Abstract
Purpose:
To compare the visual outcome, safety, safety index, efficacy, efficacy index and corneal transparency between single-step transepithelial photorefractive keratectomy (t-PRK) and conventional photorefractive keratectomy (PRK) with manual debridement of epithelium in eyes with low to high simple myopia and compound myopic astigmatism.
Methods:
In this retrospective ,case control study, we analysed and compared the postoperative uncorrected visual acuity(UCVA), postoperative best corrected visual acuity (BCVA) , safety, safety index,efficacy,efficacy index and the corneal transparency between t-PRK and PRK with 6th-generation Amaris excimer 500E laser (Schwind eye-tech-solutions) in 115 eyes of 59 patients.
Results:
Preoperative Mean Refractive Spherical Equivalent (MRSE) was - 3.88 + 0.23 Diopters(D) and -4.73 + 0.23D in PRK and t-PRK group respectively(p=0.09). In both the groups , none of the eyes lost postoperative BCVA at the end of mean follow-up period of 3.5 months . All the eyes achieved post operative UCVA of 20/40 or better in both the groups. Incidence of trace corneal haze was high in t-PRK group at the end of 3.5 months (P = 0.003).
Conclusion:
Single-step t-PRK and PRK provide similar results at the end of mean follow-up period of 3.5 months postoperatively with regards to post-operative UCVA, post operative BCVA, safety, safety index, efficacy and efficacy index. There was high incidence of trace haze in t- PRK eyes. Both the procedures are predictable, effective, and safe for correction of low to high myopia.
Keywords: Haze, Myopia, Myopic Astigmatism, Photo Refractive Keratecctomy, Trans PRK
Photorefractive keratectomy (PRK) is a surface ablation procedure which can correct myopia and myopic astigmatism. The procedure causes more postoperative pain, delayed epithelial healing, and stromal haze, when compared to Laser in situ keratomileusis (LASIK).[1,2,3] However, because of the flap-related complications of LASIK, surface ablation techniques are preferred by many surgeons.[4] Previously, in surface ablation, the epithelium was removed manually (PRK), before the excimer laser application. Later, a technique of alcohol-assisted epithelium removal, known as, laser-assisted sub-epithelial keratectomy (LASEK) was introduced. Epi-LASIK (Epipolis) is a similar kind of procedure, where a blunt oscillating blade (epikeratome) is used to make the epithelial flap.[5]
In the late 1990s, transepithelial PRK (t-PRK) was introduced, in which the epithelium is removed by phototherapeutic keratectomy (PTK), followed by the conventional PRK for stromal ablation.[6,7,8] Recently, a new variant of t-PRK, that is, single-step t-PRK, was introduced with the advancement in lasers, ablation algorithms, and nomograms. In this, excimer laser ablates the corneal surface and stroma in a single-step with a single ablation profile. Few studies, which compared single-step t-PRK and surface ablation with alcohol, have reported variable outcome results.[9,10,11]
In our study, we compared the refractive outcomes, safety, safety index, efficacy, efficacy index, and corneal transparency at the end of mean follow-up of 3.5 months, in simple myopia and compound myopic astigmatism eyes with preoperative MRSE ranging from –1.00 D to –7.00 D and –0.75 D to –7.75 D in PRK and t-PRK group respectively, performed with 6th-generation Amaris excimer 500E laser (Schwind eye-tech-solutions).
Methods
In this retrospective, observational, non-randomized, case-control study, patients were divided into two groups based on the procedure they underwent, that is, either single-step t-PRK or conventional PRK between April 2015 and October 2017. Written informed consent was obtained from all the patients. The study was approved by the Institutional Review Board (IRB). All consecutive patients, who underwent t-PRK or conventional PRK and had a minimum follow-up of 3–4 months (mean follow-up of 3.5 months), were enrolled for the study. t-PRK was performed in the patients, who had an epithelial thickness between 53 and 58 microns, measured with RTVue XR 100 anterior segment optical coherence tomography (AS-OCT). Conventional PRK was performed when the epithelial thickness was either below 53 microns or above 58 microns. All surgeries were performed by two surgeons (AKG, AS). Both eyes were operated under topical anesthesia, in a single session. Myopia was grouped as mild (MRSE is between 0 and −3.00 D), moderate (MRSE is between −3.01 D and −6.00 D), and high (MRSE is -6.01 D and above).[12] A total of 115 eyes of 59 patients were included among which 67 eyes underwent t-PRK and 48 eyes underwent PRK.
