Abstract
Background and Objectives
The purpose of this study was to identify risk and protective factors for abusive and neglectful behavior in the context of daily caregiving.
Research Design and Methods
Family caregivers who co-reside with a care recipient with Alzheimer’s disease and related dementia, recruited from social media, completed 21-days of diaries. Multilevel modeling with days (n = 831) nested within caregivers (N = 50) was used to evaluate relationships between hypothesized risk and protective factors and the odds of an abusive or neglectful behavior on a given day.
Results
Disruptions in the daily routine and stress of the caregiver related to behavioral symptoms of the care recipient are significant risk factors for abusive and neglectful behavior. Participating in a meaningful activity with the care recipient when it occurs twice in a day is a significant protective factor against use of a neglect behavior (OR = 0.19; CI 0.06–0.64; p = .01), but not for abusive behavior. Hypotheses that spending the full day together would increase risk, and that receipt of instrumental support and caregiver participation in self-care would decrease risk, were not supported.
Discussion and Implications
Findings demonstrate that risk of an abusive or neglectful behavior varies from day-to-day in the presence and absence of contextual factors, and that the majority of the variance in the odds an abusive or neglectful behavior occurring is related to day-level factors. Findings demonstrate that diary surveys are critical to identifying ecologically valid modifiable risk and protective factors for abusive and neglectful behaviors that can be targeted in future interventions.
Keywords: Elder mistreatment, Family caregiving, Dementia, Micro-longitudinal, Daily diary
The self-reported prevalence of engaging in abusive and neglectful behaviors among clinic samples of caregivers for persons with Alzheimer’s disease and related dementia (ADRD) is 47% (Wiglesworth et al., 2010). The centers for disease control (CDC) defines abusive and neglectful behaviors as intentional acts or failures to act by a caregiver, which causes or creates a risk of harm to an older adult, whether or not harm was the intended consequence (Hall, Karch, & Crosby, 2016). Importantly, the CDC definition focuses on the occurrence of the abusive or neglectful act, rather than its chronicity or perceived severity. Furthermore, the CDC definition does not qualify a behavior as abusive or neglectful based on whether or not it reaches a criminal threshold, but rather on the potential to cause harm. In the context of ADRD caregiving, environmental stressors (i.e., a single act of yelling) and unmet needs (i.e., skipping a single act of care) are suggested to cause and exacerbate symptoms of dementia (Algase et al., 2016; Hall & Buckwalter, 1987), a harmful outcome. As such, the caregiving context is important when considering the potential for harm. Furthermore, the CDC definition is consistent with the notion that quality of care is a spectrum with abusive and neglectful behavior representing the negative extreme (Phillips, Morrison, & Chae, 1990), and is not a binary concept. Caregivers can engage in both abusive and neglectful behaviors as well as adequate and exemplary ones (Christie et al., 2009). As such, it is important to understand contextual factors related to abusive and neglectful behavior to support caregivers in the ability to provide adequate and exemplary care.
A combination of non-modifiable factors (e.g., gender, relationship type, dementia status) and modifiable factors (e.g., stress, coping skills, social support) may increase the risk of caregivers engaging in abusive and neglectful behavior (Burnes et al., 2015; Fang & Yan, 2016). To date, research has focused on describing group-level characteristics of caregivers that self-report abusive and neglectful behavior (Wiglesworth et al., 2010). Thus, we have little knowledge about the context in which these behaviors occur, including when or how specific factors influence the risk of abusive or neglectful behavior in everyday life. In other words, although we have a growing body of knowledge on the “types of caregivers” who engage in abusive and neglectful behavior, little is known about the “types of situations” in which these behaviors occur. As such, this study seeks to understand the circumstances surrounding single episodes of abusive and neglectful behavior within the context of everyday caregiving experiences.
Identifying contextually based, or ecologically valid, intervention targets for complex behaviors requires an understanding of the behaviors in real-life environments (Robbins & Kubiak, 2014). An overreliance on global and retrospective measures (i.e., average stress over the last 6 months versus stress reaction related to a specific care task on a given day), especially in the absence of theory, can stagnate and mislead behavioral intervention development. Micro-longitudinal methods, such as daily diaries, capture ecologically valid experiences through intensive repeated measures investigating the covariation of feelings, situations, and behaviors (Scollon, Kim-Prieto, & Scollon, 2003). Application of this method can provide a more nuanced understanding of the variations in risk for and protection against abusive and neglectful behavior in the context of the daily experience of caregivers. This is significant given the evidence that aggregate group-level means do not accurately describe the individual experiences of dementia family caregivers, behavioral symptoms, and related stress (Fauth & Gibbons, 2014; Fauth, Zarit, Femia, Hofer, & Stephens, 2006), thus potentially introducing the ecological fallacy into intervention development research with this population.
Daily diaries have been used to examine the effects of daily caregiving experiences in ADRD (Zarit, Kim, Femia, Almeida, & Klein, 2014), and to understand daily experiences of intimate partner violence victims (Sullivan, McPartland, Armeli, Jaquier, & Tennen, 2012). However, this approach has not been applied to assess the circumstances for abusive and neglectful behavior by ADRD caregivers. Accordingly, this study seeks to fill this gap with the goal to guide future intervention development. The purpose of this micro-longitudinal study is to examine whether theoretically and empirically based factors increase or decrease the daily risk of engaging an abusive or neglectful behavior among family caregivers who co-reside with their ADRD care recipient.
The Effect of Daily Caregiving Experiences
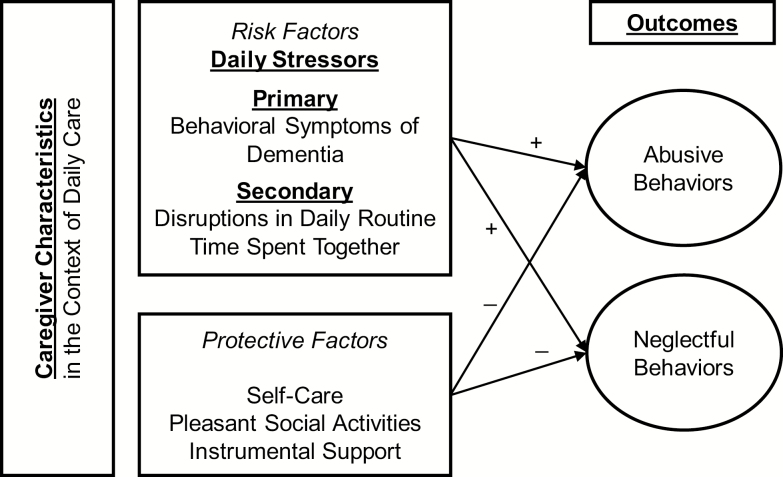
The leading explanation for abuse and neglect in caregiving is the caregiver burden theory, which is an extension of the stress-process model (Burnight & Mosqeuda, 2011; Pearlin, Mullan, Semple, & Skaff, 1990). Within the stress-process, there are four key domains including: background and situational context of stress, the primary and secondary stressors, the mediators of stress and the outcomes or manifestations of stress (Pearlin et al., 1990). The caregiver burden theory posits that abusive or neglectful behavior can be an outcome or manifestation of stress (Burnight & Mosqeuda, 2011). Furthermore, a basic premise of the stress-process model is that caregiver stress is not a singular phenomenon but rather emerges in light of an individual’s experiences, resources and situational context which is highly variable (Pearlin et al., 1990). As such, in the context of daily care, daily stressors (primary and secondary) found in different situational contexts increase the risk of abusive and neglectful behavior within caregiving. Likewise, there may also be protective factors found in different situational contexts which may mitigate the effect of stress or prevent stressors, reducing the likelihood of engaging in abusive or neglectful behavior. Therefore, from a stress-process model perspective the variability of daily experiences (i.e., situational contexts, stressors, protective factors) plays an important role in whether a caregiver engages in abusive or neglectful behavior on a given day (Figure 1).
