Abstract
Purpose:
In early 2020, the World Health Organization declared the outbreak of the disease COVID-19, caused by a new variant of coronavirus 2019-nCoV as a global pandemic. The government of India ordered a nationwide lockdown for 21 days, limiting movement of people as a preventive measure. This survey was designed and conducted during the lockdown period to assess its effect on ophthalmic practice and patient care in India.
Methods:
An online survey was sent across to practicing Indian ophthalmologists across through various social media platforms. All valid responses were tabulated and analyzed.
Results:
A total of 1260 ophthalmologists responded to the survey. Most of the respondents (775/1260; 61.5%) were in private practice and 14.8% (187/1260) were affiliated to ophthalmic institutes. At the time of taking the survey, 72.5% of the respondents (913/1260) were not seeing any patients due to the lockdown. Of those who were still examining patients, 82.9% (287/347) were only seeing emergency cases, based on their own clinical judgement. The proportion of ophthalmologists in ophthalmic institutes, government and municipal hospitals (126/253;49.8%) who were still seeing patients was significantly higher (P < 0.0001) than those in private practice (174/775;22.4%). Apart from emergencies such as trauma, retinal detachment, and endophthalmitis (81.8%), other surgeries that were still being performed included intravitreal injections (9.1%) and cataract surgeries (5.9%). Approximately, 77.5% (976/1260) of the respondents had begun telephonic/e-mail/video consultations or consultations over social media applications since the lockdown began. In addition, 59.1% (745/1260) felt that ophthalmologists were potentially at a higher risk of contracting COVID-19 compared to other specialties while examining patients. When asked about the resumption of practice upon easing off of the restrictions, 57.8% (728/1260) of the respondents said they were unsure of when to resume elective surgeries; furthermore, 62.8% (791/1260) were unsure about the preferred screening strategy or precautionary approach prior to resuming surgeries and were awaiting guidelines.
Conclusion:
Our survey shows that majority of ophthalmologists in India were not seeing patients during the COVID-19 lockdown, with near-total cessation of elective surgeries. Emergency services were still being attended to by 27.5% of ophthalmologists who responded. A large proportions of ophthalmologists had switched over to telephonic advice or other forms of telemedicine to assist patients. Most of the responding ophthalmologists were unclear about when and how to resume surgeries upon easing off of the COVID-19 related restrictions. Regulatory bodies should take note of this and issue appropriate guidelines regarding the same.
Keywords: 2019-nCoV, cataract, corona, coronavirus, eye, lockdown, ophthalmology, SARS, tears
In late 2019, a cluster of cases of pneumonia of unknown cause was seen in Wuhan, a large city in China.[1] Subsequently, in early 2020, through genomic sequencing, it was found that these cases were caused by a novel virus, which was called Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2); also known as 2019 novel Coronavirus (2019-nCoV).[2] India reported the first case of this Coronavirus disease (COVID-19) on January 30, 2020, in the state of Kerala in southern India, where a student with a history of travel to Wuhan presented with respiratory symptoms. This was followed by two more similar cases on consecutive days.[3] The World Health Organization since then has declared the outbreak to be a global pandemic.[4] As of April 1st, 2020, the total number of confirmed COVID-19 cases, globally has exceeded 9,00,000 and the number of cases in India has crossed 1,700.[5] The global pandemic has led to many governments across the globe to take swift and protective measures. It started in China, when cities were placed under complete lockdown, travel bans were put in place and schools and universities were indefinitely closed.[6] The reason for such drastic measures is that in a large proportion of cases, COVID-19 manifests only as a flu-like illness with fever, cough, sore throat, fatigue, dyspnea, occasional diarrhea, and vomiting, but in the select group of patients such as the elderlies and immunocompromised individuals, the condition deteriorates to acute respiratory distress syndrome (ARDS), septic shock, and multi-organ failure resulting in mortality. The danger is amplified due to the lack of a vaccine and effective therapeutic agents against this novel virus.[7]
The World Health Organization had notified that during previous such coronavirus outbreaks like SARS, human-to-human transmission occurred primarily through droplets, contacts, and fomites. It was suggested that the mode of transmission of COVID-19 could be similar.[8] Across the globe, healthcare workers continue to be at high risk for contracting COVID-19 in the course of their clinical duties toward affected patients. One of them was Dr. Li Wenliang, an ophthalmologist at Wuhan Central Hospital who had contracted COVID-19 from an asymptomatic glaucoma patient and succumbed to the disease later.[3]
Given the large population of over 1.3 billion, the government of India declared a total lockdown across the country as a part of its efforts to control the disease spread. At the time of the announcement, India had 519 confirmed cases and 10 reported deaths due to COVID-19. The restrictions came into force at midnight local time on 24th March 2020 and would be enforced for 21 days.[9] As a result of this lockdown, all regular out-patient departments across hospitals and clinics in India were to be shut and it was advised that all elective surgeries be deferred, but emergency healthcare services should continue to function. As a result of this step, ophthalmologists across the country temporarily ceased clinical services at their respective practice locations. With this background, this study was conceived, and a survey was circulated to assess the impact of the COVID-19 related lockdown on ophthalmic practice and patient care in India. The survey also assesses the perception among ophthalmologists regarding the risks, screening protocols, and prevention strategies related to clinical examination and surgeries after the resumption of their practices.
