Abstract
Background/aim
Widespread use of antiretroviral treatment (ART) has led to decrease in the incidence of HIV/AIDS-related mortality. Besides the availability of ART, medication adherence is essential for treatment success. There is a scarcity of data reported from Turkey regarding ART adherence among people living with HIV/AIDS (PLWHA). Therefore, this study was undertaken to determine medication adherence and related factors among PLWHA in Turkey.
Materials and methods
The sample consisted of 158 PLWHA, who were being followed up at Infectious Diseases Outpatient Clinic of Hacettepe University Hospital. Data were collected using an individual questionnaire and the Turkish version of the Morisky Medication Adherence Scale.
Results
The median patient age was 38 years, 80.4% were male, and 51.3% were married. The median duration of both HIV infection and ART was 3 years. Sixty-one percent used two drug regimens. Sixty-one percent were highly adherent to ART while 37.9% were moderately adherent. The absence/presence of social support resources, disease duration, ART duration, and being informed about the ART regimen were statistically associated with medication adherence.
Conclusion
Our results suggest that medication adherence is excellent among Turkish PLWHA. Interventions, including effective social support, and continuous counseling about ART, might further boost the adherence of PLWHA.
Keywords: HIV/AIDS, antiretroviral treatment, medication adherence, nursing
1. Introduction
There are 36.9 million people living with HIV/AIDS (PLWHA) in the world. Among them, 34.3 million are adults, and 17.4 million are women (1). According to the Turkish Ministry of Health’s National HIV Registry, about 17,000 people are living with the HIV infection in Turkey. However, due to the long latency, lack of adequate target population testing, and inadequate registry systems, this number may not be robust (2).
From 2001 to 2013, the annual number of new HIV infections declined by 38% globally, followed by a significant decline in AIDS-related deaths. However, trends in new infections have differed among regions and countries (3), and the number of new HIV diagnoses increased 450% after 2012 in Turkey (2).
There is no cure for HIV infection. Nonetheless, antiretroviral treatment (ART) can be implemented to overcome the infection-associated adverse outcomes (4,5). ART is the cornerstone of management of PLWHA. Widespread use of ART led to a decrease in the incidence of HIV/AIDS-related mortality both in the developed and developing world (6). Furthermore, ART improves the quality of life and prolongs the life expectancy (7).
Medication adherence is defined as ‘‘the act of conforming to the recommendations made by the provider with respect to timing, dosage, and frequency of medication taking’’ (8). Besides the availability of ART, medication adherence must be at least 90% to suppress HIV replication (9–11). Medication adherence is crucial in maintaining therapeutic drug levels, ensuring virologic suppression, reducing drug resistance (12), preventing immunologic decay from HIV, and, especially, reducing the risk of HIV transmission (13).
Variation in medication adherence has been reported among PLWHA by various studies. Data from Georgia, Iran, Russia, and Greece suggested that the proportion of the adherent PLWHA was 79.0%, 63.9%, 82.0%, and 81.8%, respectively (14–17). A small and older study composed of 36 PLWHA from Turkey found the ART adherence rate as 38.9% (18).
Risk factors associated with low medication adherence were being busy, forgetfulness (19,20), side effects of ART, economic problems (8), stigmatization (8,21,22), and emotional stress (23,24). In addition, lack of central insurance and therefore high cost is another reason for low adherence (25). In Turkey, it is stated in the 67th article of the Social Insurance and General Health Insurance Law that people with any communicable diseases can benefit from the General Health Insurance system without any delay. HIV infection is also classified in this list. Hence, ART and other medical costs are fully covered by the government (26). PLWHA are charged only for a small amount of the expenditure per prescription. It is called the “contribution margin” and is 10% of drug price (27).
It is important to evaluate ART adherence among PLWHA. There is a scarcity of data reported from Turkey regarding ART adherence. This study was undertaken to determine the medication adherence and related factors among PLWHA in Turkey.
2. Materials and methods
2.1. Patients
This hospital-based descriptive study was conducted at the HIV/AIDS Outpatient Clinic of Hacettepe University Hospital in Ankara between 7 September 2015 and 27 April 2016. Hacettepe University Non-invasive Ethical Research Board Study reviewed and approved the study protocol (Ref. No.: 16969557-981–02.09.2016). The researchers worked in collaboration with the clinicians in the identification of HIV/AIDS patients, who were receiving ART. A written statement was also included in the introductory part of the questionnaires, explaining the study purpose and confidentiality of the information collected. All data were obtained from respondents in a private room.