Figure 1.
Stress-process model perspective of abusive and neglectful behavior within the context of daily caregiving.
There are daily experiences that contribute to stress in caregiving, which potentially increase risk of abusive or neglectful behavior. These daily experiences include primary stressors, related to the care needs of the person with dementia, and secondary stressors, related to role and intrapsychic strain (Pearlin et al., 1990). Caregiver stress related to behavioral symptoms of dementia (BSD) of the care recipient is a risk factor for which there is strong evidence (Fang & Yan, 2016), and a primary stressor within the stress-process model (Pearlin et al., 1990). One secondary stressor is related to the amount of time spent caregiving (Pinquart & Sörensen, 2003). Caregivers who provide more than 100 hr of care per month are more likely to report engaging in neglectful behavior (Beach & Schulz, 2017). Importantly, many caregivers report that even when they are not providing “hands on” care, they are still actively and continually monitoring and supervising their care recipient, perceiving they are “on duty” 24 hr a day (Mahoney, 2003), representing an intrapsychic strain. Thus, the amount of time spent together during the day may serve as a risk factor for abusive or neglectful behavior. Finally, disruptions to the daily routine is a commonly measured item in daily stress research (Almeida, Stawski, & Cichy, 2011), representing a secondary stressor related to role strain, which may serve as a stressor among caregivers and increasing the risk for abuse or neglect.
Given the variability in responses to stressors, the stress-process model maintains that certain factors may mediate the relationship between stressors and outcomes, primarily coping and social support (Pearlin et al., 1990). As such, a number of protective contextual factors may reduce the daily stress of caregiving and protect against risk of abusive or neglectful behavior. Social support, including receipt of instrumental support from others assists caregivers in their management of daily stressors (Pearlin et al., 1990). Engaging in self-care may be an effective coping strategy for some caregivers (Won, Fitts, Favaro, Olsen, & Phelan, 2008). in addition, the quality of the relationship between the caregiver and the care recipient modulates the stress response and has been linked to outcomes, ranging from caregiver depression to abuse and neglect (Quinn, Clare, & Woods, 2009; Williamson & Shaffer, 2001). Thus, participating in pleasant social activities that are not care-related to maintain the interpersonal relationship may modulate stress reactions related to care. These daily experiences may reduce stress and protect against abusive or neglectful behavior.
Variation in daily caregiving experiences allows us to examine links to abusive and neglectful behavior in real-life context. This also allows us to evaluate if there are etiological differences between abuse and neglect behavior as suggested by emerging evidence (Burnes et al., 2015; Fang & Yan, 2016). Thus, the purpose of this study is to identify risk and protective contextual factors for abusive and neglectful behavior, as suggested by the stress-process model. The following hypotheses were tested:
H1: Stress related to BSD, disruption in the daily routine of the caregiver, and amount of time spent together will increase the daily odds of an abusive or neglectful behavior.
H2: Caregiver participation in self-care activities, engagement in meaningful activities with care recipient, and receipt of instrumental support will decrease the daily odds of an abusive or neglectful behavior.
H3: Different patterns of risk/protection will emerge for abusive behaviors versus neglectful behaviors.
Methods
Participants
We used online strategies to recruit a convenience sample of self-identified caregivers age 21 years or older, who provide at least 4 hr of unpaid assistance each day to a family member with ADRD. The participants needed to co-reside with their care recipient, have reliable access to the internet, and live in the United States.
Facebook and Instagram were used to recruit participants from online support groups and paid targeted advertising. We followed established best practices for online recruitment to ensure legitimate participants, including disqualifying entries from duplicate IP addresses, repeating the eligibility screener at two different time points to ensure answers match using varied response options (e.g., asking age at time 1 and date of birth at time 2), externally validating eligibility answers (e.g., checking for accurate residential address using Google Earth), and prohibiting open access to the surveys (King, O’Rourke, & DeLongis, 2014; Kramer et al., 2014; Tarzia, Valpied, Koziol-McLain, Glass, & Hegarty, 2017; Teitcher et al., 2015).
Researchers have found Facebook to be an effective source for recruiting convenience samples of family caregivers as well as healthy older adults (Cowie & Gurney, 2018; Herbell & Zauszniewski, 2018). Though the generalizability of ADRD family caregivers recruited through Facebook is yet to be determined, generalizability of the participants is less of a concern when the research question seeks to explain individual differences rather than describe a population (King et al., 2014). Moreover, the greater concern for our research question is getting a representative sample of daily experiences through an appropriate duration of data collection (Hektner, Schmidt, & Csikszentmihalyi, 2007).
Procedure
Data collection occurred via online surveys sent to the participants’ verified E-mails. First, participants completed a baseline questionnaire. Then, they received diary surveys twice a day for 21 consecutive days. Diary surveys were sent at 7 am and 7 pm in the participant’s time zone. They asked about events in the previous 12-hr period. Participants were allowed to skip questions. Each survey took about 4.5 min to complete.
Participants had a 3-hr window to complete the diary survey (i.e., 7–10 am, 7–10 pm). We sent reminders to all participants who had not completed a diary at the 2- and 1-hr remaining mark. After 3 hr, the survey became unavailable. We limited the reporting window to limit recall bias.
Participants were compensated $40 for completing the baseline survey and $2 per diary they completed. Participants received the first $5 within 72 hr of completing the baseline survey, and the remaining compensation amount was paid after the 21-day diary component. Compensation amounts were not included in the online advertisements.
