Abstract
Background
In June 2020, a large randomised controlled clinical trial in the UK found that dexamethasone was effective in reducing the number of deaths in patients with severe coronavirus disease 2019 (COVID-19).
Case description
We describe a patient with rapid worsening of COVID-19 pneumonia and its dramatic improvement under corticosteroids.
Discussion
Corticosteroids could be useful in patients with an inflammatory profile, considering that acute respiratory distress syndrome may be the consequence of cytokine storm syndrome.
LEARNING POINTS
One of the main pathophysiological hypotheses for severe COVID-19 pneumonia is inappropriate immunological hyperactivation.
Corticosteroid therapy may be useful in these patients.
Keywords: COVID-19, coronavirus, cytokine storm syndrome, computed tomography, corticosteroids
CASE DESCRIPTION
In March 2020, a 48-year-old man with a history of diabetes and former smoking presented with a 5-day history of fever and abdominal pain. He also reported diarrhoea, fatigue and dry cough. A thoracic computed tomography (CT) scan revealed minimal ground-glass opacity affecting <10% of the total pulmonary parenchyma. This was consistent with symptoms of coronavirus disease 2019 (COVID-19) which was confirmed by a nasopharyngeal swab. Arterial blood gas was normal; the patient was discharged.
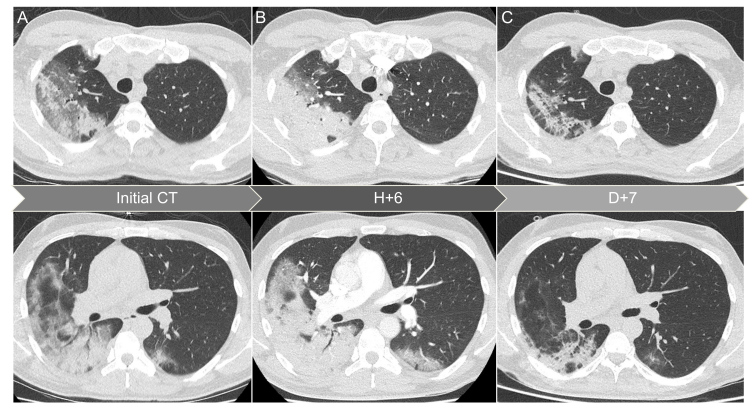
Ten days later, the patient presented with persistent cough, fever and shortness of breath. He was febrile and tachypnoeic at 25 breaths per minute. His oxygen saturation was 88% on ambient air and lung auscultation revealed bilateral crackles. A thoracic CT scan showed significant bilateral ground-glass opacities affecting 25–50% of the total pulmonary parenchyma, associated with alveolar condensations (Fig. 1A). Laboratory findings revealed elevated C-reactive protein (263 mg/l), a normal neutrophil count with mild lymphopenia (740/μl) and increased ferritin (1,970 μg/l). Supplemental oxygen was started at 6 l/min and arterial blood gas analysis revealed PaO2 95 mmHg, PaCO2 34 mmHg and pH 7·48.
Figure 1.
Thoracic CT images of a 48-year-old man with COVID-19 pneumonia. (A) Axial CT images at admission showed significant bilateral ground glass opacities with alveolar condensations; (B) 6 hours later, CT images revealed a marked increase in lesions; (C) CT images on day 7, after 5 days of corticosteroid use, showed a significant decrease in lesions
Treatment with intravenous amoxicillin and clavulanic acid was initiated. The patient exhibited an elevated level of D-dimer (6,600 μg/l) and thoracic CT angiography was conducted 6 hours after the previous CT scan. There was a dramatic increase in opacities but no evidence of pulmonary embolism (Fig. 1B). Due to the rapid worsening of the patient’s condition, he was hospitalised in an intermediate care unit and intravenous dexamethasone was started at 20 mg per day, for 5 days. His condition improved in a few hours with a decrease in oxygen requirements. He remained afebrile after corticosteroid initiation. Bacterial blood and sputum culture remained sterile. On day 7, a thoracic CT scan showed a significant decrease in the lesions previously seen (Fig. 1C). The patient was discharged the following day.
DISCUSSION
Our patient experienced rapid worsening of COVID-19 pneumonia after 2 weeks of evolution, with a dramatic increase in thoracic CT lesions within hours. This, associated with high levels of inflammatory markers and prompt improvement after corticosteroid initiation, underlines the hypothesis of cytokine storm syndrome. This syndrome is characterised by increased levels of pro-inflammatory cytokines, such as tumour necrosis factor-α or several interleukins, resulting in immunological hyperactivation and worsening of lung damage [1, 2]. Other anti-inflammatory agents or targeted therapies, such as tocilizumab, have demonstrated a potentially positive impact in these situations [3, 4]. In a recent study, Wu et al. reported a reduced risk of death in patients with acute respiratory failure receiving methylprednisolone [5]. In June 2020, the investigators of the RECOVERY (Randomised Evaluation of COVid-19 thERapY) trial, which enrolled over 11,500 patients in the UK, reported a reduction in death of up to one-third in hospitalised patients with severe respiratory complications of COVID-19 treated with dexamethasone [6]. Pending publication of the results of the RECOVERY trial, caution is advised and further studies are urgently needed to define the best therapeutic strategy in these patients.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interests.
REFERENCES
- 1.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henderson L, Canna S, Schulert G, Volpi S, Lee P, Kernan K, et al. On the alert for cytokine storm: immunopathology in COVID-19. Arthritis Rheum. 2020;72(7):1059–1063. doi: 10.1002/art.41285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Capra R, De Rossi N, Mattioli F, Romanelli G, Scarpazza C, Sormani M, et al. Impact of low-dose tocilizumab on mortality rate in patients with COVID-19 related pneumonia. Eur J Intern Med. 2020;76:31–35. doi: 10.1016/j.ejim.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toniati P, Piva S, Cattalini M, Garrafa E, Regola F, Castelli F, et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: a single center study of 100 patients in Brescia, Italy. Autoimmun Rev. 2020;19:102568. doi: 10.1016/j.autrev.2020.102568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oxford University News Release. Low-cost dexamethasone reduces death by up to one third in hospitalised patients with severe respiratory complications of COVID-19. Jun 16, 2020. Available from: https://www.recoverytrial.net/files/recovery_dexamethasone_statement_160620_v2final.pdf.