Abstract
The COVID-19 pandemic has taken tragic proportions and has disrupted lives globally. In the wake of governmental lockdowns, ophthalmologists need practical and actionable guidelines based on advisories from national health departments on how to conduct their duties during nationwide lockdowns and after these are lifted. In this paper, we present a preferred practice pattern (PPP) based on consensus discussions between leading ophthalmologists and health care professionals in India including representatives from major governmental and private institutions as well as the All India Ophthalmological Society leadership. In this document, the expert panel clearly defines the range of activities for Indian ophthalmologists during the ongoing lockdown phase and precautions to be taken once the lockdown is lifted. Guidelines for triage, governmental guidelines for use of personal protective equipment from ophthalmologists' point of view, precautions to be taken in the OPD and operating room as well as care of various ophthalmic equipment have been described in detail. These guidelines will be applicable to all practice settings including tertiary institutions, corporate and group practices and individual eye clinics and should help Indian ophthalmologists in performing their professional responsibilities without being foci of disease transmission.
Keywords: Consensus, COVID-19, Guidelines, lockdown, ophthalmology, pandemic, precautions, preferred practice
Composition of the All India Ophthalmological Society - Indian Journal of Ophthalmology Expert Group for COVID-19 Practice Guidelines includes the Writing Committee (as listed) and the following members (in alphabetical order by the first name): Anand Vinekar, Narayana Nethralaya Eye Institute, Bangalore , Karnataka and Secretary, Indian Retinopathy of Prematurity Society; Aniruddha Agarwal, Post Graduate Institute of Medical Education and Research, Chandigarh; Arshi Singh, Bababsaheb Ambedkar Hospital New Delhi; Arup Chakrabarti, Chakrabarti Eye Care Centre, Thiruvanathapuram, Kerala and Editor Proceedings, All India Ophthalmological Society; Ashok K Grover, Sir Gangaram Hospital, New Delhi; Astha Jain, Aditya Jyot Eye Institute, Mumbai, Maharashtra; Barun Kumar Nayak, P. D. Hinduja National Hospital and Medical Research Centre, Mumbai, Maharashtra and President Elect, All India Ophthalmological Society; Chitra Ramamurthy, The Eye Foundation, Coimbatore, Tamil Nadu and Chairman, Academic and Research Committee, All India Ophthalmological Society; Debasish Bhattacharya, Disha Eye hospital, Kolkata, West Bengal; Jatinder Bali, Hindu Rao Hospital and NDMC Medical College, New Delhi; Kirti Singh, Gurunanak Eye Centre, Maulana Azad Medical College, New Delhi; Lalit Verma, Centre for Sight, New Delhi and Vice President, All India Ophthalmological Society; Lingam Gopal, National University Hospital, Singapore; Mandeep Jot Singh, Centre for Sight, New Delhi; Nandini Sharma, Community Medicine, Maulana Azad Medical College, New Delhi; T. Nirmal Fredrick, Nirmal's Eye Hospital, Chennai, Tamil Nadu and Hospital Accreditation Expert, Chennai; Partha Biswas, BB Eye Foundation, Kolkata, West Bengal and Chairman, Scientific Committee, All India Ophthalmological Society; Priya Narang, Narang Eye Care and Laser Centre, Ahmedabad, Gujarat; Rajesh Sinha, Dr Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi and Treasurer, All India Ophthalmological Society; Raj Vardhan Azad, Professor Emeritus Regional Institute of Ophthalmology, Indira Gandhi Institute of Medical Sciences, Patna , Bihar and President, Indian Retinopathy of Prematurity Society; Ramamurthy D, The Eye Foundation, Coimbatore, Tamil Nadu; Savitri Sharma, Ocular Microbiology, LV Prasad Eye Institute, Hyderabad, Telangana; Soosan Jacob, Dr Agarwal's Eye Hospital, Chennai, Tamil Nadu. All authors have contributed equally and hence carry equal authorship credit.
The ongoing pandemic caused by the SARS – CoV-2 virus (COVID-19) has caused havoc across the globe, forcing entire nations into a self-imposed quarantine to contain the local transmission and community spread of infection. The Government of India (GoI) has mandated a country-wide total lockdown of all non-essential services. This lockdown remains in effect from March 25 to April 14, 2020, following which the government may partially relax the restrictions to slowly and systematically ease in routine life. It is also possible that the lockdown may be extended depending on the situation, specifically the daily incidence of new cases. In the wake of these unprecedented measures, ophthalmology clinics have been tremendously impacted, with most suspending routine care and surgery and offering only emergency services. Since ophthalmology is a stand-alone specialty with relatively fewer eye- and life-threatening emergencies, most of the practices have temporarily shut down. It is important to understand that during such potentially long-winding pandemics, we need to achieve a professional and ethical balance between becoming hotspots for viral transmission and providing services for ophthalmic emergencies.
The All India Ophthalmological Society (AIOS) has recently issued practice sustenance guidelines to its 22,000+ members.[1] An editorial in the Indian Journal of Ophthalmology (IJO) documented what was known about the COVID-19 disease from an ophthalmologist's point of view.[2] Though practical and useful, some of these guidelines were empiric. Guidelines issued by other national and international bodies may not be directly applicable to India and to Ophthalmology.[3] Also, there are several guidelines issued by health ministries of different states, with some even suggesting that ophthalmic hospitals be ready to accommodate quarantined patients, leading to confusion and panic amongst ophthalmologists. Additionally, many questions remain especially about the resumption of ophthalmic practice once the governmental restrictions are lifted. Thus, there is a need for a set of evidence-based and consensus-driven guidelines from a professional expert peer group.
In this paper, we attempt to develop a preferred practice pattern (PPP) based on consensus discussion between some of the leading ophthalmologists in India, major institutional representatives, and the AIOS leadership. This document clearly defines the gamut of activities for Indian ophthalmologists during the ongoing lockdown phase and precautions to be taken once the lockdown is lifted. Additionally, it is applicable to all practice settings including tertiary institutions, corporate and group practices and individual eye clinics.
Methods
The guidelines provided by the AIOS Governing Council 2020 was used as the base for developing this consensus-based PPP.[1] An invitation to review these guidelines was sent out by email to 38 eminent professionals (ophthalmologists, ocular microbiologists, health delivery experts, quality of care experts and administrators) across India, including heads of the major teaching institutions, both in the government and private sectors. These included members from the AIOS governing council, the editor and associate editor of IJO, and 10 experts from 6 teaching institutes in South India, 3 experts each from the north and east India all from separate institutions and 1 member each from western and central India. The experts suggested several changes in the base document that was collated,[1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22] and the consensus derived. Disagreements on guidelines were resolved by discussion between members. The consensus-based PPP were divided into those during the time of lockdown and those after the lockdown is lifted.
Practice Guidelines for Ophthalmologists During the Lockdown
Scheduled appointments
Postponement of all the routine outpatient consultations by 4 weeks or until the government of India has provided further information and instructions.[4]
Postponement of all elective surgeries and procedures for 4 weeks or as per guidelines issued by the government of India.
It may be prudent to create public awareness about what constitutes an ophthalmic emergency and create alternate channels for patients to interact with their ophthalmologists including phone calls, emails, social media interaction, and tele-consultations, if feasible. These measures will alleviate fears that patients may have and reduce unnecessary panic and visit to the emergency rooms.