Preoperative examination
Detailed systemic and ocular history, history of contact lens usage, and systemic medications were obtained from all the patients. All patients had a complete preoperative eye examination, which included UCVA, BCVA, Manifest refraction (MR), slit-lamp evaluation of the anterior segment, fundus examination, intraocular pressure (IOP) with Goldmann applanation tonometer, tear function using Schimer's test without corneal anesthesia, corneal topography using Sirius topographer (SCHWIND eye-tech-solutions GmbH, Kleinostheim, Germany). Soft contact lenses were discontinued for a minimum of 1 week and hard contact lenses for a minimum of 4 weeks before the examination or till the refraction and topography became stable. Patients were advised to instil moxifloxacin hydrochloride 0.5% eye drops every third hourly 1 day prior to the surgery in the eye to be operated.
Surgical technique
In both groups, all surgeries were performed with 6th-generation Amaris excimer laser, version 500 E (Schwind eye-tech-solutions). ORK-CAM software was used to calculate the aberration free algorithms, which are used for the ablation. Both the surgeons followed the same surgical protocol. All the refractive errors were treated with an aim to achieve postoperative UCVA equal to that of preoperative BCVA. Prior to the surgery, proparacaine hydrochloride 0.5% eye drops was instilled, eye was draped, and a closed-loop lid speculum equipped with suction was placed between the lids. One drop of proparacaine hydrochloride 0.5% eye drops was instilled again in conjunctival cul de sac and was thoroughly irrigated with balanced salt solution (BSS). In the conventional PRK group, around 8 mm diameter of the epithelium was manually debrided in a centripetal fashion using a hockey stick blade and the stromal ablation was done. In the group undergoing single-step t-PRK, the epithelium and stroma were ablated in a single-step using the transepithelial PRK nomogram. This software module, based on a spherical ablation profile, automatically considers the ablation volume of the epithelium.[13] It applies an epithelial thickness profile that is thinner with 55 μm at the centre and 65 μm at the periphery and delivers different ablation energy to the epithelium and stroma.[10]
In most of the patients, 6.50 mm was taken as the optical zone. In eyes with high astigmatism, 7 mm was taken as the optical zone, as per the machine recommendation. The transition zone was calculated by the software of the machine. The laser treatment was centered on the vertex of cornea. After the ablation in both groups, limbus was protected with viscoelastic. The ablated area was soaked with 0.02 mg% (0.2 mg/ml) of mitomycin-c (MMC), 10 s for each dioptre. Later, the stromal bed was thoroughly washed using BSS. A bandage contact lens (BCL) with 38% H2O content (ACUVUE OASYS, Johnson and Johnson vision care) was placed on the cornea and a drop of topical moxifloxacin hydrochloride 0.5% was instilled.
Postoperative care
Patients were given topical fluorometholone 0.1% 4 times a day, moxifloxacin hydrochloride 0.5% 4 times a day, lubricating eye drops every second hourly. Oral analgesics were prescribed to relieve the postoperative pain on as and when required basis.
Epithelial healing was assessed on the slit lamp. After complete epithelial healing, BCL was removed. Antibiotic eye drops were discontinued after 2 days of removal of BCL. Steroid eye drops were tapered over a period of 2, 3, and 4 months in mild, moderate, and high refractive error, respectively.[14] Patients were followed up at 1 week to 10 days, 1 month ± 2 weeks, and at 3–4 months. All patients were advised to wear ultraviolet protective glasses for a period of 6 months and comprehensive eye examination was carried out at each visit which included UCVA, BCVA, MR, IOP, and grading of corneal haze on slit lamp. Postoperatively, visual acuity was converted to Logarithm of Minimum Angle of resolution (LogMAR) for statistical analysis and refractive outcomes were analyzed at the end of mean follow-up of 3.5 months.
Definitions and cutoff values
Safety was defined as the number and the percentage of eyes losing two or more lines of preoperative BCVA.
Safety index is the ratio of mean postoperative BCVA over mean preoperative BCVA. Cutoff level was set at 0.85 to determine the success at last follow-up.
Efficacy was defined as percentage of eyes with postoperative UCVA of Log MAR 0.30 (20/40) and better.
Efficacy index is the ratio of the mean postoperative UCVA to the mean preoperative BCVA. Cutoff value was set at 0.80 to determine the success at last follow-up.[12,15]
Grading of corneal haze
Slit-lamp grading of Corneal Haze:
Grade 0 No haze, completely clear cornea
Grade 0.5 Trace haze seen with careful oblique illumination
Grade 1 Haze not interfering with visibility of fine iris details
Grade 2 Mild obscuration of iris details
Grade 3 Moderate obscuration of the iris and lens
Grade 4 Complete opacification of the stroma in the area of the scar, anterior chamber is totally obscured.[16]
Statistical analysis
Data were analyzed using R software version 3.2.0. We reported percentages for all categorical variables and mean ± SD for continuous variables. Independent t-test was used to compare continuous variables between PRK and t-PRK groups, and the Fisher's exact test was used to compare differences in categorical variables between the two groups. Statistical significance was set at P ≤ 0.05.
