Abstract
This meta-analysis examined the effects of early interventions on social communication outcomes for young children with autism spectrum disorder. A systematic review of the literature included 1442 children (mean age 3.55 years) across 29 studies. The overall effect size of intervention on social communication outcomes was significant (g = 0.36). The age of the participants was related to the treatment effect size on social communication outcomes, with maximum benefits occurring at age 3.81 years. Results did not differ significantly depending on the person implementing the intervention. However, significantly larger effect sizes were observed in studies with context-bound outcome measures. The findings of this meta-analysis highlight the need for further research examining specific components of interventions associated with greater and more generalized gains.
Keywords: Autism spectrum disorders, Social communication, Early intervention, Meta-analysis
Introduction
Autism spectrum disorder (ASD) is a developmental disorder characterized by: (1) deficits in social communication and interactions with others and (2) repetitive or restricted behaviors and interests (American Psychology Association 2013). According to the Centers for Disease Control, about 1 in 59 children are diagnosed with ASD (Baio et al. 2018). Although both core features must be present for an ASD diagnosis, social communication is of particular concern, as deficits in communication are correlated with a host of other developmental challenges, including decreased academic performance, increased problem behavior, and difficulties forming relationships with others (Koegel et al. 1992; Bauminger and Kasari 2000; Mundy et al. 1986). Early deficits in language and communication are predictive of communication abilities into adulthood (Gillespie-Lynch et al. 2012).
Social communication is defined as the sharing of information, thoughts, or ideas with another person (Mundy et al. 1986). The key feature of this definition is that it requires intentional communication to another person, meaning that it goes beyond the ability to produce spoken language, and can include nonverbal communication through gestures and eye contact. Social communication is essential to initiating joint attention, behavior regulation, and engaging in social interaction. These early social communication skills are important precursors to expressive language for children with ASD, especially in the case of joint attention behaviors. Correlational studies have found significant associations between joint attention skills and later language abilities, such that children with more early joint attention behaviors show better long-term expressive language outcomes (Mundy et al. 1990; Sigman and Ruskin 1999; Charman 2003). In addition, children who received an intervention targeting early social communication skills have shown greater long-term language improvements than children in a control group (Kasari et al. 2010). This research suggests that interventions that increase a child’s social communication skills may result in improved language use, including better long-term language and communication outcomes.
Early interventions addressing core behavioral and skill deficits associated with ASD are of particular interest given the large numbers of young children with ASD and current policies for serving these children. Currently, the American Academy of Pediatrics Council on Children with Disabilities recommends a minimum of 25 h per week in ASD related interventions (Myers and Johnson 2007). Intensive behavioral interventions for children with ASD may cost as much as $40,000–$60,000 per child per year (Amendah et al. 2011). Following recommendations for treatment of ASD may present a sizable economic burden for families and the high costs associated with treating this disorder are concerning. In this context, it is especially important to determine the effectiveness of early interventions for improving social communication.
Intervention Components Related to Outcomes
By systematically evaluating current research on interventions targeting social communication outcomes for children with ASD, it would be possible to make more informed evidence-based recommendations for treatment of this population. This includes understanding how study characteristics, including the characteristics of the study participants and the intervention delivery, and study methodology, including the measurement type and potential bias, are related to study outcomes.
Age
Age of entry into intervention programs has been linked to outcomes including school placement, such that earlier placement in services was related to placement in more inclusive school settings (Harris and Handleman 2000). In a review of early intensive behavioral interventions (EIBI), Granpeesheh et al. (2009) found a relationship between age and treatment progress such that younger children (ages 2.5–5.15 years) made more progress in their treatment programs compared to older children (ages 5.15–7.14 years), and younger children made greater gains even from lower intensity programs. These studies support the need for increased access to intervention at earlier ages.
Dosage
In addition to the relationship of age and intervention outcomes, the dosage and duration of intervention have been important factors to consider. In a meta-analysis of outcomes from interventions using the principles of applied behavior analysis (Virués-Ortega 2010), children who had received longer-term interventions (at least 45 weeks with 10 h of therapy per week) showed better outcomes. Similarly, in addition to a relationship between age and outcomes, Granpeesheh et al. (2009) found a relationship between dosage and treatment progress, such that children who had received higher intensity treatment, or more hours of treatment per week, mastered more treatment programs compared to children who received lower intensity treatments. Although these studies concluded that more treatment is better, other studies have found inconclusive relationships between dosage and outcomes (e.g., Hampton and Kaiser 2016). Understanding the effect of treatment dosage specifically on social communication outcomes may have important implications for policy and resource allocation.
Agent of Implementation
The person implementing the intervention is a critical feature in intervention delivery. Parents have been shown to be effective implementers of language and communication interventions (Roberts and Kaiser 2011). A recent meta-analysis of spoken language outcomes for early interventions for children with ASD reported that the largest outcomes were associated with interventions that included both a parent and a therapist in the intervention delivery (Hampton and Kaiser 2016). The person implementing the intervention can have an important impact on intervention outcomes as this person brings prior skills and experience, fidelity of implementation, and a relationship with the child to the intervention context. Further, the person implementing the intervention could have an important impact on dose of intervention, such that parents and school staff have the potential to implement intervention at a higher dose in the child’s daily life than therapists alone.
Measurement
Lastly, there is evidence suggesting that the context in which the outcome measures are assessed may influence the reported magnitude of effects in social communication interventions. In a review of 23 studies examining social communication outcomes for children with ASD, Yoder et al. found that studies using context-bound measures, or measurement contexts in which the settings, materials, communication partners, or interaction styles are highly similar to the treatment context, had an 82% probability of a positive treatment effect, compared to a 33% probability for studies that used generalized measures (Yoder et al. 2013). Examining how the measurement context is related to the magnitude of the results is especially important because children with ASD have difficulty generalizing communicative behaviors to untrained contexts (Hwang and Hughes 2000; Whalen and Schreibman 2003). Context-bound measures may overestimate the impact of an intervention on functional communication skills outside of the treatment setting.
Previous Reviews
To date, no quantitative meta-analyses have examined the effects of early interventions on social communication outcomes for children with ASD. In a best evidence review of early social communication interventions, Yoder et al. (2013) found that although the majority of the 23 included studies reported positive effects on social communication, this finding may have been driven by the use of context-bound outcome measures. Because the review included both single case design studies and group design studies, the authors categorized the outcomes in terms of effectiveness (e.g., strong evidence of treatment effect was demonstrated for 54% of the dependent variables) rather than calculating an aggregated effect size metric. The current meta-analysis extends the Yoder et al. (2013) review by examining group experimental design studies through 2016 and calculating an aggregated effect size to quantify the magnitude of effect.
A systematic review and meta-analysis of spoken language outcomes from early interventions for children with ASD was conducted by Hampton and Kaiser (2016). The review included 1738 child participants under age 8 from 26 group design studies. In general, early intervention had positive effects on spoken language for children with ASD; a significant aggregated effect size of g = 0.26 was reported. Largest effects were found for interventions delivered by both parents and clinicians (g = 0.42), followed by parents only (g = 0.11) and clinicians only (g = 0.08). The review examined only spoken language outcomes and did not include social communication outcomes.
Other reviews and meta-analyses have examined specific types of interventions rather than outcome measures, including social skills interventions (Bellini et al. 2007) and early behavioral interventions (Eldevik et al. 2009) for children with ASD. To date, no meta-analysis specifically examining social communication outcomes has been conducted.
Purpose and Research Questions
The purpose of the current study was to conduct a systematic review and meta-analysis of the effects of intervention on social communication in children with ASD under age 8. The following questions were addressed: (1) do early interventions result in significant increases in social communication behaviors for young children with ASD? (2) do the sizes of treatment effects on social communication vary by the age of the participants, dosage, person implementing the intervention, and measurement context?
Method
Systematic Literature Search
Eligibility Criteria
Inclusion criteria are listed in Table 1. Studies were included if they enrolled participants with ASD or at risk for ASD under 8 years of age. Only studies examining educational, naturalistic, or behavioral interventions were included in this analysis; pharmacological or dietary treatments were not included. Study design was restricted to group comparison studies (randomized control trials or quasi experimental designs). All included studies were required to have a nontreatment comparison group, which could include: business as usual, waitlist control, or parent education only. All included studies reported a measure of social communication as an outcome of the intervention. Studies reporting expressive language outcomes were eligible for this review only if the definition for expressive language specified that a social indicator was paired with language. Studies that reported standardized measures of expressive language only, such as a vocabulary measure, a measure of direct imitation, or a response to a prompt or question, were excluded. Studies that reported broader social behaviors using standardized measures were not included unless the measurement instrument had a specific subscale measuring social communication behaviors (e.g., ADOS Social Communication subscale; Lord et al. 2008). Only studies conducted in English were included. Both published and unpublished studies were eligible for inclusion.
