The novel coronavirus disease 2019 (COVID-19) was first identified in Wuhan, China in December 2019.1 Since then, the New York metropolitan region has quickly become the epicenter of the COVID-19 pandemic in the United States, with >175,000 cases and >20,000 deaths to date.2
The Columbia University Irving Medical Center (CUIMC) is a 738 adult inpatient bed tertiary care hospital in the Washington Heights neighborhood of New York City (NYC) and is one of 11 hospitals in the New York Presbyterian Hospital (NYP) system. Nephrology also staffs a second 196-bed hospital in the Inwood neighborhood of Northern Manhattan. The first patient with COVID-19 at CUIMC was diagnosed on March 1. Travel restrictions for clinical staff were instituted on March 4. By April 10, the nephrology service size had increased by 50%, and patients with COVID-19 accounted for 90% of the census (Figure 1A).
Figure 1.
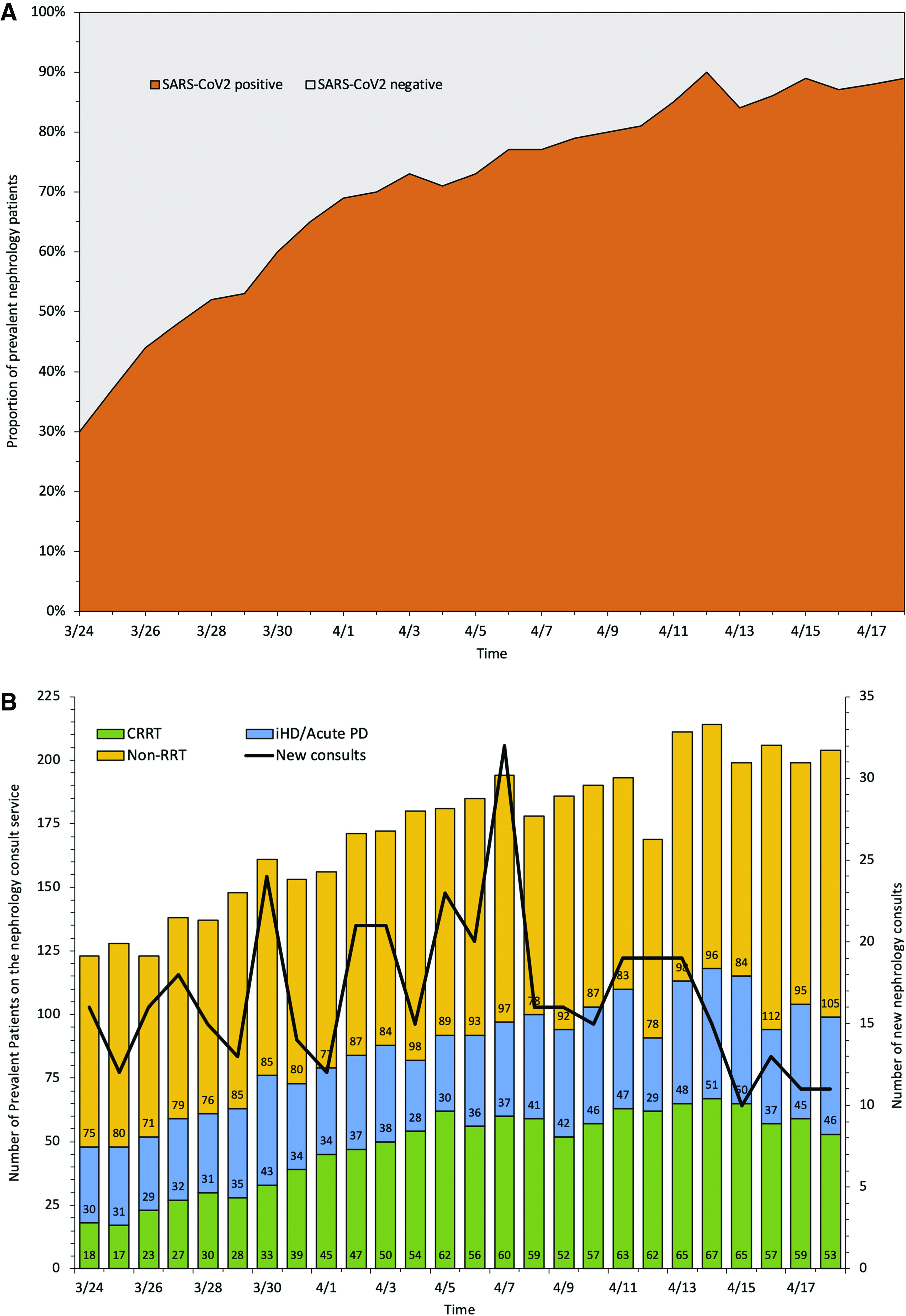

Nephrology consult service trends over time during the COVID-19 pandemic surge at Columbia University Irving Medical Center. (A) Proportion of patients with COVID-19 on the nephrology service. (B) Trends for new nephrology consults and for prevalent patients being followed by the nephrology service during the COVID-19 pandemic surge at CUIMC. (C) Comparison of the trends for patients with COVID-19 (COVID) admitted to the ICU and the number of these patients requiring CRRT. iHD, inpatient hemodialysis; PD, peritoneal dialysis; SARS-CoV2, severe acute respiratory syndrome coronavirus 2.
Although early reports did not emphasize a high prevalence of AKI in critically ill patients with COVID-19,3 it was clear that many patient populations with underlying kidney diseases would be highly vulnerable to COVID-19, such as individuals with underlying diabetes and cardiovascular comorbidities, kidney transplant recipients, patients with glomerular disease on immunosuppression, as well as individuals with ESKD treated with in-center hemodialysis