Abstract
Background/aim
Coronary artery calcification (CAC) and aortic calcification (AC) are significant risk factors for coronary atherosclerosis. This study investigated how breast arterial calcification (BAC) detected from routine mammography correlates with coronary artery calcification and aortic calcification.
Materials and methods
A total of 404 female patients above 40 years of age who, within a 6-month period, had undergone thoracic computed tomography and mammography for various reasons were screened retrospectively at our clinic. Mammographies were assessed for BAC and thoracic CT investigations were assessed for CAC and AC. Patients included in the study were scored as 0 (none), 1 (mild), 2 (moderate), or 3 (severe) depending on the number and shape of CAC, AC, and BAC lesions observed.
Results
Four hundred and four females were enrolled in the study. While BAC was detected in 123 patients, no BAC was observed in the other 281 patients. In the BAC-positive patients, the rates of CAC (45.5% vs. 19.9%, P < 0.001) and AC (67.5% vs. 32.4%, P < 0.001) were notably higher than in the BAC-negative patients. In addition, multivariate regression analysis detected the presence of BAC as an independent variable for both CAC and AC.
Conclusion
The presence of BAC appeared to be a significant risk factor for CAC and AC, and the BAC grade was considered an independent risk factor for CAC.
Keywords: Breast, coronary, aortic, calcification
1. Introduction
Mammography is a screening tool used for investigating breast cancer in women above 40 years of age. The use of mammography for screening has been proven to provide significant advantages and it has been recommended by current practice guidelines. Breast artery calcification (BAC) is an incidental finding detected during mammography that is not associated with malignancy (1). Studies show that BAC is related to age (2), chronic renal disease (3), metabolic syndrome (4), and stroke (5). In addition, some studies support the notion that coronary atherosclerosis may be associated with BAC (6–8).
Coronary artery calcification (CAC) develops during the atherosclerotic process and affects plaque build-up. The calcification that occurs in the fibrous cap of an atheroma may facilitate the development of plaque rupture and a cardiovascular event (9). In addition, there is a well-established correlation between the presence of CAC and unfavorable events (10,11). In this study, the relation between BAC and atherosclerotic calcification (both coronary and aortic) was investigated and its correlation with other risk factors was assessed.
2. Materials and methods
2.1. Patient selection
Women above 40 years of age who had been assessed with both mammography and thoracic computed tomography (CT) within a 6-month period falling between January 2010 and December 2011 were assessed retrospectively. Patients who had received unilateral mastectomy were excluded due to the potential for missing possible calcification in the breast. A total of 404 women were included in the study.
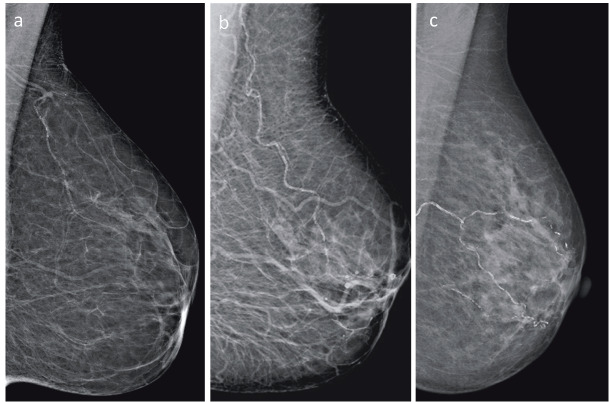
Mammograms were obtained in a bilateral fashion using the Mammomat novation DR (Siemens, München, Germany) conventional mammography device at standard positions. Mammograms were evaluated for BAC at a work station by a radiologist with 5 years of experience in breast radiology. BAC was defined as vascular calcification in one or both breasts. The grade of BAC was determined by using a classification scale defined by Loberant et al. (12). Accordingly, absence of calcification was classified as grade 0; minor punctate vascular calcification as grade I; coarse, tram-track, or ring-type calcification in <3 vessels as grade II; and coarse, vascular calcification in ≥3 vessels as grade III (Figure 1).