A total 310 PLWHA were being followed up at the HIV/AIDS outpatient clinic. The calculated sample size was 138, assuming α = 0.05 and 1-β = 0.95 in power analysis. During the study period, 186 PLWHA applied to the infectious diseases clinic for treatment and follow-up. Among them, 158 PLWHA who fulfilled the inclusion criteria and voluntarily agreed to participate in the research were included in our study. The inclusion criteria were to be on ART for at least 6 months, at least 18 years old, and to provide informed consent. Exclusion criteria included not providing informed consent and not being on ART. A total of 28 patients were excluded, as they did not meet the inclusion criteria. As a result, 85% (n = 158) of the PLWHA who applied to the infectious diseases clinic were included in the final analysis (Table 1). Our results of the 158 study participants are representative of 310 PLWHA treated in the HIV/AIDS outpatient clinic.
Table 1.
Distribution of the adherent and noncompliant people living with HIV/AIDS according to descriptive statistics of demographic variables.
| Adherence level | ||||||
| High n (%) | Medium/Low n (%) | P | ||||
| Age | 18–25 | 11 (64.7) | 6 (35.3) | 0.956 | ||
| 26–45 | 57 (62.0) | 35 (38.0) | ||||
| 46–60 | 23 (60.5) | 15 (39.5) | ||||
| >60 | 6 (54.5) | 5 (45.5) | ||||
| Sex | Male | 79 (62.2) | 48 (37.8) | 0.988 | ||
| Female | 18 (60.0) | 12 (40.0) | ||||
| Marital status | Married | 49 (60.5) | 32 (39.5) | 0.812 | ||
| Single | 48 (62.3) | 29 (37.7) | ||||
| Number of drugs taken | One-drug regimen | 17 (58.6) | 12 (41.4) | 0.464 | ||
| Two-drugs regimen | 63 (64.9) | 34 (35.1) | ||||
| Three or more drugs | 17 (53.1) | 15 (46.9) | ||||
| Education | Primary school and below | 12 (54.5) | 10 (45.5) | 0.181 | ||
| Secondary school | 9 (45.0) | 11 (55.0) | ||||
| High school | 17 (56.7) | 13 (43.3) | ||||
| Undergraduate and master degree | 59 (68.6) | 27 (31.4) | ||||
2.2. Data collection
Data were collected using an individual information questionnaire and the Turkish version of the Morisky Medication Adherence Scale (MMAS). The personal information questionnaire was developed by the researchers, using PubMed and Elsevier databases (8,19,28,29). This questionnaire included 7 questions about the participant’s demographic characteristics (sex, age, marital status, occupation, education level, social insurance, and economical status) and 22 questions on medication and disease-related factors (disease and medication duration, name and number of pills taken, patients’ thoughts about the benefits, complexity, taste, and number of the drugs; reasons for missing the doses, such as being busy, side effects, vision problems, economic problems, stigma, lack of social and health care professionals’ supports; methods used as a reminder of the dose time, and assessing if the patients had any information about the usage of the drugs)
The Turkish version of the MMAS was used to determine adherence to ART among PLWHA. The reliability and validity studies of the Turkish version of the MMAS were previously reported by Vural et al. (30). This scale consists of 6 items, each being a 2-point type, implemented in evaluating ART compliance through a face-to-face interview. Higher scores indicate lower adherence to ART. According to this scale, zero score implies high adherence, 1–2 points denote moderate adherence, and 3–6 points means noncompliant.
After informing the patient about the study, the data report form was distributed, and correspondents asked to fill the questionnaire in a private room located at the outpatient clinic, by paying attention to their privacy.