Results
Out of the 115 eyes, 48 eyes underwent PRK and 67 eyes underwent t-PRK. Preoperative variables are shown in Fig. 1 and Table 1. The mean age was 26 ± 4 years in PRK group and 26 ± 6 years in t-PRK group (P = 0.998). In PRK group, 23 (47%) were females whereas in t-PRK group 50 (73%) were females (P = 0.0006). Mean preoperative MRSE was –3.88 ± 0.23D and –4.73 ± 0.23D in PRK and t-PRK group, respectively (P = 0.09). No intraoperative complications were noted.
Figure 1.
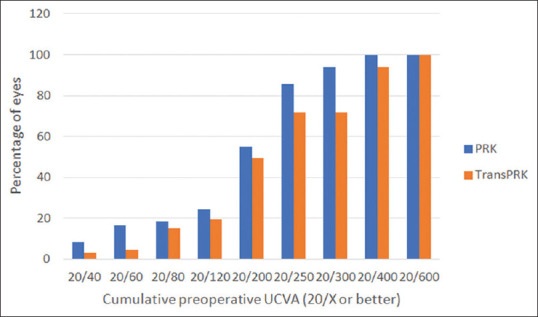
Preoperative Cumulative Uncorrected Visual Acuity (UCVA)
Table 1.
Preoperative Variables
| PRK | t-PRK | P | |
|---|---|---|---|
| Mean Age (Years) | 26±4 | 26±6 | 0.99 |
| Mean MRSE* (Diopters) | -3.65 | -4.5 | 0.09 |
| PRK (n†) | t-PRK (n) | P | |
| Sex | |||
| Females | 23 (47%) | 49 (73%) | 0.0006 |
| Males | 25 (53%) | 18 (27%) | |
| PRK (n) | t-PRK (n) | P | |
| Preoperative MRSE | |||
| 0.5-3.0 D | 15 (31%) | 15 (22%) | 0.09 |
| 3.01-6.0 D | 25 (53%) | 29 (43%) | |
| >6.01 D | 8 (16%) | 23 (34%) | |
*Mean Refractive Spherical Equivalent, †No of Eyes
At the end of 1 week to 10 days, 46 out of 48 eyes (95%) in PRK and 66 out of 67 eyes (99%) in t-PRK group had achieved UCVA of 20/40 or better, but the difference was not statistically significant (P = 0.19) [Table 2]. At the end of 1 month ± 2 weeks, 2 eyes (3%) in the t-PRK group and none among PRK group achieved UCVA of 20/16, whereas all the 47 eyes (100%) in PRK group and 68 eyes (100%) in t-PRK group achieved UCVA of 20/40 or better. Again, this observation was of no statistical significance (P = 0.64). Four eyes (8%) in PRK group and 6 eyes (9%) in t-PRK group achieved UCVA of 20/16 at the end of mean follow-up of 3.5 months, with no significant difference between the two groups (P = 0.18). Results on postoperative safety are shown in Table 3. None of the eyes in both groups lost >/=2 lines of preoperative BCVA (P = 0.18). All the eyes in both the groups achieved postoperative UCVA of 0.30 Log MAR (20/40 Snellen's equivalent) or better at the end of mean follow-up of 3.5 months (P = 0.18) [Fig. 2]. All the eyes achieved UCVA of 20/20 or better in PRK group, whereas in t-PRK group 61 eyes out of 67 eyes achieved UCVA of 20/20 or better. Other six eyes achieved BCVA of 20/20 with postoperative MRSE between +0.5 and –0.50 D.
Table 2.