Figure 1.
Breast artery calcification (BAC) score in mammography. Grade I small, punctate vascular calcifications (a); grade II coarse or tram-track calcifications, <3 vessels (b); grade III coarse or tram-track calcifications, ≥3 vessels (c).
All thoracic CTs obtained at appropriate time intervals for various etiologic reasons were included in the study. A thoracic CT 16-channel multislice CT device was used, with or without contrast, depending on the etiology. Imaging parameters included the following: 150 mAs, 120 kV, 2 × 16 mm collimation, pitch 1, reconstruction interval 1 mm, and tube rotation period 0.5 s. In order to evaluate the heart and the entire thoracic aorta, the field of view (FOV) was determined to include the space between thoracic entry and the 12th vertebra inferior. Slide thickness was determined on the basis of the etiologic cause and the results were obtained from a 3-mm section for patients with a preliminary diagnosis of pulmonary embolus and a 5-mm section for other thoracic CTs. CTs were evaluated for CAC and AC, and calcifications were scored. Vascular calcification was scored using a simple, predefined visual grading (13). Thoracic aorta calcification was measured at three different localizations as the ascending aorta (0–3), the descending aorta (0–3), and the supraaortic arteries originating from the arcus aorta (0–2). The measurements were then summed and scored as aortic calcification (0–8). On the calcification scale, the absence of calcification in the ascending or descending aorta was defined as grade 0, ≤3 foci as grade I, single calcification extending along 4–5 foci or ≥ 3 sections as grade II, and single calcification extending along >5 foci or ≥3 sections as grade III. For supraaortic arterial calcifications, absence of calcification was classified as grade 0, single artery calcification as grade I, and >1 arterial calcification as grade II. Coronary artery measurements were performed from the main coronary artery, left anterior descending artery, and right coronary artery; the values were then summed and a single number was obtained (0–12). The calcification scale defined absence of calcification as grade 0, presence of 1–2 calcification foci as grade I, single calcification extending >2 foci or ≥2 sections as grade II, and calcification along a long coronary artery segment as calcification grade III.
The protocol was approved by the institutional review boards and adhered to the Declaration of Helsinki. No informed consent was required for this retrospective study.
2.1. Statistical analysis
Statistical analyses were conducted using SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics were provided as mean, standard deviation, frequency, and percentage. The Kolmogorov–Smirnov test was used to evaluate whether continuous variables were normally distributed. Logarithmic transformation was performed for all nonnormally distributed variables. Student’s t-test was used to compare the two groups of values. A comparison of categorical values was carried out by means of the chi-square test. Any correlation between the data was tested with Spearman’s correlation analysis. Multivariate logistic-regression analysis was also performed, and the model included potential confounders (breast artery calcification, diabetes mellitus, age, hypertension, HDL-C, Hs-CRP, creatinine). While continuous data were expressed as mean ± SD (standard deviation), categorical data were expressed as percentage values, and P < 0.05 was accepted as statistically significant.
3. Results
3.1. Baseline clinical characteristics
A total of 404 women were included in the study. Breast artery calcification was detected in 123 patients, while 281 had no BAC. The baseline characteristics of both groups are presented in Table 1. While the groups were similar with respect to incidence of hypertension and diabetes, the BAC-positive patients were older (67.9 ± 9.9 vs. 54.5 ± 9.1 years, P < 0.001). In addition, Hs-CRP levels, HDL-C levels, and hemoglobin levels were all significantly different in the two groups. In 104 of the 123 patients with positive BAC (84.6%), BAC was bilateral; 10 had BAC (8.1%) in the right breast artery only and 9 had BAC (7.3%) in the left breast artery only. The calcification grade was grade I in 44 patients (35.8%), grade II in 40 patients (32.5%), and grade III in 39 patients (31.7%).