who could not exercise social distancing. In light of the dire predictions of a surge of critically ill patients in NYC and specific concerns for COVID-19 in patients with kidney disease, the Division of Nephrology at CUIMC/NYP started to reorganize in February 2020. Here, we describe the principal elements of our response, early lessons learned during the pandemic in NYC and the major reconfigurations of services (Tables 1 and 2).
Table 1.
Columbia University Division of Nephrology Clinical Services at baseline and during the pandemic surge
| Service | Usual (April 2019) | Surge (April 2020) |
|---|---|---|
| Number of ICU hospital beds | 139 | 312 |
| Number of nephrology clinical services | 6 | 9 |
| Total inpatient hemodialysis treatments | 911 | 1114 |
| Total inpatient hemodialysis unit treatments | 741 | 738 |
| Total inpatient hemodialysis bedside treatments | 170 | 376 |
| Hemodialysis bedside/total treatments (%) | 23 | 51 |
| CRRT cases per day | <24 | 67 (peak) |
| Acute peritoneal dialysis cases per day | 0 | 7 |
Table 2.
CUIMC dialysis capacity at baseline and during the pandemic surge
| Service | Baseline | Anticipated Surge Needs | Actual Surge Resources |
|---|---|---|---|
| Total hemodialysis machines | 25 | 40 | 28 |
| Total hemodialysis nurses | 34 | 48 | 37 |
| Hemodialysis unit nursing staffing ratio | 1:2 | 1:2 | 1:3 |
| Bedside hemodialysis nursing staffing ratio | 1:1 | 1:1 | 1:1 |
| CRRT machines | 27 | 73 | 50 (peak) |
Organization of the Crisis Team and Division Communication
Response to the pandemic required a team-based approach that combined multiple competencies. The division benefited from a strong preexisting administrative and communication structure anchored by weekly administrative meetings, during which physician leadership and administrators discussed ongoing clinical, research, and operational issues. The group culture was one of open discussion and shared decision-making, leading to high trust between members.