Postoperative UCVA‡ in Log MAR scale (Snellen’s Equivalent) at follow-up visits
| PRK (n) | t-PRK (n) | P | |
|---|---|---|---|
| 1 week-10 days | |||
| -0.12 (20/16) | 0 | 2 (3%) | 0.19 |
| 0.00 (20/20) | 20 (42%) | 40 (60%) | |
| 0.18 (20/30) | 20 (41%) | 20 (30%) | |
| 0.30 (20/40) | 6 (12%) | 4 (6%) | |
| 0.48 (20/60) | 1 (2%) | 1 (1%) | |
| 0.78 (20/120) | 1 (2%) | 0 | |
| PRK (n) | t-PRK (n) | P | |
| 1 month +/- 2 weeks | |||
| -0.12 (20/16) | 0 | 2 (3%) | 0.64 |
| 0.00 (20/20) | 38 (80%) | 55 (82%) | |
| 0.18 (20/30) | 8 (16%) | 9 (13%) | |
| 0.30 (20/40) | 2 (4%) | 1 (1%) | |
| PRK (n) | t-PRK (n) | P | |
| 3.5 months | |||
| -0.12 (20/16) | 4 (8%) | 6 (9%) | 0.18 |
| 0.00 (20/20) | 44 (92%) | 55 (82%) | |
| 0.18 (20/30) | 0 | 5 (7%) | |
| 0.30 (20/40) | 0 | 1 (1%) | |
‡Uncorrected Visual Acuity
Table 3.
Postoperative Safety and Efficacy
| PRK (n) | t-PRK (n) | P | |
|---|---|---|---|
| Safety (3.5 Months) | |||
| Yes§ | 48 (100%) | 67 (100%) | 0.18 |
| No|| | 0 | 0 | |
| Efficacy (3.5 months) | |||
| Y¶ | 48 (100%) | 67 (100%) | 0.18 |
| N** | 0 | 0 |
§Lost </=1 line of preoperative Best Corrected Visual Acuity (BCVA), ||Lost 2 lines of preoperative BCVA, ¶Postoperative Uncorrected Visual Acuity (UCVA) of 20/40 and better. **Postoperative UCVA of worse than 20/40
Figure 2.
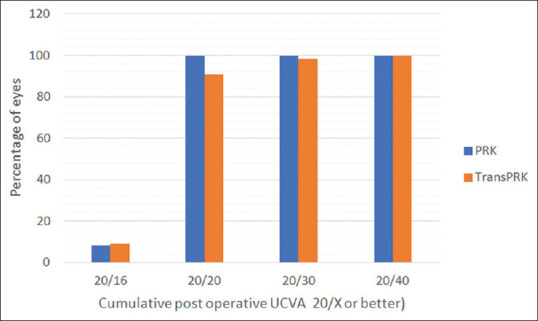
Postoperative Cumulative Uncorrected Visual Acuity (UCVA)
Safety index value below 0.85 indicate that there is loss of two or more lines. Loss of two lines indicate lack of success regarding the safety of these procedures. Efficacy Index value below 0.80 indicate loss of more than two lines. Loss of more than two lines indicate lack of success regarding the efficacy of these procedures. As shown in Table 4, safety index and efficacy index were both ≥0.99 for both the groups.
Table 4.
Safety Index (SI) and Efficacy Index (EI)
| PRK | t-PRK | |
|---|---|---|
| SI†† | 0.99 | 0.99 |
| EI‡‡ | 0.99 | 1.00 |
††Mean postoperative BCVA/Mean preoperative BCVA. ‡‡Mean postoperative UCVA/Mean preoperative BCVA
Sub-analysis of postoperative variables in mild, moderate, and high myopic groups in PRK and t-PRK are shown in Table 5. Visual recovery in the sub-group of moderate myopia among PRK and t-PRK group at the end of 1 week to 10 days was faster and was statistically significant (P = 0.01). Other postoperative parameters (UCVA at 1 month ± 2 weeks, UCVA at mean follow-up of 3.5 months, BCVA at mean follow-up of 3.5 months) among both the sub-groups was not statistically significant [Table 5].
Table 5.