Table 1.
Baseline characteristics.
| BAC-negative (n = 281) | BAC-positive (n = 123) | P | |
| Clinical data | |||
| Age, years | 54.5 ± 9.1 | 67.9 ± 9.9 | <0.001 |
| Hypertension (%) (n = 243) | 118 (42.0) | 43 (35.0) | 0.111 |
| Diabetes mellitus (%) | 50 (17.8) | 25 (20.3) | 0.319 |
| Biochemical and hematological data | |||
| Total cholesterol, mg/dL | 197.7 ± 51.8 | 189.3 ± 59.1 | 0.209 |
| Low-density lipoprotein, mg/dL | 121.8 ± 45.6 | 116.7 ± 50.3 | 0.388 |
| High-density lipoprotein, mg/dL | 48.9 ± 20.1 | 42.7 ± 18.6 | 0.012 |
| Triglyceride, mg/dL | 143.5 ± 67.8 | 146.4 ± 78.2 | 0.751 |
| Creatinine, mg/dL | 0.78 ± 0.60 | 0.82 ± 0.35 | 0.410 |
| Fasting glucose, mg/dL | 114.3 ± 46.9 | 121.4 ± 57.6 | 0.236 |
| High sensitivity CRP (mg/dL) (n = 286) | 27.2 ± 42.3 | 45.5 ± 63.9 | 0.004 |
| Hemoglobin, g/dL | 12.1 ± 1.7 | 11.4 ± 1.9 | <0.001 |
| Breast artery calcification | |||
| Right BAC | 10 (8.1) | ||
| Left BAC | 9 (7.3) | ||
| Bilateral | 104 (84.6) | ||
| Degree of breast artery calcification | |||
| 1 | 44 (35.8) | ||
| 2 | 40 (32.5) | ||
| 3 | 39 (31.7) |
BAC: Breast artery calcification, CRP: C-reactive protein.
3.2. Coronary calcification
CAC was detected in 112 (27.7%) of the 404 patients included in our study. Evaluation for coronary calcification showed a notable difference between the two groups. CAC was detected in 56 of the BAC-negative patients (19.9%), while 56 of the BAC-positive patients (45.5%) also had CAC (P < 0.001) (Figure 2). This difference preserved its significance at all coronary localizations. With respect to CAC grade, there were more severe calcifications (grades II and III) in the BAC-positive group. Grade I CAC was present in a greater number of BAC-positive patients, but there was no statistical significance (Table 2).
Table 2.
Vascular calcification of patients.
| BAC-negative (n = 281) | BAC-positive (n = 123) | P | |
| Coronary calcification | 56 (19.9) | 56 (45.5) | <0.001 |
| Localization | |||
| LMCA | 19 (6.8) | 28 (22.8) | <0.001 |
| LAD | 48 (17.1) | 49 (39.8) | <0.001 |
| LCX | 16 (5.7) | 30 (24.4) | <0.001 |
| RCA | 15 (5.3) | 30 (24.4) | <0.001 |
| Degree of coronary calcification | |||
| 1 | 42 (14.9) | 27 (22.0) | 0.085 |
| 2 | 10 (3.6) | 19 (15.4) | <0.001 |
| 3 | 4 (1.4) | 10 (8.1) | 0.001 |
| Aortic calcification | 91 (32.4) | 83 (67.5) | <0.001 |
| Degree of aortic calcification | |||
| 1 | 70 (24.9) | 55 (44.7) | <0.001 |
| 2 | 19 (6.8) | 19 (15.4) | 0.006 |
| 3 | 2 (0.7) | 9 (7.3) | <0.001 |
| Localization of aortic calcification | |||
| Supraaortic calcification | 41 (14.6) | 45 (36.6) | <0.001 |
| Ascendant aortic calcification | 27 (9.6) | 46 (37.4) | <0.001 |
| Descendent aortic calcification | 71 (25.3) | 68 (55.3) | <0.001 |
LMCA: Left main coronary artery, LAD: left anterior descending artery, LCx: left circumflex artery, RCA: right coronary artery.