Methods
An online survey (hosted by www.surveymonkey.com) was circulated among Indian ophthalmologists on the 5th day after lockdown had been enforced. The invitation to participate was circulated through multiple groups on social media, namely, Facebook, WhatsApp, and Telegram. The survey, which consisted of nine questions [Supplementary Table 1], was open for a period of 48 hours. It was mandatory to answer all questions and the survey was anonymized and did not contain any identifying information. Association between categorical variables was assessed using Fisher exact test or Chi-squared test. We considered a P < 0.05 as statistically significant. All statistical analysis was performed with GraphPad Prism 6 (GraphPad Inc, La Jolla, CA).
Supplementary Table 1.
Questionnaire sent out to practicing ophthalmologists in India
| 1. What is the nature of your practice? |
| Private practice - own clinic |
| Government/Municipal Hospital |
| Institutional practice |
| Corporate / Multi-specialty hospital |
| Charitable hospital |
| Freelancing |
| 2. Are you currently seeing / operating patients?* |
| Yes |
| No |
| 3. If you are seeing/operating patients, what kind of patients are these? (You may choose more than one option) |
| Trauma |
| Red Eye |
| Infections (Lid, Orbit, Sac, Cornea and Endophthalmitis) |
| Vision loss |
| Emergencies (as per my clinical judgement) |
| All patients who come |
| 4. Which surgeries are you performing currently? |
| Only emergency surgeries (RD, Trauma, Endophthalmitis, etc.) |
| Intravitreal Injections |
| Cataract |
| Refractive surgery |
| Glaucoma procedures/ Vitreoretinal surgeries |
| Retinoblastoma/ tumor related care / Other procedures |
| I am not performing any surgeries |
| 5. Have you started telephonic / web consultations? (You may choose more than one option) |
| Telephonic consults |
| Email/WhatsApp/Telegram / Other social media applications |
| Video consultations |
| None as of now, but I plan to start soon |
| I do not plan to do any of the above |
| 6. If you do telephonic / web consultations, what are your fees for the consultation? |
| Same as the fees for an in-person consultation |
| Higher than the fees for an in-person consultation |
| Lower than the fees for an in-person consultation |
| I do not charge for these consultations. |
| Not Applicable, I have not started tele-consultation / video consultation. |
| 7. From what information that is available what is your opinion regarding the risk that ophthalmologists face with regards to COVID 19? |
| Ophthalmologists are at EQUAL risk of contracting COVID 19 compared to other specialties when it comes to examining patients |
| Ophthalmologists are at HIGHER risk of contracting COVID 19 compared to other specialties when it comes to examining patients |
| Ophthalmologists are at LOWER risk of contracting COVID 19 compared to other specialties when it comes to examining patients |
| 8. Upon easing of the COVID 19 related restrictions, what would be your plan regarding elective surgeries? |
| Restart elective surgeries immediately after restrictions are lifted |
| Start elective surgeries 1 week after resumption of clinical duties |
| Not sure about when to start elective surgeries after resumption of clinical duties. |
| 9. Regarding surgeries that would be planned after resumption of clinical duty, what would be your preferred approach? |
| Include testing for COVID-19 as a part of pre-operative screening |
| Use additional Personal Protective Equipment (PPE) in all cases |
| Perform testing for COVID-19 preoperatively AND Use PPE in all cases |
| Unsure of what to do, therefore awaiting clear guidelines |
*Upon receiving “No” as an answer for Q2, the survey directed respondents to Q5
Results
A total of 1260 responses were received at by midnight, 31st March 2020. The respondents were asked to specify the nature of their practice. In all, 61.5% (775/1260) were private practitioners with their own clinics; 14.8% (187/1260) were affiliated to ophthalmic institutes; 9.4% (118/1260) of the respondents were working in corporate/multi-specialty hospitals; 5.2% (66/1260) were working in government/municipal hospitals; and 2.2% (28/1260) were freelancing surgeons. Detailed analysis of this data showed that a significantly higher proportion of ophthalmologists affiliated to ophthalmic institutes, government and municipal hospitals (126/253;49.8%) were currently seeing patients as compared to those in private practice (174/775;22.4%); (P < 0.0001).