Sub-analysis of mild, moderate and high myopic groups comparing postoperative results
| Grade of Myopia | Log MAR scale (Snellen’s Equivalent) | PRK (n) | t-PRK (n) | P | |
|---|---|---|---|---|---|
| UCVA (1 week to 10 Days) | Mild | -0.12 (20/16) | 0 | 0 | 0.14 |
| 0 (20/20) | 9 | 4 | |||
| 0.18 (20/30) | 4 | 9 | |||
| 0.3 (20/40) | 2 | 1 | |||
| 0.48 (20/60) | 0 | 1 | |||
| 0.6 (20/80) | 0 | 0 | |||
| Moderate | -0.12 (20/16) | 0 | 2 | 0.01 | |
| 0 (20/20) | 9 | 20 | |||
| 0.18 (20/30) | 13 | 6 | |||
| 0.3 (20/40) | 4 | 1 | |||
| 0.48 (20/60) | 0 | 0 | |||
| 0.6 (20/80) | 0 | 0 | |||
| High | -0.12 (20/16) | 0 | 0 | 0.11 | |
| 0 (20/20) | 3 | 16 | |||
| 0.18 (20/30) | 3 | 5 | |||
| 0.3 (20/40) | 0 | 2 | |||
| 0.48 (20/60) | 1 | 0 | |||
| 0.6 (20/80) | 1 | 0 | |||
| UCVA (1 month +/- 2 weeks) | Mild | -0.12 (20/16) | 0 | 0 | >0.99 |
| 0 (20/20) | 14 | 13 | |||
| 0.18 (20/30) | 1 | 2 | |||
| 0.3 (20/40) | 0 | 0 | |||
| Moderate | -0.12 (20/16) | 0 | 2 | 0.10 | |
| 0 (20/20) | 18 | 24 | |||
| 0.18 (20/30) | 7 | 3 | |||
| 0.3 (20/40) | 1 | 0 | |||
| High | -0.12 (20/16) | 0 | 0 | 0.30 | |
| 0 (20/20) | 7 | 18 | |||
| 0.18 (20/30) | 0 | 4 | |||
| 0.3 (20/40) | 1 | 1 | |||
| UCVA (Mean 3.5 months) | Mild | -0.12 (20/16) | 2 | 3 | 0.48 |
| 0 (20/20) | 13 | 10 | |||
| 0.18 (20/30) | 0 | 2 | |||
| 0.3 (20/40) | 0 | 0 | |||
| Moderate | -0.12 (20/16) | 1 | 1 | 0.74 | |
| 0 (20/20) | 25 | 26 | |||
| 0.18 (20/30) | 0 | 2 | |||
| 0.3 (20/40) | 0 | 0 | |||
| High | -0.12 (20/16) | 1 | 2 | >0.99 | |
| 0 (20/20) | 7 | 19 | |||
| 0.18 (20/30) | 0 | 1 | |||
| 0.3 (20/40) | 0 | 1 | |||
| BCVA (Mean 3.5 Months) | Mild | -0.12 (20/16) | 2 | 2 | >0.99 |
| 0 (20/20) | 13 | 13 | |||
| 0.18 (20/30) | 0 | 0 | |||
| Moderate | -0.12 (20/16) | 1 | 0 | 0.47 | |
| 0 (20/20) | 25 | 29 | |||
| 0.18 (20/30) | 0 | 0 | |||
| High | -0.12 (20/16) | 1 | 2 | >0.99 | |
| 0 (20/20) | 7 | 20 | |||
| 0.18 (20/30) | 0 | 1 | |||
| Haze | Mild | Clear Cornea | 13 | 14 | >0.99 |
| Trace Haze | 1 | 0 | |||
| Grade 1 Haze | 0 | 1 | |||
| Grade 2 Haze | 0 | 0 | |||
| Moderate | Clear Cornea | 24 | 22 | 0.26 | |
| Trace Haze | 2 | 5 | |||
| Grade 1 Haze | 0 | 2 | |||
| Grade 2 Haze | 0 | 0 | |||
| High | Clear Cornea | 8 | 14 | 0.12 | |
| Trace Haze | 0 | 6 | |||
| Grade 1 Haze | 0 | 3 | |||
| Grade 2 Haze | 0 | 1 |
Postoperative complications [Table 6] like haze and subjective glare were noted. Slit-lamp grading of subepithelial haze was less than or equal to grade1 in all the eyes in both groups except one patient in t-PRK group at the end of mean follow-up of 3.5 months. Trace haze was seen in 3 eyes (6%) in PRK group and 11 eyes (16%) in t-PRK group. Grade 1 haze was seen in 6 eyes (9%) in t-PRK group and none in PRK group. Incidence of trace haze to Grade 1 haze was higher in the t-PRK group at the end of mean follow-up of 3.5 months as compared to PRK group (P = 0.003) which was statistically significant. Corneal haze disappeared in all the patients who came for follow-up at the end of 6 months except for the one patient who had UCVA of 20/40 as mentioned above. Glare was seen in 4 eyes (8%) in PRK group and none in t-PRK group. Postoperative corneal haze among the sub-groups was not statistically significant.
Table 6.
Corneal Transparency (Haze)
| PRK (n) | t-PRK (n) | P | |
|---|---|---|---|
| Clear Cornea | 41 (86%) | 50 (75%) | 0.003 |
| Trace Haze | 3 (6%) | 11 (16%) | |
| Grade 1 Haze | 0 | 5 (9%) | |
| Grade 2 Haze | 0 | 1 |
Discussion
In our study, we compared postoperative UCVA and BCVA, safety, safety index, efficacy, efficacy index, and corneal transparency (haze) in the eyes, which underwent PRK and t-PRK with the 6th-generation Amaris excimer laser, version 500 E (Schwind eye-tech-solutions). Efficacy and safety in both the groups was found to be 100%. With regards to the safety and efficacy index of the procedures, there was no statistically significant difference between the groups. Postoperatively, trace haze was observed to be more in t-PRK group when compared to the PRK group, however, it did not affect the patient's postoperative UCVA. One patient in the t-PRK group had regression with grade 2 haze, which was visually significant after 2.5 months' follow-up period.