Table 1.
Inclusion criteria and search terms
| Inclusion criteria | Criteria | Corresponding search terms |
|---|---|---|
| Participants | Autism spectrum disorder, younger than 8 | auti* OR ASD OR PDD OR Asperger |
| Intervention | Behavioral or developmental intervention, excluding pharmacological or dietary components | intervention OR therapy OR teach* OR treat* |
| Comparison | Treatment as usual, waitlist control, general information only, or referral to other services | assign* OR “control group” OR BAU OR “wait list” OR RCT OR random* OR quasi OR “treatment group” OR “intervention group” OR “group design” OR (before AND after) OR trial |
| Outcome | Social communication | “commun*” or “social interact*” or “social function*” or “joint attention” or “joint engagement” or “ESCS” or “CSBS” |
| Study Design | Group design study, including randomized control trial and quasi experimental design | |
| Language | English journals | La.exact(English) |
Search Procedures
A total of 11 databases were searched through Proquest: Dissertations and Theses at Vanderbilt University, ERIC, International Bibliography of the Social Sciences, Linguistics and Language Behavior Abstracts, PAIS International, ProQuest Central, ProQuest Dissertations and Theses: UK and Ireland, ProQuest Dissertations and Theses Full Text, ProQuest Dissertations and Theses Global, PsycARTICLES, and PsycINFO. The final search was conducted in December 2016. In addition to searching dissertations and theses using the online databases, proceedings from relevant conferences (e.g. International Meeting for Autism Research) and reference lists were searched to identify unpublished or “gray” literature. The search and study selection process were completed by the first author and a graduate student.
Variables
Definitions of study variables are in Table 2. One effect size was extracted from each study. If a study reported more than one measure of social communication, the following hierarchy was used to select the measure for analysis: (1) scores from structured observational assessments (e.g. Early Social Communication Scales, Mundy et al. 2003), (2) scores from unstructured observational assessments (e.g. an observation of the parent and child), and (3) parent or school staff reported scores (Social Responsiveness Scale, Social Communication Subscale, Constantino 2002). This hierarchy was based on two reasons: first structured measures are more reliable and less variable, and second, because many of the studies used designs that included a parent or a member of the school staff, observational scores and reports from these individuals are susceptible to correlated measurement error and the failure to use blind reporting.
Table 2.
Variable definitions
| Variable | Definition |
|---|---|
| Age | Mean age of participants (years) |
| Dose | Total dose: total hours of intervention Duration: total number of weeks of intervention |
| Person implementing | Clinician: intervention directly implemented by the researcher or therapist Parent: parent implemented part or all of the intervention School staff: any school employee implemented part or all of the intervention |
| Measurement type | Context bound: outcome was measured with the same person and in the same context (setting and materials) as the intervention was conducted Semi-generalized: outcome was measured with the same person and in a different context (setting and materials) as the intervention was conducted Generalized: outcome was measured with a different person and in a different context (setting and materials) as the intervention was conducted |
Hedges’ g was used to calculate the standardized mean difference effect size between treatment groups (intervention and control) for social communication outcomes. Hedges’ g was selected because it corrects the slight bias in Cohen’s d that occurs in studies with small sample sizes (Borenstein et al. 2009). Because of the variability in sample sizes across studies, Hedges’ g was a more conservative estimate of effect. When studies did not report means and standard deviations, the effect size was calculated from an F-statistic or a beta weight. In the case when F-statistics were used, the effect size was derived from a group*time ANOVA, which mitigates the concern of effect-size inflation.
Risk of Bias
Risk of bias was rated for each study to characterize the quality of the studies included in the meta-analysis. Risk of bias was rated on five applicable quality indicators recommended by the Cochrane Collaboration (Higgins et al. 2011): selection (use of random assignment and establishment of pretreatment equivalence), detection (use of blind coders and blind assessors), and attrition (use of intent to treat analysis). Each item was scored using a binary scale, with a score of one assigned for compliance with the quality indicator and a score of zero assigned for noncompliance or failure to report. Scores across indicators were summed, for a total possible score of 5. Higher scores indicated more compliance with quality indicators or a reduced risk of bias. More information on risk of bias indicators is in Table 3.
Table 3.
Risk of bias definitions and quality indicators
| Risk of bias | Definition | Study quality indicator |
|---|---|---|
| Selection bias | Systematic differences between groups on relevant baseline characteristics. Minimized by random assignment and post-hoc testing to establish group equivalence at baseline | 1. Did the study use random assignment of participants to treatment groups? 2. Did the study use post-hoc testing to confirm between group equivalence on relevant pre-treatment variables? |
| Performance | Systematic differences between groups are due to exposure other than the intervention of interest. Minimized by masking participants such that they are unaware of their group assignment | Masking participants to a behavioral intervention is not generally possible. No variables coded |
| Detection | Systematic differences between groups on how outcomes are measured. Minimized by using blind assessment of outcome variables | 3. Were assessors blind to group assignment? 4. Were coders blind to group assignment? |
| Attrition | Systematic differences in withdrawals from study, including removal from analyses. Minimized by including all randomized participant in the analysis | 5. Was an intent to treat analysis (i.e. analyzed as randomized) used? |
| Reporting | Systematic differences in reporting of findings, such that significant findings are reported and/or published and nonsignificant findings are not reported | Analysis of publication bias was used to identify possible gaps in reporting |
Analytic Strategies
Due to the observed variability in types and dosage of intervention in the included studies, a random effects model was used to aggregate effect sizes. According to Borenstein et al. (2009), a random effects model assumes that the true effects of intervention are normally distributed with a between study variance represented by τ2. A random effects model assigns slightly more weight to smaller studies than a fixed-effects model. The heterogeneity of effect sizes was examined using τ2 along with the Q statistic and I2.
To address the second research question, subgroup analyses and meta-regressions were conducted for the variables identified. Continuous variables were examined via separate random effect meta-regressions for the following variables: risk of bias, dosage, and age. Risk of bias was included to understand the potential relationship between study quality and outcomes. Regression models were built using visual inspection of the data and model fit statistics to determine the appropriate form of the independent variable (e.g., quadratic). Fixed effects subgroup analyses were used for categorical variables: measurement type and person implementing. Fixed effect models were used in subgroup analyses so that between-group differences could be analyzed using Q.
All coded variables on 100% of included studies were coded by two independent coders. Overall reliability of independent ratings across all coded measures was 86.38% (SD = 14.23; range 68.96–100.00%). Disagreements were resolved via consensus coding by the two observers and verified by examining the manuscript of the study such that 100% agreement on all variables was reached. Lastly, although efforts were made to minimize publication bias by including gray literature searches, analyses were included to detect bias. Publication bias was examined through visual analysis of a funnel plot and the Egger’s test of small study bias (Egger et al. 1997).
Results
Study Selection
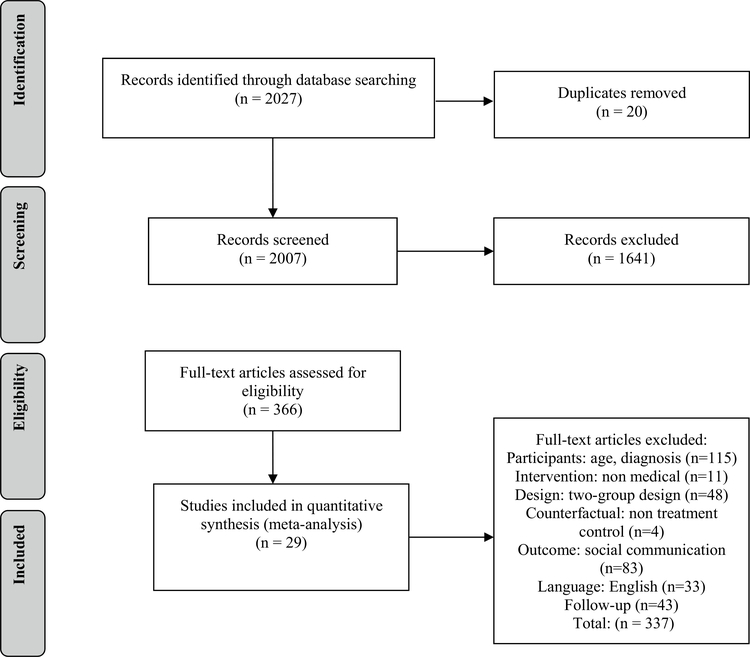
A total of 2007 studies were identified in the search after duplicates were removed. After the initial and full-text screening of the identified articles, a total of 29 studies (24 published manuscripts and 5 dissertations/theses) were included in the final analysis. A PRISMA diagram of exclusion procedures is in Fig. 1.