Figure 2.
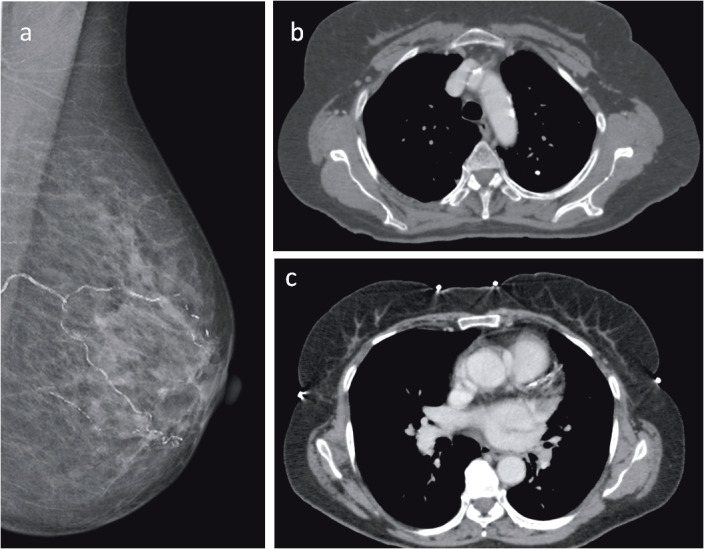
Mammography of a 62-year-old woman with grade III vascular calcification in the left breast: (a) while thoracic CT shows calcified plaques in arcus aorta (b) and left main coronary artery (c).
3.3. Aortic calcification
In terms of AC, 91 BAC-negative patients were detected to have AC (32.4%) while 83 BAC-positive patients (67.5%) had AC (P < 0.001). With respect to the grade of AC, BAC-positive patients had more aortic calcifications at all grades.
3.4. Correlation and regression analysis
Assessment of the parameters that showed correlation with the CAC grade revealed that BAC grade, age, aortic calcification grade, triglyceride level, creatinine level, fasting glucose, and Hs-CRP level positively correlated with the CAC grade. On the other hand, HDL levels showed a negative correlation (Table 3). In addition, a weak correlation was detected between Hs-CRP and BAC (r = 0.205, P < 0.001).
Table 3.
Correlation between coronary artery calcification and others parameters.
| Degree of coronary artery Calcification | ||
| R value | P | |
| Degree of breast artery calcification | 0.376 | <0.001 |
| Age, years | 0.424 | <0.001 |
| Degree of aortic calcification | 0.595 | <0.001 |
| Diabetes mellitus | 0.162 | 0.001 |
| Hypertension | 0.089 | 0.072 |
| Total cholesterol, mg/dL | –0.115 | 0.062 |
| Low-density lipoprotein, mg/dL | –0.099 | 0.079 |
| High-density lipoprotein, mg/dL | –0.180 | 0.001 |
| Triglyceride, mg/dL | 0.129 | 0.023 |
| Creatinine, mg/dL | 0.202 | <0.001 |
| Fasting glucose, mg/dL | 0.170 | 0.001 |
| High sensitivity C-reactive protein, mg/dL | 0.143 | 0.016 |
| Hemoglobin | –0.099 | 0.057 |
Multivariate regression analysis showed that BAC (OR 1.647; 95% CI 1.103–2.460; P < 0.015) and age (OR 1.065, 95% CI 1.016–1.116; P = 0.008) were independent determinants. In addition, the multivariate regression analysis performed to detect the presence of AC revealed that BAC (OR 1.448; 95% CI 1.011–1.136; P < 0.044) and age (OR 1.098; 95% CI 1.061–1.136; P < 0.001) were independent variables (Table 4).
Table 4.
