Abstract
Purpose
to report five patients all presenting with persistent unilateral epiphora as a sign of unexpected and rare lesions causing Secondary Acquired Nasolacrimal Duct Obstruction (SANDO) and the risks associated to an incomplete diagnostic work-up.
Observations
the cases presented are: (1) Fungus ball, (2) Pyogenic granuloma, (3) Sinonasal inverted papilloma (4) Sinonasal inverted papilloma with synchronous squamous cell carcinoma, (5) Squamous cell carcinoma of the lacrimal sac.
Conclusions and importance
masses are uncommon but not a rare cause of nasolacrimal duct obstruction. Surgical teams performing large numbers of dacryocystorhinostomies should be aware of such pathology and perform a systematic multidisciplinary approach.
Keywords: Fungus ball, Pyogenic granuloma, Sinonasal inverted papilloma, Squamous cell carcinoma, Lacrimal sac tumors, Tearing
1. Introduction
True epiphora is an overflow of tears over the cheek and most commonly results from insufficient drainage through the lacrimal excretory system.1 Nasolacrimal duct obstruction may have different etiologies and can be either primary or secondary, with primary acquired nasolacrimal duct obstruction (PANDO) being the most common.2, 3, 4, 5 The secondary causes, which can ultimately affect all sections of the draining lacrimal duct, include infectious, inflammatory, neoplastic, traumatic and mechanical blockage and are summarized under the term “secondary acquired nasolacrimal drainage obstruction” (SANDO).6,7 At Humanitas Research Hospital, Eye center, the diagnosis lies essentially in the ophthalmological examination, including the lacrimal duct probing with the Bowman probe and, if necessary, lacrimal duct flushing. The probe serves to distinguish a so-called soft or hard stop. In the case of a pre-saccular stenosis in the upper, lower or common tear ducts, the probe encounters resistance, “soft stop”, while in the case of a post-saccular stenosis, the probe hits the bony medial wall of the lacrimal sac and there is a “hard stop".8 If the ophthalmologist proves a post-saccular stenosis of the nasolacrimal duct, an anterior rhinoscopy and an endoscopic examination of the nose always follows. Imaging procedures are subsequently performed in individual cases.7,8 CT dacryocystography is the test of choice at our institution, although it is regarded as minor by other groups.9
2. Findings
Out of a total of 450 endoscopic endonasal dacryocystorhinostomies (Endo-DCR) procedures that have been performed in the last 5 years, we report a case series of 5 patients whose diagnostic workup or therapeutic approach ended up being peculiar and unexpected.
2.1. Case 1 (fungus ball)
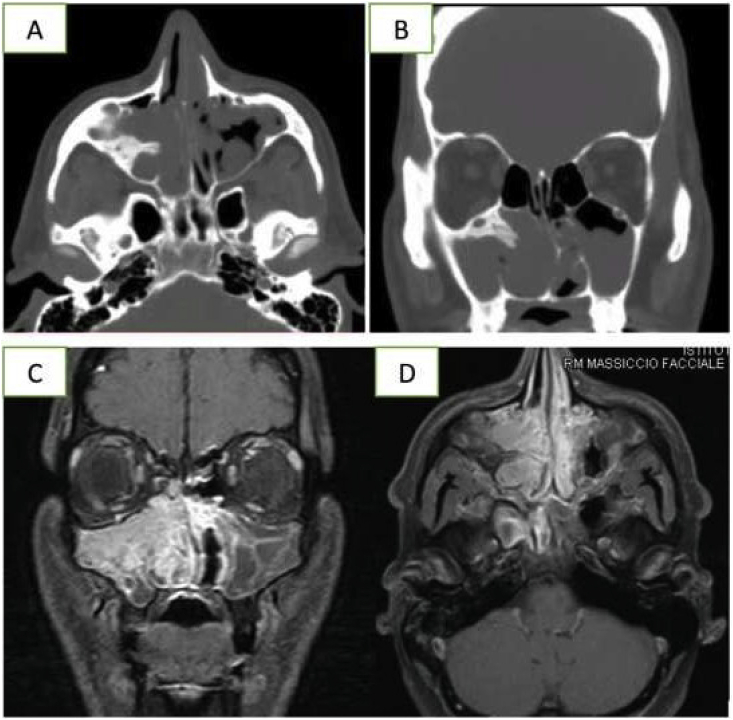