Fig. 1.
PRISMA description of exclusion process. The process of screening and excluding articles is explained
Study Characteristics
Descriptive statistics for the included studies are shown in Table 4. A total of 1592 participants (at pretest) were included across the 29 selected studies. Data on social communication outcomes for 1442 participants were included in the final analysis: 786 intervention participants and 656 control participants. The mean age of participants was 3.55 years. Twenty-six studies measured social communication outcomes using observational measures (Early Social Communication Scales, Mundy et al. 2003; Communication and Symbolic Behavior Scales; Wetherby and Prizant 2002; parent-child interactions; ADOS social communication subscale; Lord et al. 2008; and Precursors of Joint Attention Measure; Schertz et al. 2013) and three used a parent report (Social Responsiveness Scale, Constantino 2002; Parent Interview for Autism; Stone et al. 2003). The duration of intervention varied greatly, ranging from 1 week to 2 years.
Table 4.
Summary descriptions of included studies
| Study | Outcome | Study components |
Intervention components |
Participant characteristics |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author and year | Hedges’ g | Risk of bias | Measurement type | Measure | Publication type | Person implementing | Weeks of intervention | Hours per week | Participants | Mean age (years) | Male (%) | Non-white (%) |
| Goods et al. (2013) | −0.386 | 2 | Generalized | ESCS-HA | Peer reviewed | Clinician | 12 | 1 | 11 | 4.06 | – | – |
| Kasari et al. (2010) | −0.180 | 3 | Semi-generalized | CCX-IJA | Peer reviewed | Parent | 8 | 3 | 38 | 2.53 | 76.5 | 42 |
| Turner-Brown et al. (2016) | −0.158 | 4 | Context bound | PIA-Nonverbal Comm | Peer reviewed | Parent | 24 | 2 | 49 | 2.4 | 87.5 | 24 |
| Carter et al. (2011) | −0.125 | 4 | Generalized | ESCS-IJA | Peer reviewed | Parent | 20 | 0.6 | 52 | 1.75 | 82 | |
| Kamps et al. (2015) | 0.044 | 2 | Semi-generalized | Peer interaction-comm acts | Peer reviewed | School Staff | 104 | 0.46 | 85 | 5.8 | 83.2 | 24 |
| Remington et al. (2007) | 0.048 | 2 | Generalized | ESCS-IJA | Peer reviewed | Parent | 104 | 25.6 | 37 | 2.975 | – | – |
| Keen et al. (2010) | 0.049 | 4 | Generalized | CSBS-Soc Comm | Peer reviewed | Parent | 6 | 2 | 39 | 3.031 | 80.5 | – |
| Rogers et al. (2012) | 0.069 | 4 | Generalized | ADOS-Soc Affect | Peer reviewed | Parent | 12 | 1 | 81 | 1.75 | 69 | 27 |
| Venker et al. (2012) | 0.092 | 2 | Semi-generalized | CCX-comm initiation | Peer reviewed | Parent | 10 | 2.6 | 14 | 3.43 | – | – |
| Clionsky (2015) | 0.097 | 2 | Context bound | SRS-Soc Comm | Dissertation/Thesis | Parent | 12 | 1.25 | 30 | 4.75 | 80 | 13 |
| Chang et al. (2016) | 0.112 | 5 | Generalized | ESCS-IJA | Peer reviewed | School Staff | 9 | 1.77 | 63 | 4.07 | 84 | 71 |
| Green et al. (2010) | 0.135 | 5 | Generalized | ADOS-Soc Comm | Peer reviewed | Parent | 52 | 0.69 | 152 | 3.75 | 90.5 | 42 |
| Kasari et al. (2015) | 0.160 | 3 | Semi-generalized | CCX-IJA | Peer reviewed | Parent | 10 | 1 | 83 | 2.55 | 81 | 39 |
| McCalla (2014) | 0.218 | 3 | Semi-generalized | Peer interaction-comm acts | Dissertation/Thesis | Clinician | 10 | 0.5 | 19 | 4.9 | 89.5 | 15 |
| Boyd et al. (2014) | 0.321 | 2 | Generalized | Parent report | Peer reviewed | School Staff | 104 | 30 | 162 | 3.98 | 84.5 | 70 |
| Openden (2005) | 0.329 | 3 | Context bound | CCX-comm acts | Dissertation/Thesis | Parent | 1 | 20 | 32 | 4.8 | 89 | 35 |
| Hardan et al. (2015) | 0.412 | 3 | Semi-generalized | CCX-comm acts | Peer reviewed | Parent | 12 | 1.33 | 47 | 4.1 | 74.5 | – |
| Karst (2010) | 0.481 | 0 | Context bound | CCX-IJA | Dissertation/Thesis | Parent | 20 | 15 | 32 | 4.08 | 79.5 | 6 |
| Kasari et al. (2006) | 0.601 | 4 | Generalized | ESCS-IJA | Peer reviewed | Clinician | 6 | 2.5 | 58 | 3.6 | 81.5 | 30 |
| Lawton and Kasari (2012) | 0.630 | 4 | Generalized | ESCS-IJA | Peer reviewed | School Staff | 6 | 1 | 16 | 3.83 | – | 43 |
| Aldred et al. (2004) | 0.710 | 5 | Semi-generalized | CCX-comm acts | Peer reviewed | Parent | 52 | 0.75 | 28 | 4 | 89.2 | – |
| Wetherby and Woods (2006) | 0.811 | 1 | Semi-generalized | CSBS-IJA | Peer reviewed | Parent | 52 | 2 | 35 | 2.56 | 83 | – |
| Salt et al. (2002) | 0.853 | 0 | Generalized | ESCS-IJA | Peer reviewed | Clinician | 40 | 4 | 17 | 3.53 | 79.5 | – |