Independent predictors of coronary artery calcification and aortic calcification.
| CAC | AC | |||||||||||
| Univariate logistic regression | Multivariate logistic regression analysis | Univariate logistic regression | Multivariate logistic regression analysis | |||||||||
| Predict | Odds ratio | 95% CI | P-value | Odds ratio | 95% CI | P-value | Odds ratio | 95% CI | P-value | Odds ratio | 95% CI | P-value |
| Breast artery calcification | 2.425 | 1.848–3.183 | <0.001 | 1.647 | 1.103–2.460 | 0.015 | 4.332 | 2.756–6.812 | <0.001 | 1.448 | 1.011–1.136 | 0.044 |
| Diabetes mellitus | 2.687 | 1.354–5.335 | 0.005 | 1.663 | 1.005–2.753 | 0.048 | ||||||
| Age, years | 1.117 | 1.079–1.156 | <0.001 | 1.065 | 1.016–1.116 | 0.008 | 1.121 | 1.094–1.149 | <0.001 | 1.098 | 1.061–1.136 | <0.001 |
| Hypertension | 1.221 | 0.645–2.311 | 0.540 | 1.268 | 0.849–1.896 | 0.246 | ||||||
| HDL-C, mg/dL | 0.959 | 0.936–0.981 | <0.001 | 0.978 | 0.964–0.992 | 0.002 | ||||||
| Hs-CRP, mg/dL | 1.008 | 1.003–1.014 | 0.003 | 1.002 | 0.998–1.007 | 0.313 | ||||||
| Creatinine, mg/dL | 2.506 | 1.268–4.952 | 0.008 | 1.834 | 1.009–3.334 | 0.047 | 1.191 | 0.802–1.767 | 0.386 | |||
CAC: Coronary artery calcification; AC: aortic calcification, HDL: high-density lipoprotein, CRP: C-reactive protein.
4. Discussion
Mammography is a screening tool used for the early diagnosis of breast cancer, which has been proven to reduce mortality. Current guidelines recommend evaluation of women above 40 years of age by means of mammography once a year (1). BAC is a finding that is incidentally detected during mammographic assessment and is not associated with cancer risk. Studies have shown that BAC may be related to atherosclerosis, age, diabetes, and chronic renal disease (14–16).
CAC is associated with reduced vascular compliance, abnormal vasomotor response, and impaired myocardial perfusion (17,18). Alkaline phosphatase plays a central role in vascular calcification (14,15). Vascular smooth muscle cells produce matrix vesicles that control mineralization in the intima and media (16). In addition, cells such as the microvascular pericytes and the adventitial myofibroblasts have the potential to produce a mineralized matrix as well as osteoblastic differentiation (14). Inflammatory mediators and increased lipid accumulation in atherosclerotic lesions induce the osteogenic differentiation of the smooth vascular muscles.
Several studies have shown a strong correlation between CAC grade and plaque burden, severity of atherosclerosis, and future cardiac events (10,11,19). In addition, the presence of CAC is associated with poor prognosis, both in the general population and in patients who have undergone revascularization (20–21). Microcalcifications in the fibrous cap may lead to plaque rupture while calcific nodules may result in disruption of the fibrous cap and thrombosis (9,22). Obstructive fibrocalcific lesions secondary to recurrent plaque ruptures are associated with ischemic clinical outcomes. The presence of CAC also affects the results of therapeutic percutaneous intervention. An analysis that included 6296 patients showed that less complete revascularization was achieved and mortality was higher in patients with CAC (23).
The relation between cardiovascular events and BAC in the media layer has been particularly supported (24). Studies by Maas et al. (6) and Pecchi et al. (7) showed the correlation between CAC and BAC in Caucasian women. Newallo et al. (8) detected that BAC, when detected in African American women, was an independent variable for coronary artery calcium score (>100) and coronary artery stenosis (≥50%). Jiang et al. (25) published a metaanalysis that involved 10 cross-sectional studies and 3952 patients. This analysis showed that the presence of BAC was associated with a 3.86-fold increase in coronary artery disease (CAD) (95% CI 3.25–4.59). In our study, a 2.4-fold increase in CAC risk was detected for all grades of BAC. This correlation also maintained its determining characteristic in multivariate regression models.