Ophthalmic Emergencies
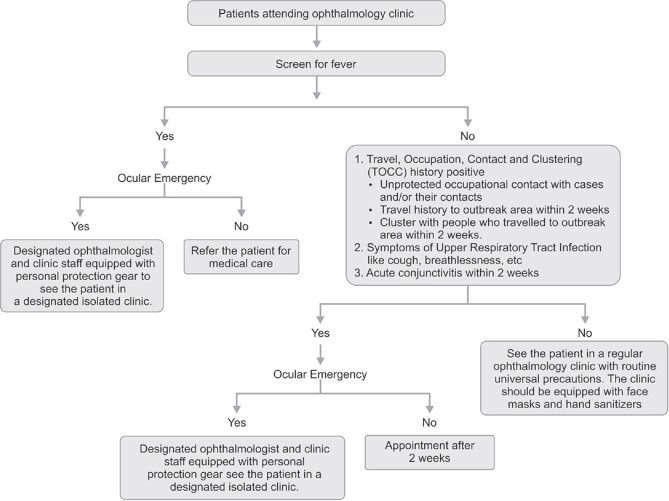
The ophthalmologists should triage patients [Fig. 1] and decide which patient requires emergent care. It is recommended by this expert group that all ophthalmologists provide only emergent care, after the triage and reschedule all elective OPD visits and procedures. Urgency is determined by the ophthalmologist's judgment of the potential risk to vision, eye and life and impact on the quality of life if untreated. One must always consider individual medical and social circumstances such as the patients' age, laterality of the disease, location of the patient, and requirement of caregiver, apart from finances and availability of medical care after the emergency surgery. In our opinion, cases that can be postponed for more than 4 weeks without considerable risk of loss of vision, general health and functioning should qualify as “elective“. Based on the triage system, the expert group has classified OPD and surgical procedures as an emergency, urgent and routine. Subspecialty-wise recommendations are listed in Table 1.
Figure 1.
Flowchart showing the triage system to be used in ophthalmology clinics[2,15]
Table 1.
Subspecialty - wise triage of ophthalmic clinical situations**
| Specialty | Emergency - See immediately | Urgent - See as soon as possible | Routine - Reschedule >3 months or Teleophthalmology |
|---|---|---|---|
| Comprehensive Ophthalmology | |||
| New/Follow-up | • Any acute/severe vision loss | • Blepharitis | |
| • Mild/moderate dry eye | |||
| • Watery eye | |||
| • Most conjunctivitis (triage via teleophthalmology) | |||
| Surgery | • Elective cataract surgery, Nd: YAG capsulotomy | ||
| • Laser refractive surgery | |||
| Cataract | |||
| New/Follow-up | • Cataract/Posterior capsule opacification | ||
| Surgery | • Cataract surgery for intractable high IOP (phacomorphic glaucoma, phacolytic glaucoma, angle-closure glaucoma), Cataract surgery for traumatic cataract with the ruptured anterior lens capsule | • Cataract surgery for cataract blindness when the patient is legally blind (i.e., combined effect of BCVA <6/60 in both eyes or field of vision constricted to 10 degrees or less of arc around central fixation in the better eye) | • Elective cataract surgery, Nd: YAG capsulotomy |
| Cornea/Refractive Surgery | |||
| New/Follow-up | • Microbial keratitis • Corneal trauma • Acute peripheral ulcerative keratitis • A neurotrophic cornea with ulceration • Therapeutic (bandage) contact lens patients • Corneal graft rejection • Ocular surface squamous neoplasia • Stevens Johnson syndrome |
• Minor trauma (e.g., abrasions, foreign bodies, recurrent corneal erosions) • Corneal ectasia with a moderate risk of progression (age <21 or documented progression>1D in 6 months) • Marginal keratitis (follow-up with teleophthalmology if appropriate) • Severe sight-threatening ocular surface disease • Routine post-operative patients |
• Blepharitis • Mild/moderate dry eye, any other ocular surface condition • Corneal ectasia with low risk of progression • Drug-induced keratopathies • Metabolic keratopathies |
| Surgery | • Urgent tectonic keratoplasty (perforations) • Therapeutic keratoplasty • Urgent primary care for chemical burns/thermal burns/Stevens Johnson syndrome |
• Keratoplasty for bullous keratopathy with a high risk of infection or pain • Keratoplasty in a patient <6/60 in both eyes with expected short term improvement • Cross-linking for progressive ectasia (either rapid progression or borderline thickness) |
• Laser refractive surgery • Routine corneal transplantation • Pterygium surgery • Collagen cross-linking for slowly progressive ectasia |
| Glaucoma | |||
| New/Follow-up | • IOP >40 mm Hg • Congenital and developmental glaucoma • Acute angle-closure • Acute neovascular glaucoma |
• After a change of glaucoma therapy where IOP is anticipated to change • Routine post-operative care for glaucoma filtration surgery/tubes • Anyone with IOP >30 mm Hg and glaucomatous visual field defect • Uncontrolled glaucoma |
• Stable glaucoma monitoring with no documented progression for 2 years • Ocular hypertension with no evidence of glaucoma and at low risk of developing glaucoma in the next 6 months |
| Surgery | • Acute uveitic glaucoma • Acute lens-related glaucoma • A new referral that the treating ophthalmologist considers urgent • Lens extraction surgery to ameliorate angle closure disease not controlled with laser or medical therapies • Glaucoma surgery for IOP lowering of any type in advanced glaucoma, rapid progression or very high IOP where clinically important progression is likely in the next 1 month, where conservative therapies have failed, are likely to fail or are contraindicated • Any surgery to manage acute sight-threatening complication of glaucoma surgery (e.g., bleb or tube infection) • Closure of cyclodialysis cleft leading to sight-threatening hypotony |
• Lens extraction surgery to ameliorate angle closure disease when the risk of progression of angle-closure or glaucoma over the next 6 months is unacceptably high. This includes the at-risk fellow eye of eyes blinded by angle closure disease • Glaucoma surgery for IOP lowering of any type in glaucoma where clinically important progression is likely in the next 6 months, where conservative therapies have failed, are likely to fail or are contraindicated |
• Elective cataract surgery in glaucoma patient not blinded by cataract • Any lens extraction procedure combined with micro bypass glaucoma surgery where the lens extraction itself does not fall into high or medium urgency |
| Medical Retina | |||
| New/Follow-up | • Suspected or confirmed active CNV needing treatment • Intravitreal injections for Neovascular AMD, Diabetic macular edema, retinal vein occlusion, other CNV, macular edema. Treat and extend to maximum interval possible. • Active proliferative diabetic retinopathy requiring treatment (PRP laser or intravitreal-anti VEGF) • Malignant hypertensive retinopathy • ROP screening and laser and anti-VEGF treatment[22] |
Macular edema requiring treatment | • Non-neovascular (dry) AMD • Low-risk diabetic retinopathy screening • Non-proliferative diabetic retinopathy without macular edema • Stable treated proliferative diabetic retinopathy • Central serous chorioretinopathy • Macular telangiectasia without CNV • Retinal dystrophies • Screening for macular drug toxicity • Angioid streaks • Hypertensive retinopathy (non-malignant) • Choroidal folds |
| Vitreoretinal Surgery/Trauma | |||
| New/Follow-up | • Acute retinal detachment • Suspected retinal tears • Open globe injuries: Including IOFB • Acute endophthalmitis • Vitreous hemorrhage (dense, requiring vitrectomy) • Dropped nucleus requiring vitrectomy/lensectomy • Submacular hemorrhage requiring vitrectomy • Aqueous misdirection requiring vitrectomy • Complex surgery post-operative (minimize visits) • Diagnostic vitrectomy for infectious or oncological causes |
• Acute full-thickness macular holes • Severe vitreomacular traction syndrome • Myopic traction maculopathy with foveal detachment • Heavy liquid removal • Exposed scleral buckles at risk of infection |
• Epiretinal membranes • Silicone oil removal (unless developing complications such as emulsification) • Intraocular lens procedures • Symptomatic vitreous opacities |
| Surgery | • Surgery for the above, surgery for ROP and drainage in cases with appositional choroidal effusion, suprachoroidal hemorrhage, or flat anterior chamber | • Surgery for the above | • Surgery for the above |
| Uveitis | |||
| New/Follow-up | • Acute anterior uveitis, posterior uveitis, panuveitis • Intermediate uveitis with vision-threatening complications • Retinal vasculitis • Patients with uveitis of any form affecting an only eye (VA in fellow eye <6/60) |