The division’s response to COVID-19 started with a decision to update the contact list for all personnel, order personal protective equipment, and assess existing capacities of clinical services. In addition, we had a series of calls with Dr. Francesco Scolari, the Chief of the Division of Nephrology at the University of Brescia (one of the hardest-hit hospitals in Italy). Dr. Scolari and other nephrology faculty members generously shared their experience and protocols with us, greatly informing and facilitating our early response.4
The existing organizational structure was then reformulated to develop a crisis team gathering unit directors, nursing leaders, and administrators (Supplemental Figure 1). Guiding principles for the crisis team included excellence in patient care, staff safety, data-driven decisions, and an adaptive structure with regular communication. Since March 2020, this leadership group has convened via video calls every evening, following a structured agenda. To make informed decisions based on current needs, physicians rounding on clinical services are invited to attend. The leadership team disseminates information to the division in a variety of communication mechanisms including frequent emails and periodic division-wide video calls where questions are also fielded.
To facilitate coordination of nephrology plans with the institutional response, members of the crisis group were nominated to departmental and hospital workgroups. As the dialysis needs began to challenge resources, the group recognized the need for a coordinated response for RRT across all NYP-affiliated hospitals. A workgroup composed of lead nephrologists from all campuses was formed and the workgroup gathered via video calls daily to track needs and inventory, share dialytic resources, and develop common protocols and innovative solutions. Additional communication channels were maintained with division directors at other academic institutions as well as the American Society of Nephrology.
Developing a Data-Driven Approach
Early reports from China suggested that only 5%–10% of critically ill patients would require RRT,3 but conversations with nephrology colleagues at the University of Brescia alerted us to a higher incidence of AKI and surge of infected patients with ESKD.4
We made an early decision to develop a data-driven approach to guide our response to the anticipated surge (Table 1, Figure 1B). A baseline assessment of staff capacity and dialysis resources was conducted and our maximum capacity with existing resources was modeled. We developed a daily patient census tracking tool using a cloud-based automated spreadsheet that informed rapid changes in how clinicians were deployed (Supplemental Figure 2). We developed a tool to track our continuous RRT (CRRT) machines to confront the potential challenges of sharing machines across ten traditional and new intensive care unit (ICU) locations (Supplemental Figure 2). We developed similar tracking tools to monitor consumable usage and supplies across the NYP campuses. Nomograms were created to reduce dialysate waste (see below).
We modeled best-case and worse-case scenarios using public data from China and Italy to generate projections. We also projected needs for personnel, RRT devices, and supplies, based on the daily census growth in our own nephrology, hospital, and ICU services (Supplemental Figure 3). To date, the ICU census growth has been the best predictor of CRRT needs (Figure 1C).
Reorganization of Clinical Services
Faculty Redeployment
Our faculty includes 30 physicians, and schedules are established 1 year in advance and equitably distributed based on clinical and research responsibilities. Physicians cover 2-week blocks that do not include contiguous weekends. With the surge, the number of physicians needed to cover inpatient services greatly increased. We developed a system of parallel teams of physicians who covered the inpatient services for 7-day stretches including weekends. Each team included a back-up physician in the event the physician on service needed to be quarantined or care for a sick family member (at the time of writing, six physicians [20%] have developed COVID-19 and required quarantine). This system improved continuity of care and limited the risk of exposure of multiple providers to the same patients, particularly early in the pandemic when patient testing was limited and personal protective equipment recommendations were evolving. The week off from inpatient service allowed providers to recover, but also to address urgent outpatient telemedicine visits, outpatient dialysis rounding, and academic or administrative work.
Furthermore, services were changed to a geolocalized model. Geolocalization facilitated communication with floor teams, improved efficiency, and reduced movement within the hospital. The daily census tracking tool allowed for the early detection of changing clinical burden, which in turn informed the development of additional geolocalized teams on a regular basis. Ultimately, nine clinical services were deployed.
The reorganization of our inpatient teams was developed with close consideration to prioritizing faculty safety. To protect fellows, only attending physicians performed physical exams. A pediatric renal fellow redeployed to the expanded adult inpatient service. Faculty who were considered at high risk for complications of COVID-19 remained off inpatient services and were assigned to a new remote inpatient consultative service aiming to decompress the inpatient services. Consults for straightforward problems whose assessment did not require a physical exam were transferred to the remote-medicine nephrologist who would conduct a chart review, communicate with the primary team, leave recommendations, and conduct follow-up on a daily basis. In addition, these faculty members covered outpatient telemedicine visits and administrative tasks such as communicating with nursing leadership and other units of the hospital and working with vendors to ensure an adequate supply of dialysis consumables.