2.3. Statistical analysis
All analyses were performed using SPSS version 21.0 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Armonk, NY, USA: IBM Corp.) and Microsoft Excel 2013. Numbers, percentages, median, and the chi-square (χ2) test were used in the data analysis. The Shapiro–Wilk test was used to determine whether the data were normally distributed. Spearman’s rho coefficient (rs) allowed identifying whether there was an association between age/duration of illness/duration of medication/number of medicines used/daily dose amount, and the MMAS score. The Mann–Whitney U and Kruskal–Wallis tests were adopted to determine whether there was a statistically significant difference in the MMAS score among the groups (female/male, marital status, education level, having/not having information about drugs, experiencing/not experiencing side effects, presence/absence of social support, being satisfied/dissatisfied with the healthcare professionals, stigma, use/do not use reminders). The statistical significance level was set at P < 0.05.
3. Results
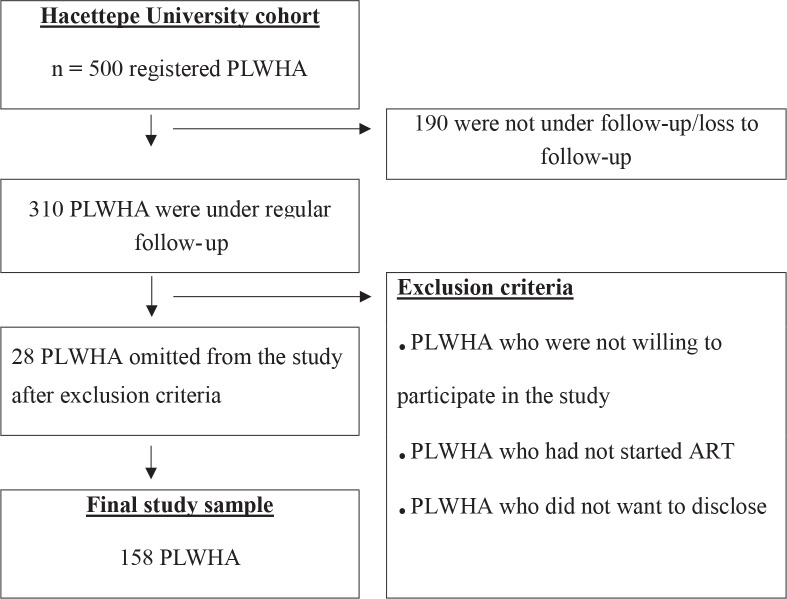
There were 500 PLWHA registered in the Hacettepe University cohort. Among them, 310 were actively under regular follow-up. One hundred and eighty-six PLWHA applied for follow-up during the study period. Twenty-eight PLWHA were excluded, and 158 PLWHA included in the final analysis (Figure). The median age was 38 (min: 19, max: 74), 80.4% (n = 127) were male, and 51.3% (n = 81) were married. The median duration of both HIV infection diagnosis and ART were 3 years. Sixty-one percent (n = 97) used two drug regimens. Table 1 summarizes the demographic values.
Figure 1.
Sampling process of the study (PLWHA, people living with HIV/AIDS; ART, antiretroviral treatment)
Nearly all the respondents (98.7%) thought that the drugs are beneficial for them, but 26.6% (n = 42) reported that they missed at least one dose because of being busy. In addition, 28.5% (n = 45) thought that the number of the pills taken daily are too many, and 29.7% (n = 47) had ART-related side effects. Also, 8.2% (n = 13) had problems affording the drugs, and 17.1% (n = 27) did not have information about the importance of adherence to ART and how to use the drugs. Furthermore, 42.4% (n = 67) had stigma-related problems.
Sixty-one percent (n = 97) were highly adherent to ART while 37.9% (n = 60) were moderately adherent. Adherence varied among the age groups. Adherent PLWHA was 64.7%, 62.0%, 60.5%, and 54.5% in the age groups 18–25, 26–45, 46–60, and over 60 years, respectively. There were no significant differences in adherence among the age groups (χ2 = 0.321; P = 0.956). Medication adherence was not associated with sex, age, marital status, education level, and the number of prescribed drugs in the ART regimen (P > 0.05) (Table 1).
Medication adherence differed in PLWHA who were previously informed about ART and those who were not. Adherence among the preinformed and uninformed patients was 65.6% and 40.7%, respectively (Table 2). Those who had information on the usage and importance of ART were statistically more adherent than those who did not have such information (χ2 = 4.856; P = 0.028).
Table 2.