A 43-year-old male was referred to the ophthalmology department only complaining with a 2-month unilateral epiphora. He denied nasal obstruction, rhinorrhea, headache, facial pain, or cacosmia. Post-saccular obstruction was diagnosed at probing and irrigation. The eye exam ruled out other causes of epiphora. Endoscopic examination of the nose highlighted edema of the lateral nasal wall with the presence of nasal polyps suspicious of inflammatory disease. The CT and MRI scan detected fungal sinus disease showing a pathognomonic pattern (Fig. 1A–D). Sinus fungus ball is characterized by an extramucosal fungal proliferation that fills one or more of the paranasal sinuses.9 Clinical diagnosis of sinus fungus ball is difficult because the symptoms are nonspecific and approximately 10%–20% of the cases are asymptomatic.11 The patient underwent Functional Endoscopic Sinus Surgery (FESS) on the inferior turbinate and the right maxillary sinus. Surgical treatment of a fungus ball consists in opening the infected sinus cavity at the level of its ostium and removing fungal concretions while sparing the normal mucosa.12 Complete resolution of the disease was obtained. Endoscopic exploration through the middle antrostomy at 10 and 21 days follow-up after surgery showed complete resolution of the disease without symptoms.
Fig. 1.
Case 1 (A–B): heterogeneous CT signaling due to areas of high attenuation caused by ferromagnetic elements (iron-like pattern) with middle turbinate pneumatization (concha bullosa). (C–D): MRI scan of the same patient.
2.2. Case 2 (pyogenic granuloma)
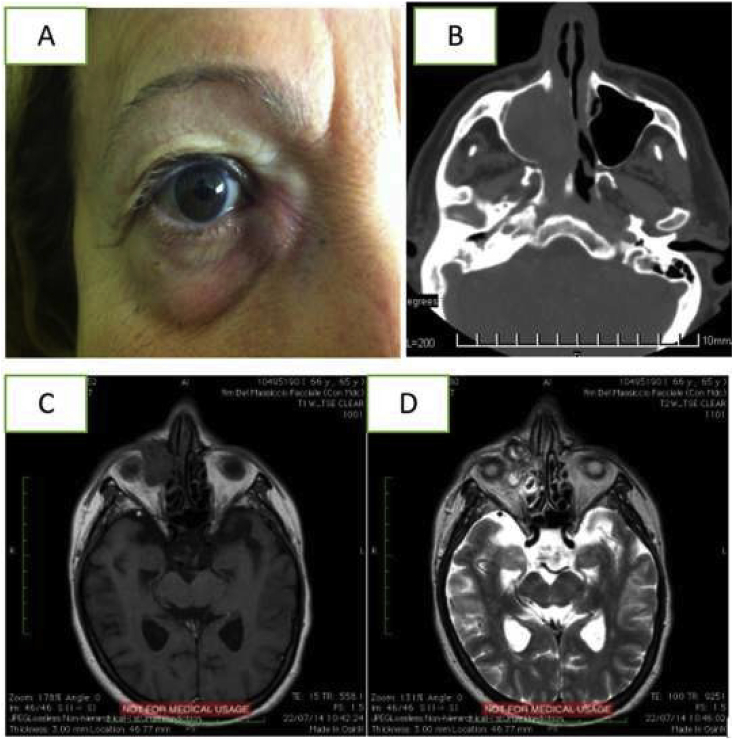
A 61-year-old male affected by Obstructive Sleep Apnea Syndrome (OSAS) was referred to the ophthalmology department for persistent unilateral epiphora. He also complained of breathing difficulty, nasal obstruction, rhinorrhea and sporadic nasal bleeding. These symptoms were attributed to allergy and the use of C-PAP. Post-saccular obstruction was diagnosed at probing and irrigation. The eye exam ruled out other causes of epiphora. Endoscopic examination of the nasal cavities revealed a red-brown bulky lesion originating from the right lateral nasal wall. The mass disrupted the anatomic landmarks and manipulation elicited active bleeding. The CT scan showed the extension of the lesion within the right nasal cavity and maxillary sinus, up to the medial wall of the maxillary sinus, which had been eroded. MRI with gadolinium better defined the mass border (Fig. 2A–D). FESS (functional endoscopic sinus surgery) was performed to obtain mass and inferior turbinate removal. Due to the erosion of the lateral nasal wall, a stoma between the lacrimal sac and the nasal cavity was created so as to maintain the lacrimal drainage system patent. The histopathological examination made the diagnosis of pyogenic granuloma, a benign vascular lesion characterized by inflammatory cells and lobular capillary proliferation.13 The patient was followed up every two months for a year and experience resolution of epiphora and no sign of recurrence.