Postoperative corneal haze formation is a well-known complication of surface ablation techniques.[17,18] The degree of haze correlates clinically with the severity of symptoms. Clinically significant corneal haze occurs in a very small percentage of eyes (0.3% to 3%). An important step in the evolution of surface ablation treatments is the introduction of MMC as an adjunctive therapy which was used to reduce the haze formation and hence played an important role in the resurgence of PRK.[19,20] In our study, though we used 0.02 mg% MMC, after 2 months, one patient still developed corneal haze with regression from UCVA 20/20 to 20/40. Possible reasons for the haze in this patient could be high preoperative refractive error -7.50 DS/-0.5DC @ 180 in Right eye and -7.50DS/-0.75DC @ 180 in left eye, poor compliance of the patient to medications, lost BCL in both eyes in the immediate postoperative period, and patient did not use ultraviolet protective glasses in the postoperative period. This patient was given steroid eye drops which were tapered over 18 months. After 20 months of the t-PRK, PTK was performed. After PTK, patient improved from UCVA of 20/40 to 20/20 with trace haze.
Various studies have reported the visual outcomes of two step and single-step t-PRK and also compared them with the other laser refractive surgeries.
In 148 patients, Kaluzny et al. (6th-generation Amaris excimer laser, version 750S Schwind eye-tech-solutions) reported that the single-step t- PRK and alcohol assisted PRK at the end of 3 months in mild to moderate myopia are predictable, effective, and safe for correction of myopia and compound myopic astigmatism.[21] Higher incidence of haze was detected in t-PRK group compared to alcohol assisted PRK group. In our study, the procedure was performed in high myopes, with the same excimer laser but with a different version (500E) and the outcome was compared with the conventional PRK. At the end of mean follow-up of 3.5 months, our results were similar to this study. There was higher incidence of corneal haze with slit lamp, which was statistically significant but visually not significant.
In 40 myopic patients who had single-step t-PRK, Chen et al. reported that the one-step topography guided t-PRK with 1 KHz excimer laser (iRES, iVIS Technology, Taranto, Italy) provided safe, effective, predictable, and stable results with low pain and no visually significant haze.[22]
In a study by Ali Fadlallah et al., between the single-step t- PRK and alcohol assisted PRK performed with transepithelial PRK nomogram of the Amaris laser's ORK-CAM software for mild to moderate myopia, concluded that at the end of 3 months, PRK group had less pain, less postoperative haze, and a faster healing time.[10] The visual outcomes with the 2 techniques were comparable, which was similar to our study.
Comparison of clinical results between mechanical and two step t-PRK was done in a study by Clinch et al., using a 193-nm excimer beam generated within the Omnimed laser (Summit Technology, Inc., Waltham, MA) and concluded that at all postoperative intervals, mechanical values tended to be superior to the transepithelial values with respect to UCVA, BCVA, MRSE, astigmatism, corneal haze, and subjective vision (glare and haloes).[23]
Kanitkar et al. performed bilateral PRK in 9 patients using the Visx S3 laser, in which one eye was de-epithelialized with PTK and the fellow eye was de-epithelialized with alcohol.[8] Ethanol-assisted mechanical debridement of the epithelium caused significantly less postoperative pain than epithelial removal using the excimer laser.
A study by Lee et al. compared conventional PRK, two-step t- PRK, and LASEK using Visx Star S3 and concluded that the postoperative pain, subepithelial opacity, and the BCVA were similar in the three groups regardless of the epithelial removal procedure.[6]
In two step t-PRK researchers used different lasers for de-epithelization.[4,8,9,6,23,24] Most of these studies observed the visual outcomes, pain score, and the rate of epithelial healing.
In our study, we observed corneal haze, safety, efficacy, safety index, and efficacy index apart from the visual outcomes using single-step t-PRK and compared with conventional PRK. We found that none of our patients lost 2 or more lines of preoperative BCVA. Thus, both the procedures are safe and as all the eyes attained a postoperative UCVA of 20/40 or better, it makes both the procedures equally efficient. Though statistically insignificant, better visual outcome (20/20 or better) was noticed in the PRK group at the end of mean follow-up of 3.5 months, and this could be attributed to the inclusion of more number of patients with high myopia in the t-PRK group, among whom, the ablation depth was more when compared to low to moderate dioptric power eyes, resulting in relatively more haze formation, though the haze resolved in all the patients who came for the follow-up after 6 months in t-PRK group.