Distribution of the adherent and noncompliant people living with HIV/AIDS, according to factors related to the disease.
| Factor | Adherence level | |||
|---|---|---|---|---|
| High n (%) | Medium/Low n (%) | P | ||
| Having information about ART | Yes | 86 (65.6) | 45 (34.4) | 0.028 |
| No | 11 (40.7) | 16 (59.3) | ||
| Having side effects due to ART | Yes | 28 (59.6) | 19 (40.4) | 0.899 |
| No | 69 (62.2) | 42 (37.8) | ||
| Having social support resources | Yes | 92 (64.8) | 50 (35.2) | 0.019 |
| No | 5 (31.3) | 11 (68.8) | ||
| Being satisfied with healthcare professionals’ attitudes | Yes | 94 (61.8) | 58 (38.2) | 0.677 |
| No | 3 (50.0) | 3 (50.0) | ||
| Stigma | Yes | 43 (64.2) | 24 (35.8) | 0.537 |
| No | 54 (59.3) | 37 (40.7) | ||
| Using reminders | Yes | 38 (66.7) | 19 (33.3) | 0.394 |
| No | 59 (58.4) | 42 (41.6) | ||
| Having financial problems | Yes | 8 (61.5) | 5 (38.5) | 1.000 |
| No | 89 (61.4) | 56 (38.6) | ||
The presence of ART-related side effects did not affect adherence. There was no difference in medication adherence between patients with and without side effects (59.6% and 62.2%, respectively) (χ2 = 0.016; P = 0.899) (Table 2). Conversely, a significant association existed between the presence of social support and medication adherence. PLWHA who confirmed the presence of social support were more adherent than the PLWHA who did not have social support (64.8% and 31.3%, respectively) (χ2 = 5.483; P = 0.019) (Table 2).
The relationships of the MMAS score with age, duration after diagnosis, duration of ART, number of medications prescribed, and number of pills taken daily were examined. A low positive correlation between duration after diagnosis, duration of ART, and the MMAS score was demonstrated (rs = 0.275 and 0.254, P ≤ 0.001, respectively) (Table 3).
Table 3.
Correlation between the Morisky Medication Adherence Scale score and selected variables
| Variable | Morisky adherence score | |
|---|---|---|
| rs | P | |
| Age | 0.028 | 0.724 |
| Duration of disease | 0.275 | <0.001 |
| Duration of drug usage | 0.254 | 0.001 |
| Number of drugs taken | 0.068 | 0.393 |
| Number of pills taken daily | 0.134 | 0.094 |
4. Discussion
Our results revealed that 61% of PLWHA were adherent to ART, whereas 1.3% were noncompliant. The adherence rate in this study was higher when compared with the reported rates in the literature. It was previously shown that 21% to 94% of PLWHA were highly adherent to ART (15,17,29,31–35). The variance in adherence rates may result from differences in the research method, characteristics of the cohort, the administrative structure of the healthcare facilities, and the social security policies of the countries. It may also arise from the economic status of the patients, because people living in Europe, Asia, Africa, and America have different socioeconomic levels.
In previous studies, ART adherence was associated with sex (23), age (36), education (19,22), economic status (8,24,25,33), substance use (19,23,25), disease duration (37), stigma (8,22,23,33,38), ART-related side effects (8,38–41), satisfaction with healthcare staff (8,33,38,39), number of pills taken daily (21,31,32,42), social support (8,38,43), mental health (23–25,43), using reminders (8,43), and having information prior to ART (38). In addition, being busy, forgetfulness (19,28,44), being away from home (41,44), lack of central insurance (25,43), and adverse taste of medicines (45) were the most common reasons for low adherence. After examining the reasons for low adherence, according to the countries, the most leading causes included being busy, being away from home, and forgetfulness, in the USA; side effects, substance abuse, and stigma in Europe; stigma, forgetfulness, and substance abuse in Asia; and lastly, economic status, side effects, satisfaction with healthcare staff, and stigma in Africa. Mental health was the common factor that was associated with ART adherence in all regions. In our study, no correlations were observed between ART adherence and age, sex, marital status, education level, economic status, stigma, ART-related side effects, satisfaction with healthcare staff, and the number of pills taken daily. The fact that our sample is small, that the study is single-centered, and that we work at the referral center for HIV/AIDS may have affected these results. In addition, the small number of people with low adherence-related risk factors, such as lack of health insurance, dissatisfaction with healthcare personnel, and economic problems, may have contributed to these results.