• Chronic/persistent anterior uveitis managed with topical therapy only, teleophthalmology recommended where possible • Quiescent/stable forms of uveitis on stable systemic therapy (prednisolone dose <=7.5 mg/daily); teleophthalmology recommended where possible • It is highly recommended that patients receiving an intravitreal depot steroid injection for uveitis have at least 1 clinic review/in-person IOP check (ophthalmologist or optometrist) 3-6 weeks post-injection |
• Patients with an established history of recurrent, self-limiting episodes of acute anterior uveitis without sight-threatening complications (e.g., cystoid macular edema, steroid response) could be considered for teleophthalmology consult at the onset of a recurrence and for follow-up at 6-8 weeks, with clinical review if indicated • Uveitis cases in remission (quiescence without any treatment) |
| Surgery | • Vitreous biopsy and/or AC tap for infectious/inflammatory uveitis or malignant tumors | • Most uveitic cataracts | |
| Ocular Oncology | |||
| New/Follow-up | • Suspected malignant ocular tumors (e.g., retinoblastoma, uveal melanoma, metastases, intraocular lymphoma, etc.) • Confirmed malignant ocular tumors requiring acute treatment • Tumors previously booked for 3 months planned follow-up interval |
• Fundus tumors/lesions causing macular exudation (choroidal haemangioma, Coats, retinal capillary haemangioblastoma) • Tumors previously booked for up to 6 months planned follow-up interval |
• Stable choroidal naevi, CHRPE, iris cysts • Stable treated tumors • Tumors previously booked for over 6 months planned follow-up interval |
| Surgery | • Surgery for malignant tumors (including plaque brachytherapy for choroidal melanoma, enucleation, EUA and focal therapy, chemotherapy, etc) | Surgery for the above | |
| Oculoplastics | |||
| Alert: Due to the high risk of COVID 19 infection from the nasopharynx, avoid all nasal syringing, lacrimal surgery and nasal endoscopy. Treat thyroid eye disease medically first. If orbital decompression is still required, avoid medial wall/floor decompression which creates an entry into the paranasal sinuses. | |||
| New/Follow up | • Severe thyroid eye disease • Orbital tumors (sight threatening or malignant-suspected/known) • Orbital vascular lesions (carotid-cavernous fistula, progressive/sight-threatening vascular anomalies- e.g., extensive haemangioma, progressive vascular malformation e.g., acute bleed) • Orbital inflammatory disease (orbital/periorbital cellulitis, orbital abscess; sight-threatening orbital inflammation of any cause; acute dacryocystitis/lacrimal abscess, panophthalmitis) • Periocular malignancy (biopsy-proven or suspected) including melanoma (invasive and in situ), sebaceous carcinoma, squamous cell carcinoma, other high-grade malignancy (Merkel cell, adnexal carcinoma, etc.), high-risk basal cell carcinoma (medical or lateral canthal, recurrent, high-risk subtype, locally advanced i.e., orbital invasion) |
• Progressive benign orbital tumors • Moderately severe thyroid eye disease • Entropion (triage with teleophthalmology if appropriate) • Basal cell carcinoma (triage with teleophthalmology if appropriate) • Lacrimal: Recurrent/low-grade dacryocystitis, canaliculitis. Treat medically first, if requires surgery prefer percutaneous drainage, avoid DCR due to COVID-19 risk • Post-operative simple surgery • Pediatric ptosis with known/high risk of amblyopia (visual deprivation, failed amblyopia therapy) |
• Orbit: all other, including TED (stable mild-moderate) • Other eyelid malpositions: ptosis, brow ptosis, dermatochalasis, ectropion • Some low-risk BCC that has previously been examined (triage with telehealth if appropriate) • Benign periocular tumors (e.g.,chalazion/papilloma) • Lacrimal: All other |
| • Severe unilateral ptosis in an infant • Post-operative complex surgery • Recent trauma including eyelid and canalicular lacerations, orbital fractures and suspected orbital foreign body • Dacryocystocele (pediatric CNLDO with nasal involvement not resolving/acutely infected). Treat medically first, if requires surgery prefer percutaneous drainage, avoid DCR due to COVID-19 risk |
|||
| Surgery | • Surgery for the above | • Surgery for the above | • Surgery for the above |
| Genetics | |||
| New/Follow-up | • Most patients | ||
| Pediatric Ophthalmology | |||
| New/Follow-up | • Sight or potential life (systemic) threatening conditions • Cataracts causing amblyopia or under 4 months old • Reduced vision in both eyes • Reduced vision in one eye under age 7 years • ROP screening • Children on medication (drops or systemic) for glaucoma, uveitis, corneal disease • Post-operative within last 2 months |
• Patients having amblyopia treatment. Where possible, use teleophthalmology • Pediatric oculoplastic/adnexal cases • Reduced vision in one eye over age 7 years. Where possible, use teleophthalmology video/photos to triage • Examination under anesthesia where management is time-sensitive |
• Case by case triage |
| Surgery | • Cataract surgery in under<4 month age or where causing amblyopia • Retinoblastoma treatment • Pediatric glaucoma surgery where conservative therapies have failed • ROP treatment |
||
| Strabismus | |||
| New/Follow-up | • Triage of referrals on a case by case basis (accept suspected neurological strabismus) | • Triage of referrals on a case by case basis (except strabismus where amblyopia management is also required). Where possible, use teleophthalmology | • Most other non-acute strabismus cases |
| Surgery | • Acute trauma-related conditions requiring immediate surgery | • Most strabismus surgery and botulinum muscle injections | |
| Neuro-Ophthalmology | |||
| New/Follow-up | • Patient by patient triage needed (except acute optic neuropathies, suspected SOL or raised intracranial pressure, neurological diplopia, acute pupillary signs) | • Where possible, use teleophthalmology | • Stable patients or patients where management will not change outcomes |
| Surgery | • Optic nerve sheath fenestration for severe visual loss in idiopathic intracranial hypertension, Temporal artery biopsy | ||
**Adapted from the guidelines issued by the Royal Australian and New Zealand College of Ophthalmologists (RANZO)[5]
This diagnosis-based triage can only be done after the patient has been seen by the medical staff. However, if the patient has contacted the call centre of the hospital for an appointment or is met with by the non-medical staff such as the Front Office or Registration Desk before the medical triage, then they may be given a checklist of presenting complaints that may indicate true emergencies. These include the following:
Injury to the eye (chemical, thermal, mechanical)
Sudden loss of vision
Acute pain
Acute red eye
Acute onset of eyelid lesions
Acute onset of double vision or sudden onset of drooping of the eyelid
Acute onset of colored halos, photophobia, floaters or flashes of light
Acute onset of discharge from the eye
Acute or subacute (days to weeks) onset bulging of the eye
Since it may be difficult to keep smaller clinics open throughout the day in the midst of the lockdown, local ophthalmology societies at the district and city level can endeavor to bring ophthalmologists together and suggest time-bound slots for each practice to remain open at different times of the day or one practice open for an entire day by rotation in a given geographical location, or one centralized facility (with ophthalmologists on a roster) open for fixed hours or 24/7 depending on the locally anticipated patient volume. This will help distribute the emergency load on ophthalmologists and will not inconvenience the needy patients who may have genuine ophthalmic emergencies unrelated to the COVID-19 crisis.