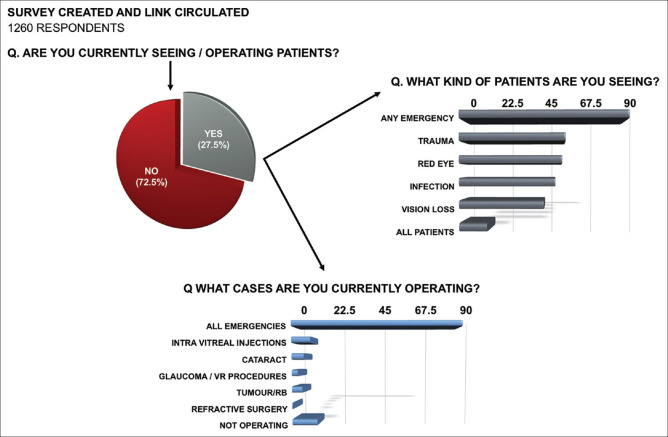
The respondents were asked if they were still examining/operating patients, and an overwhelming majority-72.5% (913/1260) indicated that they had completely stopped all clinical work during the lockdown [Fig. 1]. The remaining 27.5% (347/1260), who indicated that they were still seeing and operating patients, were asked to specify the type of cases that they were currently seeing. While trauma (51.9%) was the most common type of case being examined, most respondents indicated that any case that would be classified as an emergency (82.9%) were also seen by them. Furthermore, 13.5% (47/347) specified that they were seeing all patients who came to their clinics with no form of triage/screening being performed.
Figure 1.
Chart showing the type of cases currently being seen by ophthalmologists who are attending to patients during the lockdown period in India
Regarding surgical procedures, 81.8% (284/347) indicated that they were operating only emergency cases including trauma, retinal detachments, and endophthalmitis. Of the other procedures, 9.1% (32/347) were administering intravitreal injections and 5.7% (20/347) were performing cataract surgery. It was also noted that 4.9% (17/347) of the ophthalmologists were involved in other procedures like tumor/retinoblastoma related care, whereas 12.1% (42/347) were only examining patients presenting with emergencies, but not operating any.
The respondents were asked if they had explored and initiated other avenues of attending to their patients' needs such as telemedicine. Telephonic consultations (54.9%) were the most popular mode of reaching out to patients, followed by email and social media applications like WhatsApp and Telegram (48%). Video-calls for consultation were being used by 9.9% of the ophthalmologists who took the survey. In all, 77.5% (976/1260) of the ophthalmologists had begun utilizing some form of telemedicine since the lockdown began; 12.9% (163/1260) were not currently treating patients remotely but had plans to do so [Fig. 2]. In contrast, 9.6% (121/1260) of the clinicians had no plans to start telephonic/electronic consultations. Of those who were currently involved in some form of telemedicine, 90.7% (886/976) were not asking any professional fees from patients; 5.8% (57/976) were charging the same professional fees as they would for an in-person consultation and the professional fees for tele-consultation were less than that for an in-person consultation for 2.9% (28/976) of the ophthalmologists. A small minority 2.9% (5/976) were charging higher than usual fees.
Figure 2.