Finally, due to the creation of multiple new ICUs, the department of medicine requested redeployment of physicians to help staff the ICUs. Nephrologists were highly sought after for their expertise in critical care. Ultimately, three nephrologists who volunteered were redeployed to assist the department of medicine. One nephrologist was also redeployed as acting chair of the Allen Hospital.
Outpatient Clinics
Our projections indicated that the surge of inpatients would adversely affect our ability to staff outpatient clinics. Providers were encouraged to move to telemedicine, which was not previously used in the division but was facilitated by a recent transition to a new electronic medical record with an embedded telemedicine tool. Several patient-level barriers to adopting telemedicine were identified, including unfamiliarity with the smartphone-based application needed to communicate with providers and incorporating translators into telemedicine visits for non-English–speaking patients. Research coordinators were redeployed to call and assist patients with participating in telemedicine encounters before the actual visit. When “shelter-in-place” orders were announced in New York, all outpatient clinics were closed and clinic staff were provided mobile telephones and laptops to work remotely.
Kidney Transplant Program
All deceased and living donor kidney transplants were stopped, with the last transplant performed on March 17. Our kidney transplant waitlist was inactivated using the new United Network for Organ Sharing functionality that facilitated this, with the exception of our most highly sensitized patients who might never receive a subsequent kidney offer. Although offers for these patients were considered, no actual transplants were performed. The inpatient service, shared by all solid organ transplant programs, was divided into two geographically separated units: one for transplant recipients who were positive for COVID-19, and the other for those negative for COVID-19.
In-person visits to the outpatient transplant center were limited to the most urgent cases who required face-to-face assessments. All in-person recipient and living donor evaluations were cancelled and a small number were converted to telemedicine visits given the constraints of staff and physician redeployment. This allowed redeployment of staff: some to newly opened inpatient areas, and others to join a team that was established to make daily phone calls to monitor and advise homebound patients with COVID-19 or persons under investigation. We established a registry of all patients with either confirmed or suspected COVID-19 and a standardized questionnaire was used for patient monitoring and appropriate triage. The outpatient infusion center continued to serve those who needed infusions of antirejection medications. With an increasing number of recovering patients with COVID-19 needing either in-person outpatient follow-up and/or infusions, Fridays were reserved exclusively for outpatients with COVID-19.
Outpatient bloodwork at the transplant center was limited to only those in which a rapid turnaround time was essential, such as those with recent transplants immediately preceding the surge or those with an ongoing acute complication. Patients were otherwise directed to outpatient laboratories near their homes to minimize the need for travel.
RRT during the Surge
Inpatient Hemodialysis Unit
In the initial stages of the pandemic, all patients with COVID-19 were dialyzed at the bedside, preserving the inpatient unit for negative cases. However, over time, the majority of our patients on hemodialysis were positive for severe COVID-19, prompting the creation of a COVID-19 shift at the end of the day with terminal cleaning deployed at the end of the shift. By the time of the peak of the surge, we had transitioned to one COVID-19–free shift in the morning, with the subsequent two to three shifts for patients who were positive for COVID-19.
Bedside Dialysis
Demand for bedside dialysis treatments increased rapidly given the increased census in step-down units and ICUs. Moreover, about 20% of our nursing staff were quarantined due to COVID-19 exposure. This required the hiring of additional traveling dialysis nurses and technicians to support a two- to threefold increase in bedside dialysis capacity including scheduled bedside sessions on Sundays (Tables 1 and 2). We designated specific bays in the emergency department for emergent dialysis for patients with COVID-19 who often had severe hyperkalemia. Finally, six research coordinators and noncredentialed physicians were redeployed to the inpatient dialysis unit to help monitor patients and prepare the dialysis machines, enabling increased patient/nurse ratios. This further increased nursing capacity for bedside dialysis cases. Before we were able to hire additional traveling nurses and technicians, our needs exceeded our capacity and we had to reduce all treatment times to 210 minutes or less and reduce treatment frequency to two times a week for those patients who did not have an urgent indication for dialysis.