| Ingersoll (2012) | 0.859 | 2 | Generalized | ESCS-IJA | Peer reviewed | Clinician | 10 | 3 | 27 | 3.275 | 89 | 37.5 |
| Nefdt (2007) | 0.894 | 3 | Context bound | CCX-comm acts | Dissertation/Thesis | Parent | 1 | 1 | 27 | 3.24 | 92 | 18 |
| Solomon et al. (2014) | 0.923 | 4 | Context bound | CCX-CBRS | Peer reviewed | Parent | 52 | 0.69 | 112 | 4.15 | 82 | 50 |
| Field et al. (1997) | 0.977 | 2 | Generalized | ESCS-IJA | Peer reviewed | Clinician | 4 | 0.5 | 22 | 4.5 | 54 | – |
| Shertz et al. (2013) | 1.029 | 3 | Semi-generalized | CCX-IJA | Peer reviewed | Parent | 16 | 1 | 23 | 2.05 | – | – |
| Casenhiser et al. (2013) | 1.221 | 4 | Generalized | CCX-IJA | Peer reviewed | Parent | 52 | 2 | 51 | 3.54 | – | – |
Measures are as follows: Comm acts frequency of communication acts (verbal or nonverbal); IJA initiations of joint attention; ESCS Early Social Communication Scale (Mundy et al. 2003); CCX Caregiver-child interaction; PIA-Nonverbal Comm Parent Interview for Autism- Nonverbal communication subscale, (Stone et al. 2003); CSBS-Soc Comm subscale Communication and Symbolic Behavior Scales, Social Communication subscale (Wetherby and Prizant 2002); ADOS Autism Diagnostic Observation Schedule, Social Communication algorithm or Social Affect subscale (Lord et al. 2008); CBRS Child Behavior Rating Scale (Mahoney et al. 2007); Parent report Factor score of Social Responsiveness Scale (SRS; Constantino 2002) and Pictorial Infant Communication Scale (PICS; Delgado et al. 2001)
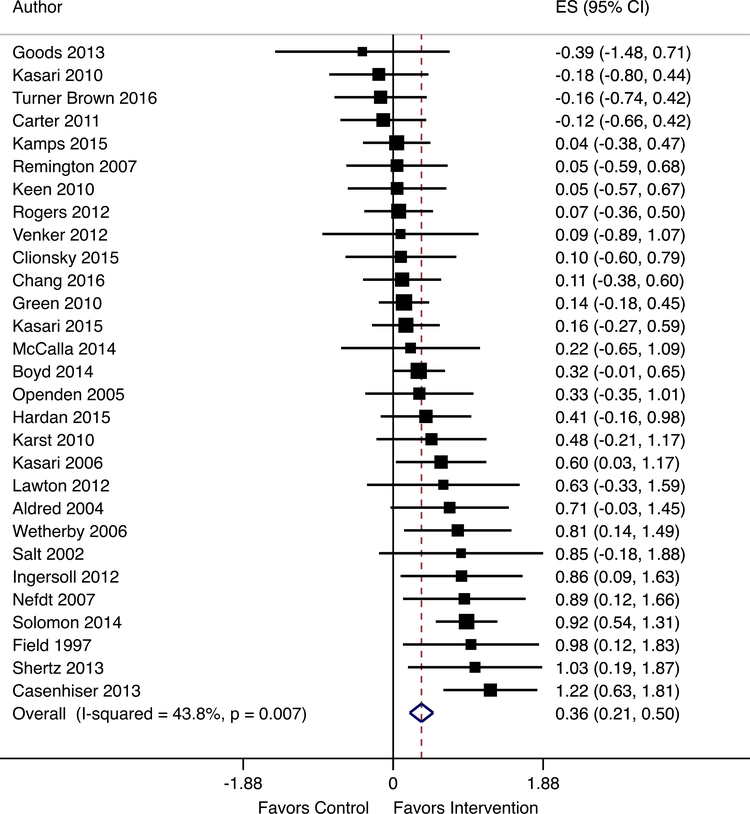
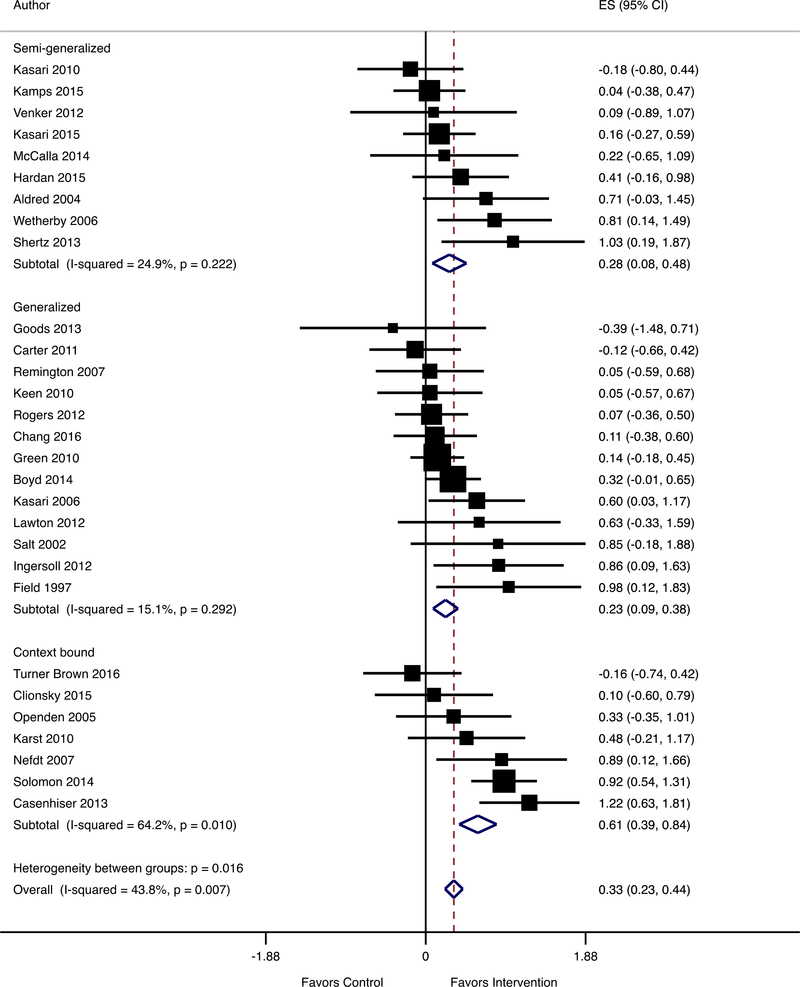
Main Effects
Figure 2 shows the results of the meta-analysis examining the effects of early interventions on social communication for children with ASD. The effect size and confidence interval for each of the 29 studies are shown. Larger black boxes around the effect sizes represent larger weights in the meta-analysis. The random effects model aggregated the effect sizes for an overall effect size of g = 0.355 (95% CI [0.207–0.503], p < 0.001). These findings suggest that children in early interventions showed significantly greater improvements on measures of social communication compared to children in control groups. The results also indicated that there was a significant amount of heterogeneity between the studies (Q = 49.83, p = 0.007, I2 = 43.8%, τ2 = 0.065). This level of observed heterogeneity justified the use of the predetermined subgroup analyses and meta-regression analyses.
Fig. 2.
Main effect of intervention on social communication outcomes. Random effect meta-regression of social communication outcomes from 29 included studies. Weighted effect sizes of included studies are represented by black boxes and standard errors are represented by black bars. Hedges’ g effect sizes and confidence intervals are reported
Risk of Bias
The studies varied in compliance with quality indicators, with an average rating of 2.93 out of 5 (SD = 1.33). The most frequent risks of bias were failure to use, or to report the use of, blind assessors, followed by the failure to use an intent to treat analysis. A meta-regression analysis showed that the risk of bias score was not significantly related to the treatment effect size on social communication outcomes (β = − 0.034, p = 0.576). Additionally, risk of bias scores did not explain any of the observed heterogeneity in the sample (I2=45.25%, Adjusted R2 = 0%).
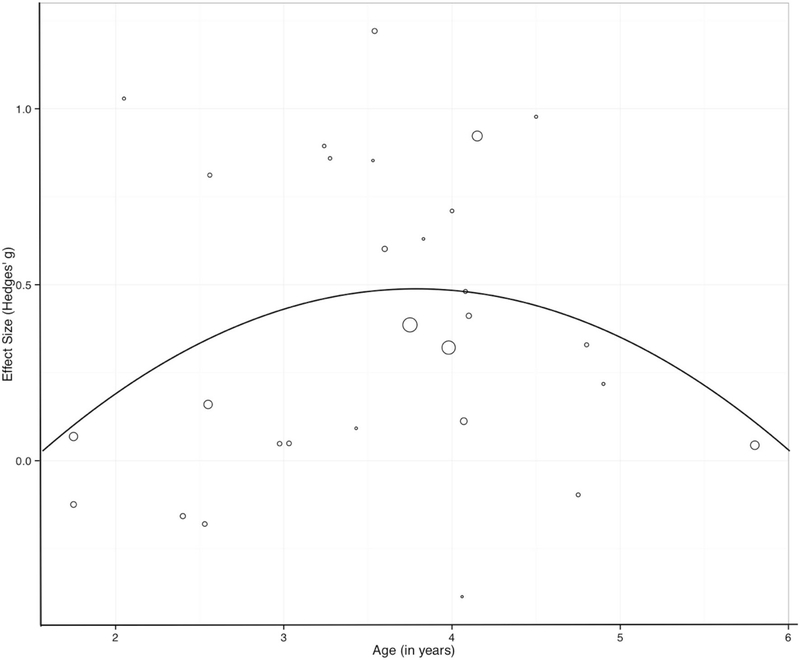
Age of Participants
A quadratic meta-regression was used to evaluate the relationship between the mean age of the participants and the treatment effect size on social communication outcomes, shown in Fig. 3. A quadratic term was included in the analysis based on (1) visual inspection of the data and (2) model fit statistics. The mean age of participants, in years, was a significant predictor of treatment effect size on social communication outcomes, such that older participants were associated with larger outcomes (β = 0.84; p = 0.039). The quadratic of participant age was also a significant predictor of treatment effect size, but in the opposite direction (β = − 0.11; p = 0.049), indicating that the benefit of age diminished as children approached 8 years. Optimal outcomes were observed at age 3.81 years. Including age in the model explains some of the observed heterogeneity in the sample (τ2 = 0.052, I2 = 37.28%, Adjusted R2 = 24.40%).
Fig. 3.