The results from previous studies investigating the correlation between BAC and inflammation are controversial. In a study by Maas et al. (26), Hs-CRP and fibrinogen levels were similar in BAC-negative and BAC-positive patients. However, Pidal et al. (27) reported that BAC-positive patients had higher Hs-CRP levels. In our study, CRP measurement was performed with 286 patients, and the BAC-positive patients were observed to have markedly higher CRP levels. Furthermore, in our study, the CRP level showed a significant correlation with both BAC and CAC.
AC reduces arterial elasticity and affects cardiovascular hemodynamics unfavorably (28). This is important when considering the wide range of conditions affected, which include arterial hypertension, aortic valve stenosis, limb ischemia, myocardial infarction, and congestive heart failure. Diffuse calcification causes an increased afterload that is secondary to reduced arterial compliance, resulting in left ventricular hypertrophy and reduced cardiac perfusion (29). Postmortem studies have revealed the association between aortic calcification and atherosclerosis (30). In a metaanalysis by Goncasves et al. (31), which included 11,250 patients, a notable increase in risk was observed for cardiovascular events, cerebrovascular events, and cardiovascular death. This is applicable to both medial and intimal atherosclerosis (32). In their study, Eisen et al. (33) found that cardiovascular events were markedly higher in stable ischemic heart disease patients with aortic calcification as compared to those without calcification. In our study, patients with BAC were observed to have notably higher AC rates and calcification severity. In addition, there was a good correlation between AC and CAC.
The most significant limitation of our study was the fact that clinical CAD data could not be analyzed. The interpretation of the results was made indirectly through CAC. This correlation may not have the same power as that of clinical events. In addition, our retrospective analysis included insufficient data on smoking, which is an important risk factor. Using a standard calcification scoring, such as Agatston, may have been more sensitive. However, simple visual grading, as previously described, was preferred because this method is simple, easy, and can be applied to a whole range of different CT protocols, including nongated CT.
Our study revealed that both CAC and AC are more common in BAC-positive women. In addition, the grade of BAC was found to be an independent risk factor for CAC. These results suggest that positive BAC findings detected in women provide indirect insight into the presence of coronary atherosclerosis and plaque pathology.
References
- Calonge N Petitti DB DeWitt TG Dietrich AJ Gregory KD Grossman D Isham G LeFevre ML Leipzig RM Marion LN Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- Topal U Kaderli A Topal NB Ozdemir B Yesilbursa D Cordan J Ediz B Aydinlar A Relationship between the arterial calcification detected in mammography and coronary artery disease. Eur J Radiol. 2007;63:391–395. doi: 10.1016/j.ejrad.2007.01.035. [DOI] [PubMed] [Google Scholar]
- Duhn V D’Orsi ET Johnson S Orsi D Adams CJ AL ’Neill O WC Breast arterial calcification: a marker of medial vascular calcification in chronic kidney disease. Clin J Am Soc Nephrol. 2011;6:377–382. doi: 10.2215/CJN.07190810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildiz S Toprak H Aydin S Bilgin M Oktay V Abaci O Kocas C The association of breast arterial calcification and metabolic syndrome. Clinics (Sao Paulo) 2014;69:841–846. doi: 10.6061/clinics/2014(12)09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn KJ Kim YJ Cho HJ Yim HW Kang BJ Kim SH Kim HS Kim KT Lee JH Whang IY Correlation between breast arterial calcification detected on mammography and cerebral artery disease. Arch Gynecol Obstet. 2011;284:957–964. doi: 10.1007/s00404-010-1742-4. [DOI] [PubMed] [Google Scholar]