In this study, people who were previously informed about ART adherence had higher adherence rates compared to those who were uninformed. Our results agree with those of Schneider et al. who demonstrated a statistically significant relationship between having information about ART and ART adherence (46). Similarly, Demirkıran et al. (47) found that informing patients about medication adherence improves adherence among PLWHA. Providing information to PLWHA on ART and adherence ensures taking medicine regularly, without missing any dose, despite feeling good/bad, having side effects, being bored of the drugs, or feeling no need to continue the medication; thereby maintaining the high ART adherence level. Furthermore, in a routine daily outpatient care, every single PLWHA applying to our clinic was informed about ART and the disease itself. Interestingly, some of the PLWHA under our care were still denying previous education on ART and the disease. This finding restresses the importance of continuous medical briefing at every visit.
Another factor that was significantly associated with ART adherence was the absence/presence of social support resources (Table 2) (P = 0.019). Kalichman et al. (48) observed that patients who had lack of support resources were less adherent to ART. In another study, in which pharmacists talked about their experience while working with PLWHA, lack of support resources was the major obstacle for ART adherence (25). Our findings are consistent with those of the previous studies in the literature. The absence of social support increases the feelings of anger, offense, despair, and depression in the later stages of HIV/AIDS infection. Consequently, all of these factors affect patients’ adherence to ART adversely.
No statistical association was found between ART adherence and having ART-related side effects, being satisfied/dissatisfied about the healthcare professionals, stigma, using reminders, and economic status (P > 0.05) (Table 2). In contrast to our findings, PLWHA who have ART drug-related side effects (8,20,36,37,49), are dissatisfied about health care professionals (50) and had stigma-related problems (8,21,22) were found to be less adherent in other studies. From this perspective, our findings were inconsistent with those in the literature. These discrepancies may be because most of our respondents were satisfied with the healthcare professionals in the HIV/AIDS Outpatient Clinic. Also, the prescribed ART was current, and therefore most of the PLWHA did not experience ART-related side effects. Furthermore, we did not use a comprehensive tool to evaluate the stigma. Instead, it was asked with only one question in the questionnaire form. These reasons may explain the lack of association between stigma, ART-related side effects, being satisfied/dissatisfied with the healthcare professionals, and ART adherence.
In our study, weak positive correlations were observed between disease duration, ART duration, and ART adherence (P = 0.001) (Table 3). It was found that taking ART for a long time could increase the motivation for medication adherence. Our findings corroborated the literature (36,51). When the duration of ART is long, PLWHA become used to the drugs, require fewer reminders, and the drugs become a regular part of their lives. All these factors are thought to maintain a high medication adherence among PLWHA.
This work is the first extensive study from Turkey, determining ART adherence and related factors. Our study was undertaken in a tertiary level referral center, with strict case and outcome definition criteria. The prospective study design minimized the missing data. Our sample size is statistically sufficient to draw a conclusion on the ART adherence among Turkish PLWHA. Conversely, the single-center design, lack of a reliable stigma scale, and lack of pharmacy refill dates are main limitations in our study.
In conclusion, the absence/presence of social support resources, disease duration, ART duration, and being informed about the ART regimen were statistically associated with medication adherence. Therefore, PLWHA must be continuously informed about the ART daily dosing regimen, as an intervention to maintain a high ART adherence. Suggesting reminders, ensuring and searching social support resources, and determining the factors that negatively affect ART adherence represent the other solutions and propositions for increasing ART adherence within the framework of nursing. Finally, considering that newly diagnosed patients and those who are new to ART have relatively low drug compliance, informing PLWHA on the use of ART should be further intensified in newly diagnosed individuals and those who have just started ART.
Acknowledgments
This study was supported by a grant from the Yıldırım Beyazıt University Scientific Research Department (Project No.: 3049).
References
- Foresto JS Melo ES Costa CRB Antonini M Gir E Reis RK Adherence to antiretroviral therapy by people living with HIV/AIDS in a municipality of São Paulo. Rev Gaúcha Enferm. 2017;38:e63158–e63158. doi: 10.1590/1983-1447.2017.01.63158. [DOI] [PubMed] [Google Scholar]
- Bulaşıcı Hastalıklar Daire Başkanlığı İstatiksel Verileri. 2016.