We took multiple steps to ensure that research data remained anonymous to the study staff given the sensitive nature of the questions. Enrollment information was kept in a separate file from the survey data. The daily surveys were set up so that each survey could be linked across time points, but not to identifying (i.e., enrollment) data. This anonymizing feature was programmed into the survey software to eliminate the need for a key to relink IDs to longitudinal data. At the end of each survey, participants were redirected to an online survey in a different platform and asked to enter their E-mail address so that the participant could be reimbursed. Keeping enrollment, survey, and participant reimbursement information in separate databases allowed the survey responses to remain anonymous at all times. All study procedures were approved by the University’s Institutional Review Board as exempt.
Measures
The outcomes of interest were days on which an abusive or neglectful behavior occurred. On each survey, participants reported if they engaged in an abusive or neglectful behavior in the 12-hr time frame with yes/no response options. To test the study hypotheses, we combined data from two 12-hr periods to the day-level to examine the frequency (count of the variable presence that day including none, once a day, twice a day) of daily contextual factors.
Abusive behaviors
Abusive behaviors were measured with six items about psychological aggression and physical aggression from the revised Conflict Tactics Scale (CTS2) (Straus, Hamby, Boney-McCoy, & Sugarman, 1996). The CTS2 is valid and reliable tool in elder abuse and neglect research used for family caregiver to self-report abusive behaviors (Cooper, Maxmin, Selwood, Blanchard, & Livingston, 2009; Fang & Yan, 2017; Kishimoto et al., 2013; Wiglesworth et al., 2010). We combined both physical and psychological aggression for this measure since at the day-level, physical aggression rarely occurs in isolation and is more likely to co-occur with psychological aggression. We coded days with “abuse present” if participants endorsed at least one of the following behaviors on a given day: shouting or yelling, insulting or swearing, pushing or shoving, grabbing the person with ADRD, throwing things, or stomping out of the room in disagreement.
Neglectful behaviors
Neglectful behaviors were measured with three items. One item assessed failure to provide needed care for activities of daily living (ADLs). A second item measured skipping oral care. Not receiving help with ADLs even though it is needed is a common method of measuring neglect (Burnes et al., 2015). A third item asked about any other action that made the participant feel guilty or embarrassed afterwards. It had an optional free response to describe the “guilty” action, in which answers were reviewed for face validity. Failing to provide supervision even though it was needed was the most frequent answer for this item. We coded days with “neglect present” if a caregiver endorsed any of the following behaviors on a given day: skipping a care activity or not providing help even though the ADRD care recipient needed it, skipping oral care, or any other action that made them feel guilty or embarrassed afterwards.
Risk and protective contextual factors for abusive and neglectful behavior were chosen in alignment with the stress-process model, representing either primary and secondary stressors (risk factors), or mediators (protective factors) known to be related to the stress-process in ADRD caregiving. The hypothesized risk factors (BSD-related stress, disruptions in care recipient’s routine, amount of time spent together) and protective factors (engaging in self-care, participation in pleasant social activities, receipt of instrumental support) were selected as they were likely to vary on a day-to-day basis. These factors were measured as follows:
BSD-related stress. Participants reported their stress level when they observed any of nine possible BSD. Six BSD items mirrored the CTS2 to capture physically and psychologically aggressive BSD: if the person with ADRD pushed/shoved, grabbed, threw something, insulted, shout/yelled at them, or stomped out of the room in disagreement. To capture non-aggressive agitation, three items asked about resisting care and repetitive activities from the Neuropsychiatric Inventory (Cummings et al., 1994) and any other inappropriate behaviors. Participants rated their stress related to BSD on a 7-point scale, ranging from 1 (not at all stressful) to 7 (extremely stressful). Days with no BSD were assigned a zero. We computed the average score of the stress across the nine BSD items for each participant for each in the 24-hr period.
Disruptions in daily routine. Unexpected events and disruptions to daily routines were captured with the following question: “Did anything out of the ordinary or not part of your normal daily routine happen whether it was positive or not (e.g., a household member became sick, doctor’s appointment, friends came over)?” We coded days as having no disruptions, one, or two in the 24-hr period.
Spending all day together. Participants reported how many hours they spent in the same physical location as the care recipient regardless of whether or not they were providing care. Owing to the bimodal distribution, we coded days as “24 hr spent together” or “less than 24 hr spent together.”
Engaging in self-care. Participants reported if they “got to spend some time doing a relaxing activity or something that was just for your own enjoyment.” We coded days as having none, one, or two instances of self-care in the 24-hr period.
Participating in pleasant social activities. Participants reported if they had a pleasant or meaningful social interaction with the care recipient. We coded days as having none, one, or two instances of meaningful connection in the 24-hr period.
Receipt of instrumental support. Participants indicated if they had help from someone else in caring for or supervising the care recipient with ADRD. We coded days as having none, one, or two instances of support from others in the 24-hr period.
Additional variables
Demographic information was collected at enrollment including age, gender, race/ethnicity, employment, education, and relationship to the care recipient. We included whether or not the caregiver received any amount of paid assistance with a yes/no question. Caregiver burden was calculated using the level of care index from the AARP Caregiver Report, which assigns points based on hours of care provided a day and assistance with different numbers of ADLs and instrumental activities of daily living (National Alliance for Caregiving & American Association of Retired Persons, 2015). Premorbid relationship quality was measured using the Mutual Communal Behaviors Scale, which asks the caregiver to rate the types of interactions they had with the care recipient prior to the onset of illness. The 10-item scale scores in a range from 20 to 40 with higher scores indicating greater mutual responsiveness (α = 0.88) (Williamson & Schulz, 1995). Depression severity of the caregiver participant was measured with the Patient Health Questionnaire (PHQ-9) (sensitivity = 0.80 and specificity 0.92 major depressive disorder) (Gilbody, Richards, Brealey, & Hewitt, 2007; Kroenke, Spitzer, & Williams, 2001).
Analysis
Evaluation of Missing Data
A total of 50 participants completed surveys two times a day over 21 consecutive days. Aggregating data on day-level resulted in 831 daily observations and 20% missing data (of 1,050 possible observations). On average, each participant provided 16 days of data. As there were no substantial differences in missingness between observations by independent variables or covariates, we assumed that data were missing completely at random. This assumption allowed us to run analyses using a list-wise deletion approach for handling missing data, without biasing estimates (Little & Rubin, 2014; Rubin, 2004).
Multilevel Modeling of Diary Data
We examined characteristics that increase odds of engaging in an abusive or neglectful behavior on a given day using generalized two-level mixed models. SAS PROC GLIMMIX used adaptive Gauss–Hermite quadrature rule with marginal log likelihood to account for clustering of daily responses from participants (Ene, Leighton, Blue, & Bell, 2015). The random effects component consisted of a random intercept (i.e., we assumed that participants varied in their odds of engaging in abusive or neglectful behaviors) and an autoregressive covariance structure, a common structure for daily diary data (Rovine & Walls, 2006).