Bubble plot of meta regression outcomes for the quadratic relationship between age and effect size. Size of the circle represents the studies’ relative weight in the random effects model
Dosage of Intervention
The total dosage of intervention (measured as the total number of hours) and the duration or intervention (measured as length in weeks) were used as two measures of intervention dosage. Total dosage and duration were not significant predictors of treatment effect sizes on social communication outcomes, using separate meta-regressions (total dosage: β=− 0.00003, p = 0.746; duration: β = 0.00082, p = 0.972). Additionally, neither dose nor duration explained any of the observed heterogeneity in the sample (dosage: I2 = 48.34% Adjusted R2 = 0%; duration: I2=45.81% Adjusted R2=0%).
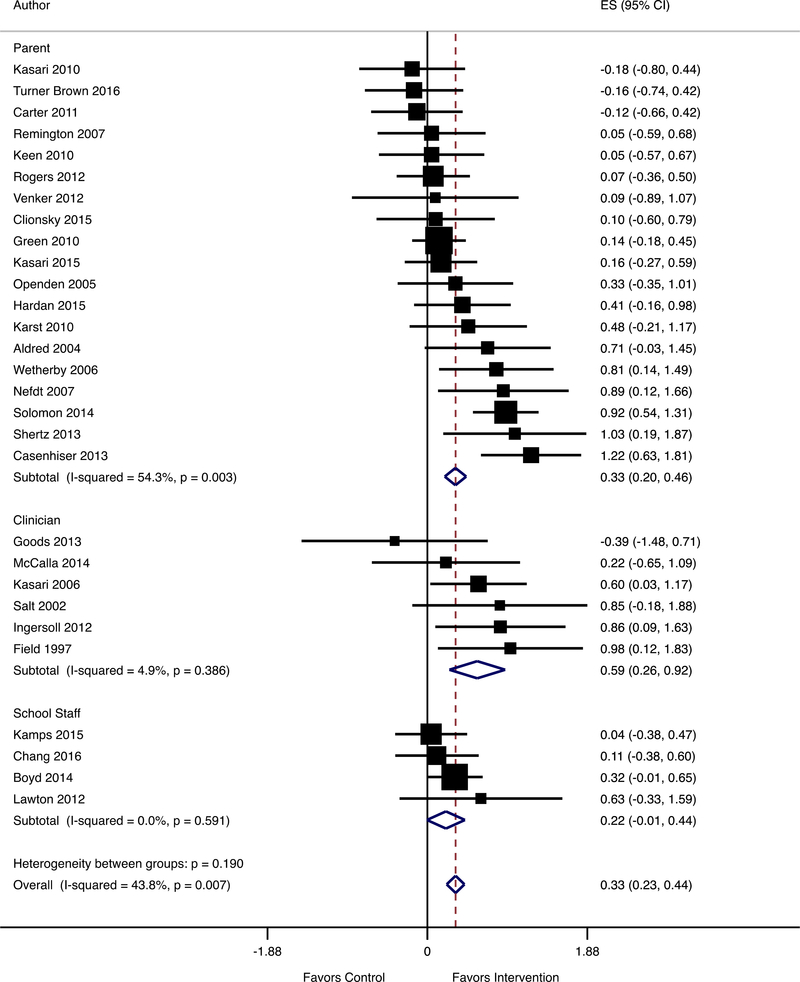
Person Implementing
A subgroup analysis examined the effect of the person who delivered the intervention. The results of this analysis are shown in Fig. 4. A total of 19 studies included the parent in the intervention, four studies included school staff in the intervention, and six studies were implemented directly by clinicians (researcher or therapist). The largest effect sizes were shown when the intervention was delivered by clinicians (g=0.587, 95% CI [0.258–0.916], p < 0.001, Q = 5.26, I2 = 4.9%, k = 6), followed by parents (g = 0.330, 95% CI [0.203–0.447], p < 0.001, Q = 39.35, I2 = 54.3%, k = 19), and school staff (g = 0.218, 95% CI [− 0.006 to − 0.441], p = 0.057, Q = 1.91, I2 = 0%, k = 4). The only effect size that was not statistically significant at the 0.05 level was the effect for interventions implemented by school staff; however, this effect size was calculated from only four studies. There was no significant between-group variance (Q = 3.32, p = 0.190), indicating that the effect size of intervention did not differ significantly based on the interventionist.
Fig. 4.
Subgroup analysis of social communication outcomes by person implementing the intervention. Diamonds represent the aggregated effect size of each subgroup using a fixed effect meta-analysis. Hedges’ g effect sizes and confidence intervals are reported. Nonsignificant heterogeneity between groups (p = 0.190) indicates no significant different results dependent on implementer
Measurement Type
The type of measure was examined with a subgroup analysis of the three measurement types: context-bound, semi-generalized, and generalized. The results of this analysis are shown in Fig. 5. The largest effect sizes were observed when the measurement tool was context-bound, or measured with the same partner, setting, and materials as the intervention was delivered. For context-bound measures, the aggregated effect size was g = 0.615 (95% CI [0.394–0.836], p < 0.001, Q = 16.75, I2 = 64.2%, k = 7). For semi-generalized measures, where the partner was the same but the setting and materials were different, the aggregated effect size was smaller but remained significant (g = 0.279, 95% CI [0.077–0.481], p = 0.007, Q = 10.65, I2 = 24.9%, k = 9). For generalized measures, in which the partner, setting, and materials were different in the measurement context compared to the intervention context, the aggregated effect size was smaller compared to the effect size for context-bound measures but similar to the effect size of the semi-generalized measures (g = 0.234, 95% CI [0.086–0.381], p = 0.002, Q = 14.14, I2 = 15.1%, k = 13). There was significant between-group variance (Q = 8.29, p = 0.016), indicating the effect size of intervention differed significantly based on the measurement type.
Fig. 5.
Subgroup analysis of social communication outcomes by measurement type. Diamonds represent the aggregated effect size of each subgroup using a fixed effect meta-analysis. Hedges’ g effect sizes and confidence intervals are reported. Significant heterogeneity between groups (p = 0.007) indicates significant different results dependent on measurement type
Relationship Between Variables
Table 5 provides information on the relationships between variables. There were no significant relationships (using ANOVAs) between the two categorical variables (person implementing and measurement type) and the four continuous variables (risk of bias, age, hour of intervention, or weeks of intervention), with the exception that interventions delivered by school staff was associated with higher average ages of participants.
Table 5.
Relationship between variables
| Subgroup | Risk of bias (SD) | Age (SD) | Dosage-hours (SD) | Dosage-weeks (SD) | % Context bound | % Semi-generalized | % Generalized |
| Parent (k = 19) | 3.11 (1.29) | 3.23 (0.94) | 4.4 (7.28) | 27.16 (26.55) | 37% | 26% | 37% |
| Researcher (k = 6) | 2.17 (1.33) | 3.98 (0.63) | 1.92 (1.46) | 13.67 (13.23) | 0% | 17% | 83% |
| School (k = 4) | 3.25 (1.5) | 4.42 (0.93)* | 8.31 (14.47) | 55.75 (55.73) | 0% | 25% | 75% |
| Risk of bias (SD) | Age (SD) | Dosage-hours (SD) | Dosage-weeks (SD) | % Parent | % Researcher | % School | |
| Context bound (k = 7) | 2.86 (1.46) | 3.85 (0.86) | 5.99 (8.01) | 23.14 (21.53) | 100% | 0% | 0% |
| Semi-generalized (k = 9) | 2.79 (1.09) | 3.55 (1.26) | 1.40 (0.92) | 30.44 (32.88) | 78% | 11% | 11% |
| Generalized (k = 13) | 3.08 (1.50) | 3.39 (0.85) | 5.67 (9.92) | 29.62 (35.97) | 38% | 38% | 24% |
Significant between-subgroup difference
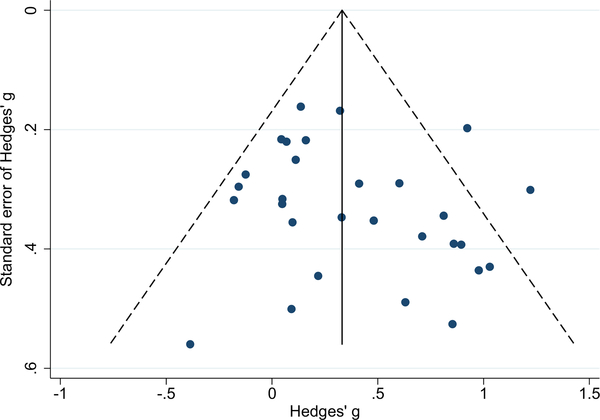
Publication Bias
A funnel plot of the relationship between effect size and standard error is shown in Fig. 6. An Egger’s test of small study bias had a p-value of 0.267. The null hypothesis that no small-study bias exists from this value cannot be rejected, suggesting that the slight asymmetry in the funnel plot is not a significant concern.