Fig. 2.
Case 2 (A): External appearance of patient. CT (B) and Gadolinium MRI (C, D) showing the radiological pattern of the bulky tumor centered on the inferior turbinate and the lateral nasal wall with involvement of Hasner's valve. The high vascularity is responsible for signal voids. The medial wall of the maxillary sinus and the nasolacrimal duct manifest erosion due to the compression but there is no radiological sign of secondary to bone infiltration.
2.3. Case 3 (sinonasal inverted papilloma)
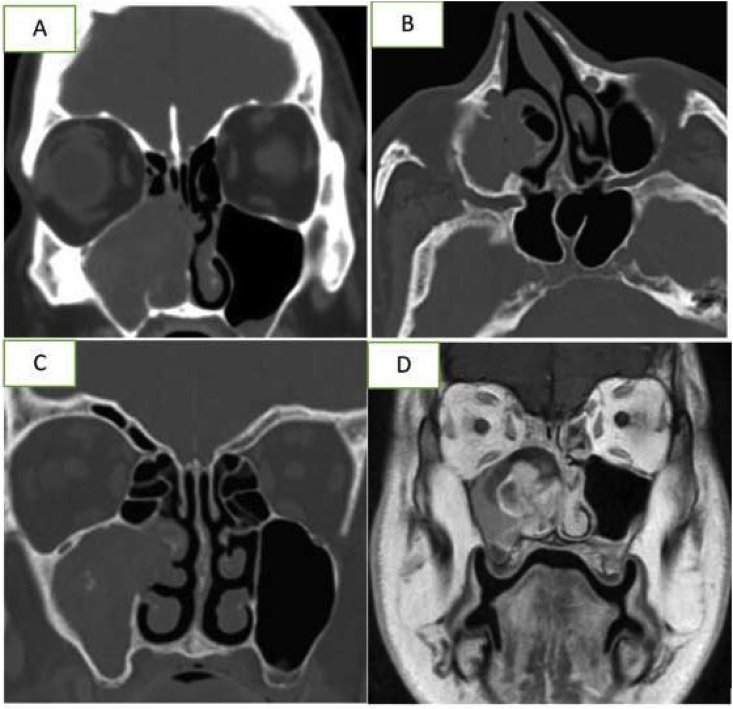
A 37-year-old male underwent right external dacryocystorhinostomy in 2007 for persistent epiphora associated with bilateral nasal obstruction and rhinorrhea. After 15 months no improvement of symptoms was observed, so the patient was referred to our hospital for right side recurrent epiphora. Post-saccular obstruction was diagnosed at probing and irrigation. The eye exam ruled out other causes of epiphora. Endoscopic examination of the nasal cavities showed bilateral nasal polyps with involvement of ostiomeatal complex and purulent rhinorrhea of uncertain etiology. Initially the patient was treated with systemic antibiotics and steroids for 10 days. A further endoscopic examination revealed an underlying right lateral nasal wall mass. This presented as a gray, firm, lobulated lesion filling the middle meatus suspicious for inverted papilloma. CT scan showed bilateral nasal fossa opacity and maxillary sinus opacity. In the right cavity, the mass was displacing the nasal septum towards the left side. MRI pointed out the radiological features of a local invasive mass (Fig. 3A–D). Finally, pathologic examination confirmed the diagnosis of inverted papilloma, a rare sinonasal tumor characterized by three features: a relatively strong potential for local destruction, high rate of recurrence, and a risk of carcinomatous evolution.14 The surgical approach consisted in endoscopic maxillectomy (removal of the medial wall of the right maxillary sinus), resection of the nasolacrimal duct and endonasal DCR.