The fixed-effects component included level-1 (day-level) predictors and level-2 (person-level) covariates. The level-1 predictors included BSD-related stress, time spent together, disruption in routine of the care recipient, presence of instrumental support and caregiver engagement in self-care. BSD-related stress rating was person-mean centered to account for deviations from person’s average stress level. This is consistent with other studies that examine contextual effects of stress to account for within-person variance (Hoffman & Stawski, 2009).
At level-2 (person-level), we controlled for age, relationship status, months of caregiving, and months since ADRD diagnosis, as covariates. We did not include gender and ethnicity, as they were not significantly associated with abusive or neglectful behaviors in our sample. Our strategy was to generate a parsimonious fixed-effects component, so we deleted nonsignificant predictors and retained significant predictors. We report both full and trimmed models. Models were estimated for abusive behaviors and neglectful behaviors separately to test our third hypothesis.
Results
Caregiver demographics are shown in Table 1. On average, participants were women caring for a parent for 15 hr a day. Participants tended to report a high level of caregiver burden. Within-person averages for each contextual factor are shown in Table 2. Most participants (74%, N = 37/50) reported at least one day on which they engaged in an abusive or neglectful behavior with most common being psychological aggression (64% of participants) followed by neglect (50%) and physical aggression (12%). Across the 21 observation days, participants reported an average of 3.6 (SD = 3.5) days with abusive behavior and 2.7 (SD = 2.5) days with neglectful behavior. The majority of days did not have any abusive or neglectful behavior. On 20% of days (n = 152/746) when these behaviors occurred, psychological aggression was most frequent (13% of days) followed by neglect (9%) and physical aggression (2%).
Table 1.
Characteristics of Caregivers (N = 50). ADRD = Alzheimer’s disease and related dementia
| Mean ± SD (range) or % | |
|---|---|
| Caregiver characteristics | |
| Age | 53 ± 11 (26–73) |
| Female | 93% |
| White | 87% |
| Hispanic | 14% |
| Relationship | |
| Child | 60% |
| Spouse | 29% |
| Othera | 11% |
| Years since ADRD diagnosis | 4.2 ± 2.6 (0.4–10) |
| Years of being caregiver | 3.8 ± 2.7 (0.4–12) |
| Employment | |
| Employed | 35% |
| Unemployed | 31% |
| Retired | 31% |
| Student | 2% |
| Education | |
| Less than high school | 2% |
| High school or GED | 22% |
| Some college | 28% |
| 4-year college degree | 30% |
| Professional degree | 14% |
| Receive paid care/assistance | 29% |
| High caregiver burden | 91% |
| Mutual Communal Behaviors Scaleb | 31 ± 5 (20–40) |
| Depression | |
| Mild | 39% |
| Moderate | 22.9% |
| Severe | 12.5% |
| Suicidal ideation past 2 weeks | 8.3% |
Note: a“other” category includes “daughter-in-law” and “other.”
bHigher scores indicate greater mutual responsiveness in premorbid relationship.
Table 2.
Daily Contextual Factors Co-occurring With Abusive or Disruptive Behavior. BSD = behavioral symptoms of dementia
| Average per person | Abusive behavior | Neglectful behavior | |
|---|---|---|---|
| Person-centered BSD-stress | 0 | 0.75 | 0.59 |
| Days per person (mean ± SD) | Abusive behavior (mean ± SD) | Neglectful behavior (mean ± SD) | |
| Disruptions in routine | |||
| None | 10.28 ± 5.63 | 2.11 ± 2.22 | 1.48 ± 1.90 |
| Once a day | 3.84 ± 3.32 | 1.40 ± 2.17 | 1.00 ± 1.26 |
| Twice a day | 0.74 ± 1.23 | 0.17 ± 0.51 | 0.28 ± 0.68 |
| Meaningful activity | |||
| None | 4.60 ± 5.11 | 1.56 ± 2.34 | 1.04 ± 1.62 |
| Once a day | 6.02 ± 3.59 | 1.50 ± 1.87 | 1.48 ± 1.64 |
| Twice a day | 4.26 ± 4.94 | 0.53 ± 0.91 | 0.24 ± 0.60 |
| Instrumental support | |||
| None | 8.26 ± 7.50 | 2.03 ± 2.92 | 1.28 ± 1.99 |
| Once a day | 4.16 ± 4.08 | 0.83 ± 1.06 | 0.68 ± 0.99 |
| Twice a day | 2.50 ± 4.34 | 0.78 ± 2.02 | 0.80 ± 1.61 |
| Engaging in self-care | |||
| None | 5.56 ± 5.16 | 1.42 ± 2.09 | 0.80 ± 1.19 |
| Once a day | 5.62 ± 3.56 | 1.36 ± 1.88 | 1.20 ± 1.44 |
| Twice a day | 3.74 ± 5.00 | 0.86 ± 1.64 | 0.76 ± 1.20 |
| Together all day | 8.2 ± 6.1 | 2.4 ± 2.3 | 1.5 ± 0.8 |
| Abuse | 3.6 ± 3.5 | — | 2.5 ± 2.1 |
| Neglect | 2.7 ± 2.5 | 2.5 ± 2.1 | — |
Note: Person-centered stress reflects a point difference from person’s average level of stress centered at zero. Original BSD-related stress can range from 1 “no stress” to 7 “extreme stress”.
Effect of Contextual Factors on Abusive and Neglectful Behaviors
To examine variance in the outcome, we calculated the intraclass correlation coefficient (ICC) from intercept and residual variance components. Preliminary analysis with the empty model for daily abusive behaviors revealed an ICC of 0.35, indicating 35% of the variance was at the between-person level and 65% was within-person (i.e., day-to-day). For neglectful behaviors, ICC was 0.4, indicating 40% of the variance was at the between-person level and 60% was within-person. These data indicate that a substantial amount of the variance in odds of engaging in abusive and neglectful behavior on a given day is driven the daily context.
Risk
Our linear mixed effects model (Table 3) shows that daily BSD-related stress is significantly associated with the odds of engaging in abusive or neglectful behavior on a given day. Increase from a person’s baseline in BSD-related stress significantly increases the risk of both abusive and neglectful behaviors. BSD-related stress has a stronger association with abusive (OR = 1.92; CI 1.56–2.37; p = .001) than with neglectful behaviors (OR = 1.42; CI 1.14–1.77; p = .001). This suggests, for example, if a caregiver usually perceives BSD as moderately stressful (score of 4), then on days that they perceive BSD as very stressful (score of 5) they are 92% more likely to engage in an abusive behavior. However, in this same situation (i.e., a 1-point increase in stress) they are 42% more likely to engage in a neglectful behavior.