Fig. 6.
Funnel plot of included studies: effect size and standard error
Discussion
This meta-analysis examined the effects of early interventions on social communication outcomes for young children with ASD. A random effects model of the 29 included studies resulted in an aggregated effect size of g = 0.355. Participants in intervention groups showed significantly greater improvements on social communication outcomes than participants in control groups (p < 0.001). This effect size represents about five additional initiations of social communication during the ESCS or approximately one additional communicative initiation every 5-min. Although this may seem like a small change, this is a notable increase for children with ASD who are characterized by functional deficits in this area. In addition, because initiations of social communication set the occasion for responsive communication and linguistic input from others, this change in child behavior may be important. In general, the more the child with ASD initiates, the more frequently other persons respond. Increased social initiations may result in increased contingent language modeling as well as more positive responses from others, which may reinforce the child for communicating. Increased social initiations are especially important given evidence that social communication correlates with positive long-term language outcomes (Mundy et al. 1990; Sigman and Ruskin 1999; Charman 2003). Thus, the findings of this meta-analysis are important in demonstrating that social communication can be increased as a result of early intervention.
Mean study age was associated with treatment effect size on social communication outcomes; optimal social communication outcomes were observed when the mean age of the participants was 3.81 years, with positive effects diminishing somewhat after that age. This finding is important from a practical standpoint as it may indicate an optimal age to focus early intervention for this particular skill. Alternatively, children with ASD around this age may be more developmentally ready to learn the skills targeted in these interventions than children at younger ages. Further research is needed to better understand why interventions to improve social communication are most effective at this age including examining developmental covariates such as symbolic play, emerging verbal repertoire, and responsiveness to joint attention. In addition, further research is needed to develop more effective strategies for improving social communication in children with ASD at younger ages. However, these findings should be taken cautiously; the meta-regression used the study-level variable of mean participant age to predict the between-group difference effect size of social communication outcomes across studies. Using individual data would be better suited for this question; however, it was not possible to acquire individual participant data from all 29 included studies.
Although the magnitude of effects of social communication interventions varied depending on the type of individual providing the intervention, the differences were not significant. The largest effect sizes were associated with clinician- implemented intervention. Studies in which a researcher or therapist provided the intervention had the largest aggregated effect (g = 0.587). When parents were included in the delivery of the intervention, the effects tended to be smaller in magnitude and more variable, but remained significant. When school staff implemented the intervention, the effect was not significant. The overall effect size for parents was g = 0.330 which is comparable to the effect sizes for communication outcomes in a meta-analysis of parent-implemented interventions (Roberts and Kaiser 2011). However, these findings differ from those of Hampton and Kaiser (2016) in which the parent plus clinician model of implementation resulted in the largest increases in spoken language. Further research needs to examine factors that may explain the apparent reductions in effectiveness when interventions are delivered by parents or teachers rather than clinicians or researchers. One reason may be in issues related to intervention fidelity. Few studies measured and reported both the researcher’s fidelity in training the parent or school staff member and the parent or school staff member’s fidelity in delivering the intervention to the child. By understanding fidelity at these two levels, we can better identify whether it is the training protocol for teaching adults to implement the intervention strategies or the fidelity with which intervention strategies are implemented with the child that reduces the benefits of intervention. Furthermore, measures of dosage, discussed below, are difficult to estimate in studies where parents or school staff are trained to deliver an intervention across daily activities at home or in the classroom. In schools, where staff may teach several children with ASD in one classroom, the dosage may be variable based on child characteristics and staffing assignments. Lastly, the finding should be considered cautiously because only four studies examined interventions delivered by school staff members, and these studies included children who were older compared to studies implemented by parents and researchers. More research is needed to better understand the potential effects of school-based social communication interventions.
The magnitude of effect sizes was associated with measurement type, consistent with Yoder et al.’s previous findings (2013). Studies reporting context-bound measurements had an aggregated effect size more than two times the size of the aggregated effect of studies reporting semi-generalized and generalized measures. To put this into perspective, the aggregated effect size for studies using a proximal measure equates to about 8.6 more initiations of social communication compared to the control group during a 25-min observation, whereas interventions that measured communication with a generalized measure would show a benefit of only about 3.6 communicative initiations in the same amount of time. This finding is important for two reasons. First, it demonstrates that the measures used in a study can have a substantial impact on the study findings. Second, it may indicate that although the interventions used across these studies are, in general, effective in improving social communication outcomes, optimal performance of these behaviors may depend on partner support. Both context-bound and semi-generalized measures are dyadic in nature. That is to say, because the person implementing the intervention is being trained in novel strategies, the outcome measure is capturing the child’s behavior change in the presence of the partner’s behavior change. The smaller effect sizes associated with generalized outcome measures indicate that children may not be demonstrating changes in communication behaviors to the same extent in the absence of the trained partner. Although the aggregated effect size of semi-generalized measures was more similar to that of generalized measures than to that of context-bound measures, the same limitations of measurement are also true of semi-generalized outcomes measures, given that these measures are also dyadic in nature. The smaller effect sizes associated with semi-generalized measures could indicate that the child is not generalizing the social communication behaviors to the new context with the trained partner, or could indicate that the partner is not generalizing their newly trained intervention strategies to an untrained context. In this meta-analysis, the majority of studies (k = 16) used a dyadic measure of social communication, which limits the interpretations of the results. It is crucial for future studies that use a mediated approach to intervention (delivered by either parent or school staff) to include a measure of generalization to an untrained partner. Further research is needed to examine the relationship between social communication and measurement context and to improve generalization of social communication across contexts and to untrained partners.
Limitations
One limitation was the wide range of outcome variables the studies reported. The majority of studies used observational measures, and many of these used different criteria to determine the construct of social communication. For this reason, this meta-analysis included all intentional communication with a social partner in the definition of social communication. Considering the important nature of this specific skill as a core feature of ASD, future studies should attempt to measure this behavior using a consistent and systematic definition of the behavior.
A second limitation was in the definition of dosage used in the analysis. Intervention dosage (total number of hours) and intervention duration (total number of weeks) were not associated with outcomes. This is contrary to the expectation that interventions with a higher dosage would be associated with more positive outcomes. However, this finding is consistent with Hampton and Kaiser’s (2016) findings that intervention dosage was not significantly related to spoken language outcomes for young children with ASD. This finding may be due, in part, to the difficulty in estimating the exact dosage of the interventions in this sample of studies. Of the 29 included studies, 23 studies used a mediated treatment approach, meaning that parents or school staff members were trained to implement the intervention with the participating children. In the majority of these studies, the dosage of intervention reported was not the time the implementers used the intervention strategies with the children, but rather the time research personnel were training the parents or school staff. The sessions typically included practice with the target children, but the proportion of session time allocated to teaching the implementer vs the implementer delivering the intervention was not reported. Studies rarely reported the implementers’ use of the social communication intervention when the research personnel were not present. Thus, it is difficult to accurately measure the dosage of intervention that the children received in studies that used a mediated approach. For this reason, duration was included as a more appropriate measure of dosage than total hours of intervention. However, there are limitations with this as well, given the variability in intensity of intervention, particularly for long term studies. For example, Kamps et al. (2015) provided an intervention that was low in dosage over a long period of time (0.46 h per week for 104 weeks) while Boyd et al. (2014) provided high-dosage, early intervention programs over the same period of time (25.6 h per week for 104 weeks). Overall, estimated dosage for studies in this sample may not be an accurate indicator of the amount of intervention children actually received. Additionally, both measures of dosage were measured on a continuum; threshold effects of dosage could not be modeled.
Another limitation was variability within the sample of studies. The studies included a wide range of measures, dosage, intervention types, and intervention agents. This variability is likely the reason for the significant amount of heterogeneity in the analysis. Although some study-level variables accounted for a part of the heterogeneity, a moderate amount of heterogeneity (I2 = 37.28%) was unexplained. Additional analyses could further examine this heterogeneity, but measures of important child-level variables such as IQ, autism severity, and treatment history and intervention- level variables such as implementation fidelity were not consistently reported across studies to conduct additional analyses. Consistent and comprehensive reporting of child and intervention characteristics would allow for a future meta-analysis that could analyze the active ingredients of intervention that are associated with better outcomes for children with ASD. Identifying the active ingredients of intervention would have a critical impact on the development of more efficient and effective intervention strategies for this population.