Point of entry screening and check-in
Triage should be done by an ophthalmologist or a trained ophthalmic technician or an optometrist.
Telephonic triaging to be done where possible with respect to emergency/ non-emergency nature of visit as well as with respect to possible COVID-19 symptoms. If the condition is deemed an emergency, the patient should be given a specific time to report to the clinic/hospital to avoid crowding. Restrict the entry of children and the elderly (>65 years) into the hospital unless they are patients themselves.
Every hospital/clinic to set up an entry control and screening facility at the point of entry
Personal Protective Equipment (PPE) in the form of surgical caps, surgical scrub suits, three-ply surgical masks/N95 masks and gloves must be provided to the health care workers (HCW) at the point of entry.[6] There should be a security barrier at the entry point so that only the patient and one attendant can enter the hospital.
If there are >3 patients at a time, they should be asked to wait in a designated open area.
At all times, a distance of one meter must be maintained between each patent and between the patient and the hospital staff (except for the HCW who performs point of entry screening).
-
Point of entry screening includes
- Travel screening: Direct questioning for international travel <2 weeks
- Occupational screening: Unprotected occupational contact with COVID-19 patients and/or their contacts
- Contact screening: Contact with a COVID-19 patient or a suspected COVID-19 patient and/or their contacts
- Cluster screening: Cluster with individuals with international travel <2 weeks or contacts of a COVID-19 patient or a suspected COVID-19 patient or their contacts
- Symptom screening: History of fever, cough, breathlessness, loss of smell or acute conjunctivitis in patients or attendants or family members in the last 2 weeks
- Fever screening: Body temperature screening with an infrared non-contact thermometer. Anyone with temperature of 98.6 F (37 C) must be triaged for an ophthalmic emergency with potential loss of vision, eye or life if untreated. Such patients are to be immediately escorted to an isolated waiting area and seen by an ophthalmologist in complete PPE in a pre-designated examination room. In the absence of an ophthalmic emergency, the patient should be referred to a Physician or a COVID-19 Treatment Centre as appropriate.
Once entry screening is passed, the patients and their attendants should be provided with three-ply surgical masks and hand sanitizers (at least 70% alcohol-based) to disinfect their hands before they enter the waiting room. Surgical masks should be worn by everyone who enters the hospital. There should be mandatory hand sanitization at the point of entry
Medical records of all the follow-up patients should be pulled out prior to the patient visit. Formal check-in at the reception desk should be avoided. For new patients, patient information should be collected at the waiting room App-based online or submitted on messaging services such as WhatsApp. If possible, App-based mobile phone check-in and payment should be enabled, without patients having to queue-up at the reception desk
A special consent should be obtained from all the patients which should state as follows: “I declare that during this lockdown and suspension of routine outpatient services and elective procedures in the wake of current COVID-19 pandemic, I have come to the hospital on my own volition for an emergency treatment. If I am an asymptomatic carrier or an undiagnosed patient of COVID-19, I understand that it may endanger fellow patients, doctors and the hospital staff, and that it is my responsibility to take appropriate precautions and to follow the safety protocols prescribed by them. I am also aware that I may contact infection during my visit to the hospital. I will take personal precautions to prevent it, but if I do get infected, I will not hold the doctor or the hospital liable“ and be timed, dated and signed by the patient and the attendant
A daily list of all HCW, patients, their attendants and other hospital visitors with their verified mobile number and verified ID proof should be maintained (for contact tracing if necessary, in the future).
The patient and the attendant are mandated to download the Aarogya Setu COVID-19 tracking App by the Government of India and register with their mobile number for possible future digital tracking of warranted.
Case definitions[7]
A suspected case of COVID-19 as per Indian Council for Medical Research (ICMR) definitions is:
All symptomatic individuals who have undertaken international travel in the last 14 days
All symptomatic contacts of laboratory-confirmed cases
All symptomatic HCW
Asymptomatic direct and high-risk contacts of a confirmed case.
A confirmed case is a person with laboratory confirmation of COVID-19 infection, irrespective of clinical signs and symptoms. Patients meeting the above criteria must be immediately notified to both infection control personnel at your health care facility and your local or state health department for further investigation of COVID-19 as per GoI-ICMR guidelines.
Waiting hall guidelines
Maintain a one meter distance at points where a queue is likely to form – the screening desk, the front office/ registration counter, the billing counter, the pharmacy, etc
Mothers with their infants waiting for Retinopathy of Prematurity (ROP) screening must maintain social distance while infants are undergoing dilatation and screening and during counseling
Keep the waiting room as sparse as possible
Keep the waiting time minimum in the hospital premises
Seating to be arranged in a manner that patients should remain at least 1 meter from each other.
Maintain the unidirectional flow of patients, i.e., entry and exit must be diffirent if there are two doors. Place partitions to separate the movement of patients going in and out of the waiting area
Only one attendant per patient
Coupled, numbered, dated sticker to be given to each patient and his attendant, to disallow tricking of the system
Three-ply face masks for all the patients and their attendants
Provision of hand sanitizers in the waiting hall
Keep open as many doors as possible to avoid touching of doorknobs. Try to follow an open-door and no-AC policy if possible.
Sanitize the waiting hall and most-touched surfaces periodically as follows.
Cleaning of the emergency room and waiting halls
After every 2 hours or 3 patients, the emergency room areas, which come in contact such as doorknobs, handles, silt-lamps (head and chin rest), tables, benches must be cleaned with freshly prepared 1% Sodium Hypochlorite or 1% Bacillocid Extra solution
Every day, the floor and common contact surfaces must be cleaned with 1% Bacillocid Extra solution before work begins and every 2 hours with Lizol
The slit-lamp apparatus, especially the joystick, switches and other parts must be thoroughly cleaned with alcohol wipes
The rooms should be well-ventilated and well lit
All residents/fellows and other HCWs must be instructed to clean and disinfect (using the standard procedure as recommended by the manufacturer) their equipment such as lenses, indirect and direct ophthalmoscopes, pen, and torches, and other such items.