Table 3.
Effect of Daily Context on the Odds of Abusive or Neglectful Behavior. BSD = behavioral symptoms of dementia
| Daily contextual factors | Abusive behaviora | Neglectful behavior | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Person-centered BSD-stress | 1.92 | [1.56–2.37] | .001 | 1.42 | [1.14–1.77] | .001 |
| Disruption in routine | ||||||
| Once a day | 2.35 | [1.31–4.22] | .001 | 1.69 | [0.87–3.28] | |
| Twice a day | 1.43 | [0.44–4.65] | 5.14 | [1.51–17.47] | .01 | |
| Meaningful activity | ||||||
| Once a day | 0.81 | [0.43–1.55] | 0.88 | [0.42–1.86] | ||
| Twice a day | 0.72 | [0.30–1.73] | 0.19 | [0.06–0.64] | .01 | |
| Instrumental support | ||||||
| Once a day | 1.85 | [0.71–4.84] | 1.66 | [0.59–4.67] | ||
| Twice a day | 0.77 | [0.34–1.74] | 1.05 | [0.44–2.50] | ||
| Engaging in self-care | ||||||
| Once a day | 0.70 | [0.31–1.60] | 1.26 | [0.59–2.69] | ||
| Twice a day | 0.70 | [0.31–1.60] | 2.20 | [0.85–5.69] | ||
| Together all day | 0.72 | [0.35–1.47] | 1.74 | [0.70–4.34] |
aWe compared a model with all six items for abusive behavior outcome to a model that excluded “stomping out of the room” from the outcome, which revealed no statistical or practically meaningful differences.
Disruption in care recipient’s daily routine is a significant risk factor for both abusive and neglectful behaviors. However, the frequency of disruption (whether it occurred once or twice that day) has a distinct effect. One instance of disruption more than doubles the odds of an abusive behavior in the same day (OR = 2.35; CI 1.31–4.22; p = .001). Disruption significantly increases odds of a neglectful behavior by more than 5, but only when it happens twice in a day (OR = 5.14; CI 1.51–17.47; p = .01).
Spending all day (i.e., 24 hr) together with the care recipient did not significantly increase the odds of engaging in either abusive or neglectful behaviors.
Protective factors
Participation in meaningful activities has a protective effect on neglectful but not abusive behaviors. The frequency of protective activities matters as well. If the caregiver had a meaningful non-care-related interaction with their care recipient twice in one day, they are 20% less likely to engage in neglectful behaviors (OR = 0.19; CI 0.06–0.64; p = .01). Meaningful non-care activities do not significantly affect the odds of abusive behavior on a given day.
Neither receiving instrumental support nor engaging in self-care activities by the caregiver significantly reduced the odds of either abusive or neglectful behavior on the same day.
Discussion
This study is among the first micro-longitudinal investigations of abusive and neglectful behavior in ADRD family caregiving. It makes a significant contribution by demonstrating that the risk of engaging in these behaviors varies from day-to-day in the presence of contextual factors. Moreover, the ICC, a measure of variability, in the use of abusive and neglectful behavior demonstrates that greater variance is at the day level rather than person level. When data are measured on a person level, such as in studies comparing groups of abusive and non-abusive caregivers, the analysis fails to capture the day-to-day variation in the context and the outcome. Such inferences lead to assumptions that group characteristics apply consistently to individuals regardless of their daily experiences. This could be the reason that interventions designed to reduce abuse and neglect in ADRD family caregiving have failed despite targeting “known” population risk factors (Cooper, Barber, Griffin, Rapaport, & Livingston, 2016).
This study is also among the first to evaluate the multiple domains of the stress-process model in relation to the outcome of abusive and neglectful behavior. Consistent with the model assumptions, our findings show that different situational contexts, stressors and protective factors do affect the outcomes of stress by either increasing or decreasing risk of abusive or neglectful behavior. With that, although all the variables measured were chosen because of prior research showing their relevance to the stress-process model, not all were significant contributors the outcome. This suggests while the stress-process model does have some explanatory power in the outcomes of abusive and neglectful behavior more research is needed to identify exactly which situational contexts, stressors and protective factors are most relevant to these outcomes. Furthermore, the stress-process model posits protective factors have a mediating role, rather than a direct relationship, with the outcomes. This is an area of exploration for future research with larger sample sizes.
For our first hypothesis, only BSD-stress among caregivers and disruptions in the daily routine significantly increased risk of both abusive and neglectful behaviors. Our findings are consistent with others who reported correlations between caregiver stress and increased risk of abuse and neglect (Yan & Kwok, 2011). Spending all day together with the care recipient did not significantly affect the odds of engaging in either abusive or neglectful behaviors. Future studies with larger samples might have greater variation in responses and can examine whether there is a “tipping point” in the number of hours spent together that increases the odds of an abusive or neglectful behavior, and if there is a difference between the total time spent together compared to the amount of time providing care.
For the second hypothesis, the caregivers’ participation in pleasant social activities with the care recipient was the only significant protective factor. Others have reported that social support, including instrumental support with caregiving activities, is protective against abuse and neglect within caregiving (Yan & Kwok, 2011). A strength of micro-longitudinal methods is that it can uncover temporal proximity of related factors (Hektner et al., 2007). As such, the protective effect found in other studies may be due to characteristics of the people who receive instrumental support, rather than the actual receipt of support itself, as suggested by our data measured in near-real-time. In addition, others suggest perceived social support has a clinically significant impact on caregiving outcomes whereas actual social support does not (Del-Pino-Casado, Frias-Osuna, Palomino-Moral, Ruzafa-Martinez, & Ramos-Morcillo, 2018). This may also be true for risk of abusive and neglectful behaviors, suggesting that interventions to increase perceptions of social support such as cognitive restructuring is important. Finally, it may be that instrumental support, if sporadically or inconsistently provided, creates a disruption in the daily routine, which in turn increases the risk.
Engaging in a self-care activity among caregivers did not affect the odds of abusive or neglectful behavior. The stress-process model suggests coping skills, such as self-care acts, can serve as mediators by reducing the impact of stress on the outcome. As stress is related to risk of engaging in abusive and neglectful behaviors within caregiving, it was hypothesized self-care would reduce the risk. Importantly, we measured perceptions of self-care rather than specific types of self-care activities so it could be that the type of self-care activity matters. This finding also suggests that other factors related to stress, such as emotion reactivity and regulation (Moskowitz et al., 2019), may be more important than simply self-care or stress-reduction.