The strength of our study is that this is first study which compared the safety, efficacy, and complications apart from visual outcomes in the conventional PRK and single- step t-PRK in low to high myopia in the Asian Indian Eyes, whereas most of the other studies have compared two step t-PRK with the alcohol assisted PRK or single-step t-PRK with alcohol assisted PRK.
Limitation of this study is shorter mean follow-up time (i.e., 3.5 months) and no upper limit for the grade of myopia (as our main inclusion criteria was to include patients who had come for all the follow-up visits and there were more patients of high myopia among the t-PRK group). Despite these limitations, our results at the end of mean follow-up of 3.5 months shows that the postoperative UCVA, postoperative BCVA, efficacy, safety, safety index, and efficacy index of the t-PRK group for the treatment of low to high myopia with and without astigmatism in Asian Indian Eyes were same as compared to PRK group, using the 6th-generation Amaris excimer laser, version 500E (Schwind eye-tech-solutions).
Conclusion
We conclude that the single-step t-PRK and conventional PRK produce similar results after a mean follow-up of 3.5 months. These procedures are predictable, effective, and safe for the correction of low to high myopia and compound myopic astigmatism. There was higher incidence of corneal haze in the t-PRK group, when compared to the PRK group, which was statistically significant. Also, a follow-up period of at least 6 months would have been better to assess the corneal transparency in the t-PRK group.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Dr Anupama Kalwad, Anand Eye Institute, Hyderabad.
References
- 1.Margo JA, Munir WM. Corneal haze following refractive surgery: A review of pathophysiology, incidence, prevention, and treatment. Int Ophthalmol Clin. 2016;56:111–25. doi: 10.1097/IIO.0000000000000112. [DOI] [PubMed] [Google Scholar]
- 2.Netto MV, Mohan RR, Ambrósio R, Jr, Hutcheon AE, Zieske JD, Wilson SE. Wound healing in the cornea: A review of refractive surgery complications and new prospects for therapy. Cornea. 2005;24:509–22. doi: 10.1097/01.ico.0000151544.23360.17. [DOI] [PubMed] [Google Scholar]
- 3.Shortt AJ, Allan BD, Evans JR. Laser-assisted in-situ keratomileusis (LASIK) versus photorefractive keratectomy (PRK) for myopia. Cochrane Database Syst Rev. 2013:CD005135. doi: 10.1002/14651858.CD005135.pub3. doi: 101002/14651858CD005135pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghadhfan F, Al-Rajhi A, Wagoner MD. Laser in situ keratomileusis versus surface ablation: Visual outcomes and complications. J Cataract Refract Surg. 2007;33:2041–8. doi: 10.1016/j.jcrs.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 5.Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumidi II. Advances in subepithelial excimer refractive surgery techniques: Epi-LASIK. Curr Opin Ophthalmol. 2003;14:207–12. doi: 10.1097/00055735-200308000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Lee HK, Lee KS, Kim JK, Kim HC, Seo KR, Kim EK. Epithelial healing and clinical outcomes in excimer laser photorefractive surgery following three epithelial removal techniques: Mechanical, alcohol, and excimer laser. Am J Ophthalmol. 2005;139:56–63. doi: 10.1016/j.ajo.2004.08.049. [DOI] [PubMed] [Google Scholar]
- 7.Wang DM, Du Y, Chen GS, Tang LS, He JF. Transepithelial photorefractive keratectomy mode using SCHWIND-ESIRIS excimer laser: Initial clinical results. Int J Ophthalmol. 2012;5:334–7. doi: 10.3980/j.issn.2222-3959.2012.03.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanitkar KD, Camp J, Humble H, Shen DJ, Wang MX. Pain after epithelial removal by ethanol-assisted mechanical versus transepithelial excimer laser debridement. J Refract Surg. 2000;16:519–22. doi: 10.3928/1081-597X-20000901-06. [DOI] [PubMed] [Google Scholar]