The last limitation of this analysis was in the coding definitions used to assess risk of bias. Risk of bias was not significantly associated with outcomes. It is possible that bias in the body of literature had an effect on the outcomes, but that a more comprehensive measure of bias was needed to detect this. However, due to inconsistent reporting of study procedures, a more comprehensive measure of bias was not possible. For example, many studies failed to report necessary measures such as fidelity (including both the fidelity of the researcher training the parent and the fidelity of the parent implementing the strategies with the child), assessment fidelity, and coding reliability. Future studies should more consistently report these methodological aspects that are related to study quality.
Conclusions
The findings of this meta-analysis indicate that social communication is a characteristic of children with ASD that can be improved by early intervention. Largest effect sizes were observed for studies that had an average age of participants of 3.81 years. Although the largest effects were observed when the intervention was delivered by clinicians, the outcomes of interventions implemented by parents were also significant. However, the effect sizes following intervention were largest for outcomes measured in contexts similar to the intervention context, and smaller in size when the effects were measured in a generalized setting. Given these results are based on meta-analyses of 29 group experimental design studies, the results appear to be both trustworthy and important, with the limitations discussed.
Future research should examine the specific components of interventions that are associated with greater gains in social communication and should include strategies for improving the delivery of effective intervention strategies by parents, school staff, and other community providers, as well as improved abilities to generalize social communication behaviors to novel contexts and untrained partners. It is important to continue to develop interventions for young children with ASD during the period when social communication typically emerges.
Acknowledgments
This research was supported in part by OSEP Grant #H325D100034A (Doctoral Leadership Training in Early Childhood Special Education, U. S. Department of Education; A. Kaiser, PI). We acknowledge the contributions of Emily Tanner-Smith, Ph.D. to earlier drafts of this paper and Lauren H. Hampton, Ph.D. for her reliability coding support.
Funding This research was supported in part by OSEP Grant #H325D100034A (Doctoral Leadership Training in Early Childhood Special Education, U. S. Department of Education; A. Kaiser, PI).
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Compliance with Ethical Standards
Research Involving Human Participants and/or Animals This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent For this meta-analysis, all data came from published or publicly available manuscripts, and thus formal consent was not required.
Publisher′s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aldred C, Green J, & Adams C (2004). A new social communication intervention for children with autism: Pilot randomised controlled treatment study suggesting effectiveness. Journal of Child Psychology and Psychiatry, 45(8), 1420–1430. [DOI] [PubMed] [Google Scholar]
- Amendah D, Grosse SD, Peacock G, & Mandell DS (2011). The economic costs of autism: A review In Amaral D, Geschwind D & Dawson G (Eds.), Autism spectrum disorders (pp. 1347–1360). Oxford: Oxford University Press. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, … Durkin, M. S. (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveillance Summaries, 67(6), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauminger N, & Kasari C (2000). Loneliness and friendship in high-functioning children with autism. Child Development, 71(2), 447–456. [DOI] [PubMed] [Google Scholar]
- Bellini S, Peters JK, Benner L, & Hopf A (2007). A meta-analysis of school-based social skills interventions for children with autism spectrum disorders. Remedial and Special Education, 28(3), 153–162. [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, & Rothstein HR (2009). Introduction to meta-analysis Chichester: Wiley. [Google Scholar]
- Boyd BA, Hume K, McBee MT, Alessandri M, Gutierrez A, Johnson L, … Odom SL (2014). Comparative efficacy of LEAP, TEACCH and non-model-specific special education programs for preschoolers with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44(2), 366–380. 10.1007/s10803-013-1877-9. [DOI] [PubMed] [Google Scholar]
- Carter AS, Messinger DS, Stone WL, Celimli S, Nahmias AS, & Yoder P (2011). A randomized controlled trial of Hanen’s “More than Words” in toddlers with early autism symptoms. Journal of Child Psychology and Psychiatry, 52(7), 741–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casenhiser DM, Shanker SG, & Stieben J (2013). Learning through interaction in children with autism: Preliminary data from a social-communication-based intervention. Autism: The International Journal of Research and Practice, 17(2), 220–241. [DOI] [PubMed] [Google Scholar]
- Chang YC, Shire SY, Shih W, Gelfand C, & Kasari C (2016). Preschool deployment of evidence-based social communication intervention: JASPER in the classroom. Journal of Autism and Developmental Disorders, 46(6), 2211–2223. [DOI] [PubMed] [Google Scholar]
- Charman T (2003). Why is joint attention a pivotal skill in autism? Philosophical Transactions of the Royal Society of London B: Biological Sciences, 358(1430), 315–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clionsky LN (2012). Child directed interaction training for young children with autism spectrum disorders: The impact on child language, social skills, adaptive skills, and problematic behaviors. Retrieved from ProQuest Central; ProQuest Dissertations & Theses Global. [Google Scholar]
- Constantino JN (2002). Social responsiveness scale (SRS). Los Angeles: Western Psychological Services. [Google Scholar]
- Delgado C, Mundy P, & Block J (2001). Pictorial Infant Communication Scales (PICS), Version 1.3. Coral Gables: University of Miami. [Google Scholar]
- Drew A, Baird G, Baron-Cohen S, Cox A, Slonims V, Wheel-wright S, et al. (2002). A pilot randomized control trial of a parent training intervention for pre-school children with autism: Preliminary findings and methodological challenges. European Child and Adolescent Psychiatry, 11, 266–272. [DOI] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldevik S, Hastings RP, Hughes JC, Jahr E, Eikeseth S, & Cross S (2009). Meta analysis of early intensive behavioral intervention for children with autism. Journal of Clinical Child & Adolescent Psychology, 38(3), 439–450. [DOI] [PubMed] [Google Scholar]
- Field T, Lasko D, Mundy P, Henteleff T, Kabat S, Talpins S, & Dowling M (1997). Brief report: Autistic children’s attentiveness and responsivity improve after touch therapy. Journal of Autism and Developmental Disorders, 27(3), 333–338. 10.1023/A:1025858600220. [DOI] [PubMed] [Google Scholar]
- Gillespie-Lynch K, Sepeta L, Wang Y, Marshall S, Gomez L, Sigman M, & Hutman T (2012). Early childhood predictors of the social competence of adults with autism. Journal of Autism and Developmental Disorders, 42(2), 161–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goods KS, Ishijima E, Chang Y-C, & Kasari C (2013). Pre-school based JASPER intervention in minimally verbal children with autism: Pilot RCT. Journal of Autism and Developmental Disorders, 43(5), 1050–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granpeesheh D, Dixon DR, Tarbox J, Kaplan AM, & Wilke AE (2009). The effects of age and treatment intensity on behavioral intervention outcomes for children with autism spectrum disorders. Research in Autism Spectrum Disorders, 3(4), 1014–1022. [Google Scholar]
- Green J, Charman T, McConachie H, Aldred C, Slonims V, How- lin P, … Pickles A (2010). Parent-mediated communication- focused treatment in children with autism (PACT): A randomised controlled trial. The Lancet, 375(9732), 2152–2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampton LH, & Kaiser AP (2016). Intervention effects on spoken- language outcomes for children with autism: A systematic review and meta-analysis. Journal of Intellectual Disability Research, 60(5), 444–463. [DOI] [PubMed] [Google Scholar]
- Hardan AY, Gengoux GW, Berquist KL, Libove RA, Ardel CM, Phillips J, … Minjarez MB (2015). A randomized controlled trial of Pivotal Response Treatment Group for parents of children with autism. Journal of Child Psychology and Psychiatry, 56(8), 884–892. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris SL, & Handleman JS (2000). Age and IQ at intake as predictors of placement for young children with autism: A four-to six-year follow-up. Journal of Autism and Developmental Disorders, 30(2), 137–142. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Altman DG, Gøtzsche PC, Juni P, Moher D, Oxman AD, … Sterne JA (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ, 343, d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang B, & Hughes C (2000). The effects of social interactive training on early social communicative skills of children with autism. Journal of Autism and Developmental Disorders, 30(4), 331–343. [DOI] [PubMed] [Google Scholar]