For the third hypothesis, our findings are consistent with others who have suggested abusive and neglectful behaviors may be driven by different casual mechanisms (Burnes et al., 2015). We found notable differences in risk and protective factors. First, the dosage for disruption to routines affected odds of engaging in abusive versus neglectful behaviors differently, with one event increasing odds for abuse while two events increased odds for neglect. We measured disruptions regardless of whether they were perceived as a negative or positive event. Future research could examine whether a specific type of disruption is most important to the risk of abusive or neglectful behavior.
n addition, participation in pleasant social activities played a protective role against neglectful, but not abusive behaviors. The lack of a protective relationship for abusive behaviors may be because of the type of pleasant social activity the caregiver planned was inappropriate for a person with dementia (thus potentially escalating stress and BSD), even if it would have been something the person with dementia enjoyed prior to the disease. More research on pleasant social activities as a protective factor for abusive behaviors is needed. Educational interventions on planning an appropriate activity may be warranted, such as that offered by the REACH intervention program (Gitlin et al., 2003). Interestingly, for neglectful behaviors, participation in pleasant social activities was only protective when it occurred twice a day. It could be that those caregivers who plan for multiple activities in a day have a better relationship quality with their care recipient or are more committed to the caregiver role and thus less likely to engage in neglectful behaviors. It may also be that the type of activity the caregiver planned helped to decrease isolation. Future research should explore in more detail non-care-related interactions between caregivers and care recipients, types of recreational or leisure activities the dyad engages in, and ways in which daily relationship quality affects risk of abusive and neglectful behaviors.
We examined risk and protective factors for co-residing family members to engage in abusive or neglectful behavior on a given day of caregiving for a person with ADRD. Our approach, focusing on individual differences and understanding factors leading to abusive and neglectful behaviors, is novel as to date the field has focused on population-based estimates of chronic abuse and neglect, and risk factors being an abusive caregiver (rather than for abusive behaviors). These studies of chronic abuse and neglect define “case-ness” by counting abuse and neglect as present if a respondent indicates a certain number of abusive or neglectful behaviors occurred over a certain period of time (Dong, 2014). For comparison purposes, if the rate of abusive and neglectful behaviors in our sample were to remain stable over the course of a year, than the average participant in this study will have had 60 episodes in which they engaged in an abusive behavior and 47 episodes in which they engaged in a neglectful behavior, which would achieve the “case-ness” criteria of these previous studies.
Strengths and Limitations
The primary strength of the study is the daily tracking of behaviors using daily surveys which reduces recall bias and increases ecological validity. The micro-longitudinal method provided a large sample size for robust analyses of the daily contextual variables. As such, this study demonstrates that not only are diary studies feasible among ADRD family caregivers but that studying abusive and neglectful behaviors in the context of daily life can help expand our understanding of risk and protective factors as well as their casual mechanisms. This methodology is feasible and safe, as we did not see rates of adverse behaviors increase during the 21-day duration. In fact, participants provided unsolicited feedback thanking the research team for the opportunity to participate in this study.
The primary limitation of the study is that analyses were limited by the person-level sample size (N = 50). This means that hypotheses on how caregiver characteristics influence odds of abusive or neglectful behavior either directly or through interactions with day-level predictors could not be tested. A second limitation is the lack of racial diversity in the sample, particularly among African American and Asian American participants. In the future, targeted recruitment methods are needed to effectively recruit these two racial groups using social media.
Finally, an additional limitation of the study, which is not unique to this study but rather an issue the field has yet to address, relates to the measurement of neglect and the lack of knowledge on how caregivers provide care (i.e., the care processes they use and decision they make in light of competing demands and situational contexts). As such, although the neglectful behaviors measured in this study had the potential to increase harm to the care recipient, it is not known if these were deliberate decisions within the care process. For example, within professional nursing care, in light of competing demands and limited resources, nurses engage in prioritized decision making around which care activities have the greatest impact on patient health, resulting in “missed care” or “intentionally rationed care” (Jones, Hamilton, & Murry, 2015). Within informal family caregiving these same behaviors have largely been labeled as “neglect.” Although the rationale behind the behavior doesn’t reduce the risk of harm, nor should it legitimize the acceptability of using abusive or neglectful actions against a care recipient with dementia, it points to the need to better understand how abusive and neglectful behaviors fit into the bigger picture of care processes for family caregiving to ensure more valid measurement and more relevant intervention responses to support caregivers in providing high quality and safe care.
Implications
Our findings address a critical issue of examining contextual-level predictors of abusive or neglectful behavior among family caregivers of persons with ADRD. This study highlights several areas of future research. First, given the lack of theory on elder abuse and neglect within caregiving the measures selected were related to the stress-process model. As our analyses only found some of the hypothesized risk and protective factors to be significant, future research needs more detailed assessments of daily context including more factors known to influence risk within other areas of family violence (e.g., alcohol use, coping skills) and other theories (e.g., social learning theory). Future research should also explore other known factors important for successful caregiving outcomes such as self-efficacy and confidence in caregiving tasks (Gallagher et al., 2011). With larger sample sizes, future studies should examine the impact of time in relation to the daily contextual risk/protective factors (e.g., does a higher-then-normal stress rating have a lagged-effect on the odds of engaging in an abusive or neglectful behavior the next day?). Finally, it is also important for future studies to examine how changes in personal stressors (e.g., depression, financial strain) develop over time and their potential interaction with day-level contextual factors to increase likelihood of engaging in an abusive or neglectful behavior. Together, these different avenues of research will help to produce more ecologically valid risk/protective factors and guide development of a comprehensive framework for prevention of abuse and neglect in ADRD family caregiving.
Funding
Support for this work was provided by University of Texas Health Science Center at San Antonio.
Conflict of Interest
None reported.
