing, and well demarcated from the descending aorta in the posterior mediastinum. Based on these imaging findings, the most probable diagnosis was liposarcoma or lymphoma. Considering the concomitant polyarthralgia, however, a neuroendocrine tumor could not be excluded.
Figure 1.
Imaging findings and needle biopsy. (a) Coronal T2 fat saturation magnetic resonance image showing bilateral multiple inhomogeneous paravertebral lesions. (b) Prone computed tomography-guided core needle biopsy of the lesion for definitive diagnosis.
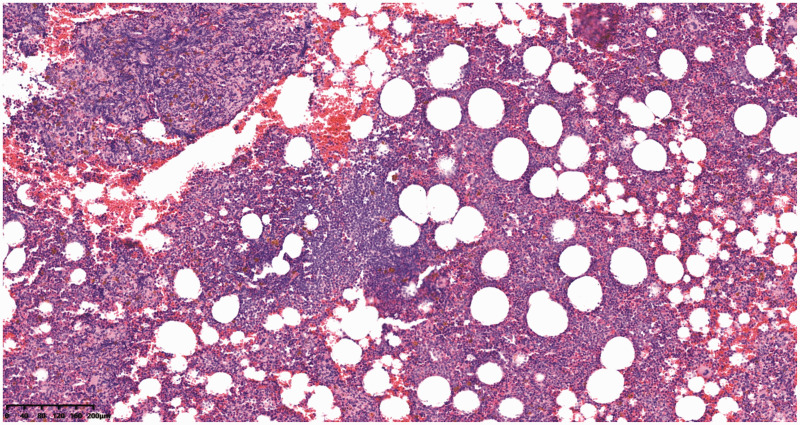
The diagnosis was uncertain, and the patient declined a surgical operation because he had mild respiratory symptoms. After he provided informed consent, the patient underwent a percutaneous CT-guided core biopsy of the lesion (Figure 1(b)). Histopathologically, the mass consisted of mature adipose tissue combined with myeloid and erythroid cells (Figure 2). Immunohistochemistry revealed negativity to synaptophysin, chromogranin A, CD56, and S-100 antibodies and positivity to myeloperoxidase. A diagnosis of mediastinal myelolipoma was made. The patient was prescribed celecoxib (Celebrex® capsules; Pfizer, New York, NY, USA) at 200 mg twice a day for 2 weeks, and his polyarthralgia significantly improved. Conservative observation was selected because the lesions were small. During 24 months of follow-up, imaging examinations showed that the lesions were nonprogressive, and the patient was thus able to avoid a surgical procedure.
Figure 2.
Histopathologic examination. Microscopically, predominantly mature adipose tissue combined with myeloid and erythroid cells was observed (hematoxylin and eosin, ×100).
Discussion
EAMLs are rare, and until 2017, only 49 cases of mediastinal myelolipomas (including our case) had been reported.4 Patients with EAML are generally older (mean age of 64 years) than patients with adrenal myelolipoma (mean age of 55 years). EAML seems to occur with female predominance (2:1 female:male ratio).5 The pathogenesis has not yet been completely established. These tumors are often asymptomatic and detected incidentally, and they have a good prognosis; however, they may also cause a wide variety of nonspecific symptoms. A primary diagnosis of thoracic spinal tuberculosis or paravertebral cold abscess was initially suspected in our patient because his plain chest radiograph showed a paravertebral spindle high-density shadow. Because of his polyarthralgia, we also considered Poncet’s disease (reactive arthritis associated with tuberculosis). However, repeated smears for acid-fast bacilli and a polymerase chain reaction assay for Mycobacterium tuberculosis from sputum and blood samples were negative, and Poncet’s disease was excluded.
EAMLs are usually well-defined round masses with a mean diameter of 5.9 cm (range, 1.5–25 cm).6 CT and MRI can be used to effectively diagnose myelolipoma. The different ratios of bone marrow tissue and adipose tissue in EAMLs can explain the diversity of CT densities. On CT, fat generally has low attenuation of ≤20 Hounsfield units and appears darker than muscle and brighter than air. It is important to identify the high-attenuation area of the predominant myeloid element in the low-attenuation area of the fatty element.7 On T1- and T2-weighted MRI, EAMLs show high-signal intensity for mature adipose tissue. The signal of the myeloid element is low on T1-weighted imaging and moderate on T2-weighted imaging. Fat tissue can be easily detected on MRI using a fat saturation technique. In our patient, the CT and MRI findings did not coincide with those of a tuberculosis-associated paravertebral abscess.