Precautions at ophthalmic evaluation and OPD procedures[8]
Protections for head, mouth, nose, and eye (with a surgical cap, three-ply surgical mask, goggles/face shield) for the examiner and a three-ply surgical mask for the patient. Masks should be changed every 6 hours or immediately when contaminated or wet
Slit-lamp barriers or breath shields. These can be designed indigenously by cutting out a transparent plastic sheet of an appropriate thickness [Fig. 2]. The slit lamp touch-contact parts should be cleaned by alcohol wipes after examining every patient and the barriers should be changed for each patient. Barriers can be washed with soap water, dried and reused
Alcohol-based hand sanitizer before and after examining each patient
Speak as little as possible. The patient should also be informed not to speak during the examination
Disposable gowns, gloves and eye protection, cap and N95 mask are recommended if a procedure is planned that will result in aerosols. Details are provided in Table 2
Avoid dilatation and nasolacrimal syringing if possible. If dilatation is mandatory for a follow-up patient, home dilatation is ideal if there is no known contraindication.
Avoid all aerosol-based procedures including non-contact tonometer (NCT). Use of Tonopen with a disposable tip or Goldmann applanation tonometry (with the cleaning of the applanation cone after every patient) is recommended if IOP measurement is necessary
Refraction can be performed using autorefractor or a streak retinoscope where mandated. Trial frame and the metal rim of the lenses used should be cleaned with alcohol-based sanitizer after use.
Avoid contact lens trial unless therapeutic
Optical dispensing and Pharmacy services should be available, but with 1-meter distancing protocol using distance separators and PPE for the staff (hand sanitizers, three-layer surgical masks and gloves)
Disinfect (using standard protocols) all instruments, and probes used in direct contact to the patient's tear film and ocular surface before re-use as per recommendations given below
The retinal examination should be done in patients who need it, strictly with an indirect ophthalmoscope. Avoid direct ophthalmoscopy and contact lens-based fundus examination
Infants undergoing ROP screening must be placed on a designated crib with a plastic or polythene sheet, by the mother who uncovers the face of the infant and steps away more than 2 meters. The screener walks to the baby and screens (using indirect ophthalmoscopy or a retinal camera). The barrier sheet is replaced or sanitized between successive infants
In case of urgent ophthalmic problems in a patient who is at high risk for COVID-19, eye care is best provided in the multispecialty hospital setting. Transmission precautions for treating ophthalmologists include full-body protection (full PPE or an HIV kit)
In case of urgent ophthalmic problem in a patient with documented COVID-19 or a person under investigation, the patient should remain in the multispecialty hospital setting, ICMR-GoI guidelines should be followed, along with transmission precautions for treating ophthalmologists, including full-body protection (full PPE or an HIV kit)
Patients with conjunctivitis should be seen in a designated OPD room with an isolated waiting room by a designated ophthalmologist. Since conjunctivitis is reported as part of the disease spectrum of COVID-19,[9–12] all patients with conjunctivitis should be COVID-19 suspects and should be examined in isolation, with slit lamp breath shields, using N95 mask and disposable gloves Table 2
All HCW coming in direct patient contact and ophthalmologists should change into surgical scrub suits at the entry to the hospital and change out to street clothes at the exit. They should be encouraged to take a soap bath at once they reach home
All HCW should be encouraged to bring minimum possible personal items to the hospital to minimize seeding at home and vice versa. If needed, items such as food carriers can be carried in a larger outer case that can be easily disinfected
Optimize support staff and HCW allocation (one-third to half of the regular staff per day)
Prophylaxis: ICMR has advised oral Hydroxychloroquine (HCQ) 400 mg BD on day 1, followed by 400 mg OD weekly for 7 weeks.[13] This must be taken only after direct consultation with an internal medicine expert
Keep all undesignated areas of the hospital closed for entry by the patients or the staff.
Digital prescriptions for glasses and medicines, digital medical report and electronic medical records if feasible.
Figure 2.

Breath shield for the slit lamp made using a thick transparent plastic sheet
Table 2.
Recommendations for use or PPE by ophthalmologists based on the COVID-19 status, risk of vision loss, duration of expected contact with a patient and need for aerosol-generating procedures
| COVID-19 status | Risk of life- or sight- threatening harm if not seen urgently (based on triage) | Brief close contact (e.g., slit-lamp examination) | Prolonged close contact (e.g., laser, intravitreal procedures) | Aerosol-generating procedures (e.g., general anesthetic, ophthalmic surgery involving high-speed devices) |
|---|---|---|---|---|
| Asymptomatic | Low | Discharge or postpone until after pandemic or offer remote consultation. | ||
| Asymptomatic | High | Slit-lamp breath shield, Three-ply surgical face mask, Protective goggles, Surgical cap, Surgical scrub suit | Slit-lamp breath shield, Three-ply surgical face mask, Protective goggles, surgical cap, Surgical scrub suit | Slit-lamp breath shield, N95 face mask, Protective goggles, Surgical cap, Disposable sterile gloves, Disposable surgical gown worn over surgical scrub suit |
| Suspected or confirmed COVID-19 | Low | Discharge or postpone until after pandemic or offer remote consultation. | ||
| Suspected or confirmed COVID-19 | High | Isolate the patient Slit-lamp breath shield, N95 face mask, Protective goggles, Surgical cap, Surgical scrub suit, Disposable plastic apron, Disposable gloves | Isolate the patient Slit-lamp breath shield, N95 face mask, Protective goggles, Surgical cap, Surgical scrub suit, Disposable plastic apron, Disposable gloves | Isolate the patient Slit-lamp breath shield, FF3 respirator, Protective goggles, Face shield, Surgical cap, Surgical scrub suit, Disposable plastic apron, Disposable gloves, Disposable shoe cover |
**Adapted from guidelines issued by the Ministry of health and family welfare, Government of India and the Royal College of Ophthalmologists, London[14]
Precautions at diagnostic procedures
Non-essential testing and imaging should be deferred, and equipment used should be kept at a minimum as these can act as fomites, harbor the virus on the surface and act as a nidus of infection to everyone
Gonioscopy and visual field examination should be avoided unless an mandatory
Optical coherence tomography (OCT) and retinal imaging procedures to be done based on ophthalmologist's discretion, preferably only in patients with worsening or progression of retinal disease. Routine examinations should be deferred
All imaging equipment should be cleaned before and after each patient, using the technique recommended by each manufacturer.