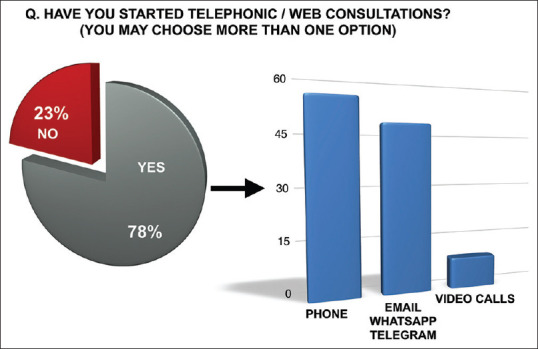
Graph showing the responses of the ophthalmologists when asked about tele-medicine
Ophthalmologists were asked about their perceptions of the risk they face while examining patients, given the scenario of the global COVID-19 pandemic: 59.1% (745/1260) felt that ophthalmologists were at a higher risk of contracting COVID-19 compared to other specialties when it comes to examining patients.
The last part of the survey focused on strategies upon resumption of regular clinical duties after the lockdown period. When asked what their plan regarding elective surgeries would be, upon easing off of the COVID-19 related restrictions, 11.8% (148/1120) said that they would immediately resume elective surgeries as before and 30.4% (383/1260) expressed that they would wait for at least one week before resuming elective surgeries. However, 57.8% (729/1260) were not sure about when to start elective surgeries after the resumption of clinical duties. The respondents were also asked about what their preferred prevention strategy would be, regarding pre-operative screening: majority of the clinicians (62.8%; 792/1260) were unsure of what should be done and were awaiting guidelines; 16.6% (135/1260) indicated that they would prefer to use additional personal protection equipment (PPE) for surgeries; 9.9% (124/1260) indicated that they would want to perform testing for COVID-19, pre-operatively prior to any elective surgery; 10.7% (135/1260) said they would include pre-operative screening for COVID-19 as well as use PPE for all surgeries.
Discussion
Our survey showed that the majority of the practicing ophthalmologists in India were in total lockdown. While the clinicians themselves may be available, the unavailability of managerial, administrative, nursing and other support staff may pose logistical and operational challenges to running a health care facility in times of a pandemic. It was noted that most of the ophthalmologists working in large institutes and government hospitals (126/253;49.8%) were still seeing and operating cases. This is understandable since large hospitals tend to be better equipped in terms of staff, protective equipment, medicines, and in-patient facilities for isolation. Majority of the stand-alone private practitioners (601/775; 77.5%) had closed their practices and were not actively involved in direct patient care.
While emergencies such as trauma and other conditions that qualified for emergent care, based on the judgement of the clinician, remained the most common procedures still being performed, it was interesting to note that at the time of responding to the survey, 9.1% (32/347) of those who were still operating, continued to administer intravitreal injections and 5.7% (20/347) were still performing cataract surgery. There are rare circumstances where a cataract surgery may be classified as an emergency, such as phacolytic glaucoma, subluxated/traumatic cataract, etc., However, the survey was not designed to capture those specific details. Surprisingly, one respondent indicated that he/she was performing refractive surgeries at the time of responding to the survey.