- 9.Aslanides IM, Padroni S, Arba Mosquera S, Ioannides A, Mukherjee A. Comparison of single-step reverse transepithelial all-surface laser ablation (ASLA) to alcohol-assisted photorefractive keratectomy. Clin Ophthalmol. 2012;6:973–80. doi: 10.2147/OPTH.S32374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fadlallah A, Fahed D, Khalil K, Dunia I, Menassa J, El Rami H, et al. Transepithelial photorefractive keratectomy: Clinical results. J Cataract Refract Surg. 2011;37:1852–7. doi: 10.1016/j.jcrs.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 11.Luger MH, Ewering T, Arba-Mosquera S. Consecutive myopia correction with transepithelial versus alcohol-assisted photorefractive keratectomy in contralateral eyes: One-year results. J Cataract Refract Surg. 2012;38:1414–23. doi: 10.1016/j.jcrs.2012.03.028. [DOI] [PubMed] [Google Scholar]
- 12.Gomel N, Negari S, Frucht-Pery J, Wajnsztajn D, Strassman E, Solomon A. Predictive factors for efficacy and safety in refractive surgery for myopia. PLoS One. 2018;13:e0208608. doi: 10.1371/journal.pone.0208608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arba Mosquera S, Awwad ST. Theoretical analyses of the refractive implications of transepithelial PRK ablations. Br J Ophthalmol. 2013;97:905–11. doi: 10.1136/bjophthalmol-2012-302853. [DOI] [PubMed] [Google Scholar]
- 14.Aras C, Ozdamar A, Aktunç R, Erçikan C. The effects of topical steroids on refractive outcome and corneal haze, thickness, and curvature after photorefractive keratectomy with a 6.0-mm ablation diameter. Ophthalmic Surg Lasers. 1998;29:621–7. [PubMed] [Google Scholar]
- 15.Koch DD, Kohnen T, Obstbaum SA, Rosen ES. Format for reporting refractive surgical data. J Cataract Refract Surg. 1998;24:285–7. doi: 10.1016/s0886-3350(98)80305-2. [DOI] [PubMed] [Google Scholar]
- 16.Fahd D dJ, Jain S, Azar D. Corneal haze after refractive surgery. In: Alio J, Azar DT, editors. Management of Complications in Refractive Surgery. Berlin, German: Springer; 2008. pp. 179–86. [Google Scholar]
- 17.Fini ME. Keratocyte and fibroblast phenotypes in the repairing cornea. Prog Retin Eye Res. 1999;18:529–51. doi: 10.1016/s1350-9462(98)00033-0. [DOI] [PubMed] [Google Scholar]
- 18.Wilson SE, Liu JJ, Mohan RR. Stromal-epithelial interactions in the cornea. Prog Retin Eye Res. 1999;18:293–309. doi: 10.1016/s1350-9462(98)00017-2. [DOI] [PubMed] [Google Scholar]
- 19.Majmudar PA, Schallhorn SC, Cason JB, Donaldson KE, Kymionis GD, Shtein RM, et al. Mitomycin-C in corneal surface excimer laser ablation techniques: A report by the American Academy of Ophthalmology. Ophthalmology. 2015;122:1085–95. doi: 10.1016/j.ophtha.2015.01.019. [DOI] [PubMed] [Google Scholar]
- 20.Carones F, Vigo L, Scandola E, Vacchini L. Evaluation of the prophylactic use of mitomycin-C to inhibit haze formation after photorefractive keratectomy. J Cataract Refract Surg. 2002;28:2088–95. doi: 10.1016/s0886-3350(02)01701-7. [DOI] [PubMed] [Google Scholar]
- 21.Kaluzny BJ, Cieslinska I, Mosquera SA, Verma S. Single-step Transepithelial PRK vs alcohol-assisted PRK in myopia and compound myopic astigmatism correction. Medicine (Baltimore) 2016;95:e1993. doi: 10.1097/MD.0000000000001993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stojanovic A, Chen S, Chen X, Stojanovic F, Zhang J, Zhang T, et al. One-step transepithelial topography-guided ablation in the treatment of myopic astigmatism. PLoS One. 2013;8:e66618. doi: 10.1371/journal.pone.0066618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clinch TE, Moshirfar M, Weis JR, Ahn CS, Hutchinson CB, Jeffrey JH. Comparison of mechanical and transepithelial debridement during photorefractive keratectomy. Ophthalmology. 1999;106:483–9. doi: 10.1016/S0161-6420(99)90135-5. [DOI] [PubMed] [Google Scholar]
- 24.Buzzonetti L, Petrocelli G, Laborante A, Mazzilli E, Gaspari M, Valente P, et al. A new transepithelial phototherapeutic keratectomy mode using the NIDEK CXIII Excimer laser. J Refract Surg. 2009;25(1 Suppl):S122–4. doi: 10.3928/1081597X-20090115-08. [DOI] [PubMed] [Google Scholar]