Additional precautions at multispecialty hospitals
In a multispecialty hospital, the Ophthalmology department may be classified as “other clinical specialties with limited or no responsibility for critically ill patients“. It is important for the Ophthalmology team to:
Learn about the SOPs of the hospital
Restrict movement to areas of the hospital which are actively involved in the treatment of COVID-19 patients
When called to consult for a patient with suspected COVID-19 or confirmed COVID-19, the ophthalmology team should use PPE as per the hospital/GoI protocols.[6]
Precautions at OR procedures/surgeries[7]
All surgeries must be daycare unless the medical conditions or the Government of India rules (e.g., for plaque brachytherapy) strictly mandate admission. Conditions requiring optional admission are Retinopathy of prematurity, Retinoblastoma, and Congenital glaucoma
Defer all procedures and surgery on a COVID-19 patient until the patient recovers, unless deferral of treatment by 2 weeks has a potential risk for loss of vision, eye, and life. If a procedure or a surgery is mandated, it should be performed in a multispecialty hospital approved by the GoI for COVID-19 treatment and all the HCW involved in the procedure/surgery should have full PPE and possibly HCQ prophylaxis. Develop a dedicated COVID-19 OR to control the spread of the disease - Empty OR of all nonessential materials; consider a negative pressure anteroom with separate access to be used for donning/doffing of PPE; and Separate OR instrument trolley. If a patient requires general anesthesia, a dedicated COVID-19 anesthetist team will be required
Before operating on an asymptomatic suspected COVID-19 patient, testing should be performed. A physician fitness to be obtained for every patient including ruling out airway pathologies, particularly underlying pneumonia. Defer all procedures and surgery by 2 weeks, unless deferral of treatment has a potential risk for loss of vision, eye, and life. If a procedure or a surgery is mandated, it should be performed in a multispecialty hospital approved by the GoI for COVID-19 treatment, and all the HCW involved in the procedure/surgery should have full PPE and possibly HCQ prophylaxis
Air Handling Units (AHU) with increased fresh air exchange. If possible, consider retrofitting dynamic UV and ultrafilters to HEPA, reduce turbulence in OR e.g., minimize opening and closing doors and moving machines
Screening chest X-ray for all patients for surgery
Avoid surgeries off-hours or with an incomplete team
Faculty or senior fellows or senior residents should preferably do the surgery – quick and safe surgery is warranted
Choose the quickest possible surgical procedure
Try to avoid GA unless mandatory
Prefer topical anesthesia over local anesthesia
PPE for all OT staff as per guidelines in Table 2
All universal precautions as usual
Minimum number of staff in the OT
Stop positive ventilation in theatre during the procedure if feasible and for at least 20 minutes after the patient has left the theatre
Smoke evacuation for diathermy
Aerosol generating procedures such as intubation, extubation, bag masking, electrocautery should be done by the anesthetist and the surgeon while wearing full personal protective equipment
If emergency phacoemulsification is required, after triage as given in Table 1, it should be assumed that phacoemulsification with excess BSS near the vibrating tip can generate aerosols. Considering there are a few reports of 2019-n-CoV in tears,[11] a clear plastic sheet over the surgical area to catch any generated aerosols is recommended. Additional PPE as recommended in Table 2 should be used
No two patients should be handled together. There should be a 20-min time out between each surgery
Protocol-based disinfection of the OT should be done after each surgical procedure.
Personal protective equipment (PPE)
PPEs are protective gear designed to safeguard the health of workers by minimizing the exposure to a biological agent.[6] Components of PPE are goggles, face-shield, mask, gloves, coverall/gowns (with or without aprons), head cover and shoe cover. Table 2 shows recommendations for use of PPE by ophthalmologists based on the COVID status, risk of vision loss, duration of expected contact with the patient and need for aerosol-generating procedures.
There is a lot of confusion regarding the need or otherwise of PPE to examine quarantined patients kept in an isolated area of the eye clinic/hospital, most of whom are asymptomatic patients with no fever or cough but recently visited hot spots in the country or outside. The American Academy of Ophthalmology does not recommend PPE for this step.[3] However, authorities in Singapore, Hong Kong, and others insist on the use of PPE for these patients.[15] Considering the scarcity of PPE, this expert panel feels that the full PPE kit is best reserved for actually treating COVID or suspect cases rather than for asymptomatic subjects returning from hot spots. In these cases, examination with N95 masks and gloves should be enough coupled with one meter distancing as far as possible, minimizing conversations and hand hygiene after the examination is over. Similar recommendations are made for the hospital staff other than ophthalmologists involved in the OPD and OR settings.[6] Table 3 summarizes these recommendations.
Table 3.
Recommendations for use of PPE for hospital staff**
| Setting | Activity | Risk | Recommended PPE | Comments |
|---|---|---|---|---|
| Entry Screening | Screening patients and attendants with non - contact thermometers | Moderate Risk | Surgical cap, Surgical scrub suits, Three-ply surgical face mask, Disposable gloves | A minimum distance of one meter needs to be maintained between patients. |
| Waiting area staff such as triaging ophthalmologist, receptionist, optometrist, nurse | Interviewing patients, refraction, dilatation, scanning, etc. | Low risk | Three-ply surgical face mask, Disposable gloves | A minimum distance of one meter needs to be maintained between patients. |
| Sanitary staff | Cleaning frequently touched surfaces/Floor/cleaning linen | Moderate risk | Surgical cap, Surgical scrub suits, Three-ply surgical face mask, Disposable gloves | |
| Administrative staff not exposed to patients | Providing administrative support | No Risk | Three-ply surgical face mask | No contact with patients of COVID-19. They should not venture into areas where a suspect COVID-19 cases are being managed |
| Staff attending to all patients alongside ophthalmologists | Same PPE recommendations as shown in table 2 | |||
**Developed as per recommendations of the Ministry of health and family welfare, the government of India
Infection control and prevention measures[7]
Hand hygiene: HCW should perform hand hygiene using alcohol-based hand rub (minimum 20 seconds) or by washing with soap and water (minimum 20 seconds). If hands are visibly soiled, use soap and water for hand wash. Hand hygiene should be performed frequently, before and after examination of a patient
-
Mask and PPE etiquette
- Appropriate use and disposal of masks and PPE is essential to ensure they are effective and to avoid any increase in the risk of transmission associated with their incorrect use and disposal
- Place the mask carefully to cover mouth and nose and tie securely to minimize any gaps between the face and the mask. Wear the PPE as instructed by experts.
- While in use, avoid touching the mask
- Remove the mask by using the appropriate technique (i.e., do not touch the front but remove the lace from behind)
- Remove PPE in the reverse order that it was worn and discard the material in appropriately colored disposal bags for infective plastic items (red)
- Do not reuse or use three-ply surgical mask/N 95 masks for more than 8 hours. If using the same mask while examining multiple patients, transmission to the patient must be avoided by not touching the front of the mask. Additionally, do not allow the mask to hang down on shirt/clothing when not examining patients
- Mask and PPE etiquettes should be followed by hospital staff as well.
Environmental hygiene: Environmental cleaning is part of standard precautions, which should be applied to all patients in all healthcare facilities. Ensure that cleaning and disinfection procedures are followed consistently and correctly. Freshly prepared 1% Sodium Hypochlorite or 1% Bacillocid Extra solution can be used as a disinfectant for cleaning and disinfection for ophthalmic instruments between patients. Leaving the solution for a contact time of at least 10 minutes is recommended. Alcohol (e.g., isopropyl 70% or ethyl alcohol 70%) can be used to wipe down surfaces where the use of bleach is not suitable, e.g., metals. The slit lamp contact surfaces should be cleaned after every patient. Disinfection of high touch surfaces like (doorknobs, telephone, call bells, bedrails, stair rails, light switches, wall areas around the toilet) should be done every 2 hours. For low-touch surfaces (walls, mirrors, etc.), mopping should be done at least once daily
OPD areas and the OT are fumigated with 2% Bacillocid Special at the end of every day
UV sterilizer lights may be installed in all the areas used for patient care and switched on for 3 hours at the end of all patient care activities.
Use of smaller elevators (base< 10 sft) should be restricted to two people at a time and larger elevators to 2 persons per 10 sft base area.
Follow an open door, non-AC environment if feasible.
Avoid all outreach activities including community screening camps.
Techniques of donning and doffing PPE and disposal, and sensitize them in personal hygiene measures and physical distancing.