References
- Algase D. L., Beck C., Kolanowski A., Whall A., Berent S., Richards K., & Beattie E (2016). Need-driven dementia-compromised behavior: An alternative view of disruptive behavior. American Journal of Alzheimer’s Disease, 11, 10–19. doi: 10.1177/153331759601100603 [DOI] [Google Scholar]
- Almeida D. M., Stawski R. S., & Cichy K. E (2011). Combining checklist and interview approaches for assessing daily stressors: The daily inventory of stressful events. In Contrada R. J. & Baum A. (Eds.), Handbook of stress science: biology, psychology, and health (pp. 583–595). New York, NY: Springer Publishing. [Google Scholar]
- Beach S. R., & Schulz R (2017). Family caregiver factors associated with unmet needs for care of older adults. Journal of the American Geriatrics Society, 65, 560–566. doi: 10.1111/jgs.14547 [DOI] [PubMed] [Google Scholar]
- Burnes D., Pillemer K., Caccamise P. L., Mason A., Henderson C. R. Jr, Berman J., . . . Lachs M. S (2015). Prevalence of and risk factors for elder abuse and neglect in the community: A population-based study. Journal of the American Geriatrics Society, 63, 1906–1912. doi: 10.1111/jgs.13601 [DOI] [PubMed] [Google Scholar]
- Burnight K. & Mosqeuda L (2011). Theoretical model development in elder mistreamtnet; Final report submitted to the National Institute of Justice, grant number 2005-IJ-CX-0048 Retrieved from https://www.ncjrs.gov/pdffiles1/nij/grants/234488.pdf
- Christie J., Smith G. R., Williamson G. M., Lance C. E., Shovali T. E., & Silva L. C (2009). Quality of informal care is multidimensional. Rehabilitation Psychology, 54, 173–181. doi: 10.1037/a0015705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper C., Barber J., Griffin M., Rapaport P., & Livingston G (2016). Effectiveness of START psychological intervention in reducing abuse by dementia family carers: Randomized controlled trial. International Psychogeriatrics, 28, 881–887. doi: 10.1017/S1041610215002033 [DOI] [PubMed] [Google Scholar]
- Cooper C., Maxmin K., Selwood A., Blanchard M., & Livingston G (2009). The sensitivity and specificity of the Modified Conflict Tactics Scale for detecting clinically significant elder abuse. International Psychogeriatrics, 21, 774–778. doi: 10.1017/S1041610209009387 [DOI] [PubMed] [Google Scholar]
- Cowie J. M. & Gurney M. E (2018). The use of Facebook advertising to recruit healthy elderly people for a clinical trial: Baseline metrics. JMIR Research Protocols, 7, e20. doi: 10.2196/resprot.7918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J. L., Mega M., Gray K., Rosenberg-Thompson S., Carusi D. A., & Gornbein J (1994). The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology, 44, 2308–2314. doi: 10.1212/wnl.44.12.2308 [DOI] [PubMed] [Google Scholar]
- Del-Pino-Casado R., Frias-Osuna A., Palomino-Moral P. A., Ruzafa-Martinez M., & Ramos-Morcillo A. J.(2018). Social support and subjective burden in caregivers of adults and older adults: A meta-analysis. PLoS One, 13, e0189874. doi: 10.1371/journal.pone.0189874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X. (2014). Do the definitions of elder mistreatment subtypes matter? Findings from the PINE Study. The Journal of Gerontology, Series A: Biological Sciences and Medical Sciences, 69(Suppl 2), S68–75. doi: 10.1093/gerona/glu141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ene M., Leighton E. A., Blue G. L., & Bell B. A. (2015, November). Multilevel models for categorical data using SAS® PROC GLIMMIX: The basics. SAS Global Forum 2015 Proceedings, Document no. 3430–2015. Retrieved from http://support.sas.com/resources/papers/proceedings15/3430-2015.pdf [Google Scholar]
- Fang B. & Yan E (2016). Abuse of older persons with dementia: A review of the literature. Trauma, Violence, and Abuse, 19, 127–147. doi: 10.1177/1524838016650185 [DOI] [PubMed] [Google Scholar]
- Fang B. & Yan E (2017). Abuse of older persons with cognitive and physical impairments: Comparing percentages across informants and operational definitions. Journal of Interpersonal Violence, 088626051774215. doi: 10.1177/0886260517742150 [DOI] [PubMed] [Google Scholar]
- Fauth E. B. & Gibbons A (2014). Which behavioral and psychological symptoms of dementia are the most problematic? Variability by prevalence, intensity, distress ratings, and associations with caregiver depressive symptoms. International Journal of Geriatric Psychiatry, 29, 263–271. doi: 10.1002/gps.4002 [DOI] [PubMed] [Google Scholar]
- Fauth E. B., Zarit S. H., Femia E. E., Hofer S. M., & Stephens M. A (2006). Behavioral and psychological symptoms of dementia and caregivers’ stress appraisals: Intra-individual stability and change over short-term observations. Aging and Mental Health, 10, 563–573. doi: 10.1080/13607860600638107 [DOI] [PubMed] [Google Scholar]
- Gallagher D., Ni Mhaolain A., Crosby L., Ryan D., Lacey L., Coen R. F., . . . Lawlor B. A (2011). Self-efficacy for managing dementia may protect against burden and depression in Alzheimer’s caregivers. Aging and Mental Health, 15, 663–670. doi: 10.1080/13607863.2011.562179 [DOI] [PubMed] [Google Scholar]
- Gilbody S., Richards D., Brealey S., & Hewitt C (2007). Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): A diagnostic meta-analysis. Journal of General Internal Medicine, 22, 1596–1602. doi: 10.1007/s11606-007-0333-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin L. N., Belle S. H., Burgio L. D., Czaja S. J., Mahoney D., Gallagher-Thompson D., … Ory M. G.; REACH Investigators (2003). Effect of multicomponent interventions on caregiver burden and depression: The REACH multisite initiative at 6-month follow-up. Psychology and Aging, 18, 361–374. doi: 10.1037/0882-7974.18.3.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall G. R. & Buckwalter K. C (1987). Progressively lowered stress threshold: A conceptual model for care of adults with Alzheimer’s disease. Archives of Psychiatric Nursing, 1, 399–406. [PubMed] [Google Scholar]
- Hall J. E., Karch D. L., & Crosby A. E (2016). Elder abuse surveillance: Uniform definitions and recommended core data elements for use in elder abuse surveillance, version 1.0 Retrieved from Altanta, GA: http://www.cdc.gov/violenceprevention/pdf/ea_book_revised_2016.pdf [Google Scholar]
- Hektner J. M., Schmidt J. A., & Csikszentmihalyi M (2007). Experience sampling method: Measuring the quality of everyday life. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Herbell K. & Zauszniewski J. A (2018). Facebook or Twitter?: Effective recruitment strategies for family caregivers. Applied Nursing Research, 41, 1–4. doi: 10.1016/j.apnr.2018.02.004 [DOI] [PubMed] [Google Scholar]
- Hoffman L. & Stawski R. S (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6, 97–120. doi: 10.1080/15427600902911189 [DOI] [Google Scholar]