Fig. 3.
Case 3 (A–B): CT scan showing the erosion of the middle wall of maxillary sinus and the hyperostosis of the inferior orbital wall as only peculiar sign. (C–D): MRI pointing out the characteristic features of inverted papilloma, including the convoluted pattern on contrast-enhanced T1 and T2-weighted images. This characteristic aspect is related to the alternating hypointense and hyperintense signal within the mass.
2.4. Case 4 (sinonasal inverted papilloma with synchronous squamous cell carcinoma)
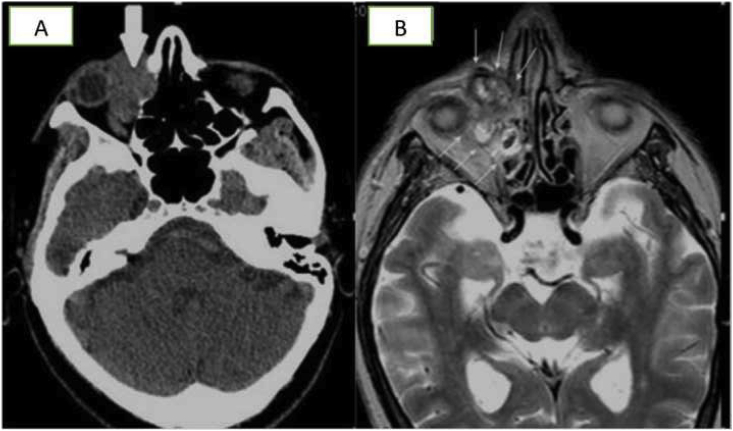
A 66-year-old woman presented to the ophthalmology department with long lasting unilateral epiphora recently worsen by a progressive right medial canthal mass and proptosis, previously misdiagnosed as mucocele. Post-saccular obstruction was detected at probing and irrigation. Endoscopic examination of the nasal cavities showed nonspecific edema of the right lateral nasal wall, resembling inflammation secondary to mucocele superinfection. CT and Gadolinum MRI scans revealed local extension to the paranasal sinuses up to the cribriform plate and orbit (Fig. 4A and B). The patient underwent lateral rhinotomy with orbitotomy. The orbital cavity was filled with a penduculated temporal muscle flap, covered with a dermo-epidermal skin graft (Thiersch grafts). The histological examination diagnosed a sinonasal inverted papilloma with synchronous squamous cell carcinoma. Synchronous carcinoma is a malignancy found in a mean of 7% of cases of inverted papilloma and is associated with a worse prognosis.15 The patient underwent adjuvant radiotherapy after surgery. In such condition life-long follow up is recommended.15
Fig. 4.
Case 4 (A) Non enhanced axial CT shows bone erosion of the papyracea lamina of ethmoid bone. (B) Axial T2 weighted sequence shows an extraconal and intraconal mass (white arrows) in the right orbit, with non-homogeneous hyperintensity ed irregular margins. The lesion involves the nasolacrimal canal, the papyracea lamina and the anterior ethmoid cells.