Given the close physical contact nature of their work and the previously discussed modes of transmission of the virus, it is clear that ophthalmologists are one of the more at-risk medical specialists for COVID-19 transmission. The results of our survey indicate that Indian ophthalmologists also perceive themselves to be at a higher risk of contracting COVID-19 as compared to other specialties [Fig. 3]. An eye clinic is a high-risk environment for both: the examining doctor as well as the patient and it is important for the ophthalmologist to know why. The knowledge that we have on the ophthalmic implications of the SARS-CoV-2 virus is limited and constantly evolving. Lu et al., in February 2020, reported that ocular surfaces may be a potential target for SARS-CoV-2 invasion.[10] However, some authors do not fully support this. This is primarily because, while some COVID-19 patients do have conjunctivitis, not all of them test positive for SARS-CoV-2 nucleic acid in conjunctival sac swabs. Conversely, there were some patients, who did not have conjunctivitis but tested positive for the SARS-CoV-2 nucleic acid in their conjunctiva sac swabs.[11] It was also speculated that the virus enters the tears through droplets, which may pass through the nasolacrimal ducts and then into the respiratory tract.[11] Xia et al. in their study to investigate the presence of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection enrolled a total of 30 patients in their study. They reported that only two samples of tear and conjunctival secretions that were obtained from one patient with conjunctivitis yielded positive reverse transcription polymerase chain reaction (RT-PCR) results, but the isolation of the virus was unsuccessful. In all, 58 samples from other patients were negative.[2] Soon after this study was published, Jun et al. put forth their paper, where 64 tear samples were collected from a total of 17 COVID-19 patients between the third and twentieth days following the initial symptoms. They found that neither viral culture nor RT-PCR detected the virus, suggesting a low risk of ocular transmission.[12] A more recent study by Wu and colleagues reported that from 38 patients that were included in the study, 28 patients (73.7%) had positive findings for COVID-19 on RT-PCR from nasopharyngeal swabs, and of these, 2 patients (5.2%) yielded positive findings for SARS-CoV-2 in their conjunctival as well as nasopharyngeal specimens. They reported that one-third of patients with COVID-19 included in their study had ocular abnormalities such as conjunctival hyperemia, chemosis, and epiphora which frequently occurred in patients with more severe COVID-19. The authors concluded that although there is a low prevalence of SARS-CoV-2 in tears, it is possible to transmit via the eyes.[13] It is clear that as time goes by, and more clinicians see more COVID-19 cases; the exact mechanism and the magnitude of spread of the disease through tears will be clearer.
Figure 3.
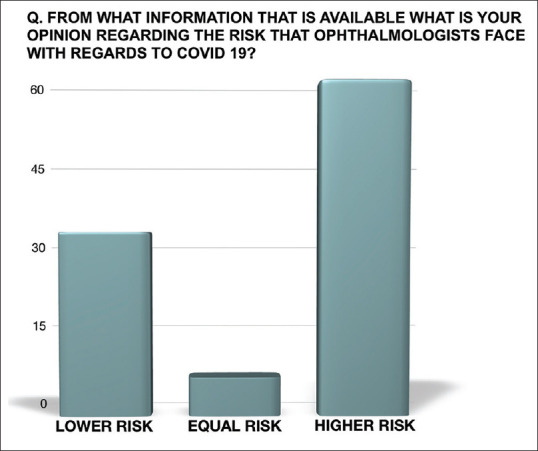
Graph showing the responding ophthalmologists' perceptions of the risk they face while examining patients, given the scenario of the global COVID-19 pandemic
It has been postulated from genomic and structural analyses that the SARS-CoV-2 has a similar receptor-binding motif as SARS-CoV, which allows it to infect host cells via the angiotensin-converting-enzyme-2 (ACE2).[14] The virus uses this as a cell entry receptor to invade respiratory and lung epithelium through the spike (S) protein.[15] ACE2 is mainly expressed in posterior tissues of the eye, namely, the retina and the retinal pigment epithelium.[16,17] While ACE2 has been found in the aqueous humour, the expression of ACE2 in more anterior tissues such as human conjunctival and corneal epithelium has yet to be established.[16,18] Hence, the hypothesis of SARS-CoV-2 ocular infection through ACE2 must be investigated.
While elective surgeries such as cataract and refractive surgeries can be rescheduled and planned at a later date, other patients such as trauma, postoperative patients, patients with sudden vision loss and infections need to be examined and treated on an urgent basis. It was noted that in our survey, 77.5% of the ophthalmologists who took the survey had begun engaging in some form of telemedicine since the lockdown began and a further 12.9% of the population were planning on starting soon. In India, telemedicine practice guidelines were issued recently to enable medical practitioners to provide healthcare using telemedicine.[19] It is important to reach out to existing patients or those with existing appointments to inform about the change in their appointments. In Hong Kong, during the COVID-19 outbreak, eye hospitals utilized short message service (SMS) to send information to patients via their electronic mobile devices, at least one week in advance before their scheduled appointments, providing them with an enquiry phone number so they could call to postpone their appointments.[8] Traditionally, tele-ophthalmology has been employed mainly for patients in under-served rural areas in need of specialty care. However, at times of public health emergencies like a pandemic, a simple phone call or a video-call between the ophthalmologist and the patient serves as a telemedicine tool that can help in deciding if the case requires emergent medical care or not.[20] A “virtual triage,“ either using smartphones or webcam-enabled computers allows patients to be efficiently screened, is both patient-centered and conducive to self-quarantine, and it protects patients, clinicians, and the community from exposure.[21] Situations such as a global pandemic pose unique challenges to the healthcare delivery system. Although tele-medicine will not solve them all, it remains well suited for scenarios such as the one we face today, where infrastructure remains intact and clinicians are available to see patients.[21]
In an effort to reduce the risk of the SARS-CoV-2 virus transmission from human to human and the rate of new case development, many ophthalmic societies, such as the American Academy of Ophthalmology (AAO) as well as the All India Ophthalmological Society (AIOS) have issued recommendations regarding cessation of routine clinical and surgical duties.[3,22] The AIOS has recommended postponement of all routine consultations and elective surgeries by four weeks. It was also recommended that all ophthalmologists provide urgent or emergent care, and triage and reschedule all elective OPD visits and procedures. This has been found to be very useful in ensuring that emergent patient care is not compromised and the potential for disease spread is kept to a minimum during the pandemic and lockdown period.