Continuous RRT
In the provision of RRT, there were several unexpected challenges that required us to innovate quickly. The volume of patients with AKI needing CRRT increased 370% by April 14 (Figure 1C), requiring a daily midmorning virtual huddle to coordinate resources across the multiple geolocalized services. Ahead of the teleconference, an email from each service with their CRRT requests was submitted. When needed, we shared machines every 24 hours rather than every 12 hours to limit the rate of cartridge utilization and reduce nursing burden associated with transitions on or off CRRT. Initially, CRRT dialysate rates were maintained at 25 ml/kg per hour. However, during our peak surge, while working to secure a guaranteed supply of dialysate to meet our needs, for those patients who could metabolically tolerate lower dialysate flow rates, we used a rate of 15–20 ml/kg per hour. After direct coordination with multiple vendors, we were able to increase our dialysate supplies and return flows to our clinical norm.
A senior nephrology fellow coordinated the CRRT service needs across services, liaising with biomedical engineering. Two research coordinators were redeployed to physically locate CRRT machines throughout the hospital and communicate the information to the coordinating fellow. A spreadsheet was created and stored on a shared drive that tracked machine usage and ensured an accurate tally of machines and patients in real time (Supplemental Figure 4). At the conclusion of the teleconference, decisions were communicated to the individual ICU charge nurses by the nephrology fellow and redeployed staff helped track and move machines to their designated locations. This team approach for coordination allowed clinicians to focus on patient care. In newly opened ICU locations, staffed by nurses who were not familiar with CRRT devices, cardiac surgery perfusionists were trained to perform CRRT under the supervision of ICU nursing staff.
Given concerns for a potential shortfall of dialysate, nomograms were created (Supplemental Figure 5) to ensure that there was no dialysate waste, either because of incomplete usage of a dialysate bag or because too many bags were inadvertently spiked at the initiation of CRRT. Concerns about limited consumable supplies led to an effort to expand bedside intermittent hemodialysis to patients on low-dose vasopressor agents and the use of ultrafiltration-only treatment for volume management in patients without metabolic derangements. We also initiated a low-volume, rapid-start acute peritoneal dialysis program for patients who were nonobese with positive end expiratory pressure of 10 cm water or less. Strategies to use lactated Ringer solution or to generate dialysate on-site for the high ongoing CRRT needs have been established. The hypercoagulability that resulted in the frequent loss of CRRT circuits was also a challenge that required rapid escalation of our anticoagulation protocol, including the institution of anti-Xa monitoring for these patients in partnership with hematology.
Finally, the rapid escalation of RRT needs also forced us to become significantly more cognizant of our consumable supply chain, something that is not usually a consideration at other times. The data-driven approach enabled the divisional and departmental leadership to alert hospital leadership, dialysis providers, and vendors of the expanding need for additional machines and supplies. Daily teleconferences were held between the six campuses of the NYP system. Data on CRRT machine supply, CRRT fluids, hemodialysis machine inventory, and availability of personnel were charted daily. The attendees included nursing directors and physicians from each campus. These meetings facilitated the acquisition and equitable distribution of additional CRRT machines and supplies as well as nursing man power for both CRRT and hemodialysis. Based on projections, we also requested and received additional nursing personnel and technicians to help run dialysis treatments at hospitals that were critically affected. Hospital leadership was in contact with state and regulatory agencies to communicate our needs and help navigate challenges with the supply chain. Departmental and division leadership personally worked with multiple vendors to ensure adequate supplies to meet the increased demand.
Outpatient Dialysis
Early on, we recognized the need to communicate with dialysis providers to coordinate outpatient dialysis services given the large number of patients with ESKD being admitted to our hospital.5 We collaborated with outpatient dialysis vendors to open a COVID-19–dedicated dialysis unit. This unit allowed transfer of outpatient ESKD patients with COVID-19 to avoid hospitalization and also facilitated discharge of hospitalized ESKD patients with COVID-19 when stable. The unit opened on April 4, 2020 and serves 43 patients as of the date of writing.