Guidelines for maintenance of equipment
Equipment maintenance to be done once a week by trained OT Technicians
All ACs, AHU, dehumidifiers to be switched on at least twice a week
All OPD and OT machines, other than Excimer and Femtosecond laser machines, to be switched on for a minimum of 15 minutes twice a week. All the OT equipment should be maintained as recommended by the manufacturer. It may be ideal to prime and run phacoemulsification machine and vitrectomy machine once in 3 days. It is advisable that all equipment be connected to UPS to avoid power surge related damage in these times when electricity flow can be erratic
Excimer and Femtosecond laser machines need to be calibrated and tested at the end of the lockdown period and before any patient is posted for these procedures. It will be prudent to discuss maintenance guidelines with the specific manufacturer and systematically shut down if possible
All batteries in remotes, ophthalmoscopes, retinoscopes, etc. should be removed
For OCT, topographers, etc. all printers need to be given one print command as test print at least once a week
After all daily exercise is over for the day, all the equipment should be shut down properly and covered. All AC's, AHU and dehumidifiers should be switched off before leaving the center for the day. Night mode of the Air-handling Unit should be activated (if such a setting is available) if the OT is infrequently used.
All lasers, including Nd: YAG and retina lasers, will need to fire for 50 blank spots at least once a week
IT-related equipment such as servers, computer terminals, and UPS should be checked physically once a week.
Telemedicine[16]
Ophthalmologists should make use of telemedicine facilities for their patients wherever possible
The ophthalmologists should follow the AIOS guidelines and make sure they are aware of all the procedures to be followed when dealing with patients using telemedicine such as informed consent, prescription, sharing of photographs, and other aspects[17]
The doctors can make sure of facilities such as video-conferencing with other referring doctors and general practitioners
Telemedicine practice should be widely advertised on social media and other platforms so that it reaches to peers and patients.
Guidelines for the staff and duty rosters
It is important that the Heads of the Institutes/Directors prepare a duty roster for all HCWs including doctors, nurses, and paramedical staff so that only one-third to one-half staff is working at any given time[18]
This practice will ensure the availability of manpower if the need arises in the future
The residents and fellows must be also given specific duties so that all of them do not enter the hospital and crowd the emergency/OPD areas. Only necessary staff, optometrists and nurses must be called
If any HCW, faculty, resident or fellow has any travel history to international/national conferences in areas that bring high risk, or has developed symptoms, or has a family member with symptoms, they should be strictly quarantined and the nearest authorities should be informed immediately
The residents/fellows and other HCW must be given adequate moral support in this time of crisis
It is important to circulate positive messages and counsel staff and doctors working in your institute so that they maintain a positive outlook and take care of their family members.
All the staff should sanitize their hands with alcohol-based hand sanitizer before entering the hospital. Touch points should be minimal. Finger print biometry login and staff check-in should be replaced with non-touch modes.
All the staff should be screened at the point of entry for fever and explicitly asked for symptoms, international travel, COVID-19 patient/suspect contact or clustering
All the staff who come in direct contact with the patient should change into clean surgical scrubs at entry and change out at exit. They should be encouraged to take a soap bath at home.
All the staff should strictly practice hand hygiene before and after physical contact with each patient.
Teaching activities at hospitals
It is mandatory that all teaching hospitals and institutes discourage and stop lectures in classes/closed rooms or halls
Any teaching activity can be performed using online portals such as web meetings, Skype, Zoom, and other mobile apps
Bedside teaching and rounds must be strictly forbidden.
Residents and fellows must be encouraged to utilize the time during this pandemic to study theory and prepare for their future examinations, and focus on research activities that can be performed from home
All residents and fellows must be advised to learn from online material and read from e-journals.
Resumption of Work after the Lockdown is Lifted
Since there are no governmental guidelines as to how quickly the restrictions will be lifted, it is difficult to provide guidelines on how to proceed with routine OPD and surgical work. However, it is certain that, after the lockdown is lifted, the viral infection will still be prevalent in the population and health care workers, especially ophthalmologists and others who come in close contact with patients will continue to be at increased risk of contracting the infection unless some precautions are continued to be taken. A lot of the OPD and OR procedures can be adapted for routine use irrespective of a pandemic, and we encourage ophthalmologists to do so. Additionally, most of the measures mentioned above to be adopted during the lockdown could be continued even after the lockdown is gradually lifted till such time as active cases exist in the country and threat of virus spread is relatively high.
It is advisable that for healthy patients with no history of COVID-19 infection in the past, no COVID-19 suspicion as per definitions given above and are asymptomatic, the following measures be taken in OPD till such time as the pandemic has abated and safety norms are lifted by government agencies, or a proven drug or vaccine has been established for effective management:
Appointments to be spaced out to avoid hall congestion; if necessary extend the work hours to cater to the increased volume, but avoid congestion
Remote patient check-in and payment if feasible
All Point of Entry screening and sanitization measures will continue
All waiting hall precautions will continue
Disposable three-ply masks for all HCW who come in direct contact with patients and the patients and attendants
All hand and personal sanitization measures to continue
All slit lamps should have breath shields
Minimum conversation with patient /colleagues should continue
Any patient with conjunctivitis to be taken directly to an isolated room and be directly seen by a doctor wearing a PPE. Treatment for conjunctivitis alone will be instituted and no other tests (including visual acuity testing) will be done. If the redness is not due to conjunctivitis, they will join the other patients for examination and treatment
Instrument cleaning protocols should be maintained as described during the lockdown
For a patient with suspected COVID-19, use a separate OPD room with an isolated waiting area. The OPD room should not be with positive pressure. N95 mask to be provided for HCW engaged in patient examination and management. Examination protocols are mentioned above. Sanitize the room after patient exits and the next such patient to be examined after 20 minutes gap. HCW to change gloves for each examination.
Routine surgical procedures may be initiated based on the triage where those labeled as urgent [Table 1] can be taken up for surgery sooner than later. However, this expert panel feels that all elective surgeries such as phacoemulsification, refractive surgeries, etc. may be avoided in the first 4 weeks after the lockdown is lifted. We may ease our way into these procedures after the situation proceeds towards normalcy and Government directives are clearer. If the OT has been unused for a prolonged time (>72 hours). fumigation as per the standard protocol and negative microbiological cultures from standard key locations are mandatory before restarting surgery. All the surgical instruments should be sterilzied and all the equipment should be cleaned and disinfected/sterilized as per the manufacturers' recommendation. If a rapid COVID-19 screening test becomes universally available and is affordable and is permitted by the Government of India, it can be included in the panel of pre-operative screening. However, it is premature to form definite guidelines at this time and we must use our own discretion while planning elective procedures in such volatile times.
Discussion
The COVID-19 infection has led to an unprecedented number of infections and deaths in recent times and continues to pose a colossal challenge to the health care system.[19] Ophthalmologists are at a slightly higher risk of transmission due to their close contact with patients,[20,21] tears[11] as well as procedures that generate aerosols. It is important to triage patients effectively, using preferred practices and recommendations given by this expert panel so that genuine emergencies can be tackled effectively and efficiently without facilitating disease transmission. We provide clear guidelines on the use of PPE in the ophthalmic setup and emphasize that, due to their paucity, these be reserved specifically for those who are catering to COVID-19 positive cases with severe illness. Precautions to be taken during OPD and surgical services, both during and after the lockdown have been elucidated. We hope that these guidelines become the preferred practices of all ophthalmologists in India and around the globe where they may be applicable.