- Maas AH van der Schouw YT Atsma F Beijerinck D Deurenberg JJ Mali WP Breast arterial calcifications are correlated with subsequent development of coronary artery calcifications, but their aetiology is predominantly different. Eur J Radiol. 2007;63:396–400. doi: 10.1016/j.ejrad.2007.02.009. [DOI] [PubMed] [Google Scholar]
- Pecchi A Rossi R Coppi F Ligabue G Modena MG Romagnoli R Association of breast arterial calcifications detected by mammography and coronary artery calcifications quantified by multislice CT in a population of postmenopausal women. Radiol Med. 2003;106:305–312. [PubMed] [Google Scholar]
- Newallo D Meinel FG Schoepf UJ Baumann S De Cecco CN Leddy RJ Vliegenthart R Möllmann H Hamm CW Morris PB Mammographic detection of breast arterial calcification as an independent predictor of coronary atherosclerotic disease in a single ethnic cohort of African American women. Atherosclerosis. 2015;242:218–221. doi: 10.1016/j.atherosclerosis.2015.07.004. [DOI] [PubMed] [Google Scholar]
- Kelly-Arnold A Maldonado N Laudier D Aikawa E Cardoso L Weinbaum S. Revised micro-calcification hypothesis for fibrous cap rupture in human coronary arteries. P Natl Acad Sci USA. 2013;110:10741–10746. doi: 10.1073/pnas.1308814110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland P LaBree L Azen SP Doherty TM Detrano RC Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- Loecker TH Schwartz RS Cotta CW Hickman JR Fluoroscopic coronary artery calcification and associated coronary disease in asymptomatic young men. J Am Coll Cardiol. 1992;19:1167–1172. doi: 10.1016/0735-1097(92)90319-i. [DOI] [PubMed] [Google Scholar]
- Loberant N Salamon V Carmi N Chernihovsky A Prevalence and degree of breast arterial calcifications on mammography: a cross-sectional analysis. J Clin Imaging Sci. 2013;3:36–36. doi: 10.4103/2156-7514.119013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shemesh J Henschke CI Farooqi A Yip R Yankelevitz DF Shaham D Miettinen OS Frequency of coronary artery calcification on low-dose computed tomography screening for lung cancer. Clin Imaging. 2006;30:181–185. doi: 10.1016/j.clinimag.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Demer LL Tintut Y Vascular calcification: pathobiology of a multifaceted disease. Circulation. 2008;117:2938–2948. doi: 10.1161/CIRCULATIONAHA.107.743161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RC Leopold JA Loscalzo J Vascular calcification: pathobiological mechanisms and clinical implications. Circ Res. 2006;99:1044–1059. doi: 10.1161/01.RES.0000249379.55535.21. [DOI] [PubMed] [Google Scholar]
- Abedin M Tintut Y Demer LL Vascular calcification: mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol. 2004;24:1161–1170. doi: 10.1161/01.ATV.0000133194.94939.42. [DOI] [PubMed] [Google Scholar]
- Wang L Jerosch-Herold M Jacobs DR Shahar E Detrano R Folsom AR MESA Study Investigators. J Am Coll Cardiol. 2006;48:1018–1026. doi: 10.1016/j.jacc.2006.04.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalra SS Shanahan CM Vascular calcification and hypertension: cause and effect. Ann Med. 2012;44:85–92. doi: 10.3109/07853890.2012.660498. [DOI] [PubMed] [Google Scholar]
- Sangiorgi G Rumberger JA Severson A Edwards WD Gregoire J Fitzpatrick LA Schwartz RS Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol. 1998;31:126–133. doi: 10.1016/s0735-1097(97)00443-9. [DOI] [PubMed] [Google Scholar]