The most crucial bit of information that the survey highlighted was the lack of clarity among clinicians about how to proceed after the resumption of routine services, once the lockdown period is over [Figs. 4 and 5]. In our survey, many respondents indicated that they would prefer to use additional personal protection equipment (PPE) for surgeries or perform testing for COVID-19 pre-operatively prior to any elective surgery or even both. Unless there is unequivocal evidence that proves the utility of these additional measures in all patients, they would add to the cost of patient care. There is also uncertainty over the possibility of an extended lockdown, but that notwithstanding, it is important that ophthalmic societies consult with experts, study the available literature and issue clear guidelines about the timing for resumption of routine elective surgery and the necessary steps to be taken by all ophthalmic surgeons to minimize the chances of COVID-19 contraction and spread. Complicating this issue further is the presence of asymptomatic or pre-symptomatic COVID-19 patients who exhibit no clinical signs of the disease but test positive for COVID-19 and can potentially infect others.[23]
Figure 4.
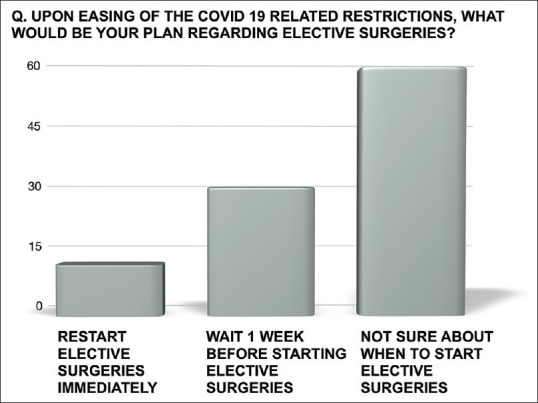
The ophthalmologists' responses when asked about timing for re-starting elective surgeries upon lifting up of the lockdown
Figure 5.
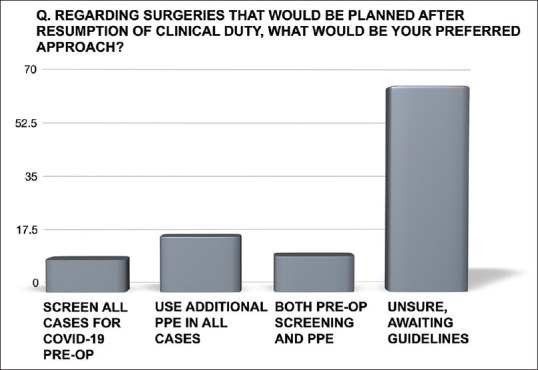
Graphical representation of the responses when asked about surgical strategies upon resumption of elective surgeries after the lockdown
The lockdown, which was a first in the country, brought with it, many uncertainties; not just on the personal front but also on the professional front for most medical practitioners. In this survey, a total of 1260 responses were recorded: even though this is a very large number, we understand that this does not represent the complete Indian ophthalmic fraternity. Given the fast-evolving scenario, it was not feasible to have a validated survey; also, the authors felt it necessary to keep the survey open only for a short period of time during the lockdown itself. Age and geographic information of the respondents could have provided more insights such as areas where emergency eye care was unavailable, among other things.