- Ingersoll B (2012). Effect of a focused imitation intervention on social functioning in children with autism. Journal of Autism and Developmental Disorders, 42(8), 1768–1773. 10.1007/s10803-011-1423-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamps D, Thiemann-Bourque K, Heitzman-Powell L, Schwartz I, Rosenberg N, Mason R, & Cox S (2015). A comprehensive peer network intervention to improve social communication of children with autism spectrum disorders: A randomized trial in kindergarten and first grade. Journal of Autism and Developmental Disorders, 45(6), 1809–1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karst JS (2010). Child and caregiver social behavior and joint attention change following P.L.A.Y. project intervention (M.S.). Marquette University, United States—Wisconsin: Retrieved from http://search.proquest.com.proxy.library.vanderbilt.edu/docview/821240017/abstract/C2464529FB3144AFPQ/22?accountid=14816#. [Google Scholar]
- Kasari C, Freeman S, & Paparella T (2006). Joint attention and symbolic play in young children with autism: A randomized controlled intervention study. Journal of Child Psychology and Psychiatry, 47(6), 611–620. 10.1111/j.1469-7610.2005.01567.x. [DOI] [PubMed] [Google Scholar]
- Kasari C, Gulsrud A, Paparella T, Hellemann G, & Berry K (2015). Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. Journal of Consulting and Clinical Psychology, 83(3), 554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C, Gulsrud AC, Wong C, Kwon S, & Locke J (2010). Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. Journal of Autism and Developmental Disorders, 40(9), 1045–1056. 10.1007/s10803-010-0955-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keen D, Couzens D, Muspratt S, & Rodger S (2010). The effects of a parent-focused intervention for children with a recent diagnosis of autism spectrum disorder on parenting stress and competence. Research in Autism Spectrum Disorders, 4(2), 229–241. 10.1016/j.rasd.2009.09.009. [DOI] [Google Scholar]
- Koegel RL, Koegel LK, & Surratt A (1992). Language intervention and disruptive behavior in preschool children with autism. Journal of Autism and Developmental Disorders, 22(2), 141–153. 10.1007/BF01058147. [DOI] [PubMed] [Google Scholar]
- Lawton K, & Kasari C (2012). Teacher-implemented joint attention intervention: Pilot randomized controlled study for preschoolers with autism. Journal of Consulting and Clinical Psychology, 80(4), 687–693. 10.1037/a0028506. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, Dilavore PC, & Risi S (2008). Autism diagnostic observation schedule (ADOS). Boston: Hogrefe. [Google Scholar]
- Mahoney G, Kim JM, & Lin C (2007). Pivotal behavior model of developmental learning. Infants & Young Children, 20(4), 311–325. [Google Scholar]
- McCalla MK (2014). Enhancing the social interactions of pre-school children with autism: The effectiveness of a peer-mediated intervention. Retrieved from ProQuest Central; ProQuest Dissertations & Theses Global; (1614189419). [Google Scholar]
- Mundy P, Delgado C, Block J, Venezia M, Hogan A, & Seibert J (2003). Early social communication scales (ESCS). Coral Gables, FL: University of Miami. [Google Scholar]
- Mundy P, Sigman M, & Kasari C (1990). A longitudinal study of joint attention and language development in autistic children. Journal of Autism and Developmental Disorders, 20(1), 115–128. [DOI] [PubMed] [Google Scholar]
- Mundy P, Sigman M, Ungerer J, & Sherman T (1986). Defining the social deficits of autism: The contribution of non-verbal communication measures. Journal of Child Psychology and Psychiatry, 27(5), 657–669. [DOI] [PubMed] [Google Scholar]
- Myers SM, & Johnson CP (2007). Management of children with autism spectrum disorders. Pediatrics, 120(5), 1162–1182. [DOI] [PubMed] [Google Scholar]
- Nefdt N (2007). The use of a self-directed learning program to provide introductory training to parents of children with autism (Ph.D). University of California, Santa Barbara, Ann Arbor: Retrieved from ProQuest Dissertations & Theses Full Text. (304881365). [Google Scholar]
- Openden DA (2005). Pivotal response treatment for multiple families of children with autism: Probable efficacy and effectiveness of a group parent education workshop (Ph.D.). University of California, Santa Barbara, Ann Arbor: Retrieved from ProQuest Dissertations & Theses Full Text; (305004072). [Google Scholar]
- Remington B, Hastings RP, Kovshoff H, degli Espinosa F, Jahr E, Brown T, … Ward N. (2007). Early intensive behavioral intervention: Outcomes for children with autism and their parents after two years. American Journal on Mental Retardation, 112(6), 418–438. 10.1352/0895-8017(2007)112[418:EIBIOF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Roberts MY, & Kaiser AP (2011). The effectiveness of parent- implemented language interventions: A meta-analysis. American Journal of Speech-Language Pathology, 20(3), 180–199. [DOI] [PubMed] [Google Scholar]
- Rogers SJ, Estes A, Lord C, Vismara L, Winter J, Fitzpatrick A, … Dawson G (2012). Effects of a brief Early Start Denver Model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 51(10), 1052–1065. 10.1016/j.jaac.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salt J, Shemilt J, Sellars V, Boyd S, Coulson T, & McCool S (2002). The Scottish Centre for Autism preschool treatment programme. Autism, 6(1), 33–46. 10.1177/1362361302006001004. [DOI] [PubMed] [Google Scholar]
- Schertz HH, Odom SL, Baggett KM, & Sideris JH (2013). Effects of joint attention mediated learning for toddlers with autism spectrum disorders: An initial randomized controlled study. Early Childhood Research Quarterly, 28(2), 249–258. 10.1016/j.ecresq.2012.06.006. [DOI] [Google Scholar]
- Sigman M, & Ruskin E (1999). Social competence in children with Autism, Down syndrome and other developmental delays: A longitudinal study. Monographs of the Society for Research in Child Development, 64(1), 1–114. [DOI] [PubMed] [Google Scholar]
- Smith T, Groen AD, & Wynn JW (2000). Randomized trial of intensive early intervention for children with pervasive developmental disorder. American Journal on Mental Retardation, 105, 269–285. [DOI] [PubMed] [Google Scholar]
- Solomon R, Van Egeren LA, Mahoney G, Huber MSQ, & Zimmerman P (2014). PLAY Project Home Consultation intervention program for young children with autism spectrum disorders: A randomized controlled trial. Journal of Developmental and Behavioral Pediatrics, 35(8), 475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone WL, Coonrod EE, Pozdol SL, & Turner LM (2003). The Parent Interview for Autism-Clinical Version (PIA-CV): A measure of behavioral change for young children with autism. Autism, 7(1), 9–30. [DOI] [PubMed] [Google Scholar]
- Turner-Brown L, Hume K, Boyd BA, & Kainz K (2016). Preliminary efficacy of Family Implemented TEACCH for toddlers: Effects on parents and their toddlers with autism spectrum disorder. Journal of Autism and Developmental Disorders. 10.1007/s10803-016-2812-7. [DOI] [PubMed] [Google Scholar]
- Venker CE, McDuffie A, Weismer SE, & Abbeduto L (2012). Increasing verbal responsiveness in parents of children with autism: A pilot study. Autism, 16(6), 568–585. 10.1177/1362361311413396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virués-Ortega J (2010). Applied behavior analytic intervention for autism in early childhood: Meta-analysis, meta-regression and dose-response meta-analysis of multiple outcomes. Clinical Psychology Review, 30(4), 387–399. [DOI] [PubMed] [Google Scholar]
- Wetherby AM, & Prizant B (2002). Communication and symbolic behavior scales developmental profile. Baltimore: Paul H. Brookes. [Google Scholar]
- Wetherby AM, & Woods JJ (2006). Early Social Interaction Project for children with autism spectrum disorders beginning in the second year of life: A preliminary study. Topics in Early Childhood Special Education, 26(2), 67–82. [Google Scholar]
- Whalen C, & Schreibman L (2003). Joint attention training for children with autism using behavior modification procedures. Journal of Child Psychology and Psychiatry, 44(3), 456–468. [DOI] [PubMed] [Google Scholar]
- Yoder PJ, Bottema-Beutel K, Woynaroski T, Chandrasekhar R, & Sandbank M (2013). Social communication intervention effects vary by dependent variable type in preschoolers with autism spectrum disorders. Evidence-Based Communication Assessment and Intervention, 7(4), 150–174. [DOI] [PMC free article] [PubMed] [Google Scholar]