- Gökengin D Doroudi F Tohme J Collins B Madani N HIV/AIDS: trends in the Middle East and North Africa region. Int J Infect Dis. 2016;44:66–73. doi: 10.1016/j.ijid.2015.11.008. [DOI] [PubMed] [Google Scholar]
- Cihlar T Fordyce M Current status and prospects of HIV treatment. Curr Opin Virol. 2016;18:50–56. doi: 10.1016/j.coviro.2016.03.004. [DOI] [PubMed] [Google Scholar]
- Wasti SP Simkhada P Randall J Freeman JV Van Teijlingen E Barriers to and facilitators of antiretroviral therapy adherence in Nepal: a qualitative study. J Health Popul Nutr. 2012;30:410–419. doi: 10.3329/jhpn.v30i4.13294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumarasamy N Patel A Pujari S Antiretroviral therapy in Indian setting: When & what to start with, when. Indian J Med Res. 2011;134:787–800. doi: 10.4103/0971-5916.92626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atuyambe L Neema S Otolok-Tanga E Wamuyu-Maina G Kasasa S Wabwire-Mangen F The effects of enhanced access to antiretroviral therapy: A qualitative study of community perceptions in Kampala City, Uganda. Afr Health Sci. 2008;8:13–19. [PMC free article] [PubMed] [Google Scholar]
- Bezabhe WM Chalmers L Bereznicki LR Peterson GM Bimirew MA Kassie DM Barriers and facilitators of adherence to antiretroviral drug therapy and retention in care among adult HIV positive patients: a qualitative study from Ethiopia. PloS One. 2014;9:e97353–e97353. doi: 10.1371/journal.pone.0097353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaecher KL The importance of treatment adherence in HIV. Am J Manag Care. 2013;19:S231–S237. [PubMed] [Google Scholar]
- Chaiyachati KH Ogbuoji O Price M Suthar AB Negussie EK Bärnighausen T Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. AIDS. 2014;28:S187–S204. doi: 10.1097/QAD.0000000000000252. [DOI] [PubMed] [Google Scholar]
- Willie TC Overstreet NM Sullivan TP Sikkema KJ Hansen NB Barriers to HIV medication adherence: Examining distinct anxiety and depression symptoms among women living with HIV who experienced childhood sexual abuse. Behav Med. 2016;42:120–127. doi: 10.1080/08964289.2015.1045823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceylan E Koç A HIV(+)/AIDS hastalarında antiretroviral tedaviye uyumun önemi (Literatür çalışması) Jinekoloji-Obstetrik ve Neonatoloji Tıp Dergisi. 2017;14:74–81. [Google Scholar]
- Günthard HF Saag MS Benson CA Del Rio C Eron JJ Gallant JE Mugavero MJ Sax PE Thompson MA Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2016 recommendations of the International Antiviral Society–USA panel. Jama. 2016;316:191–210. doi: 10.1001/jama.2016.8900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chkhartishvili N Abutidze A Dvali N Kempker R Tsertsvadze T Long-term adherence to antiretroviral therapy in Georgia. 2017;2:4–9. [Google Scholar]
- Moradi A Alavi SM Fahimfar N Haghighizadeh MH Mirzaei B Study of determinants of adherence to antiretroviral treatment among HIV patients covered by Ahwaz Jundishapur University of Medical Sciences. Int J Med Res Health Sci. 2016;5:477–484. [Google Scholar]
- Amirkhanian YA Kelly JA DiFranceisco WJ Kuznetsova AV Tarima SS Yakovlev AA Musatov VB Predictors of HIV care engagement, antiretroviral medication adherence, and viral suppression among people living with HIV infection in St. Petersburg, Russia. AIDS Behav. 2018;22:791–799. doi: 10.1007/s10461-016-1638-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- What role do psychosocial factors play in influencing HIV positive peoples’ compliance with medical treatment? PhD 2013.
- HIV/AIDS’li hastaların tedaviye uyumunu etkileyen psikososyal faktörler. Türk HIV/AIDS Dergisi. 2003.