Conclusion
COVID-19 pandemic will change the way we practice forever. Changes in the clinic management policy: scheduling appointments, active screening, patient healthcare declarations, expedited consults for sick patients, and other waiting room policies, may become permanent. Staff protection and environmental precautions to prevent droplet and fomite transmission are also likely changes.[24] It is possible that in the days to come, evidence will emerge which may change the prevention and treatment strategies for COVID-19. The disease and the restrictions in place for limiting its spread are challenges for the Indian ophthalmic community, and the global ophthalmic fraternity at large. But for the ophthalmology community to get back to serving society at large in an optimal and secure way, clear guidelines need to be evolved by the regulatory bodies to help resume patient care without compromising on safety; both––their patients' as well as their own.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–3. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020 doi: 10.1002/jmv.25725. doi: 101002/jmv 25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khanna RC, Honavar SG. All eyes on Coronavirus—What do we need to know as ophthalmologists. Indian J Ophthalmol. 2020;68:549–53. doi: 10.4103/ijo.IJO_516_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. [Last accessed on 2020 Mar 31]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus- 2019 .
- 5. [Last accessed on 2020 Mar 31]. Available from: https://www.worldometers.info/coronavirus/
- 6.Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9:103–4. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shetty R, Ghosh A, Honavar SG, Khamar P, Sethu S. Therapeutic opportunities to manage COVID-19/SARS-CoV-2 infection: Present and future. Indian J Ophthalmol. 2020 doi: 10.4103/ijo.IJO_639_20. [Epub ahead of print] doi: 104103/ijoIJO_639_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: An experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. 2020 doi: 10.1007/s00417-020-04641-8. doi: 101007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. [Last accessed on 2020 Mar 31]. Available from: https://www.bbc.com/news/world-asiaindia-52024239 .
- 10.Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qing H, Li Z, Yang Z, Shi M, Huang Z, Song J, Song Z. The possibility of COVID19 transmission from eye to nose. Acta Ophthalmol. 2020 doi: 10.1111/aos.14412. doi: 101111/aos 14412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jun ISY, Anderson DE, Kang AEZ, Wang LF, Rao P, Young BE, Lye DC, Agrawal R. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. 2020 doi: 10.1016/j.ophtha.2020.03.026. doi: 101016/jophtha 202003026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu Ping, Duan F, Luo C. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020 doi: 10.1001/jamaophthalmol.2020.1291. doi: 101001/jamaophthalmol 20201291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by novel coronavirus from Wuhan: An analysis based on decade-long structural studies of SARS. J Virol. 2020 doi: 10.1128/JVI.00127-20. doi: 101128/JVI00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–3. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holappa M, Vapaatalo H, Vaajanen A. Many faces of renin-angiotensin system-focus on eye. Open Ophthalmol J. 2017;11:122–42. doi: 10.2174/1874364101711010122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes?? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020:1–5. doi: 10.1080/09273948.2020.1738501. doi: 10.1080/09273948.2020.1738501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choudhary R, Kapoor MS, Singh A, Bodakhe SH. Therapeutic targets of renin-angiotensin system in ocular disorders. J Curr Ophthalmol. 2016;29:7–16. doi: 10.1016/j.joco.2016.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. [Last accessed on 2020 Apr 03]. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf .
- 20.Tang RA, Morales M, Ricur G, Schiffman JS. Telemedicine for eye care. J Telemed Telecare. 2005;11:391–6. doi: 10.1177/1357633X0501100803. [DOI] [PubMed] [Google Scholar]
- 21.Hollander JE, Carr BG. Virtually perfect Telemedicine for COVID-19. N Engl J Med. 2020 doi: 10.1056/NEJMp2003539. doi: 101056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 22. [Last accessed on 2020 Mar 31]. Available from: https://www.aao.org/headline/new- recommendations-urgent-nonurgent-patient-care .
- 23.Qian G, Yang N, Ma AHY, Wang L, Li G, Chen X, et al. A COVID-19 Transmission within a family cluster by presymptomatic infectors in China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa316. doi: 101093/cid/ciaa316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wan KH, Huang SS, Young A, Chiu Lam DS. Precautionary measures needed for ophthalmologists during pandemic of the coronavirus disease 2019 (COVID-19) Acta Ophthalmol. 2020 doi: 10.1111/aos.14438. doi: 101111/aos14438. [DOI] [PMC free article] [PubMed] [Google Scholar]