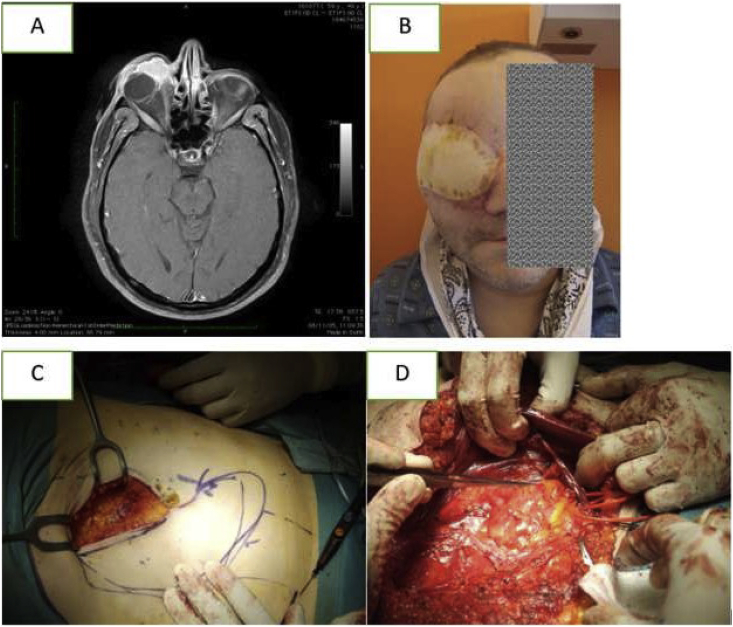
2.5. Case 5 (squamous cell carcinoma of the lacrimal sac)
A 55-year-old Iranian male was referred to our ophthalmology department a few weeks after external right DCR was performed at another hospital. He had been experiencing persistent unilateral right epiphora associated with recurrent conjunctival infections, recently complicated by a right medial canthus and eyelids swelling. Saccular obstruction was detected at probing and irrigation. Severe conjunctival chemosis was present. Endoscopic examination of the nasal cavities showed no signs of disease. CT scan and MRI revealed a primary lacrimal sac involvement with the mass extending to the right orbit (Fig. 5 A). An external biopsy of conjunctival mucosa diagnosed squamous cell carcinoma. Tumors of the lacrimal sac are rare but their recognition and early management are imperative, as they are locally invasive and potentially life-threatening. At present, a total of about 430 cases of primary malignant lacrimal sac tumor have been reported in the literature, with squamous cell carcinoma being the most common type.16 The patient underwent external craniofacial resection by lateral rhinotomy and orbitectomy. The orbital cavity was filled with a rectus abdominis free flap (Fig. 5B–D). A combination of adjuvant chemo and radiotherapy was administered. Sadly, the patient died two years later because of brain metastases.
Fig. 5.
Case 5 (A) T1-weighted MRI showing a mass involving the lacrimal sac and extending to the orbit. (B) 1-month follow-up appearance. (C–D) The orbital cavity was filled with a pedunculated flap of rectus abdominis through anastomosis with internal jugular vein and facial artery.
3. Discussion
Epiphora was the chief complaint shared by the diverse etiologies presented, underscoring the importance of ruling out conditions that may bear poor prognosis. Distinguishing mass related nasolacrimal duct obstruction from other conditions that present as persistent unilateral tearing relies on a high index of suspicion and the accuracy of thorough diagnostic work-up. The multidisciplinary approach changed the clinical history and the surgical strategy in all reported cases.
4. Conclusions
Masses are uncommon but not a rare cause of nasolacrimal duct obstruction and since they may bear a poor prognosis, it always seems to be worthwhile to undergo a thorough diagnostic work-up in order to rule them out. External and endonasal DCR procedures are equally effective in creating an alternative route for drainage of tears. The choice is up to surgeon's preference.17 Nevertheless, independent of the personal choice between these two procedures, surgical teams performing large numbers of dacryocystorhinostomies should be aware of such pathology and perform a systematic multidisciplinary approach.
Patient consent
Written consent to publish this case has not been obtained. This report does not contain any personal identifying information.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: ADM, FC, RP, LB, LM.
Acknowledgements
None.