- Vliegenthart R Oudkerk M Hofman A Oei HH Rooij FJ Witteman JC Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 2005;112:572–577. doi: 10.1161/CIRCULATIONAHA.104.488916. [DOI] [PubMed] [Google Scholar]
- Vavuranakis M Toutouzas K Stefanadis C Chrisohou C Markou D Toutouzas P Stent deployment in calcified lesions: can we overcome calcific restraint with high-pressure balloon inflations? Catheter Cardiovasc Interv. 2001;52:164–172. doi: 10.1002/1522-726x(200102)52:2<164::aid-ccd1041>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Virmani R Kolodgie FD Burke AP Farb A Schwartz SM Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000;20:1262–1275. doi: 10.1161/01.atv.20.5.1262. [DOI] [PubMed] [Google Scholar]
- Bourantas CV Zhang YJ Garg S Iqbal J Valgimigli M Windecker S Mohr FW Silber S de Vries T Onuma Y Prognostic implications of coronary calcification in patients with obstructive coronary artery disease treated by percutaneous coronary intervention: a patient-level pooled analysis of 7 contemporary stent trials. Heart. 2014;100:1158–1164. doi: 10.1136/heartjnl-2013-305180. [DOI] [PubMed] [Google Scholar]
- London GM Guerin AP Marchais SJ Metivier F Pannier B Adda H Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant. 2003;18:1731–1740. doi: 10.1093/ndt/gfg414. [DOI] [PubMed] [Google Scholar]
- Jiang X Clark M Singh RK Juhn A Schnatz PF Association of breast arterial calcification with stroke and angiographically proven coronary artery disease: a meta-analysis. Menopause. 2015;22:136–143. doi: 10.1097/GME.0000000000000300. [DOI] [PubMed] [Google Scholar]
- Maas AH van der Schouw YT Beijerinck D Deurenberg JJ Mali WP Arterial calcium on mammograms is not associated with inflammatory markers for heart disease risk. Heart. 2006;92:541–542. doi: 10.1136/hrt.2005.065953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pidal D Sánchez Vidal MT Rodríguez JC Corte MD Pravia P Guinea O Pidal I Bongera M Escribano D González LO Relationship between arterial vascular calcifications seen on screening mammograms and biochemical markers of endothelial injury. Eur J Radiol. 2009;69:87–92. doi: 10.1016/j.ejrad.2007.08.030. [DOI] [PubMed] [Google Scholar]
- Mackey RH Venkitachalam L Sutton-Tyrrell K Calcifications, arterial stiffness and atherosclerosis. Adv Cardiol. 2007;44:234–244. doi: 10.1159/000096744. [DOI] [PubMed] [Google Scholar]
- Clinical Hypertension. 8th ed. Philadelphia, PA, USA: Lippincott Williams and Wilkins. 2002.
- Giachelli CM Vascular calcification mechanisms. J Am Soc Nephrol. 2004;15:2959–2964. doi: 10.1097/01.ASN.0000145894.57533.C4. [DOI] [PubMed] [Google Scholar]
- Bastos Gonçalves F Voûte MT Hoeks SE Chonchol MB Boersma EE Stolker RJ Verhagen HJ Calcification of the abdominal aorta as an independent predictor of cardiovascular events: a meta-analysis. Heart. 2012;98:988–994. doi: 10.1136/heartjnl-2011-301464. [DOI] [PubMed] [Google Scholar]
- Fantus D Awan Z Seidah NG Genest J Aortic calcification: novel insights from familial hypercholesterolemia and potential role for the low-density lipoprotein receptor. Atherosclerosis. 2013;226:9–15. doi: 10.1016/j.atherosclerosis.2012.08.026. [DOI] [PubMed] [Google Scholar]
- Eisen A Tenenbaum A Koren-Morag N Tanne D Shemesh J Imazio M Fisman EZ Motro M Schwammenthal E Adler Y Calcification of the thoracic aorta as detected by spiral computed tomography among stable angina pectoris patients: association with cardiovascular events and death. Circulation. 2008;118:1328–1334. doi: 10.1161/CIRCULATIONAHA.107.712141. [DOI] [PubMed] [Google Scholar]