Conclusion
The fight against the SARS-CoV-2 virus appears to be a long one. Using preferred practices as far as possible will help us prevail in these difficult times. Triage based on the severity of the ophthalmic disease and COVID-19 status, appropriate and judicious use of masks and other PPE, social distancing, sanitization along with other mandatory precautions mentioned in this paper should help Indian ophthalmologists in performing their professional responsibilities without being the foci of disease transmission.
Disclaimer
The expert panel would like to declare that this document contains guidelines based on the information issued by various relevant organizations, and State and Central Governments as on the date of their release. These guidelines are provided for informational and educational purposes only. Adherence to any recommendations included in this document may not ensure a successful outcome in every situation. Furthermore, the recommendations contained in this document should not be interpreted as setting a standard of care or be deemed inclusive of all proper methods of care nor exclusive of other methods of care reasonably directed to obtaining the same results. These guidelines reflect the best available information at the time the document was prepared. The results of future studies may require revisions to the recommendations to reflect new data. The guidelines do not replace or override existing national/regional/local statutory requirements. The guidelines are to be tempered with the regional, local and individual hospital guidelines and expertise. The ultimate judgment regarding the propriety of any specific therapy must be made by the physician and the patient considering all the circumstances presented by the individual patient, and the known variability and biological behavior of the medical condition. This expert panel does not warrant the accuracy or completeness of the guidance and assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this guidance or for any errors or omissions. We will not be a party to for medico legal implications arising out of following or not following these recommendations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Honavar SG, Sharma N, Sachdev MS for the Governing Council of the All India Ophthalmological Society. AIOS-Operational-Guidelines-COVID19. [Last accessed on 2020 Apr 04]. Available from: https://aios.org/pdf/AIOSOperational-Guidelines-COVID19.pdf .
- 2.Khanna RC, Honavar SG. All eyes on Coronavirus—What do we need to know as ophthalmologists. Indian J Ophthalmol. 2020;68:549. doi: 10.4103/ijo.IJO_516_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chodosh J, Holland GN, Yeh S. Important coronavirus updates for ophthalmologists. [Last accessed on 2020 Apr 04]. Available from: https://wwwaaoorg/headline/alert-important-coronavirus-context .
- 4.Ministry of Health and Family Welfare, Govt of India. Advisory for Hospitals and Medical Education Institutions. [Last accessed on 2020 Apr 04]. Available from https://www.mohfw.gov.in/pdf/AdvisoryforHospitalsandMedicalInstitutions.pdf .
- 5.RANZCO COVID-19 Triage Guidelines. 2020. [Last accessed on 2020 Apr 04]. Available from: https://ranzco.edu/policies_and_guideli/11661/
- 6.Ministry of Health and Family Welfare, Govt of India, Directorate General of Health Services. Novel Coronavirus Disease 2019 (COVID-19): Guidelines on rational use of Personal Protective Equipment. [Last accessed on 2020 Apr 04]. Available from: https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf .
- 7.Ministry of Health and Family Welfare, Government of India. Guidelines for notifying COVID-19 affected persons by Private Institutions. [Last accessed on 2020 Apr 06]. Available from: https://www.mohfw.gov.in/pdf/GuidelinesfornotifyingCOVID-19affectedpersonsbyPrivateInstitutions.pdf .
- 8.Ministry of Health and Family Welfare, Government of India. NATIONAL GUIDELINES FOR INFECTION PREVENTION AND CONTROL IN HEALTHCARE FACILITIES. [Last accessed on 2020 Apr 04]. Available from: https://www.mohfw.gov.in/pdf//National%20Guidelines%20for%20IPC%20in%20HCF%20-%20final%281%29.pdf .
- 9.Mungmungpuntipantip R, Wiwanitkit V. Ocular manifestation, eye protection, and COVID-19 [published online ahead of print, 2020 Mar 30] Graefes Arch Clin Exp Ophthalmol. 2020 doi: 10.1007/s00417-020-04662-3. doi: 101007/s00417-020-04662-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li JO, Lam DSC, Chen Y, Ting DSW. Novel Coronavirus disease 2019 (COVID-19): The importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104:297–8. doi: 10.1136/bjophthalmol-2020-315994. [DOI] [PubMed] [Google Scholar]
- 11.Liang L, Wu P. There may be virus in conjunctival secretion of patients with COVID-19 [published online ahead of print, 2020 Mar 18] Acta Ophthalmol. 2020 doi: 10.1111/aos.14413. doi: 101111/aos14413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (COVID-19) in Hubei Province, China [published online ahead of print, 2020 Mar 31] JAMA Ophthalmol. 2020:e201291. doi: 10.1001/jamaophthalmol.2020.1291. doi:101001/jamaophthalmol20201291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ministry of Health and Family Welfare, Government of India. Advisory on use of hydroxy-chloroquine as prophylaxis ofor SARS-CoV-2. [Last accessed on 2020 Apr 04]. Available from: https://www.mohfw.gov.in/pdf/Advisoryontheuseof HydroxychloroquinasprophylaxisforSARSCoV2infection.pdf .
- 14.Royal College of Ophthalmologists. PPE and staff protection requirements for ophthalmology. [Last accessed on 2020 Apr 04]. Available from: https://wwwrcophthacuk/wp-content/uploads/2020/04/PPE-and-staff-protection-requirements-for-ophthalmology-Principlesdocx-1pdf .
- 15.Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: An experience from Hong Kong [published online ahead of print, 2020 Mar 3] Graefes Arch Clin Exp Ophthalmol. 2020 doi: 10.1007/s00417-020-04641-8. doi: 101007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ministry of Health and Family Welfare, Govt of India. Telemedicine Practice Guidelines. [Last accessed on 2020 Apr 04]. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf .
- 17.AIOS Governing Council. AIOS Telemedicine Practice Guidelines. [Last accessed on 2020 Apr 04]. Available from: https://aios.org/pdf/AIOS-Telemedicine-Practice-Guidelines.pdf .
- 18.Ministry of Health and Family Welfare, Govt of India. SOP for reallocation of residents/ PG students and nursing students as part of hospital management of COVID. [Last accessed on 2020 Apr 04]. Available from: https://www.mohfw.gov.in/pdf/COVID19SOPfordoctorsandnurses.pdf .
- 19.Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis [published online ahead of print, 2020 Mar 12] J Med Virol. 2020 doi: 10.1002/jmv.25757. doi: 101002/jmv25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qing H, Li Z, Yang Z, Shi M, Huang Z, Song J, et al. The possibility of COVID-19 transmission from eye to nose [published online ahead of print, 2020 Mar 18] Acta Ophthalmol. 2020 doi: 10.1111/aos.14412. doi: 101111/aos14412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seah I, Agrawal R. Can the Coronavirus Disease 2019 (COVID-19) Affect the Eyes? A Review of Coronaviruses and Ocular Implications in Humans and Animals [published online ahead of print, 2020 Mar 16] Ocul Immunol Inflamm. 2020;28:391–5. doi: 10.1080/09273948.2020.1738501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vinekar A, Azad RV, Dogra MR, Jalali S, Bhende P, Narendran V, et al. for the Indian Retinopathy of Prematurity Society. Retinopathy of Prematurity screening and treatment guidelines during the COVID-19 lockdown. 2020. [Last accessed on 2020 Apr 05]. Available from: https://sitesgooglecom/view/iropsociety/newsroomauthuser=0 .