Maintaining Our Academic Mission
With the rapidly evolving pandemic, several divisional conferences were replaced with divisional information sessions. However, resuming these weekly conferences was considered vital to continuing our academic mission as well as maintaining morale within the division. All conferences were converted to a remote videoconferencing system with an increased reliance on internal speakers. Laboratory directors maintained laboratory meeting schedules via video calls. As laboratories were required to ramp down, research assignments were refocused on remote activities such as data curation and analysis. All clinical research visits were either paused or transitioned to tele-visits, except for patients in clinical trials requiring medication administration. To assure retention in clinical studies, we developed a plan to contact research participants and provided them with updates regarding COVID-19 and its impact on research.
Given the relative paucity of data relative to kidney injury in COVID-19 at the time of the surge in New York, the public health value of reporting our experience and early findings was acknowledged within the division. We developed a division-wide institutional review board protocol to track nephrology-specific data and outcomes for our patients. Standardized data capture and survey instruments were developed in collaboration with institution-wide efforts which included a biobank for patients with evidence of severe acute respiratory syndrome coronavirus 2. Research projects were coordinated within the division using a team-based approach for data collection and manuscript writing depending on areas of interest and expertise. Several research laboratories were reoriented to COVID-19 research in an effort to characterize the molecular, genetic, and immunologic basis of disease and its relation to kidney injury. These activities have already led to several early analyses that are in various stages of peer review or publication.5–8
Maintaining Morale
The effects of social distancing and the resultant isolation, the stress of caring for a surge of critically ill patients, and the anxiety of providers concerned for themselves and their families made attentiveness to provider wellness and division morale critical. Division leadership stayed in close daily communication with any faculty member, trainee, or staff under quarantine. Faculty meetings continued and the frequency increased via videoconferencing to provide continued updates as well as ensuring that good news such as faculty promotions and research publications continued to be shared. Daily check-ins were done with all physicians on service in a nightly videoconference call to ensure no one was feeling overwhelmed. The fellowship program director provided a daily update on fellow morale and contributed to the service redesign process, including the formation of a fellow night float system. This system allowed for fellows working in a surge environment to get uninterrupted rest at night and was overwhelmingly well received. Online social events were created for individual groups including research personnel and fellows to minimize feelings of social isolation. The hospital offered various counseling options and wellness areas, the details of which were made available on the hospital website. During the initial weeks of the pandemic, there was—understandably—considerable anxiety among the nursing staff. The medical director and dialysis nursing leadership had daily and open communication with nursing, and their concerns were brought to the daily divisional meeting and addressed in real time. Additional support from the research coordinators and the recruitment of additional staff to help during the surge contributed to a significant reduction of anxiety and improved team morale.
Summary and Planning for the Post-COVID-19 Period
As of this writing, we are still in the middle of the pandemic, but there are early signs that hospital admissions in NYC are declining. Models suggest that there will be a lag phase in ICU admissions, with prolonged hospital stays expected for the patients who are the most critically ill. We are thus expecting a continuation of active participation of nephrologists in the care of many of these patients. Nonetheless, we are cautiously planning for a ramp-up of outpatient clinical services, in coordination with the state-wide relaxation of sheltering recommendations. We anticipate that the ramp-up will place a greater emphasis on remote coordination of care and telemedicine, but—ultimately—in-person patient encounters will be necessary, particularly for patients who postponed urgent nephrology care during the crisis.
In summary, response to a pandemic requires a coordinated approach between nephrologists and other clinical teams, hospital administrators, industry, and regulatory agencies. We described our divisional-wide, data-driven response to the COVID-19 pandemic that allowed us to reorganize our clinical services to provide care for a surge of patients while ensuring provider safety, supporting our academic mission, and supporting our public health obligation of sharing our experiences as widely as possible to inform the community and enable better disaster preparedness (Table 3).
Table 3.