- Hansana V Sanchaisuriya P Durham J Sychareun V Chaleunvong K Boonyaleepun S Schelp FP Adherence to antiretroviral therapy (ART) among people living with HIV (PLHIV): A cross-sectional survey to measure in Lao PDR. BMC Public Health. 2013;13:617–617. doi: 10.1186/1471-2458-13-617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran BX Nguyen LT Nguyen NH Hoang QV Hwang J Determinants of antiretroviral treatment adherence among HIV/AIDS patients: a multisite study. Glob Health Action. 2013;6:19570–19570. doi: 10.3402/gha.v6i0.19570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talam NC Gatongi P Rotich J Kimaiyo S Hospital Referral Factors affecting antiretroviral drug adherence among HIV/AIDS adult patients attending HIV/AIDS clinic at Moi Teaching. East Afr J Public Health. 2008;5:74–78. [PubMed] [Google Scholar]
- Waite KR Paasche-Orlow M Rintamaki LS Davis TC Wolf MS Literacy, social stigma, and HIV medication adherence. J Gen Intern Med. 2008;23:1367–1372. doi: 10.1007/s11606-008-0662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negash T Ehlers V Personal factors influencing patients’ adherence to ART in Addis Ababa, Ethiopia. J Assoc Nurses AIDS Care. 2013;24:530–538. doi: 10.1016/j.jana.2012.11.004. [DOI] [PubMed] [Google Scholar]
- Kalichman SC Grebler T Stress and poverty predictors of treatment adherence among people with low-literacy living with HIV/AIDS. Psychosom Med. 2010;72:810–816. doi: 10.1097/PSY.0b013e3181f01be3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kibicho JW Owczarzak J Pharmacists’ perspectives on promoting medication adherence among patients with HIV. J Am Pharm Assoc. 2011;51:746–755. doi: 10.1331/JAPhA.2011.10190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosyal Sigortalar ve Genel Sağlık Sigortası Kanunu ( Resmi Gazete. 2006;5510 [Google Scholar]
- Resmi Gazete (Sayı: 28597) 2013.
- Chandwani S Koenig LJ Sill AM Abramowitz S Conner LC D’ Predictors of antiretroviral medication adherence among a diverse cohort of adolescents with HIV. J Adolesc Health. 2012;51:242–251. doi: 10.1016/j.jadohealth.2011.12.013. [DOI] [PubMed] [Google Scholar]
- Genberg BL Lee Y Rogers WH Four types of barriers to adherence of antiretroviral therapy are associated with decreased adherence over time. AIDS Behav. 2015;19:85–92. doi: 10.1007/s10461-014-0775-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vural B Acar TÖ Topsever P Filiz TM Reliability and validity of Turkish version of Modified Morisky Scale. Turk Fam Physician. 2012;3:17–20. [Google Scholar]
- The determinants of antiretroviral therapy adherence and the relationship of healthcare expenditures to adherence among Florida Medicaid-insured patients diagnosed with HIV or AIDS. PhD. 2013.
- Letta S Demissie A Oljira L Dessie Y Factors associated with adherence to antiretroviral therapy (ART) among adult people living with HIV and attending their clinical care, Eastern Ethiopia. BMC Int Health Hum Rights. 2015;15:33–33. doi: 10.1186/s12914-015-0071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oku AO Owoaje ET Ige OK Oyo-ita A Prevalence and determinants of adherence to HAART amongst PLHIV in a tertiary health facility in south-south Nigeria. BMC Infect Dis. 2013;13:401–401. doi: 10.1186/1471-2334-13-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intasan J Bunupuradah T Vonthanak S Kosalaraksa P Hansudewechakul R Kanjanavanit S Ngampiyaskul C Wongsawat J Luesomboon W Apornpong T Comparison of adherence monitoring tools and correlation to virologic failure in a pediatric HIV clinical trial. AIDS Patient Care STDs. 2014;28:296–302. doi: 10.1089/apc.2013.0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison SD Rashidi V Sarnquist C Banushi VH Hole MK Barbhaiya NJ Gashi VH Osterberg L Maldonado Y Harxhi A Antiretroviral therapy adherence and predictors to adherence in Albania: a cross-sectional study. J Infect Dev Ctries. 2014;8:853–862. doi: 10.3855/jidc.3563. [DOI] [PubMed] [Google Scholar]