Although CT and MRI are effective in diagnosing myelolipoma, the imaging differential diagnoses for fat-containing lesions are often extensive and include non-neoplastic, benign, and malignant entities. Thus, a definitive diagnosis of EAML is difficult to establish by imaging alone. Among posterior mediastinal tumors, the most commonly differential diagnosis is a malignant retropleural fat-containing tumor (liposarcoma). Myelolipomas tend to have clear margins in contrast to liposarcomas, which tend to be less well-circumscribed and vary according to the subtypes. Well-differentiated liposarcoma typically contains more than 75% adipose tissue, and dedifferentiated liposarcoma can be quite complex on imaging, often containing heterogeneous nonlipomatous components.8 Other differential diagnoses include extramedullary hematopoiesis, neurogenic tumor, lymphoma, and teratoma. Therefore, some authors have suggested conducting a CT-guided or ultrasonography-guided fine-needle aspiration or core biopsy to obtain a definitive diagnosis,5,7,9,10 as highlighted in the present case. However, because most EAMLs occur in the posterior mediastinum (93%), the spine may block the biopsy approach if entering from the posterior chest wall. Additionally, the biopsy procedure may be associated with risks such as hemorrhage, pneumothorax, or tumor cell seeding. Thus, some authors do not advocate performing a core biopsy for posterior mediastinal lesions.4 In our opinion, however, percutaneous CT-guided core biopsy is precisely targeted, safe, and effective.11
Myelolipoma can be classified into two types according to its pathology. Type I shows mostly adipose tissue with a small focal distribution of hematopoietic tissue. Type II shows myeloid components mainly containing the rich marrow hematopoietic tissue. Routine hematoxylin and eosin staining is usually adequate for the diagnosis. For the differential diagnosis, immunohistochemistry for neurogenic, myeloid, and lymphoid antibodies can be performed as in the present case. It is difficult and important to discriminate myelolipoma from extramedullary hematopoiesis. The microscopic features are similar between the two. Extramedullary hematopoietic tumors occur at multiple sites and are most commonly located in the thoracic paravertebral area, where they appear more lobulated and nested against the costovertebral angle.12 In contrast, the characteristic feature of myelolipoma is a round or oval solitary mass or, in rare cases, bilateral masses.
Treatment of EAML is either observational or surgical. There is no clear consensus regarding what lesion size is most appropriate for observation or an operation. Many reports have suggested that if the diameter of an asymptomatic EAML is less than 4 cm, the patient can choose dynamic observation.13 If the patient presents with symptoms such as coughing, panting, or nerve compression, an operation should be performed. The surgical approach (video-assisted thoracoscopic surgery or thoracotomy) is determined according to the size and location of the tumor.14,15 Our patient was treated with oral celecoxib, and his polyarthralgia significantly improved. Conservative observation was selected because his lesions were small. For 24 months, his follow-up imaging examinations showed no progression, and surgery was withheld. Further follow-up will continue.
Although CT and MRI are effective in diagnosing myelolipoma, a definitive diagnosis of EAML is difficult to establish by imaging alone. We advocate conducting a precisely targeted, minimally invasive CT-guided core biopsy to obtain a definitive preoperative diagnosis and thus avoid unnecessary surgery for this benign nonfunctioning tumor.
Authors’ contributions
XQR and SZ analyzed and interpreted the patient’s data. DAQ performed the biopsy of the lesion and was a major contributor in writing the manuscript. HB performed the pathological tests. All authors read and approved the final manuscript.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Ethics
Ethics approval for this report was granted by the Shanxi Medical University Ethics Committee. The patient provided consent for publication of his anonymized data.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
De-an Qin https://orcid.org/0000-0002-3025-2706
References
- 1.Oberling C. Les formations myelo-lipomateuses. Bull Assoc Fr Etude Cancer 1929; 18: 234–246. [Google Scholar]
- 2.Singla AK, Kechejian G, Lopez MJ. Giant presacral myelolipoma. Am Surg 2003; 69: 334–338. [PubMed] [Google Scholar]
- 3.Nakagawa M, Kohno T, Mun M, et al. Bilateral video-assisted thoracoscopic surgery resection for multiple mediastinal myelolipoma: report of a case. Korean J Thorac Cardiovasc Surg 2014; 47: 189–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi Q, Pan S, Bao Y, et al. Primary mediastinal myelolipoma: a case report and literature review. J Thorac Dis 2017; 9: E219–E225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kenney PJ, Wagner BJ, Rao P, et al. Myelolipoma: CT and pathologic features. Radiology 1998; 208: 87–95. [DOI] [PubMed] [Google Scholar]
- 6.Xiong Y, Wang Y, Lin Y. Primary myelolipoma in posterior mediastinum. J Thorac Dis 2014; 6: E181–E187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kawanami S, Watanabe H, Aoki T, et al. Mediastinal myelolipoma: CT and MRI appearances. Eur Radiol 2000; 10: 691–693. [DOI] [PubMed] [Google Scholar]
- 8.Teniola O, Wang KY, Wang WL, et al. Imaging of liposarcomas for clinicians: characteristic features and differential considerations. J Surg Oncol 2018; 117: 1195–1203. [DOI] [PubMed] [Google Scholar]
- 9.Wadood DQ, Qureshi DSA, Singh DP, et al. A rare case of co-existing adrenal and pelvic myelolipomas. Radiol Case Rep 2018; 13: 999–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Itani M, Wasnik AP, Platt JF. Radiologic–pathologic correlation in extra-adrenal myelolipoma. Abdom Imaging 2014; 39: 394–397. [DOI] [PubMed] [Google Scholar]
- 11.Qin DA, Song JF, Li XF, et al. Tophaceous gout of lumbar spine with fever mimicking infection. Am J Med 2018; 131: e353–e356. [DOI] [PubMed] [Google Scholar]
- 12.Koch CA, Li CY, Mesa RA, et al. Nonhepatosplenic extramedullary hematopoiesis: associated diseases, pathology, clinical course, and treatment. Mayo Clin Proc 2003; 78: 1223–1233. [DOI] [PubMed] [Google Scholar]
- 13.Franiel T, Fleischer B, Raab BW, et al. Bilateral thoracic extraadrenal myelolipoma. Eur J Cardiothorac Surg 2004; 26: 1220–1222. [DOI] [PubMed] [Google Scholar]
- 14.Ventura L, Martella EM, Rusca M, et al. Posterior mediastinal myelolipoma resected by video-assisted thoracic surgery. J Minim Access Surg 2019; 15: 65–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shen C, Zhou K, Lai Y, et al. Review of primary extra-adrenal myelolipoma of the thorax. J Surg Res 2017; 207: 131–137. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.