Major challenges and responses to the severe acute respiratory syndrome coronavirus 2 pandemic
| Challenge | Response | Comments |
|---|---|---|
| Organization | Development of a multidisciplinary crisis team with broad representation of physician, nursing, and administrative staff | At peak, ICU beds increased from 139 to 312. OR and cardiac catheterization suites were converted to ICUs. CRRT performed in OR (perfusionists) and regular ICUs (nursing staff) |
| Reorganization of attending and fellow inpatient rotations | ||
| Flexible clinical service structure based on volume data | ||
| Communication | Daily crisis team video call | Supplemental Figure 1 |
| Liaison with institutional workgroups and leadership. Daily intercampus conference call | ||
| Communication with industry | ||
| Communication with regulatory agencies | ||
| Advice from medical centers with special expertise | ||
| Tracking information | Tracking daily census on inpatient services | Supplemental Figures 2–5 |
| New tools for tracking inpatient volume, dialysis machines, and supplies | ||
| Predictive models for patient volume and resources | ||
| Inpatient services | Transition to weekly schedule and adjustment of clinical service based on patient volume | Inpatient services increased from six (hemodialysis, transplant, consults, CRRT, nephro-cardiac, and Allen [Community Hospital]) to nine geolocalized services and one virtual consult service. Number of CRRT patients increased from an average of 20 presurge to a peak of 65. A pediatric renal fellow redeployed to the adult inpatient service |
| Rapid redeployment of attendings, fellows, and research staff | ||
| Geolocalization of services | ||
| Inpatient telemedicine service | ||
| Inpatient RRT | Multi-institutional workgroup to track dialysis resources | 40 new and five rental CRRT machines acquired for six hospitals |
| Interhospital sharing of RRT resources | Ten nurses and four technicians were provided by a CRRT vendor | |
| Daily CRRT huddle to prioritize RRT needs | Identification of “hot spots” based on daily crosscampus teleconference and immediate redeployment of CRRT machines or personnel | |
| New protocols for in-house dialysate production | ||
| Redeployment of research coordinators to assist in the dialysis unit, tracking CRRT machines, and preparation of CRRT dialysate | ||
| Outpatient CKD and ESKD care | Complete conversion to telemedicine | |
| Maintain essential infusions and kidney biopsies | ||
| Dedicated COVID-19+ outpatient dialysis unit | ||
| Redeployment of research coordinator as telemedicine navigators | ||
| Transplantation | Suspension of transplantation program | |
| COVID-19–free and COVID-19–positive designated wards and separate outpatient facilities | ||
| Redeployment of nurses and coordinators to telemedicine calls for outpatients | ||
| Establishment of a registry of patients with COVID-19 and PUI | ||
| Daily calls to all outpatients with COVID-19 and PUI for monitoring/management | ||
| Academic mission | Maintain academic conferences | |
| Convert research efforts to remote activities | ||
| Outreach to participants in observational studies | ||
| Covid-19 IRB protocol for observational studies | ||
| Coordinated COVID-19 research plans | ||
| Share early experience with COVID-19 with community | ||
| Morale and safety | Assignment of at-risk staff to telemedicine activities | |
| Participation of all members of the division in clinical or research activities | ||
| Frequent communication with division members with communication of good news | ||
| Maintenance of administrative activities, promotions, and hiring | ||
| Planning for post-COVID-19 ramp-up |
OR, operating room; PUI, persons under investigation; IRB, institutional review board.
Data Sharing Statement
The tracking tools have been deposited to our university data repository (https://academiccommons.columbia.edu), where they are publicly available for download (https://doi.org/10.7916/d8-kja6-k736 and https://doi.org/10.7916/d8-8619-gn42).
Disclosures
The working group has nothing to disclose.
Funding
None.