References
- 1.Barry K., Jackson J., Williams K. The tearing patient. Elsevier Disease-a-Month. March 2017;63(3):68–71. doi: 10.1016/j.disamonth.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Nemet Arie Y. The etiology of epiphora: a multifactorial issue. Semin Ophthalmol. 2016;31(3):275–279. doi: 10.3109/08820538.2014.962163. [DOI] [PubMed] [Google Scholar]
- 3.Paulsen F. New insights into the pathophysiology of primary acquired dacryostenosis. Ophthalmology. 2001;108(12):2329–2336. doi: 10.1016/S0161-6420(01)00946-0. [DOI] [PubMed] [Google Scholar]
- 4.Yazici H., Bulbul E., Yazici A. Primary acquired nasolacrimal duct obstruction: is it really related to paranasal abnormalities? Surg Radiol Anat. 2015;37:579–584. doi: 10.1007/s00276-014-1391-6. [DOI] [PubMed] [Google Scholar]
- 5.Linberg J.V., McCormick S.A. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology. 1986;93:1055–1063. doi: 10.1016/s0161-6420(86)33620-0. [DOI] [PubMed] [Google Scholar]
- 6.Bartley G.B. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 2. Ophthalmic Plast Reconstr Surg. 1992;8:243–249. [PubMed] [Google Scholar]
- 7.Ginzkey C., Mlynski R. Die Behandlung von Tränenwegsstenosen aus HNO-ärztlicher Sicht. HNO. 2016;64(6):394–402. doi: 10.1007/s00106-016-0168-0. [DOI] [PubMed] [Google Scholar]
- 8.Weber R.K., Keerl R., Schaefer S.D., Rocca R.C. Springer; 2007. Atlas of Lacrimal Surgery. [Google Scholar]
- 9.Roos J., Ezra D., Rose G. ‘Preoperative imaging should be performed for all cases of acquired nasolacrimal duct obstruction’—No. Eye. 2017;31:349–350. doi: 10.1038/eye.2016.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dufour X., Kauffmann-Lacroix C., Ferrie J.C. Paranasal sinus fungus ball: epidemiology, clinical features and diagnosis. A retrospective analysis of 173 cases from a single medical center in France, 1989-2002. Med Mycol. 2006;44:61–67. doi: 10.1080/13693780500235728. [DOI] [PubMed] [Google Scholar]
- 12.Dufour X., Kauffmann-Lacroix C., Ferrie J.C. Paranasal sinus fungus ball and surgery: a review of 175 cases. Rhinology. 2005 Mar;43(1):34–39. [PubMed] [Google Scholar]
- 13.Lopez A., Tang S., Kacker A., Scognamiglio T. Demographics and etiologic factors of nasal pyogenic granuloma. Int Forum Allergy Rhinol. 2016;6:1094–1097. doi: 10.1002/alr.21781. [DOI] [PubMed] [Google Scholar]
- 14.Lisan Q., Laccourreye O., Bonfils P. Sinonasal inverted papilloma: from diagnosis to treatment, Elsevier Review. Eur Ann Otorhinolaryngol Head Neck Dis. November 2016;133(Issue 5):337–341. doi: 10.1016/j.anorl.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Mirza S., Bradley P.J., Acharya A., Stacey M., Jones N.S. Sinonasal inverted papillomas: recurrence, and synchronous and metachronous malignancy. J Laryngol Otol. 2007;121 doi: 10.1017/S002221510700624X. 09. [DOI] [PubMed] [Google Scholar]
- 16.Krishna Y., Coupland S.E. Lacrimal sac Tumours-a review. Asia Pac J Ophthalmol. 2017;6:173–178. doi: 10.22608/APO.201713. [DOI] [PubMed] [Google Scholar]
- 17.Jawaheer L., MacEwen C.J., Anijeet D. Endonasal versus external dacryocystorhinostomy for nasolacrimal duct obstruction. Cochrane Database Syst Rev. 2017;2(2) doi: 10.1002/14651858.CD007097.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]