- Jones T. L., Hamilton P., & Murry N (2015). Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. International Journal of Nursing Studies, 52, 1121–1137. doi: 10.1016/j.ijnurstu.2015.02.012 [DOI] [PubMed] [Google Scholar]
- King D. B., O’Rourke N., & DeLongis A (2014). Social media recruitment and online data collection: A beginner’s guide and best practices for accessing low-prevalence and hard-to-reach populations. Canadian Psychology/Psychologie Canadienne, 55, 240–249. doi: 10.1037/a0038087 [DOI] [Google Scholar]
- Kishimoto Y., Terada S., Takeda N., Oshima E., Honda H., Yoshida H., . . . Uchitomi Y (2013). Abuse of people with cognitive impairment by family caregivers in Japan (a cross-sectional study). Psychiatry Research, 209, 699–704. doi: 10.1016/j.psychres.2013.01.025 [DOI] [PubMed] [Google Scholar]
- Kramer J., Rubin A., Coster W., Helmuth E., Hermos J., Rosenbloom D., . . . Lachowicz M (2014). Strategies to address participant misrepresentation for eligibility in web-based research. International Journal of Methods in Psychiatric Research, 23, 120–129. doi: 10.1002/mpr.1415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., & Williams J. B (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little R. J. & Rubin D. B (2014). Statistical analysis with missing data (Vol. 333). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Mahoney D. F. (2003). Vigilance. Evolution and definition for caregivers of family members with Alzheimer’s disease. Journal of Gerontological Nursing, 29, 24–30. doi: 10.3928/0098-9134-20030801-07 [DOI] [PubMed] [Google Scholar]
- Moskowitz J. T., Cheung E. O., Snowberg K. E., Verstaen A., Merrilees J., Salsman J. M., & Dowling G. A (2019). Randomized controlled trial of a facilitated online positive emotion regulation intervention for dementia caregivers. Health Psychology, 38, 391–402. doi: 10.1037/hea0000680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Caregiving & American Association of Retired Persons (2015). Caregiving in the U.S. 2015—Appendix B: Detailed methodology Retrieved from https://www.caregiving.org/wp-content/uploads/2015/05/CGV016-Main-Report-Appendix-B-Detailed-Methodology-5.21.15.pdf
- Pearlin L. I., Mullan J. T., Semple S. J., & Skaff M. M (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30, 583–594. doi: 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Phillips L. R., Morrison E. F., & Chae Y. M (1990). The QUALCARE Scale: Developing an instrument to measure quality of home care. International Journal of Nursing Studies, 27, 61–75. doi: 10.1016/0020-7489(90)90024-D [DOI] [PubMed] [Google Scholar]
- Pinquart M. & Sörensen S (2003). Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. The Journal of Gerontology. Series B, Psychological Sciences and Social Sciences, 58, P112–P128. doi: 10.1093/geronb/58.2.p112 [DOI] [PubMed] [Google Scholar]
- Quinn C., Clare L., & Woods B (2009). The impact of the quality of relationship on the experiences and wellbeing of caregivers of people with dementia: A systematic review. Aging and Mental Health, 13, 143–154. doi: 10.1080/13607860802459799 [DOI] [PubMed] [Google Scholar]
- Robbins M. L. & Kubiak T (2014). Ecological momentary assessment in behavioral medicine: Research and practice. In Mostofsky D. I.(Ed.), The handbook of behavioral medicine (1st ed) ( pp 429–446). Oxford, UK: John Wiley & Sons. [Google Scholar]
- Rovine M. J. & Walls T. A (2006). Multilevel autoregressive modeling of interindividual differences in the stability of a process. In Walls T. A & Schafer J. L.(Eds.), Models for intensive longitudinal data (pp. 124–147). New York, NY: Oxford University Press. doi:10.1093/acprof:oso/9780195173444.003.0006 [Google Scholar]
- Rubin D. B. (2004). Multiple imputation for nonresponse in surveys (Vol. 81). New York, NY: John Wiley & Sons. [Google Scholar]
- Scollon C. N., Kim-Prieto C., & Scollon C. N (2003). Experience sampling: Promises and pitfalls, strengths and weaknesses. Journal of Happiness Studies, 4, 5–34. doi:10.1023/a:1023605205115 [Google Scholar]
- Straus M. A., Hamby S. L., Boney-McCoy S., & Sugarman D. B (1996). The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric Data. Journal of Family Issues, 17, 283–316. doi: 10.1177/019251396017003001 [DOI] [Google Scholar]
- Sullivan T. P., McPartland T. S., Armeli S., Jaquier V., & Tennen H (2012). Is it the exception or the rule? Daily co-occurrence of physical, sexual, and psychological partner violence in a 90-day study of substance-using, community women. Psychology of Violence, 2, 154–164. doi: 10.1037/a0027106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarzia L., Valpied J., Koziol-McLain J., Glass N., & Hegarty K (2017). Methodological and ethical challenges in a web-based randomized controlled trial of a domestic violence intervention. Journal of Medical Internet Research, 19, e94. doi: 10.2196/jmir.7039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teitcher J. E., Bockting W. O., Bauermeister J. A., Hoefer C. J., Miner M. H., & Klitzman R. L (2015). Detecting, preventing, and responding to “fraudsters” in internet research: Ethics and tradeoffs. The Journal of Law, Medicine & Ethics, 43, 116–133. doi: 10.1111/jlme.12200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiglesworth A., Mosqueda L., Mulnard R., Liao S., Gibbs L., & Fitzgerald W (2010). Screening for abuse and neglect of people with dementia. Journal of the American Geriatrics Society, 58, 493–500. doi: 10.1111/j.1532-5415.2010.02737.x [DOI] [PubMed] [Google Scholar]
- Williamson G. M. & Schulz R (1995). Caring for a family member with cancer: Past communal behavior and affective reactions1. Journal of Applied Social Psychology, 25, 93–116. doi: 10.1111/j.1559-1816.1995.tb01586.x [DOI] [Google Scholar]
- Williamson G. M. & Shaffer D. R (2001). Relationship quality and potentially harmful behaviors by spousal caregivers: How we were then, how we are now. The Family Relationships in Late Life Project. Psychology and Aging, 16, 217–226. doi: 10.1037/0882-7974.16.2.217 [DOI] [PubMed] [Google Scholar]
- Won C. W., Fitts S. S., Favaro S., Olsen P., & Phelan E. A (2008). Community-based “powerful tools” intervention enhances health of caregivers. Archives of Gerontology and Geriatrics, 46, 89–100. doi: 10.1016/j.archger.2007.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan E. & Kwok T (2011). Abuse of older Chinese with dementia by family caregivers: An inquiry into the role of caregiver burden. International Journal of Geriatric Psychiatry, 26, 527–535. doi: 10.1002/gps.2561 [DOI] [PubMed] [Google Scholar]
- Zarit S. H., Kim K., Femia E. E., Almeida D. M., & Klein L. C (2014). The effects of adult day services on family caregivers’ daily stress, affect, and health: Outcomes from the Daily Stress and Health (DaSH) study. The Gerontologist, 54, 570–579. doi: 10.1093/geront/gnt045 [DOI] [PMC free article] [PubMed] [Google Scholar]