- Poles G Li M Siril H Mhalu A Hawkins C Kaaya S Aris E Chalamilla G Hirschhorn LR Factors associated with different patterns of nonadherence to HIV care in Dar es Salaam, Tanzania. J Int Assoc Provid AIDS Care. 2014;13:78–84. doi: 10.1177/1545109712467068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Protopopescu C Raffi F Roux P Reynes J Dellamonica P Spire B Leport C Carrieri MP Factors associated with non-adherence to long-term highly active antiretroviral therapy: a 10 year follow-up analysis with correction for the bias induced by missing data. J Antimicrob Chemother. u2e2b;64:599–606. doi: 10.1093/jac/dkp232. [DOI] [PubMed] [Google Scholar]
- Tabatabai J Namakhoma I Tweya H Phiri S Schnitzler P Neuhann F Understanding reasons for treatment interruption amongst patients on antiretroviral therapy – A qualitative study at the Lighthouse Clinic. Glob Health Action. 2014;7:24795–24795. doi: 10.3402/gha.v7.24795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross AJ Aung M Campbell L Ogunbanjo GA Factors that positively influence adherence to antiretroviral therapy by HIV and/or AIDS patients and their caregivers. Afr J Prim Health Care Fam Med. 2011;3:196–200. [Google Scholar]
- Sekoni AO Obidike OR Balogun MR. Stigma, medication adherence and coping mechanism among people living with HIV attending General Hospital. Afr J Prim Health Care Fam Med. 2012;4:417–426. [Google Scholar]
- Senkomago V Guwatudde D Breda M Khoshnood. AIDS Care. 2011;23:1246–1253. doi: 10.1080/09540121.2011.564112. [DOI] [PubMed] [Google Scholar]
- Sax PE Meyers JL Mugavero M Davis KL Adherence to antiretroviral treatment and correlation with risk of hospitalization among commercially insured HIV patients in the United States. PLoS One. 2012;7:e31591–e31591. doi: 10.1371/journal.pone.0031591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzman CW Shea JA Glanz K Jacobs LM Gross R Hines J Mounzer K Samuel R Metlay JP Yehia BR Mapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen’s behavioral model. AIDS Care. 2015;27:817–828. doi: 10.1080/09540121.2015.1009362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu AY Hessol NA Vittinghoff E Amico KR Kroboth E Fuchs J Irvin R Sineath RC Sanchez T Sullivan PS Medication adherence among men who have sex with men at risk for HIV infection in the United States: implications for pre-exposure prophylaxis implementation. AIDS Patient Care STDs. 2014;28:622–627. doi: 10.1089/apc.2014.0195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonell K Naar-King S Huszti H Belzer M Barriers to medication adherence in behaviorally and perinatally infected youth living with HIV. AIDS Behav. 2013;17:86–93. doi: 10.1007/s10461-012-0364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider J Kaplan SH Greenfield S Li W Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med. 2004;19:1096–1103. doi: 10.1111/j.1525-1497.2004.30418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demirkıran F Terakye G Depresif hastaların ilaç tedavisine uyumları ve destekleyici hemşirelik uygulamalarının uyum düzeyine etkisi. Kriz Dergisi. 1998;9:29–39. [Google Scholar]
- Kalichman SC Ramachandran B Catz S Adherence to combination antiretroviral therapies in HIV patients of low health literacy. J Gen Intern Med. 1999;14:267–273. doi: 10.1046/j.1525-1497.1999.00334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monreal MT da Cunha RV Trinca LA Compliance to antiretroviral medication as reported by AIDS patients assisted at the University Hospital of the Federal University of Mato Grosso do Sul. Braz J Infect Dis. 2002;6:8–14. doi: 10.1590/s1413-86702002000100002. [DOI] [PubMed] [Google Scholar]
- Yeap AD Hamilton R Charalambous S Dwadwa T Churchyard GJ Geissler PW Grant AD Factors influencing uptake of HIV care and treatment among children in South Africa – a qualitative study of caregivers and clinic staff. AIDS Care. 2010;22:1101–1107. doi: 10.1080/09540121003602218. [DOI] [PubMed] [Google Scholar]
- Joshi B Chauhan S Pasi A Kulkarni R Sunil N Bachani D Mankeshwar R ART Adherence Study Group. Level of suboptimal adherence to first line antiretroviral treatment&its determinants among HIV positive people in India. Indian J Med Res. 2014;140:84–95. [PMC free article] [PubMed] [Google Scholar]