Supplementary Material
Acknowledgments
We thank the dialysis nursing staff and technicians for their tireless effort and excellence in patient care. We thank Susan Tanzi-Pfeifer for coordination of RRT resources during the crisis. We are grateful to Nan Chen and Ruijin Hospital for a gift of personal protective equipment. We are immensely grateful to the University of Rochester Division of Nephrology for provision of RRT supplies and Fresenius Medical Care for provision of additional nursing staff, CRRT devices, and supplies at the peak of the crisis.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Contributor Information
Collaborators: Syeda B. Ahmad, Wooin Ahn, Jane Akomeah, Qais Al-Awqati, Maria Alejandra Aponte, Gerald B. Appel, Jonathan Barasch, Irina Y. Baramidze, Andrew Beenken, Andrew S. Bomback, Pietro Canetta, Jae-Hyung Chang, Nisha Clement, David J. Cohen, Bessie N. Craig, Emily Daniel, Russell J. Crew, Denzil Douglas, Geoffrey Dube, Hilda Fernandez, Robin Ferrer, Ali G. Gharavi, Iman Azam Ghavami, Syed Ali Husain, Sean Kalloo, Pascale Khairallah, Jung Soo Kim, Krzysztof Kiryluk, Donald Landry, Jordann Lewis, Meeran Lee, Bruno Lovisi, Allyson R. Medina, Maddalena Marasa, Daisy Mathew, Yonatan Peleg, Karla Mehl, Maria M. Morban, Andrew Moses, Sumit Mohan, Heather Morris, Bradley Nelson, Jordan Gabriela Nestor, Vanna M. Nicasio, Tom Nickolas, Kathryn Paget, Stacey Piva, Jai Radhakrishnan, Maya K. Rao, Simone Sanna-Cherchi, Vaqar Shah, Rosemary V. Sampogna, Shayan Shirazian, Eric Siddall, Piotr Starakiewicz, Jacob S. Stevens, Katherine Toma, Anthony Valeri, Hector Alvarado Verduzco, Gail Williams, Jason Zheng, Sumit Mohan, Maya K. Rao, Jacob S. Stevens, Jai Radhakrishnan, and Ali G. Gharavi
Supplemental Material
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2020040520/-/DCSupplemental.
Supplemental Figure 1. Composition of the crisis team (large oval).
Supplemental Figure 2. Divisional Renal Replacement Therapy Resource Utilization Dashboard (screenshot, DOI pending).
Supplemental Figure 3. Projected growth vs. Actual census growth.
Supplemental Figure 4. CRRT Sharing Protocol Tool.
Supplemental Figure 5. Dialysate Conservation Protocol.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al.: Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China [published correction appears in Lancet 395: 496, 2020]. Lancet 395: 497–506, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.New York City Department of Health and Mental Hygiene: COVID-10: Data. New York, NY, New York City Department of Health and Mental Hygiene, 2020. Available at: https://www1.nyc.gov/site/doh/covid/covid-19-data.page. Accessed May 10, 2020
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al.; China Medical Treatment Expert Group for, Covid-19: Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708–1720, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alberici F, Delbarba E, Manenti C, Econimo L, Valerio F, Pola A, et al.; on behalf of the Brescia Renal COVID Task Force: Management of patients on dialysis and with kidney transplantation during the SARS-COV-2 (COVID-19) pandemic in Brescia, Italy. Kidney Int Rep 5: 580–585, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valeri AM, Robbins-Juarez S, Stevens J, Ahn W, Radhakrishnan J, Gharavi AG, et al.: Presentation and outcomes of patients with end stage kidney disease and COVID-19. J Am Soc Nephrol 31: 1409–1415, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Columbia University Kidney Transplant : Early description of coronavirus 2019 disease in kidney transplant recipients in New York. J Am Soc Nephrol 31: 1150–1156, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pereira MR, Mohan S, Cohen DJ, Husain SA, Dube GK, Ratner LE, et al.: COVID-19 in solid organ transplant recipients: initial report from the US epicenter [published online ahead of print April 24, 2020]. Am J Transplant . Available at: 10.1111/ajt.15941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Husain SA, Dube G, Morris H, Fernandez HE, Chang J-H, Sritharan S, et al.: Early outcomes of outpatient management of kidney transplant recipients with Coronavirus Disease 2019. Clin J Am Soc Nephrol 15: 2020, In press 10.2215/CJN.05170420 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


